January/February 2015 The Offi cial Publication of the ...€¦ · health care and a positive...
Transcript of January/February 2015 The Offi cial Publication of the ...€¦ · health care and a positive...

The Offi cial Publication of the American Chiropractic Association
January/February 2015
www.acatoday.org
ATHEROSCLEROSISSUBLUXATION
MEDICARE All DCs are required
to document the same way
Modic Classifi cations
Childhood Concussion
Ankylosing Spondylitis
Joint Commission Includes Chiropractic

JANUARY/FEBRUARY 20152
FeaturesHealth and Wellness
Chiropractic and Ankylosing Spondylitis 24
When Does Wellness Testing Cause More Harm Than Good? 26
Business and Practice
Managing Risk: Protect Yourself and Your Patients 30
Medical Marketing Priorities for 2015 32
Minute with a Member
A Man of Many Roles – James Lehman, DC, MBA, FACO 14
ColumnsChairman’s Message
Addressing and Improving Medicare Error Rates 1
Integrative Care
Bone Morphology and Modic Classifi cations 22
DepartmentsACA: Your Advocate 4
Chiropractic Added to Joint Commission Standard 8
JA CA Pages: Evidence in Action What should I do after my child has had a concussion? 28
Students and Education 35
ACA: Your Partner in Practice 36
In This Issue
Vol. 11, No. 1 | January/February 2015
ACA News © 2015 American Chiropractic Association. All rights reserved.
ACA News is indexed in the Cumulative Index to Nursing
and Allied Health Literature (CINAHL).
ACA NEWS:James G. Potter Chief Executive Offi cerAnnette Bernat Communications Vice PresidentLori Burkhart, JD Director of PublicationsAmanda Donohue Communications Coordinator
Graphic design: Lynn Riley Design, Inc.
ACA PUBLICATIONS BOARDDana Lawrence, DC, MMedEd, MA, chairman
Reed Phillips, DC, PhD, DACBR, ACA News executive editor
Cheryl Hawk, DC, PhD
Steven R. Conway, DC, Esq.
Thomas Hyde, DC, DACBSP
William J. Lauretti, DC
George McClelland, DC
Stephen Perle, DC, MS
Daniel Redwood, DC
Lawrence H. Wyatt, DC, DACBR, FICC
Michael Jacklitch, DC
Michael Simone, DC (board liaison)
EDITORIAL POLICYManuscripts published in ACA News are screened by the ACA Publications Editorial Board. However, neither the ACA nor its contributors, offi cers, or personnel investigate, endorse, or approve any statements of fact or opinion, which are solely the responsibility of the authors and sources of information. They are published on the authority of the writer(s) over whose name they appear and are not to be regarded as expressing the views of the ACA. Articles accepted for publication are subject to editing.
ADVERTISING INQUIRIES For rates on display ads, classifi eds; or to request media kits, contact Kelly Miller, M. J. Mrvica Associates, Inc., at [email protected] or (856) 768-9360. (Media kit available upon request.)
ADVERTISING POLICYWhile advertisements that appear in ACA News are subject to ACA advertising policy/guidelines, acceptance/publication of an advertisement does not imply endorsement or approval of the company, product, or services by the ACA or ACA News. Readers should use due diligence and/or consult with their respective State Board of Chiropractic Examiners for further information on advertised products/services.
THE PUBLISHERThe American Chiropractic Association (ACA) is dedicated to preserving, protecting, improving and promoting the chiroprac-tic profession and the services of doctors of chiropractic for the benefi t of the patients they serve. ACA provides leadership in health care and a positive vision for the chiropractic profession and its natural approach to health and wellness.
ACA BOARD OF GOVERNORSRichard Bruns, DC, Chairman (District 4)
Anthony Hamm, DC, ACA President
David Herd, DC, ACA Vice-President
Keith Overland, DC, Immediate Past President
Kelli K. Pearson, DC, (District 1)
James L. Rehberger, DC, (District 2)
Ray Tuck, DC, (District 3)
Craig Newman, DC, (District 5)
Michael Simone, DC, (District 6)
Joseph Morelli, DC, (District 7)
Karen Konarski-Hart, DC, President, Council of Delegates
Leo Bronston, DC, Vice-President, Council of Delegates
REPRINTSFor reprint permission, e-mail [email protected].
ACA News (ISSN 0744-9984) is published monthly (except February and July) by the American Chiropractic Association (ACA), 1701 Clarendon Blvd., Suite 200, Arlington, VA 22209. It is designed to pro-vide information about the chiropractic profession and ACA initiatives.
Address editorial inquiries to ACA News, 1701 Clarendon Blvd., Suite 200, Arlington, VA 22209. Phone: (703) 276-8800; Fax: (703) 243-2593; E-mail: [email protected].
ACA News subscription rate for members is $75, which is included in the annual dues. Periodicals postage paid at Arlington, VA, and at additional mailing offi ces. POSTMASTER note: Send address changes to ACA News c/o ACA, 1701 Clarendon Blvd., Suite 200,Arlington, VA 22209 or [email protected].
