Inpatient Sepsis Toolkit - Ministry of Health · Sepsis is a medical emergency just like a heart...
Transcript of Inpatient Sepsis Toolkit - Ministry of Health · Sepsis is a medical emergency just like a heart...

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 1
INPATIENT PROGRAM
IMPLEMENTATION GUIDE
May 2014
SEPSIS TOOLKIT

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 2

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 3
TABLE OF CONTENTS
FOREWORD ....................................................................................................................................................................... 4
PART A - IMPLEMENTATION GUIDE ................................................................................................................................ 5
INTRODUCTION ................................................................................................................................................................ 6
BACKGROUND .................................................................................................................................................................. 7
SEPSIS KILLS PROGRAM ................................................................................................................................................. 8
SEPSIS AND THE DETERIORATING PATIENT.................................................................................................................. 9
FIVE ELEMENTS OF THE PROGRAM ............................................................................................................................. 10
GOVERNANCE................................................................................................................................................................. 11
Key roles in the local health district ...................................................................................................................................... 11
Getting started ...................................................................................................................................................................... 13
CERS AND SEPSIS TOOLS ............................................................................................................................................. 17
Sepsis pathways ................................................................................................................................................................... 17
Antibiotic guidelines .............................................................................................................................................................. 19
Sepsis 48 hour management plan........................................................................................................................................ 20
EDUCATION ..................................................................................................................................................................... 21
EVALUATION.................................................................................................................................................................... 22
REFERENCES .................................................................................................................................................................. 24
PART B - TOOLS & RESOURCES ................................................................................................................................... 25
ACKNOWLEDGEMENTS: Thank you to: Clinical Excellence Commission Sepsis Advisory Group Sepsis Management Group and Paediatric Sepsis Reference Group, Clinical Excellence Commission Between the Flags team, Liverpool Hospital and South Western Sydney LHD, Westmead Hospital and Western Sydney LHD, Griffith Base Hospital and Murrumbidgee LHD, Orange Health Service and Western NSW LHD and Peter McCallum Cancer Centre, Melbourne.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 4
FOREWORD Sepsis is a world-wide public health issue and claims thousands of lives each year. The incidence of sepsis is escalating as the population ages, and its treatment is becoming an increasingly significant burden on national health care expenditure. Sepsis is a medical emergency just like a heart attack or stroke. It arises when the body’s response to infection causes a generalised inflammatory response that can lead to shock, multiple organ failure and death. Early recognition and prompt treatment is essential to improve survival. The Clinical Excellence Commission (CEC) launched the SEPSIS KILLS program in May 2011 in emergency departments and the program has been extended to the inpatient wards. The program seeks to engage and support our clinical staff in hospitals across New South Wales to make sustainable improvement in the recognition and management of severe infection and sepsis. Patients with sepsis are high risk and may deteriorate rapidly. The program is closely aligned with the Between the Flags system which facilitates early recognition, response and management of the deteriorating patient. Sepsis awareness, early identification, resuscitation and referral to specialist care will ensure that all patients with sepsis receive timely and appropriate care. I encourage each of your facilities, and all of your staff (clinical and managerial) to implement the program. Clifford F Hughes, AO CLINICAL PROFESSOR CEO, CLINICAL EXCELLENCE COMMISSION

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 5
PART A - IMPLEMENTATION GUIDE

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 6
INTRODUCTION Welcome to the Inpatient SEPSIS KILLS program implementation toolkit. It is a practical guide for managers and clinicians to improve the recognition and management of sepsis in adult and paediatric patients in inpatient wards of medium and large hospitals in NSW. It has been developed from the collective knowledge and experience of clinicians and CEC staff who have been involved in the SEPSIS KILLS program development and implementation. The toolkit provides:
• Tools to plan, implement and evaluate a sepsis improvement project in hospital wards • Education resources • Communication resources
The toolkit is not exhaustive. Over time, new tools and resources will be developed in response to clinician feedback and program needs. These resources will be made available on the SEPSIS KILLS program page of the CEC website www.cec.health.nsw.gov.au/programs/sepsis.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 7
BACKGROUND Sepsis is one of the leading causes of death in hospital patients worldwide. It causes more deaths than prostate cancer, breast cancer and HIV/AIDS combined1. There are approximately 15,000 cases of severe sepsis and septic shock in Australian and New Zealand intensive care units per year2. Sepsis is a life-threatening condition that arises when the body’s response to infection injures its own tissues and organs3. Sepsis can present in any patient, in any clinical setting and is a medical emergency. Despite this, awareness of sepsis and the need for prompt and targeted treatment is limited. Appropriate recognition and timely management of patients with severe infection and sepsis is a significant problem in NSW hospitals and in health care facilities around the world. Delayed treatment is associated with high mortality rates, significant morbidity and high costs to the health care system. In paediatric patients, sepsis is one of the leading causes of death, with mortality rates as high as 10 per cent. Many of these deaths are preventable4. The mortality rate for adult patients with septic shock is around 25 per cent5. It has been shown to increase by 7.6 per cent for every hour of delay, after the onset of hypotension, in starting antibiotic therapy6. In the complex hospital ward environment, there are frequently long delays between medical review and antibiotic prescription, particularly when decision making is by junior medical officers7. The CEC Clinical Focus Report on Recognition and Management of Sepsis8 found deficits in a range of clinical settings in NSW health care facilities in 2009. The lack of timely recognition and appropriate management was further demonstrated in the findings from the 2011 CEC Quality Systems Assessment9. The CEC SEPSIS KILLS Economic Analysis10 estimates that if the status quo is maintained over the next ten years, sepsis-related conditions in the NSW health system will constitute $3.7 billion, 1.3 million bed days, 701,000 cost weighted separations and an unknown number of potentially avoidable deaths.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 8
SEPSIS KILLS PROGRAM The SEPSIS KILLS program is a quality improvement initiative that has been developed from international evidence-based practice11,12,13. The goal is to reduce preventable harm to patients with sepsis through early recognition and prompt management. It provides significant benefits at both the clinical and system levels, including:
• Enhanced clinician skills in sepsis recognition and management • More timely, standardised and effective detection and management of sepsis • Reduced mortality, morbidity and bed-stays from sepsis-related conditions • Improved quality and safety of care and a better and safer patient experience.
The program started in May 2011 and has been implemented in 180 NSW public hospital emergency departments. Since it was launched, time to antibiotic administration has greatly improved. Median time to antibiotic administration in emergency departments has been reduced from more than four hours, to consistently less than sixty minutes in 2013 and 2014.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 9
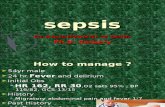
SEPSIS AND THE DETERIORATING PATIENT The inpatient phase of the SEPSIS KILLS program is focused on improving the recognition and management of sepsis in adults and children in the inpatient wards of public hospitals in NSW. It directly links with the Between the Flags system (BTF), the NSW Health Policy: Recognition and Management of Patients who are Clinically Deteriorating (PD2013_049) and the Australian Commission on Safety and Quality in Health Care national accreditation standards14. Deteriorating patients with sepsis can be escalated via the NSW Standard Observation Charts and the Clinical Emergency Response System (CERS). By undertaking routine clinical observations, nurses and doctors play a vital role in identifying and escalating sepsis. The clinician is encouraged to think why the patient is deteriorating and ask “could this be sepsis?”. The ‘track and trigger’ design of the NSW Health Standard Observation Charts includes standard calling criteria for Clinical Review and Rapid Response which are pivotal in supporting clinical staff to recognise deterioration. All NSW public hospitals and acute care facilities have an established CERS so that deteriorating patients receive an appropriate clinical response. CERS are developed and tailored to the health service/facility's needs and resources. The main components of this system of escalation include:
• A Clinical Review process that has the capacity to respond within 30 minutes to a breach in Yellow Zone observations or additional criteria
• A Rapid Response process that is immediately available in response to a breach in the Red Zone observations or additional criteria
• Necessary equipment is available to perform advanced resuscitation • An escalation process for transferring patients that require a higher-order of care to a facility that can provide
it. Preliminary NSW sepsis data suggests that 30 per cent of adults who require a Rapid Response are septic. This is replicated in national and international literature15, with sepsis being a leading cause for clinical deterioration, accounting for one in three calls for a Rapid Response team. The tools provided by the BTF system and SEPSIS KILLS program give clinicians objective criteria, backed by policy for escalation, which empowers them to call for senior clinical help when they judge a patient to be deteriorating or are concerned about the patient’s condition. This is illustrated in the following diagram:
Recognition Is my patient ‘Between the Flags’? (BTF) Response If not, what should I do? (Yellow & Red Zone response) Root Cause Why is my patient deteriorating? (SEPSIS KILLS) Response How should I treat him or her? (SEPSIS KILLS)