Atherosclerosis, Subluxation and Medicare All DCs are required to document the same way 16
Cover Story
30
28
32

ACA Your ADVOCATE
ACA Annual Meeting NoticeThere will be an annual meeting of the ACA House of Delegates on Friday,
Feb. 27 and Saturday, Feb. 28, 2015 at the Hyatt Regency Washington in D.C.
Proposed amendments to the ACA bylaws must be submitted to the ACA
Corporate Secretary at least sixty (60) days prior to the meeting. ACA bylaws
in odd numbered calendar years may be amended by a two-thirds (2/3) vote
of the House of Delegates, only after the proposed amendment is designated
as “emergency” by a majority of the House of Delegates (Article XII, Section A).
Deadline for receipt of proposed amendments to bylaws is Dec. 29, 2014.
Proposed resolutions must be sent to the ACA Corporate Secretary at least forty-
fi ve (45) days prior to the meeting (ACA Standing Rules, Article 9, Section C(7)(a)
(iv)). Deadline for receipt of proposed resolutions is Jan. 13, 2015.
All offi cers of the ACA, the board of governors, the executive offi cers,
department heads, ACA specialty councils and ACA committee chairmen must
fi le written reports of the year’s activities. The reports must be submitted to
the ACA corporate secretary at least forty-fi ve (45) days prior to the opening of
the annual meeting. (Article VIII, Section C(2)). Deadline for receipt of reports
is Jan. 13, 2015.
Please email all proposed resolutions in Word format to the corporate
secretary at [email protected]. For a bylaw or resolution
template, please email Janet Ridgely at [email protected].
ACA ANNUAL AWARDSSubmit Nominations for ACA Chiropractor, Humanitarian,
Delegate, Alternate Delegate, Flynn-Lynch, Academic and
Research of the Year Awards.
The following awards will be presented at the ACA 2015 annual House of
Delegates meeting:
Chiropractor of the Year
Humanitarian of the Year
Delegate of the Year
Alternate Delegate of the Year
Flynn-Lynch Memorial Award
George B. McClelland - Researcher of the Year
Academic of the Year
Nominations—which must include the name of the nominee, a brief essay on
why he or she should be considered for the specifi c award and the nominee’s
CV— must be sent to the ACA secretary at least forty-fi ve (45) days prior to the
annual business meeting or by Jan. 13, 2015. All nominations should be sent to
the ACA Corporate Secretary at [email protected].
James G. Potter
ACA Corporate Secretary
JANUARY/FEBRUARY 20156
SCOTT HALDEMAN, DC, MD, PHD, a respected author
and expert in evidence-based medicine whose
work has helped to advance the understand-
ing and treatment of spinal disorders, will
give the keynote address during the inaugu-
ral McAndrews Leadership Lecture at ACA’s
National Chiropractic Leadership Conference
(NCLC), Feb. 25-28, 2015, in Washington, D.C.
NCLC is the premier national confer-
ence for doctors of chiropractic, chiroprac-
tic assistants and chiropractic doctoral
students. � e event prepares chiropractic’s
leaders — current and future — for success
by exposing them to professional briefi ngs,
cutting-edge educational programs and
opportunities to meet with elected offi cials.
Dr. Haldeman’s presentation will focus
on the historical challenges of chiropractic
clinical practice and how current movements such as evi-
dence-based practice and value-based payment models will
infl uence how and where doctors of chiropractic practice and
their role in the continuum of care.
“We are honored to welcome Dr. Scott Haldeman to NCLC
2015,” said ACA President Anthony W. Hamm, DC. “His work
provides invaluable insight into the future of health care
practice and how the chiropractic profession can continue to
adapt and thrive for the benefi t of our patients.”
Dr. Haldeman is well-known for his published works on
the management and economics of spinal disorders. He is an
authority on evidence-based medicine and guidelines devel-
opment. He served on the federal government’s AHCPR Clini-
cal Guidelines Committee on Acute Low Back Problems in
Adults and on the Bone and Joint Decade 2000 to 2010 Task
Force on Neck Pain and Its Associated Disorders. A graduate
of Palmer College of Chiropractic and the University of British
Columbia medical school, Dr. Haldeman also holds a PhD in
neurophysiology. He currently serves as an associate profes-
sor of neurology at the University of California at Irvine.
Dr. Scott Haldeman to Give Keynote
Address at NCLC
Scott Haldeman, DC
“ We are honored to welcome Dr. Scott Haldeman to
NCLC 2015. His work provides invaluable insight
into the future of health care practice and how the
chiropractic profession can continue to adapt and
thrive for the benefi t of our patients.”
— ACA President Anthony W. Hamm, DC

JANUARY/FEBRUARY 20158
ACA Your ADVOCATE
THE CHIROPRACTIC PROFESSION GOT OFF TO A
GREAT START in 2015 as the Joint Com-
mission revised its pain management
standard to include chiropractic ser-
vices. Clinical experts in pain man-
agement who provide input into the
commission’s standards affi rmed that
treatment strategies may consider both
pharmacologic and nonpharmacologic
approaches. Previously nonpharma-
cologic approaches were not included.
Services provided by doctors of chiro-
practic (who were recognized in 2009
as physicians by the commission) and
acupuncture are now included in the
standard of care for pain management,
effective January 2015.
� e new standard also advises orga-
nizations, when considering the use of
medications to treat pain, to weigh the
benefi ts to the patient, as well as the
potential risks of dependency, addic-
tion and abuse of opioids. � e change
allows the chiropractic profession
to help more patients who might not
previously have been informed by their
health care system or doctor of non-
drug approaches to pain management.
Cultural Shift� e news of this guideline change
reached ACA via Karen Erickson, DC,
FACC, who sits on the board of trustees
at New York College of Chiropractic.
She is an ACA media spokesperson and
owns a practice in New York City. Dr.
Erickson previously worked with the
two non-chiropractors responsible for
the guideline change.
Having chiropractic mentioned in
guidelines that apply to every hospi-
tal and most major outpatient centers
in the United States is of great conse-
quence, even though guidelines are not
a mandate. “What’s important is that it
changes the culture of health care,” Dr.
Erickson notes. “It’s like redrawing a
map; the new map’s contours now have
two categories for pain management
— there is the pharmacologic category
and the nonpharmacologic category,”
she says. In essence, a new paradigm
has been created, where providers will
become educated about nonpharmaco-
logic approaches to consider, including
chiropractic and acupuncture.
“It’s also signifi cant from a cultural
point of view that the commission uses
the words ‘chiropractic’ and ‘osteopa-
thy’ and didn’t use ‘manipulation,’” Dr.
Erickson points out. “It’s of cultural
signifi cance, because there has been a
tendency even in excellent chiroprac-
tic research literature to use the word
‘manipulation.’” She says using chiro-
practic “puts us on the map and cor-
rectly identifi es our profession.”
Hospital CredentialingDr. Erickson makes clear that this win
for chiropractic at the Joint Commis-
sion was accomplished by Arya Nielsen,
PhD, director of the Acupuncture Fel-
lowship for Inpatient Care, Mount Sinai
Beth Israel Department of Integra-
tive Medicine, with support from Ben
Kligler, vice chair of the department
of integrative medicine at Mount Sinai
Beth Israel.
Dr. Erickson’s role at the Beth Israel
Medical Center from 2001 to 2004,
tells a lot about the early history of
chiropractic and integrative health
care. She was the fi rst clinician hired
at the Continuum Center for Health
and Healing, part of the Beth Israel
Medical Center, in New York City
(since bought by Mount Sinai so its
name has changed), which is the
largest integrative health center in
the United States. Her practice at the
center was the largest.
When the executive director,
Woodson Merrell, MD, author of � e Detox Prescription and chairman of the
Department of Integrative Medicine
at Beth Israel Medical Center, invited
her to join the Continuum Center, Dr.
Erickson became the fi rst chiroprac-
tic physician credentialed at a major
teaching hospital in the United States.
At the time, there were no credentialing
guidelines for a DC.
� e Continuum Center is an outpa-
tient center located off the Beth Israel
campus, and it has department status
at the hospital. Beth Israel needed to
create credentialing guidelines for DCs.
Initially an outside consultant worked
with the credentialing committee and
Dr. Merrell to negotiate guidelines; Dr.
Erickson found them unacceptable.
� ese proposed guidelines said a DC
could practice at the Continuum Center,
but patients would be required to obtain
a letter from their MDs saying there
were no contraindications to chiroprac-
tic care. “I thought that was outrageous,
regressive, insulting and patronizing on
every level,” says Dr. Erickson. “In one
fell swoop, they had wiped out 30 years
of work done to gain parity by the chi-
ropractic profession.”
Dr. Erickson believes the chiroprac-
tic profession owes a debt of gratitude
to Dr. Merrell for what he did next. He
reconvened the committee and had her
negotiate the credentialing guidelines.
� e credentialing committee is made
up of every department head at the
hospital. � e re-negotiated guidelines
allow DCs to practice within their scope
in New York State. “Dr. Merrell truly
understands the importance of hav-
ing chiropractic physicians practicing
at a major teaching hospital like Beth
Israel,” Dr. Erickson says.
Great value came from her oppor-
tunity to teach during grand rounds
held every week within the center. “All
physicians collaborated. I learned a lot
about medicine and how MDs clinically
think about and treat conditions; I also
had the opportunity to educate medical
Chiropractic Added to Joint Commission
Standard on Pain Management By Lori A. Burkhart

All DCs are required to document the
same way
ATHEROSCLEROSISSUBLUXATION
MEDICARE
JANUARY/FEBRUARY 201516
On the surface, it might appear that there is not much in common among
atherosclerosis, subluxation and Medicare; however, the opposite is true.
By David Seaman, DC

17www.acatoday.org JANUARY/FEBRUARY 2015
therosclerosis originated in the early
1900s, which is the same period when doctors of
chiropractic (DCs) began to embrace the word
“subluxation.” It is important to note that the word
did not originate in the chiropractic profession.