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 10
FIVE ELEMENTS OF THE PROGRAM The five elements of the SEPSIS KILLS program align with the BTF system and are designed to establish a sustainable Statewide initiative which will deliver improved systems for recognition and response to patients with sepsis. The five inter-dependent elements of the program are:
1. Governance: establishment of guidelines for an administrative structure to oversee the implementation and sustainability of the system in the acute hospitals in NSW.
2. Clinical Emergency Response System (CERS): process for escalation of concern and response to the deteriorating patient with sepsis in every facility.
3. Sepsis Tools: to guide clinical decision making in parallel with the local CERS to facilitate the following:
RECOGNISE risk factors, signs and symptoms of sepsis RESUSCITATE with rapid intravenous fluids and antibiotics within the first hour of recognition of sepsis REFER to senior clinicians and specialty teams, including retrieval as required
4. Education: to ensure appropriate skills and knowledge for the recognition and management of the patient
with sepsis.
5. Evaluation: standard performance indicators to be collected and used to inform users of the system and to guide sepsis recognition and management improvement.
The following sections of the Sepsis Toolkit provide guidelines, tools and resources to support implementation of the five elements in your health care facility.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 11
GOVERNANCE The success and long-term sustainability of the SEPSIS KILLS program is dependent on appropriate governance structures and processes at all levels of the health care facility. Leadership by both management and clinicians will enable a top-down, bottom-up approach to drive and sustain improved outcomes for patients with sepsis. The governance of the program should be integrated with existing structures for the recognition and management of patients who are clinically deteriorating.
Key roles in the local health district (LHD) Each LHD and health care facility will need to identify and appoint key position holders with operational responsibility for implementation of the program. These position holders will work closely with appropriate advisory committees, program teams and expert advisors. Suggested roles and responsibilities for LHD and facility personnel are detailed below.
LHD executive sponsor • Ensure key personnel have been identified and appointed • Establish an effective LHD governance structure which integrates with the deteriorating patient strategy • Implement the five elements of the program in all medium and large LHD facilities • Assist and support the LHD sepsis leads to coordinate the LHD implementation strategy.
LHD sepsis lead
• Coordinate the implementation of the program in all medium and large LHD facilities in collaboration with the LHD and facility executive sponsors
• Ensure stakeholders at LHD and facility levels have been consulted in the development of the implementation strategy
• Work with the facility executive sponsors to engage senior clinicians and department heads • Liaise with the CEC on LHD progress and strategies developed to overcome barriers
Facility executive sponsor
• Appoint a facility sepsis program lead • Establish an implementation team • Establish an effective governance structure for the facility which integrates with the deteriorating patient
strategy • Identify and allocate resources to support implementation • Ensure that all key personnel have been identified and appointed including medical and nursing
ward/unit clinical leads/champions • Assist and support ward/unit clinical leads/champions by endorsing the program as a vital initiative
which is part of the deteriorating patient strategy • Facilitate senior medical staff discussion on supervision and escalation processes for junior medical
staff • Provide reports to the LHD sepsis lead and executive sponsor on implementation progress and results
Facility sepsis program lead
• Assist and support ward/unit clinical leads/champions to engage senior clinicians and implement the sepsis program in their local areas
• Facilitate senior medical staff discussion on supervision and escalation processes for junior medical staff
• Coordinate facility sepsis communication and education strategies

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 12
• Ensure materials are available and promoted • Provide regular feedback and progress reports to the facility Executive Sponsor
Facility clinical leads/champions
• Participate in the development of local systems for the program • Work with the facility sepsis program lead and executive sponsor to engage senior clinicians and
implement the program in wards/units • Coordinate ward/unit based communication and education • Support clinicians as they adapt to the altered clinical environment • Provide feedback and progress reports to the facility sepsis program lead

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 13
Getting started Each health care facility will need to develop a strategy to effectively implement the program in all wards. This section of the toolkit provides information on a ten-step implementation process which can be adapted to suit local environments. STEP 1: Establish a case for change Making a change to existing practice can be challenging and requires time, effort and resources. A good case for change will help to convince others that it is necessary to change the current practices i.e. it provides compelling evidence of why there is a problem, what will improve and the expected outcome. A short written document and /or presentation can be used to gain peoples’ interest. Include evidence that timely sepsis recognition and management is an international problem and sepsis is a medical emergency. Local data showing how sepsis is currently managed is a powerful tool to convince clinicians why the change is necessary. Gaining leverage from the outcomes of the emergency department sepsis project will also be influential. Benefits of the change need to be clearly indicated along with linkages to other quality and safety initiatives such as national accreditation requirements. The benefits may vary according to the target group e.g. clinical or managerial.
Resources Program summary Memo template Sepsis program general presentation
STEP 2: Establish governance arrangements and a program team Governance is a critical foundational element of the program. Defining clear roles and responsibilities for governance is a high priority and need to be established early. The program should be linked with the facility quality and safety plan, deteriorating patient strategy and relevant national accreditation standards. The following roles need to be identified at both LHD and facility levels:
• Executive sponsor • Program lead • Program team to oversee the improvement process
The program team will need multidisciplinary senior managers and clinicians to provide organisational and ward/unit leadership and support. A responsible committee will need to be identified with agreement on communication and reporting channels between the program team, responsible committee and the LHD sepsis lead/clinical governance unit. An initial task for the team is to develop an overall implementation plan. The CEC has developed an implementation plan template for NSW facilities to promote consistency and to help identify key elements required. The plan will guide the team and ensure relevant activities are managed from the outset including risk assessment, communication and evaluation strategies. The program plan will be endorsed by the facility executive sponsor and the LHD sepsis lead.
Resources Facility implementation plan Facility implementation checklist

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 14
STEP 3: Recruit respected and influential leaders and champions Senior leadership is crucial to the success of the program. It is recommended that each ward/unit has medical and nursing leads/champions. These people need to be senior clinicians who are willing and able to drive organisational change. The sepsis leads from the emergency department will be able to provide helpful insights to the leadership role as well as ideas for the program implementation strategy. Some of the medical and nursing leads may also be program team members.
STEP 4: Identify sepsis management barriers and enablers A review of the current process for managing sepsis should be undertaken. If resources are available, it is useful to undertake a retrospective audit of sepsis cases to provide insights into current practice. A brainstorming session to identify the causes of inadequate or delayed recognition and treatment of sepsis will be helpful to better understand sepsis management barriers and enablers. Areas to consider are people, patients, processes, knowledge, skills, equipment, communication, escalation and supervision A list of common causes of delay in recognition and treatment of sepsis is provided in Section B: Tools and Resources. The list was derived from CEC pilot study feedback in several large hospitals. It should be noted however, that the brainstorming activity is far more effective if it is undertaken by the facility program team and by wards/units to identify the local issues. When undertaking the brainstorming process, it is important to involve representatives from all levels/disciplines to ensure that relevant issues are identified. The program team or ward/unit can then develop an action plan to address the main barriers.
Resources Common causes of delay in recognising and treating sepsis in the wards Implementation action plan
STEP 5: Adapt the sepsis tools to align with the clinical emergency response system (CERS) and other local processes A range of tools have been developed to support sepsis recognition and management. The CERS and Sepsis Tools section in the Toolkit provides details on each of the tools. It is important to ensure that the sepsis pathway is aligned with the local CERS. This may include changing terminology if hybrid systems are in place. Discussions with senior medical staff should be facilitated to establish processes for escalation of sepsis to the Attending Medical Officer (AMO), infectious diseases experts and intensive care. Suggested triggers for escalation to the AMO and infectious diseases are provided in the Toolkit Section B to assist each department or facility to initiate discussions and establish local processes. The CEC sepsis antibiotic guideline can be reviewed by the facility and/or LHD drug committee and aligned with local drug and antimicrobial stewardship processes. Patients with sepsis are at a high risk of deterioration in the days following initial treatment. It is important that a high level of vigilance and monitoring is maintained. Local minimum monitoring requirements for ward patients with sepsis should be established and the CEC 48 hour sepsis management plan can be adapted for local use.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 15
Resources Adult and paediatric sepsis pathways Sepsis 48 hour management plan Adult inpatient sepsis intravenous antibiotic guideline ISBAR tool Escalation triggers for calling an AMO for patients with sepsis Frequently asked questions
STEP 6: Identify tools and resources to support sepsis management Other tools and resources may be required to support implementation of improved sepsis management. Sepsis trolleys or packs that hold the necessary equipment for managing a patient with sepsis have been found to be useful in both the emergency and ward settings. Sepsis trolleys also provide a clear message to ward staff that sepsis is an emergency and necessitates rapid intervention. Establishing processes for timely lactate testing is important to support identification and management of sepsis. High serum lactate levels are strongly associated with increased mortality. Accessing results for formal serum lactate levels may take considerable time in most hospitals. Point of care testing may be available through the intensive care unit or emergency department and could be considered as an alternative process to provide quick access to lactate results.
Resources Ward implementation checklist Sepsis trolley/pack content list
STEP 7: Develop an education strategy Training and education is important to initiate a clinical practice change and is also vital to help sustain and spread the change over time. An initial step is to identify the education tiers or groups and to document a plan to provide tailored education for specific professional and craft groups. The strategy will vary in each facility however it may be helpful to consider how the education was rolled out for the BTF system. At a minimum, there will need to be awareness training (key sepsis messages and orientation to the sepsis pathway) for all nursing and medical staff in direct contact with patients. More detailed training can be provided for the Rapid Responders and other key stakeholders who will be required to provide clinical decision support to wards and clinicians. Master classes for medical staff, nurse unit managers, educators, clinical nurse consultants and nurse managers could be adopted. Evaluation of the education strategy can be undertaken using the multiple choice questionnaire provided in Part 2: Tools and Resources or by using a locally developed pre and post education survey. Education can be incorporated into the BTF Tier Two education (DETECT training), as well as orientation programs for junior medical officers and new staff starting at the hospital.
Resources SEPSIS KILLS video SEPSIS KILLS general presentation SEPSIS KILLS clinical presentation: adults SEPSIS KILLS clinical presentation: paediatrics SEPSIS KILLS e-learning module SEPSIS KILLS multiple choice questions