Subluxation had been around since the late 1600s;
the chiropractic profession embraced the word
because it seemed to fi t the condition/dysfunction
being treated with the adjustment.
An examination of the history of atherosclero-
sis shows how our understanding of the disease
has changed since the early 1900s.
� e current understanding of athero-
sclerosis is now completely different.
� e name is the same, but its meaning
has changed since 1900. � is would
be a useful approach for us to apply
to subluxation.
Consider that atherosclerosis is far
less emotional than subluxation as a
topic. Also, there is no internal profes-
sional war within medicine regard-
ing the nature of atherosclerosis. For
example, medical doctors in one faction
do not accuse those in another faction
of being anti-medical because they do not believe in
atherosclerosis. Unfortunately, our chiropractic pro-
fession has such factions. In some circles, if one does
not believe in the traditional subluxation model, one
is castigated for being anti-chiropractic.
� e problem is that one faction embraces tra-
ditional subluxation, another faction denies all
things subluxation and a third tries to ignore the
fi ghting factions. In my opinion, all three factions
are missing an obvious fact. Medicare has opera-
tionally defi ned subluxation for us, which means
that all three factions need to change their mind-
sets and focus on Medicare. It does not matter
whether you are a believer, denier or ignorer of
subluxation: As a matter of federal law, specifi c
subluxation criteria and other important details
must be documented in the record based on spe-
cifi c history and examination fi ndings. And most
interesting, the nature of Medicare subluxation is
very different from what the believers, deniers and
ignorers think it is.
AtherosclerosisAtherosclerosis was originally thought to be a
buildup of plaque on the arterial wall resulting from
endothelial cell injury. � is view is still embraced
today to varying degrees, but began to change in the
late 1900s. � e evolution of the understanding of
atherosclerosis may be useful for chiropractic physi-
cians to apply to their understanding of subluxation.
Until about 1970, atherosclerosis was incorrectly
perceived as a type of lipid storage disease. Lipid and
other plaque components were thought to form on
the surface of the arterial wall. Libby states that “this
traditional concept viewed atherosclerosis as analo-
gous to the buildup of rust in a water pipe.1” � en
Russell Ross published several papers in the 1970s
that changed the perception that atherosclerosis was
a “vessel wall reaction to injury.2-5” Originally, it was
thought that endothelial cells were denuded during
the injury process, leading to plaque formation.
It was later discovered that atheromas devel-
oped beneath uninjured endothelial cells. So in
1986, Ross wrote an update in the New England Journal of Medicine (NEJM) that served to revive his
hypothesis.6 He stated that endothelial cells may
be injured but remain intact and that the atheroma
grows beneath them. Ideally, Ross should have
stated, “While I have embraced, promoted and
made my living on the reaction to injury hypothe-
sis, perhaps it is wrong.” However, that is tough for
humans to do. But Ross did so 13 years later.
In 1999, Ross wrote another article in NEJM, enti-
tled, “Atherosclerosis — an infl ammatory disease.” It
IT DOES NOT MATTER WHETHER YOU ARE A BELIEVER, DENIER
OR IGNORER OF SUBLUXATION: AS MATTER OF FEDERAL LAW,
SPECIFIC SUBLUXATION CRITERIA AND OTHER IMPORTANT
DETAILS MUST BE DOCUMENTED IN THE RECORD BASED ON
SPECIFIC HISTORY AND EXAMINATION FINDINGS.
Dr. Seaman is a professor of clinical sciences at the National University of Health Sciences in Pinellas Park, Fla. He has authored a book on clinical nutrition for pain and infl ammation and has written several chapters and articles on this topic. His website, defl ame.com, is devoted to this topic. Dr. Sea-man’s book The DeFlame Diet is soon to be released.
Cover Story

is important to note that despite this clear title, he
still clung a bit to the “reaction to injury” view:7
“Numerous pathophysiologic observations in
humans and animals led to the formulation of the
response-to-injury hypothesis of atherosclerosis,
which initially proposed that endothelial denu-
dation was the fi rst step in atherosclerosis. � e
most recent version of this hypothesis emphasizes
endothelial dysfunction rather than denudation.
Whichever process is at work, each characteris-
tic lesion of atherosclerosis represents a different
stage in a chronic infl ammatory process in the
artery; if unabated and excessive, this process will
result in an advanced, complicated lesion.”
hen he states, “whichever process is at
work,” in the context of endothelial
dysfunction or a denudation, we see
that he is still clinging to hope that a
denuding injury might be important. While Ross
did not completely give up his reaction-to-injury
model, he substantially changed his position over
a 25-to-30-year period. Chiropractic physicians
should consider making similar concessions
regarding subluxation.
Since 1999, it has been established that no
denuding injury is needed for atherosclerosis to
develop. It develops in areas of turbulence and is
known to be a chronic infl ammatory process that
does not heal.