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 16
STEP 8: Pilot the new sepsis process The program team will now be ready to implement a pilot study of the new sepsis process using short Plan, Do, Study, Act cycles. It is important to keep the pilot study a manageable size choosing one or two wards where there is strong clinical leadership and commitment to change. Groundwork will need to be done to prepare the staff in the pilot area with education and promotion activities. Collecting feedback from stakeholders frequently is important. It is recommended that an issues log is used to document concerns as they arise (particularly important out of hours) as well as having regular forums to discuss progress. Reviewing and revising the process during and after the pilot will help to identify unintended consequences and reinforce the importance of staff feedback and generation of solutions. Data collection to demonstrate improvement will need to be established at the outset of the pilot and should include quantitative data (time to IV fluid and antibiotic administration) as well as qualitative data (staff feedback).
Resources Sepsis issues log
STEP 9: Sustain and spread the process to other wards/units When the pilot study is complete, the process can be spread to other wards and units in the hospital in a phased approach. The pilot outcomes can be communicated using a variety of methods including meetings, newsletters and intranet posts to share the benefits gained and the lessons learnt. Organizational guidelines on sepsis management principles and procedures can be developed and embedded into structures and routines e.g. clinical handover, orientation programs, junior medical staff education programs and BTF Tier Two education (DETECT training). STEP 10: Measure, evaluate and improve Evaluation is a systematic process to determine if an improvement is being made. Developing an evaluation plan is important for both the short term and long term success of an improvement program. Evaluation can help to identify any unintended consequences as well as providing lessons for future improvement. It is suggested that consideration is given to using a range of evaluation methods. These could include medical record audit, observational audit, survey and focus groups. Displaying evaluation data and discussing the findings at ward meetings will help to drive improvement. Each health care facility and LHD will establish processes for reporting results to local committees and the LHD. Further details on sepsis measures and methodology can be found in the Evaluation section of the Toolkit.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 17
CERS AND SEPSIS TOOLS A range of tools and resources are available to assist clinicians to identify and treat sepsis, in accordance with national and international best practice. The tools have been developed in collaboration with clinical experts and other key stakeholders from tertiary, metropolitan and regional/rural facilities across NSW. The main three clinical tools are:
• Sepsis pathways • Antibiotic guidelines • Sepsis 48 hour management plan
The tools and resources are provided in Part B of the Toolkit and/or the sepsis page of the CEC website.
Sepsis pathways The sepsis pathways for adult and paediatric inpatients provide clear guidelines for sepsis recognition, notification, escalation and initial management. They are built around three key actions:
RECOGNISE risk factors, signs and symptoms of sepsis RESUSCITATE with rapid intravenous fluids and antibiotics within the first hour of recognition of sepsis REFER to senior clinicians and specialty teams including retrieval as required
The pathways are based on the following logic which directly links the pathways with the BTF system and the NSW Health Policy: Recognition and Management of Patients who are Clinically Deteriorating (PD2013_049). The left side of the flow diagram illustrates the process used from recognition to treatment of patients with sepsis. The right side of the flow diagram describes the tools, processes and steps currently used in the hospital inpatient wards. The following section provides information on the linkage of the logic (above) with the sepsis pathways.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 18
Recognition Recognition of sepsis risk factors, signs and symptoms may be facilitated via any of the following systems and relates to the recognition section of the sepsis pathway:
NSW Health Standard Observation Charts In line with NSW Health policy, observations must be recorded on a NSW Health Standard Observation Chart (SAGO, or age-specific SPOC). In the absence of a documented monitoring plan, frequency of observations should be completed as indicated by the patient’s condition. This should be no less than three times per day, at eight hourly intervals.
REACH (Recognise, Engage, Act, Call, Help is on its way) This is a patient and family activated Rapid Response program. REACH empowers patients and families to escalate care if they are concerned about the condition of the patient by first encouraging engagement with the treating clinicians at the bedside. Ward Rounds A patient may be identified as being at risk of or having sepsis during a ward round where medical, nursing and allied health staff comes together at the patient’s bedside to discuss the patient’s current clinical status and plan of care.
Escalation A Clinical Review or Rapid Response must be activated for the deteriorating patient in accordance with local CERS. Patients who are identified as septic at the time of a ward round or during a routine medical consultation require a Rapid Response call if the patient’s observations are in the Red Zone.
Could this be sepsis? Consideration should be given to whether sepsis or any other time critical conditions such as a new arrhythmia, hypovolaemia/haemorrhage, PE/DVT, pneumonia/atelectasis, an AMI, stroke or overdose / over-sedation could be the cause of the patient’s deterioration. Teachings advocated in the BTF Tier Two education (DETECT training) including A-G assessment apply when assessing patients with suspected sepsis.
Sepsis is a difficult clinical diagnosis that requires experience and a high index of suspicion for interpretation of history, signs and symptoms. Early senior clinician involvement is imperative to ensure that the required skills and knowledge are available to facilitate appropriate diagnosis and management. Suggested triggers for escalation to the AMO/infectious diseases physician are provided in the Toolkit Section B. The ISBAR framework can be used to structure the conversation to ensure completeness of information and standardize communication. Sepsis treatment, reassessment and referral The sepsis pathways provide clear resuscitation guidelines for patients with severe sepsis or septic shock sepsis using an A-G approach. The guideline is based on a bundle of care which should be delivered within one hour of recognition/diagnosis. The six components are:
1. Oxygen 2. Blood cultures 3. Serum lactate 4. Intravenous fluids 5. Antibiotics 6. Monitoring and reassessment

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 19
Reassessment of the patient is required to determine the effectiveness of treatment. Referral to a higher level of care such as an intensive care unit, specialist service or another facility may be required. The AMO should be informed that the patient has had a Clinical Review or Rapid Response call and commenced on the sepsis pathway. Clinicians who suspect a paediatric patient of having sepsis should follow a stepped approach for escalation Step 1 – facility (senior onsite medical officer), Step 2 – LHD (on-call paediatrician), Step 3 – State (NETS) as outlined in the NSW Health Policy: Recognition and Management of Patients who are Clinically Deteriorating (PD2013_049). Communicating that the patient has been treated for sepsis and is at risk of further deterioration is essential at handover between shifts and when transferring patients to another ward/unit or hospital. NOTE: The adult and paediatric sepsis pathways are not intended for patients at risk of febrile neutropenia. Patients with a recent haematological or oncology diagnosis should be managed using relevant local guidelines for febrile neutropenia.
Antibiotic guidelines Prompt administration of antibiotics and resuscitation fluids is vital for effective management of sepsis in combination with effective source control. The goal is to commence antibiotic therapy within the first hour of recognition and diagnosis of sepsis. Antibiotic therapy should not be delayed whilst waiting for investigations or results. The Inpatient Sepsis Intravenous Antibiotic Guideline aims to guide the prescription and timely administration of antibiotics for patients that have a diagnosis of sepsis and have been admitted to hospital for 48 hours or more. It is based on the recommendations in Therapeutic Guidelines: Antibiotic version 14, 201016 and is intended to provide an accessible resource which can be adapted to suit individual facility preferences in liaison with the antimicrobial stewardship team, local antimicrobial susceptibility patterns and senior clinicians.
Escalation to the Attending Medical Officer (AMO) for antibiotic advice A flow chart is provided in the antibiotic guideline to assist the treating doctor in determining (for each case of sepsis) if the Antibiotic Guideline can be used or if escalation to the AMO for further advice is required. Antibiotic prescribing for patients with sepsis due to hospital-acquired infections is complex because of: • Unfamiliarity with the dosing, efficacy, toxicity, and spectrum of activity of rarely used and/or newer
generation drugs e.g. meropenem, daptomycin, linezolid, tigecycline, colistin, amikacin, caspofungin • Local resistance patterns of multi-drug resistant bacteria e.g. MRSA, VRE, ESBLs, MBLs, other MDR-GNBs
and their association with different sources of infection • Propensity for drug-resistance due to time spent in hospital, overseas travel, certain procedures, and
previous antimicrobial therapy • Constraints such as renal and/or hepatic failure, drug allergy and potential interactions with other
medications • Difficulty in assessing positive or negative microbiology results when rationalising therapy at 48-72 hours
Escalation to the infectious diseases physician or clinical microbiologist In many cases, the AMO will feel comfortable prescribing antibiotics for such patients. It is anticipated however, that there will be times when the AMO recognises the triggers above as prompts for seeking immediate advice from a specialist Infectious Diseases Physician or Clinical Microbiologist. A 24-hour a day referral pathway should exist for all NSW hospitals to obtain such advice on the authority of the patient’s AMO, who can then direct the junior medical officer (or registrar if possible) to call.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 20
Review of antibiotic therapy Antibiotic therapy must be reviewed within 24 hours of commencement and again when microbiology results are available. Antibiotics should be changed or ceased (if appropriate) when results are available. See the sepsis 48 hour management plan below.
Sepsis 48 hour management plan Patients with a diagnosis of sepsis are at high risk of deterioration and require close monitoring and follow up care. The sepsis pathways are intended for the immediate management of sepsis only. Follow up management should be determined in consultation with the AMO and other expert clinicians. A sepsis management plan is recommended to ensure that the patient is closely monitored, test results and antibiotic choices are reviewed in appropriate timeframes and the patient management plan is adjusted accordingly. The CEC sepsis 48 hour management plan can be used for patients in the emergency department, ward or intensive care. The plan can be adapted to meet individual facility preferences.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 21
EDUCATION Resources have been developed that can be used by health care facilities to support widespread engagement with the program and develop clinician knowledge and skills. They can be adapted to meet health care facility needs and can be incorporated into existing education processes, such as BTF Tier Two education (DETECT training). It is highly recommended that local sepsis case studies and data are used. The CEC provides a program of interactive webex / teleconference sepsis learning sessions. Details of the program and instructions for joining the sessions are distributed in advance via the LHD sepsis lead. The following education resources are available on the CEC sepsis website and are periodically updated.
SEPSIS KILLS video (4 minutes) Key messages on the SEPSIS KILLS program and why sepsis is a medical emergency. This video can be used as a stand-alone resource to quickly convey key messages or it can be incorporated into a wider education session. SEPSIS KILLS general presentation A presentation overview incorporating the five elements of the program and the NSW implementation strategy. SEPSIS KILLS clinical presentation: adults Key concepts of recognition, resuscitation and referral for adult patients with sepsis in the inpatient ward. SEPSIS KILLS clinical presentation: paediatrics Key concepts of recognition, resuscitation and referral for paediatric patients with sepsis in the inpatient ward SEPSIS KILLS multiple choice questions This short quiz has evidence based questions to test sepsis knowledge and is suitable for a broad range of clinical staff caring for adult and/or paediatric patients.
SEPSIS KILLS frequently asked questions The FAQ sheets address the commonly asked questions about the program. SEPSIS KILLS eLearning sepsis module This online module is available via the HETI Moodle site and includes adult and paediatric case studies on emergency department and ward patients.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 22
EVALUATION Evaluation is a systematic process to determine the extent of the improvements that have been made. Measurement ensures that clinical practice changes are carried out and provide a source of feedback and learning. CEC sepsis database The CEC sepsis database provides a tool to collect and analyse data. It is a web based application, which is accessed by entering hospital facility or LHD username and password on the NSW Health intranet system. CEC is working with HealthShare NSW to facilitate integration with other data collection programs. The measures for the inpatient wards for both adults and paediatrics, have been agreed in consultation with clinicians and clinical governance units as follows:
Measure Description Definition Data collection
Antibiotics Time to administration of antibiotics
Timely administration of antibiotics increases the likelihood of survival and better patient outcomes
Time of CERS call / sepsis recognition to time of administration of first intravenous antibiotic
Time taken recorded on CEC sepsis data collection form that is then entered into CEC sepsis database
Resuscitation fluids Amount of bolus fluid administered
Timely administration of intravenous resuscitation fluids increases the likelihood of survival and better patient outcomes
Amount of bolus fluid administered within 60 minutes of CERS call / sepsis recognition
Record on CEC sepsis data collection form that is then entered into CEC sepsis database
Systolic Blood Pressure (Adults only) SBP recorded at time of CERS call / sepsis recognition
Hypotension is a significant indicator in severe sepsis and septic shock
The first systolic blood pressure measurement taken at time of CERS call / sepsis recognition
SBP measurement level recorded on CEC sepsis data collection form that is then entered into CEC sepsis database
Clinical Review Call or Rapid Response
Indicates escalation of care is required
Level of escalation Clinical Review Call or Rapid Response recorded on data collection form that is then entered into CEC sepsis database
Lactate
High serum lactate levels are an indicator of poor tissue perfusion and are strongly associated with morbidity and mortality
A serum lactate level collected within 60 minutes of CERS call / sepsis recognition
Collected Yes / No and if Yes serum lactate level recorded on CEC sepsis data collection form that is then entered into CEC sepsis database
Transfer of Care
Where the patient was managed or transferred to as a result of the sepsis episode
Ward, HDU / ICU, other hospital or tertiary referral
Ward, HDU / ICU, other hospital or tertiary referral recorded on CEC sepsis data collection form that is then entered into CEC sepsis database