Metabolic SyndromeWhat was just described is how scientifi c think-
ing and the scientifi c process have led to a more
accurate understanding about the nature of ath-
erosclerosis. � e related practice of medicine has
not been so scientifi c. � e current challenge for
medicine is to overcome the dogma surrounding
saturated fats and cholesterol, which have been
deemed to be the absolute causes of infl ammatory
atherosclerosis. For a recent critique written by an
interventional cardiologist that properly criticized
his profession, please read, “Saturated fat is not
the major issue,” which was published in the Brit-ish Medical Journal.8 In short, Malhotra explained
that saturated fat and cholesterol are not the cause
of heart disease; saturated fat is protective. � e
real issue is metabolic syndrome. And regarding
treatment, adopting the Mediterranean diet after
a heart attack is almost three times as powerful as
statin therapy in reducing mortality.8
Understanding how metabolic syndrome creates
heart disease does involve cholesterol, but not in
the way we are taught. We are told that LDL cho-
lesterol rises and HDL cholesterol lowers, and this
somehow damages arteries and leads to plaque.
� e dietary issue is the consumption of excess
foods made of sugar, fl our and trans fats. When
these chemicals hit the blood-stream, they cre-
ate low-grade infl ammation in many ways. It is
very well known that HDL is anti-infl ammatory;
however, what is not well known is that HDL trans-
forms into a radicalized and infl amed HDL. � e
consumption of refi ned carbohydrates and trans
fats over time is associated with the expression
of metabolic syndrome and the transformation of
HDL into a molecule that is no longer capable of
participating in proper cholesterol transport and
actually promotes atherosclerosis.
� e story for LDL cholesterol is similar. Normal
LDL is soft and buoyant; however, the consumption
of refi ned carbohydrates and trans fats increases
the total amount of LDL and converts it into a mol-
ecule that is small and dense (sd-LDL). � e contin-
ued consumption of pro-infl ammatory foods and
the development of metabolic syndrome further
transform sd-LDL into oxidized sd-LDL (ox-sd-
LDL), which is highly infl ammatory. � e immune
system behaves as if ox-sd-LDL is a foreign antigen
and wages an all-out attack that is initially silent
but will eventually lead to excess plaque formation
in the vessel that may result in a vascular event.
Oxidized LDL is not yet a commonly available
clinical laboratory test. � e only indication we have
that suggests that LDL is in the transformation pro-
cess is the identifi cation of elevated LDL.
When we see low HDL and elevated LDL, we need
to consider that the patient may have metabolic syn-
drome. � is is an important concern for DCs because
patients with metabolic syndrome are at greater risk
for developing the most common musculoskeletal
pains that have traditionally been perceived as being
solely mechanical in nature (e.g. BMI, weight gain,
ppm, met syn). Statins and red yeast rice are incor-
rectly believed to correct the dietary imbalance-
induced infl aming of LDL and HDL.
Lessons LearnedSo, what does the history of atherosclerosis teach
us? In my view, we can learn two important les-
sons. First, we should endeavor to absolutely
change our perceptions about the nature of a
health condition if the science supports such a
change – that is the nature of evidence-based
healthcare. Second, we should abandon treatments
if they are deemed to be ineffective. Medicine has
succeeded in the fi rst lesson, but has in many cases
failed miserably in the second. DCs, in my opin-
ion, have failed in the fi rst lesson; we have not
adequately advanced the science of subluxation
JANUARY/FEBRUARY 201518

19www.acatoday.org JANUARY/FEBRUARY 2015
in a professionally benefi cial fashion. However,
regarding the second lesson, we have succeeded
in delivering a primary treatment (the adjust-
ment) that has proven to be very benefi cial for
many forms of musculoskeletal pain and related
symptomatology.9,10
Step back for a moment and consider the sublux-
ation battle that continues to rage within chiroprac-
tic, and it seems that the profession has lost focus.
� e believers continue to call deniers anti-chiro-
practic, and the deniers scoff at subluxation because
it is unscientifi c and yet to be a proven clinical entity.
Each side is fi rmly entrenched in its positions, and it
does appear to be a situation that will not improve or
be resolved. I believe subluxation should be viewed
similarly to atherosclerosis, and thus, subluxation
should be reframed. � e believers, deniers and
ignorers of subluxation far outnumber people like
me who could be called reframers. But my percep-
tion, as well as the perceptions of believers, deniers
and ignorers is also irrelevant in the context of
Medicare. Subluxation does exist in a very specifi c
manner within federal law; this is true whether you
are a believer, denier, ignorer or reframer.
SubluxationTo understand the operational defi nition of
subluxation in Medicare, a mind-set change is
required. Whether one is a believer, denier, ignorer
or reframer, all DCs have to unlearn our precon-
ceptions and do what Medicare directs us to do. In
other words, Medicare subluxation is a new reality.
rom a mental health perspective, focusing on
Medicare would also be benefi cial because it
would avoid the negative outcomes associ-
ated with blaming others for having a
contrasting view of subluxation. � is would benefi t
current and future DCs in making them effective at
addressing subluxation in the context of Medicare.