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 23
Other measures that can be used to review care of patients with sepsis Some additional measures that can be used at facility or LHD level to ascertain the effectiveness of the program include:
• Hospital length of stay for patients with sepsis • Number of patients transferred to ICU with sepsis • ICU length of stay for patients with sepsis • Morbidity and mortality rates for patients with sepsis • Root Cause Analysis data • Clinical Review/Rapid Response data.
Monitoring and reporting your data It is important to monitor, report and evaluate the program data to ensure that clinical practice and processes for recognition and management of the patient with sepsis are effective. The roles are outlined below.
Facility Processes should be established for ward/unit and facility monitoring of progress. It is suggested that monitoring and report processes be integrated with existing Clinical Emergency Response Systems (CERS) for the deteriorating patient. Local Health District Clinical governance units have established monitoring and reporting requirements and systems at LHD level and will liaise with facilities on the local requirements. Clinical Excellence Commission Monitors and reports on statewide progress. Reports are provided six-monthly to LHD and facilities.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 24
REFERENCES
1. World Sepsis Day Organisation [internet] 2014. [cited 2014,March 31] Available from: http://www.world-sepsis-day.org/
2. Finfer S, Bellomo R, Lipman J. Adult-population incidence of severe sepsis in Australian and New Zealand intensive care units. Intensive Care Medicine 2004; 30:589–596.
3. Czura CJ Merinoff Symposium 2010: sepsis – speaking with one voice. Molecular Medicine; 2011; 17:1-2, 2-3.
4. Han Y, Carcillo J, Dragotta M, Bills D, Watson S, Westerman M, Orr R. Early Reversal of Pediatric-Neonatal Septic Shock by Community Physicians Is Associated With Improved Outcome. Pediatrics 2003; 112(4) 793-799.
5. Australasian Resuscitation in Sepsis Evaluation (ARISE) Investigators and the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) Management Committee. The outcome of patients with sepsis and septic shock presenting to emergency departments in Australia and New Zealand. Critical Care and Resuscitation 2007; 9:8-18.
6. .Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 2006; 34:1589-1596.
7. Marwick CA, Guthrie B, Pringle JE, et al. A multifaceted intervention to improve sepsis management in general hospital wards with evaluation using segmented regression of interrupted time series. British Medical Journal 2013;0:1-8
8. Clinical Excellence Commission. Clinical Focus Report: Review of Root Cause Analysis and/or Incident Information Management System (IIMS) Data Recognition and Management of Sepsis. Clinical Excellence Commission 2009; Sydney.
9. Clinical Excellence Commission. Quality Systems Assessment, Self Assessment Supplementary Report - Sepsis 2011. Clinical Excellence Commission 2011; Sydney.
10. Clinical Excellence Commission & Agency for Clinical Innovation. Cost effectiveness analysis stage one: do nothing and the case for change. ACI/CEC Policy and Technical Support Unit 2011; Sydney
11. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Critical Care Medicine. 2013;41(2):580-63
12. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B. Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal Medicine 2001;345:1368-1377.
13. Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Critical Care Medicine 2010; 38:1045-1053.
14. Australian Commission on Safety and Quality in Health Care, National Safety and Quality Health Service Standards. September 2012
15. Jones D, Duke G, Green J et al. Medical Emergency Team syndromes and an approach to their management. [cited 2014, March 31] Available from: http://ccforum.com/content/10/1/R30
16. Antibiotic Expert Group. Therapeutic Guidelines: Antibiotic Version 14. Melbourne: Therapeutic Guidelines Limited; 2010. Accessed through eTG complete.

Sepsis Toolkit | Inpatient Program Implementation Guide | Page 25
PART B - TOOLS & RESOURCES

This page has been left intentionally blank

GOVERNANCE
Program summary
Memo template
Facility implementation plan
Facility implementation checklist
Common causes of delay in recognising and treating sepsis in the wards
Implementation action plan
Ward implementation checklist
Sepsis issues log

SEPSIS KILLS PROGRAM Sepsis is an international health care problem Sepsis is a life-threatening condition that arises when the body’s response to infection injures its own tissues and organs, and can present in any patient in any clinical setting. It is one of the leading causes of death in hospital patients worldwide. More patients die from sepsis than prostate cancer, breast cancer and HIV/AIDS combined1. Severe sepsis and septic shock in adults have a mortality rate of around 25 per cent2. In paediatric patients, sepsis is one of the leading causes of death with mortality rates as high as 10 per cent. Many of these deaths are preventable3.
Appropriate recognition and timely management of patients with severe infection and sepsis is a significant problem in health care facilities. Delayed treatment is associated with high mortality rates, significant morbidity and high costs to the health care system. The mortality rate for adult patients with septic shock has been shown to increase by 7.6 per cent for every hour of delay in commencing antibiotic therapy, after the onset of hypotension4. In the complex hospital ward environment there are frequently long delays between medical review and antibiotic prescription particularly when decision making is by junior medical officers5. SEPSIS KILLS program in NSW The Clinical Excellence Commission (CEC) Clinical Focus Report on Recognition and Management of Sepsis found deficits in a range of clinical settings in NSW health care facilities6. The lack of timely recognition and appropriate management was further demonstrated in the findings from the 2011 CEC Quality Systems Assessment.
The SEPSIS KILLS program aims to reduce preventable harm to patients through improved recognition and management of severe infection and sepsis in emergency departments and inpatient wards.
The program is based on three key actions:
RECOGNISE the risk factors, signs and symptoms of sepsis
RESCUSITATE with rapid intravenous fluids and administration of antibiotics within the first hour of diagnosis of sepsis
REFER to appropriate senior clinicians and teams and retrieval if appropriate
It is founded on international evidence-based practice7 and brings significant benefits to NSW hospitals at both the clinical and system levels including:
• Enhanced clinician skills in sepsis recognition and management • More timely, standardised and effective detection and management of sepsis • Reduced mortality, morbidity and bed-stays from sepsis-related conditions • Improved and safer patient experience.
The SEPSIS KILLS program was launched in May 2011 and has been implemented in 180 NSW public hospital emergency departments. The process of care for patients with sepsis has been greatly improved. Median time to start intravenous antibiotics has been reduced from more than 4 hours in 2011, to consistently less than 60 minutes in 2013 and 2014. Inpatient Sepsis Program Phase 2 of the SEPSIS KILLS program is focused on improving the recognition and management of sepsis in adults and children in inpatient wards of medium and large hospitals. It will be introduced Statewide from May 2014. Each

Local Health District has an Executive Sponsor and a sepsis lead. There will be an Executive-led sepsis team and clinical champions in each hospital driving the implementation and evaluation.
The inpatient program directly links with the Between the Flags (BTF) system and the NSW Health Policy: Recognition and Management of Patients who are Clinically Deteriorating (PD2013_049). Preliminary NSW sepsis data suggests that 30 per cent of clinical deterioration in adults that require a Rapid Response are septic. This is replicated in national and international literature with sepsis being a leading cause for clinical deterioration, accounting for one in three calls for a Rapid Response team8. A critical component of the sepsis program is timely and appropriate escalation to a senior clinician. The tools provided by the BTF system and SEPSIS KILLS program give clinicians objective criteria backed by policy for escalation, which empowers them to call for senior clinical help when they judge a patient to be deteriorating and/or are concerned that the patient has sepsis. Implementation in (add hospital) (add local information here) Further information is available from: (add facility/LHD sepsis leads here) Sepsis Program Lead Phone: (02) 9269 5500 Email: [email protected] Web: www.cec.health.nsw.gov.au/programs/sepsis References 1. World Sepsis Day Organisation 2014. [cited 2014, April 3] Available from: http://www.world-sepsis-day.org/ 2. The Australasian Resuscitation in Sepsis Evaluation (ARISE) Investigators and the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) Management Committee. The outcome of patients with sepsis and septic shock presenting to emergency departments in Australia and New Zealand. Critical Care and Resuscitation 2007; 9:8-18. 3. Han Y, Carcillo J, Dragotta M, Bills D, Watson S, Westerman M, Orr R. Early Reversal of Pediatric-Neonatal Septic Shock by Community Physicians Is Associated With Improved Outcome. Pediatrics 2003; 112(4) 793-799 4. Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 2006; 34:1589-1596. 5. Marwick CA, Guthrie B, Pringle JE, et al. A Multifaceted intervention to improve sepsis management in general hospital wards with evaluation using segmented regression of interrupted time series. British Medical Journal 2013;0:1-8 6. Clinical Excellence Commission. Clinical Focus Report from review of root cause analysis and/or incident information management system (IIMS) data recognition and management of sepsis. Clinical Excellence Commission 2009; Sydney. 7.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock:2012. Critical Care Medicine. 2013;41(2):580-63 8. Jones D, Duke G, Green J et al. Medical Emergency Team syndromes and an approach to their management. [cited 2014, March 31] Available from: http://ccforum.com/content/10/1/R30

INTERNAL MEMORANDUM
TO
FROM
TEL DATE
SUBJECT SEPSIS KILLS program commencing at xxxx hospital
Sepsis is a medical emergency. Sepsis is the cause of more adult deaths per year than prostate cancer, breast cancer and HIV combined. Thirty per cent of inpatients who require a Rapid Response are septic and mortality for these patients increases with delays in receiving appropriate treatment. The SEPSIS KILLS program is going live in XX Hospital on xxxx 2014. It focuses on the Recognition, Resuscitation and Referral of patients who are septic. Patients at greatest risk include those with:
• Any kind of infection-bacterial, viral, parasitic, or fungal-anywhere in the body • Pre-existing (chronic) medical conditions • Underactive immune system • Surgery • Invasive procedures or IV lines
When a patient is suspected of having sepsis, the medical officer must immediately undertake six key actions in discussion with a senior doctor:
1. Administer high flow oxygen to improve oxygen delivery to tissues 2. Take TWO blood cultures and other necessary specimens 3. Measure serum lactate - elevated levels are directly linked to increased mortality 4. Give appropriate IV antibiotics within 60 minutes. Every additional hour’s delay results in mortality
increasing by 7.6% 5. Give adequate IV fluid resuscitation within 60 minutes to reduce organ dysfunction and multi-organ failure 6. Monitor urine output and vital signs after each fluid challenge and continue to re-assess
All xxxx are required to attend a session on the new sepsis recognition and management processes on xxxx 2014 and successfully complete the sepsis multiple choice questionnaire.