Space does not permit a detailed analysis of the
perceptual shortcomings held by believers and
deniers, the groups that, in my opinion, create most
of our trouble. I also say with assurance that most
believers in subluxation view me as a denier, so I
will briefl y criticize some of the perceptions of the
deniers. In particular, deniers commonly say that
“Medicare only pays us to treat subluxation, and it
makes no sense that we have to pick a vertebra
that is subluxated in order to get paid.”
DocumentationFirst, the treatment of Medicare patients is not
about subluxation in the traditional sense.
Did you know that you never have to mention the
word subluxation in the patient record if you choose
not to? Most have no idea that this is the case, yet it is
clearly stated in the Medicare Benefi t Policy Manual11
(MBPM) and every region’s Local Coverage Determi-
nation (LCD). Alternative terms are allowed that refer
to musculoskeletal dysfunction, for the purpose of
contrasting it with a non-musculoskeletal generator
of back pain, such as an abdominal aortic aneurysm.
econd, the notion is foolish that it is prob-
lematic to be required to name a painful
spinal level to be adjusted. It might be less
problematic for the deniers if the word
subluxation was not associated with naming the
offending vertebral level, and this speaks to the
misperceptions held by subluxation deniers. It
states very clearly in the MBPM and every region’s
LCD that the vertebra to be adjusted must be
capable of generating the painful symptoms. In
other words, subluxation identifi cation for
Medicare is a pain-based approach. Imagine how
foolish and scary it would be for spine surgeons to
complain about having to identify in the record
the spinal level where surgery is to be performed.
In short, the MBPM and LCDs clearly describe
what is required for documenting the treatment of
a Medicare patient. You only need to read your LCD
since each region has minor differences, which do
not contradict the MBPM. To facilitate the process
of embracing the various requirements put before
us by Medicare, Dr. Albert Luce and I developed
a chart (See Documentation Requirements and
Procedures for Medicare Patients, Page 20) to
assist DCs. We fi rst published this in Dynamic Chiropractic.12 My recommendation is to compare
the fl ow-chart we created with your LCD.
Medicare RequirementsAfter reading the chart of documentation require-
ments, it should be obvious that most chiropractic
physicians harbor misconceptions about Medicare
documentation, especially if they have yet to read
the MBPM and LCD. Medicare has essentially done
to subluxation what science has done to athero-
sclerosis; Medicare has updated and created an
operational defi nition of subluxation.
In short, it makes no difference what a believer
believes, a denier denies, an ignorer ignores or a
reframer thinks he or she is reframing, when it
comes to Medicare, the requirements are exactly the same for all of us. And if we do not comply, the
potential penalties can be swift and painful no mat-
ter the subluxation camp in which one may reside.
Medicare documentation may be an area on which
we can focus and set our differences aside.
Cover Story

Management fl ow per Medicare but
applicable to all patients
Management/documentation components required
to be Medicare compliant
Procedure and action steps to ensure
Medicare compliance
1. Medicare patient enters offi ce complaining of low-back pain that extends into his buttocks. He cites various functional limitations (disabilities) due to his pain.
Must establish medical necessity for spinal manipulation. Is the benefi ciary experiencing a signifi cant neuromusculoskeletal health problem necessitating manual manipulation by the chiropractic physician?
Based on this presentation, the answer is yes, which permits us to proceed to the history.
2. History (#s 2-8 relate to the initial visit) • Symptoms cause the patient to seek treatment• Family history, if relevant• Past health history
- prior injuries/traumas- prior surgeries- prior hospitalizations- current medications
• Check for contraindications• Description of present illness/symptoms causing patient to seek treatment—these
symptoms must bear a direct causal relationship to the spine- mechanism of trauma- quality and character- onset, duration, intensity, frequency, location and referral/radiation- aggravating and relieving factors- prior interventions, treatments and medications
• Secondary complaints
The history demonstrates medical necessity only if the patient is functionally limited, which is almost always due to pain. The chance of a functional limitation without pain is exceedingly rare.
Chiropractors should acquire or develop a new patient/history form that addresses the history components required by Medicare.
Important to note is that Medicare’s history requirements are a basic guideline. A comprehensive history is required due to all the probable red fl ag and non-red fl ag disorders that need to be considered.
Proceed with examination only if history substantiates medical necessity.
3. Red fl ags
Red fl ags (RF) are signs and/or symptoms refl ective of a visceral disorder, or a serious or potentially life threatening disease.
In Medicare terminology, RF conditions refer to relative and absolute contraindications (RC & AC):
Relative Contraindications1. Articular hypermobility and circumstances where the stability of the joint is
uncertain2. Severe demineralization of bone3. Benign bone tumors of the spine4. Bleeding disorders and anticoagulant therapy5. Radiculopathy with progressive neurological signs
Absolute Contraindications1. Acute arthropathies characterized by acute infl ammation and ligamentous laxity
and anatomic subluxation or dislocation including acute rheumatoid arthritis and ankylosing spondylitis
2. Acute fractures and dislocations or healed fractures and dislocations with signs of instability
3. An unstable os odontoideum4. Malignancies that involve the vertebral column5. Infections of bones or joints of the vertebral column6. Signs and symptoms of myelopathy or cauda equina syndrome7. For cervical spinal manipulations, vertebrobasilar insuffi ciency syndrome8. A signifi cant major artery aneurysm near the proposed manipulation
Red fl ags (RC & AC) can be identifi ed in a new patient/history form and from an individual red fl ag form.
If absolute contraindication(s) are identifi ed, then consider immediate referral.
For relative contraindications, consider a referral and precautions to HVLA thrusts.
The patient record must indicate the presence or absence of contraindications.
Chiropractors should acquire or create history forms that include screening questions for these contraindications.
4. Physical examination Medicare clearly mandates that the physical exam must demonstrate a causal relationship between the spine and the patient’s presenting complaint, which demonstrates medical necessity for spinal manipulation.
In addition, the manipulation must have a direct benefi cial therapeutic relationship to the patient’s condition. The manipulative service must provide reasonable expectation of recovery or improvement of function.
The physical examination leads to the generation of three important documentation requirements: (1) the selection of the vertebral level that is capable of generating the painful symptoms, (2) PART and (3) an appropriate ICD-9 code, all of which establish medical necessity for spinal manipulation.
5. PART The acronym PART has been used to describe the examination components indicating that a patient is suff ering from a spinal condition amenable to manipulation. At least 2 of the 4 PART criteria must be met, with at least one of them being the “A” or “R” component.
What about radiographs? They are not required to satisfy Medicare documentation requirements.
When should radiographs be used? For pathological diagnosis purposes.
The designation of PART in the record demonstrates to Medicare that the stated spinal level of dysfunction, as per the listed regional 739 code, has been examined/identifi ed and correlated to the secondary ICD-9 code.
The following quote from the 2009 OIG report demonstrates that we have not met the above documentation expectations.
From page 11 of the 2009 OIG Report (3): “The records would indicate a problem in one area of the spine which was examined, but indicated treatment to three to four areas of the spine and charged according to procedure without correlation to diagnosis.”
We suggest using/developing examination forms that lead to appropriate documentation of the correlation between PART and the 739 and secondary ICD-9 codes.
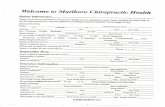
Documentation Requirements and Procedures for Medicare Patients
JANUARY/FEBRUARY 201520

21www.acatoday.org JANUARY/FEBRUARY 2015
Management flow per Medicare but
applicable to all patients
Management/documentation components required
to be Medicare compliant
Procedure and action steps to ensure
Medicare compliance
6. Generation of a diagnosis and related ICD-9 code
With the exception of regular Medicare in Florida, Puerto Rico and the U.S. Virgin Islands, the primary diagnosis for Box 21 of the 1500 billing form will be the 739 code series; one 739 code for each spinal region billed. Each primary 739 code should be followed by a secondary diagnosis, which should reflect the correlated significant neuromusculoskeletal condition that is painful and limiting a patient’s function.
In Florida, regular Medicare* billed to First CoastServices Options, the 739 code series is not billed as a diagnosis code, but all other examination, treatment, and documentation requirements are identical.
*Railroad Medicare and Medicare Advantage require 739 series on the bill.
A thorough history to include pain diagrams that is followed by an appropriate exam can help to identify the most likely pain generator, which leads to (1) the selection of the offending vertebral level and (2) the generation of an appropriate secondary diagnosis code. Chiropractors can accomplish this by developing forms that utilize appropriate spinal examination criteria:
1. Pain drawings2. Souza’s spinal examination chapters (14)3. Diagnosis-Based Clinical Decision Rule (15-19)4. Laslett’s criteria for SIJ pain (20)5. Laslett’s criteria for lumbar Z-joint pain (20)6. Wainer’s criteria for cervical radiculopathy (20)7. History predictors for lumbar stenosis (20)8. Clinical Prediction Rules for spinal manipulation (20)9. Prediction rule for spinal stability (20)
7. Treatment plan A comment from OIG Report-2009, page 17:“ In my (medical reviewer) 29 years of practice, I rarely saw documentation of a plan which included frequency, duration, goals and objective measures…they apparently have not been incorporated into the profession.”
Medicare requires the following components in the treatment plan:1. Recommended level of care (duration and frequency of visits);2. Specific treatment goals*; and3. Objective measures to evaluate treatment effectiveness.
*For long-term goals write out what the predicted maximum improvement will be for the patient. This will help you identify when the AT modifier is no longer supported, and it must be changed to GA for maintenance care.
The treatment plan must be outlined in the patient’s medical record. This will vary on a case-by-case basis.
We suggest using outcome assessment instruments such as the Quad VAS, Oswestry Disability Index, Bournemouth Neck and Back, Pain Disability Questionnaire (PDQ), etc.
It is advisable to label the patient’s spinal condition as “acute” or “chronic” in accordance with the Medicare Benefit Policy Manual (2), Chapter 15, and Section 240.1.5. This label relates to the required goals (treatment expectations), treatment frequency, duration and the prognosis for recovery or improvement.