SEPSIS KILLS PROGRA M IMPLE MENTATION PLAN Page 1
XXX HOSPITAL
INSERT FACILITY NAME IMPLEMENTATION PLAN
SEPSIS KILLS PROGRAM

SEPSIS KILLS PROGRA M IMPLE MENTATION PLAN Page 2
XXX HOSPITAL
PROGRAM BACKGROUND
Program Title: SEPSIS KILLS program
Program Aim: To improve the recognition and timely management of sepsis in the inpatient wards of xxxx hospital
Program Background: Include information here from the summary template provided in the Sepsis Toolkit plus local information to support the case for change
Program Benefits:
Implementation of the SEPSIS KILLS program will result in: • enhanced clinician skills in sepsis recognition and management • reduced mortality, morbidity and bed-stays from sepsis-related conditions • enhanced networking opportunities across the system for clinicians and
service teams • improved quality and safety of care and a better and safer patient
experience
Program Objectives: Use SMART objectives: • Specific • Measurable • Achievable • Relevant • Timely

SEPSIS KILLS PROGRA M IMPLE MENTATION PLAN Page 3
XXX HOSPITAL
SCOPE OF THE PROGRAM
This program will include: This program will not include:
Which clinical wards or units will be included, or will it be a whole of facility approach? Consider piloting in one or two wards or units before spreading to other areas.
What is out of scope?
Program Deliverables:
What will you deliver at the end of the implementation process? NOTE: these are the products you will have at the end of the process, e.g. an education program, sepsis pathway adapted for local environments, improved awareness levels etc.
Program Milestones: Key activities and dates (month/year) they will be completed
Evaluation:
How will you measure the success of the sepsis pathway implementation? NOTE: evaluation criteria must be specific and measurable eg • % clinical staff who attend an education session on sepsis recognition and
management • % Rapid Responders who attend an education session on sepsis recognition
and management and achieve 80% correct answers on the Sepsis MCQ • % of patients diagnosed with probable sepsis in xxxx facility who receive
intravenous antibiotics within one hour of recognition of sepsis
Resources: What are the resources required to undertake the program? Consider: people, space to meet and access to a computer and internet, etc.
Linkages:
Are there opportunities for this program to gain leverage or support from other groups? For example deteriorating patient program, national accreditation standards, clinical handover, antimicrobial stewardship, risk management programs.

SEPSIS KILLS PROGRA M IMPLE MENTATION PLAN Page 4
XXX HOSPITAL
RISK ASSESSMENT
Program Risks Risk Rating Mitigation Strategy
Residual Risk
Rating What are the risks to successful completion of the program?
(high, medium,
low)
List strategies to remove or minimise the risks
(high, medium,
low)
COMMUNICATION PLAN
Who do you need to engage to make this program successful?
Stakeholder Position What are their information needs?
How and when are you going to let them know?

SEPSIS KILLS PROGRA M IMPLE MENTATION PLAN Page 5
XXX HOSPITAL
PROGRAM TEAM ROLES
Executive Sponsor: Name and designation of Executive Sponsor Role of the Executive Sponsor ie what do they do?
Program Lead:
Name and designation Email Phone number Role of the Program Lead
Clinical Lead(s): Name and designations Role of the Clinical Lead
Program Team Members: Name and designations Role of the Program Team Members
Start Date: Completion Date:
ENDORSEMENT
Facility Executive Sponsor Name:
Signature and Date:
Facility Sepsis Lead Name: Signature and Date:
LHD Sepsis Lead Name: Signature and Date:
LHD Director Clinical Governance
Name: Signature and Date:
Adapted under Creative Commons Attribution 3.0 Australia (https://creativecommons.org/licenses/by/3.0/au/legalcode) from the National Institute of Clinical Studies (NICS) Acute Stroke and TIA Care Bundle Project Plan Template, National Health and Medical Research Council, http://www.nhmrc.gov.au/nics/programs/emergency/stroke_tia.htm © National Health and Medical Research Council, 2007.

FACILITY IMPLEMENTATION CHECKLIST
SEPSIS KILLS PROGRAM
GO
VE
RN
AN
CE
Step 1: Establish a strong case for change • Develop a brief summary of the problem to capture interest. • Specify the change to be made and provide evidence as to why the change should be
made now.
Step 2: Establish governance arrangements and a program team • Identify a program leader and executive sponsor • Convene a team involving key stakeholders • Identify the facility responsible committee and reporting/communication channels • Develop a program plan for endorsement by hospital executive and LHD CGU • Develop a comprehensive communication strategy.
Step 3: Recruit respected and influential leaders and champions • Recruit medical and nursing leads/champions for each ward/unit • Seek advice from emergency department sepsis clinical leads, Between the Flags
coordinators and others who have led organisational clinical change programs.
Step 4: Identify sepsis management barriers and enablers • Audit the baseline sepsis management evidence-practice gap • Brainstorm the causes of inadequate or delayed recognition and treatment of sepsis • Develop an action plan to address each barrier. Consider:
o process change (WHAT has to be done); and o people change (HOW this will be communicated)
• Identify the enablers that will support the required changes.
CE
RS
AN
D S
EP
SIS
TO
OLS
Step 5: Adapt the sepsis tools to align with CERS and other local processes • Review the sepsis pathway and align with local CERS if needed • Establish escalation process for patients with sepsis to:
o AMO o Infectious Diseases o intensive care unit
• Develop/adapt local ISBAR tool for sepsis patients • Establish minimum monitoring requirements for ward patients with sepsis • Align the CEC sepsis antibiotic guideline with local drug and AMS processes
Step 6: Identify tools and resources to support sepsis management • Consider use of sepsis blood order sets • Identify components and placement of sepsis kit/pack/trolley • Review IV cannulation access in-hours/after-hours • Review the process for timely access to lactate measurement

ED
UC
AT
ION
Step 7: Develop an education strategy • Identify education tiers or groups to meet local needs • Determine modes of education. Consider:
o face to face awareness sessions o DETECT training o orientation o simulation training
• Document a plan to provide tailored education for specific professional and craft groups • Determine education evaluation methodology.
ME
AS
UR
EM
EN
T &
EV
ALU
AT
ION
Step 8: Pilot the new sepsis process • Implement the program in one or two areas using short Plan, Do, Study, Act cycles • Consider use of an issues log to document concerns as they arise • Seek feedback from stakeholders frequently and review progress • Celebrate quick wins and adapt methods as needed • Collect qualitative/quantitative data to measure improvement
Step 9: Sustain and spread the approach to other wards/units • Sustain the changes at the pilot site(s) and embed in organisational structures and routines • Communicate the pilot outcomes using a variety of approaches including meetings,
newsletters, intranet posts • Market the good news stories and benefits to patients and staff • Spread program to other wards/units in a phased approach • Develop organisational guidelines on sepsis management principles and procedures
Step 10: Measure, evaluate and improve • Evaluate improvement – consider organisational, process and people change. • Consider using a range of methods including:
o medical record audit o observational audit o survey o focus group o consumer interviews o consumer feedback
• Display evaluation data and discuss at ward meetings • Report results/action to staff, facility and LHD levels • Promote success stories and lessons learnt.