8. Prognosis According to Medicare (2): “The chiropractor should be afforded the opportunity to effect improvement or arrest or retard deterioration in such condition within a reasonable and generally predictable period of time.” Medicare Benefit Policy Manual, Chapter 15, and Section 240.1.5.
A reasonable prognosis can be generated based on the acute/chronic nature of the condition and based on any perpetuating factors, such as biopsychosocial issues, lifestyle, nutrition, behavior, health status, etc. Factors that influence prognosis should be included in your forms/patient record – they need to be documented.
9. Subsequent visits The following is required by Medicare:1. Date2. History
• review of chief complaint• changes since last visit• system review, if relevant
3. Physical Exam• examination of area of spine involved in diagnosis• assessment of change in patient condition since last visit
4. Evaluation of treatment effectiveness5. Description of treatment given on this visit6. Any changes in treatment plan
We suggest developing a form that allows for consistent documentation of each Medicare patient visit so that each required component is satisfied. A SOAP note to include PART is most appropriate.
For exacerbations or new complaints, a new initial sequence is warranted, which requires Box 14 to be updated.
By Drs. David Seaman and Albert Luce (2009-2011)
References
1. Libby P. Inflammation and cardiovascu-
lar disease mechanisms. Am J Clin Nutr.
2006;83(suppl):456S-60S.
2. Ross R. Atherosclerosis: the role of endothelial
injury, smooth muscle proliferation and
platelet factors. Triangle 1976;15:45-51.
3. Ross R, Glomset JA. �e pathogenesis of
atherosclerosis (first of two parts). N Engl J Med 1976;295(7):369-77.
4. Ross R, Glomset JA. �e pathogenesis of
atherosclerosis (second of two parts). N Engl J Med 1976 Aug 19;295(8):420-5.
5. Ross R, Glomset J, Harker L. Response to
injury and atherosclerosis. Am J Pathol 1977;86(3):675-84.
6. Ross R. �e pathogenesis of atherosclerosis—
an update. N Engl J Med 1986;314(8):488-500.
7. Ross R. Atherosclerosis—an inflammatory
disease. N Engl J Med 1999;340(2):115-26.
8. Malhorta A. Saturated fat is not the major
issue: let’s bust the myth of its role in heart
disease. Brit Med J 2013;347:f6340 doi: 10.1136/
bmj.f6340 (Published 22 Oct 2013).
9. Nansel D, Szlazak M. Somatic dysfunction and
the phenomenon of visceral disease simula-
tion: a probable explanation for the apparent
effectiveness of somatic therapy in patients
presumed to be suffering from true visceral
disease. J Manip Physiol �er 1995;18:379-97.
10. Seaman DR, Winterstein JF. Dysafferentation,
a novel term to describe the neuropathophysi-
ological effects of joint complex dysfunction: A
look at likely mechanisms of symptom genera-
tion. J Manip Physiol �er 1998;21(4):267-80.
11. Center for Medicare Services. Medicare
Benefit Policy Manual. Chapter 15 – Covered
Medical and Other Health Services. www.cms.gov/manuals/Downloads/bp102c15.pdf.
12. Seaman DR, Luce AJ, Hamm A. �e Medicare
hurdle that continues to block our profes-
sional progress. Dynamic Chiro 2012;30(8)
www.dynamicchiropractic.com/mpacms/dc/article.php?id=55844.
13. Office of Inspector General. Inappropriate
Medicare payments for chiropractic services.
Dept Health Human Services. May 2009 http://oig.hhs.gov/oei/reports/oei-07-07-00390.pdf
14. Souza TA. Differential diagnosis and manage-
ment for the chiropractor: protocols and algo-
rithms. 4th ed. Boston: Jones and Bartlett; 2009.
15. Murphy DR. A clinical model for the diagnosis
and management of patients with cervical
spine syndromes. Australas Chiropr Osteopa-thy 2004;12(2):57-71.
16. Murphy DR, Hurwitz EL. A theoretical model
for the development of a diagnosis-based
clinical decision rule for the management of
patients with spinal pain. BMC Musculoskelet Disord 2007;8:75.
17. Murphy DR, Hurwitz EL, Nelson CF. A
diagnosis-based clinical decision rule for
spinal pain part 2: review of the literature.
Chiropr Osteopat 2008;16:7.
18. Murphy DR, Hurwitz EL, McGovern EE.
Outcome of pregnancy-related lumbopelvic
pain treated according to a diagnosis-based
decision rule: a prospective observational
cohort study. J Manipulative Physiol �er
2009;32(8):616-24.
19. Murphy DR, Hurwitz EL, McGovern EE. A
nonsurgical approach to the management
of patients with lumbar radiculopathy
secondary to herniated disk: a prospective
observational cohort study with follow-up. J Manipulative Physiol �er 2009;32(9):723-33.
20. Cleland JA. Koppenhaver S. Netter’s orthope-
dic clinical examination: an evidence-based
approach. 2nd ed. Philadelphia: Saunders Elsevier 2011.