COMMON CAUSES OF DELAY
RECOGNISING AND TREATING SEPSIS IN THE WARDS
Recognition • Lack of nursing and junior doctor knowledge of sepsis risk factors, signs, symptoms
• Observations performed infrequently so not a timely indicator for deterioration and/or sepsis
• Sepsis screening processes different in each ward
• Rationalise that fever is disease related, not sepsis OR it can’t be sepsis as there is not fever
• Night RMO does not give high priority to sepsis due to workload and/or lack of knowledge that sepsis is a
medical emergency
• Failure to communicate sepsis risk/diagnosis in clinical handover or ED to ward handover
• Not testing lactate to aid diagnosis due to lack of knowledge and/or access to testing
• Stuck in a particular diagnosis and sepsis not considered.
Escalation • Senior clinician not available to assist in making diagnosis
• No formal RMO escalation process for sepsis
• Medical registrar, AMO or ID not consulted or informed of new sepsis
• Wait for investigations/specimens and/or results before escalation
• Surgical teams in theatre and unable to respond
• Long delay between call and after hours medical review
• NFR status unavailable
• Multiple teams looking after patient – confusion as to who to inform/seek advice.
Treatment • Basic resuscitation not happening whilst awaiting arrival of Rapid Response team
• Doctor not familiar with sepsis pathway or bundle of care
• Long time to cannulation due to difficult access or not done at time of diagnosis
• Doctor or nurse cannulation skills not available on all shifts
• Fluid resuscitation volume/time for administration not standard
• Nurses (and doctors) don’t know what/how to give a rapid bolus (fluid challenge)
• Limited understanding of antibiotic prescribing choices/regimes in sepsis or give favoured antibiotics
• Senior doctor or Infectious Diseases advice not sought by junior doctors for initial treatment
• No antibiotics changed/commenced overnight – wait for morning rounds
• Wait for results of tests/investigations before commencing/changing antibiotics
• Prescription of antibiotics (writing up) and communication of same with nursing staff
• Nurses don’t consider antibiotics as urgent treatment
• Antimicrobial stewardship impacts on antibiotic choices and availability
• Antibiotics given as a slow infusion
• Equipment and resources for sepsis not centralised or available eg blood culture bottles
• Lack of monitoring of observations and urine output in patients post Rapid Response call or sepsis diagnosis.

IMPLEMENTATION ACTION PLAN – SEPSIS KILLS PROGRAM
Focus Area Action Owner Due Status / Progress 1.. Administration of antibiotics in 60 minutes or less
Implement process for MOs to check/establish IV access at the time of prescribing antibiotics.
Set up sepsis trolley or packs in all wards with cannulation equipment and antibiotics.
Review facility guidelines for administering antibiotics as IV bolus doses where appropriate.
2..
3..
4..
5..

IMPLEMENTATION ACTION PLAN – SEPSIS KILLS PROGRAM
6..
7..
8..
9..
10..

WARD IMPLEMENTATION CHECKLIST
SEPSIS KILLS PROGRAM
Gov
erna
nce Nursing sepsis lead/champion identified
Medical sepsis lead/champion identified
Communication pathways for hospital sepsis lead and executive sponsor identified
SEPSIS KILLS is an agenda item for ward meetings
CER
S an
d Se
psis
Too
ls
Sepsis pathway displayed in ward areas
Paper and electronic versions of sepsis pathway readily available in nominated areas
Sepsis trolley or pack assembled with process agreed for checking and re-stocking
Sepsis blood order sets agreed
Antibiotic guideline and antibiotics available
Lactate measurement process agreed
IV cannulation available in-hours and after-hours
Escalation processes for nursing staff agreed
Escalation processes for medical staff agreed (AMO/senior clinician/ICU)
Minimum observation/monitoring requirements for patients with sepsis agreed
Eval
uatio
n
Process for collection of sepsis pathways/audit sheets determined
Process for checking and collating sepsis data determined
SEPSIS KILLS results displayed in ward
Results/actions to improve discussed at ward meetings
Results/actions reported to sepsis lead /hospital responsible committee
Success stories and lessons learnt communicated in ward and other relevant forums
Educ
atio
n
Program for SEPSIS KILLS education developed and communicated
Posters and other promotional materials available and displayed
All staff completed the SEPSIS KILLS awareness education
All staff completed the SEPSIS KILLS multiple choice questions
All staff educated on sepsis pathway data collection requirements

ISSUES LOG XXXX WARD - SEPSIS KILLS PROGRAM
Insert additional pages as required
XXXX HOSPITAL
SEPSIS KILLS PROGRAM: ISSUES LOG
WARD XX
• Please record all concerns and issues with the use and application of the Sepsis Pathway and antibiotic guideline. • Issues that should be logged include: difficulty with decision making or use of the pathway, escalation, communication and teamwork, medications and
fluids, clinical incidents, and pathology. • All Clinical Incidents must be recorded in IIMS as per usual practice.
For support and advice please contact:
Name: Name: Name:
Position: Position: Position:
Phone: Pager: Phone: Pager: Phone: Pager:

ISSUES LOG XXXX WARD - SEPSIS KILLS PROGRAM
Insert additional pages as required
# Date Time (00:00) Patient Name MRN Details of Issue and Action Taken IIMS Notifier Noted by NUM
(or delegate)
1.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:
2.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:
3.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:
4.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:

ISSUES LOG XXXX WARD - SEPSIS KILLS PROGRAM
Insert additional pages as required
# Date Time (00:00) Patient Name MRN Details of Issue and Action Taken IIMS Notifier Noted by NUM
(or delegate)
5.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:
6.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:
7.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:
8.
:
□ Yes □ No □ N/A
Date: Time: Initial: Name:

This page has been left intentionally blank

SEPSIS TOOLS
Adult inpatient sepsis pathway
Paediatric inpatient sepsis pathway
Sepsis 48 hour management plan
Adult inpatient sepsis intravenous antibiotic guideline
ISBAR tool
Escalation triggers for calling an AMO for patients with sepsis
Sepsis trolley/pack content list

RES
PON
D &
ESC
ALA
TE
REC
OG
NIS
E
NO
Patient may have SEPSIS
• Obtain senior clinician review
• Call for a Clinical Review (as per local CERS) unless already made
• Look for other causes of deterioration
• Commence treatment as per sepsis resuscitation guideline
• Inform the Attending Medical Officer (as per local CERS)
Turn over page for sepsis resuscitation guideline
History of fevers or rigors
Cough/sputum/breathlessness
Abdominal pain/distension
Line associated infection/redness/swelling/pain
Dysuria/frequency/odour
New onset of confusion or altered LOC
Recent surgery/cellulitis/wound infection
Immunocompromised/chronic illness
Does your patient have TWO or more YELLOW ZONE observations
or additional criteria?
Patient has SEVERE SEPSIS or
SEPTIC SHOCK until proven otherwise
• Sepsis is a medical emergency
• Call for a Rapid Response (as per local CERS) unless already made
• Commence treatment as per sepsis resuscitation guideline
• Inform the Attending Medical Officer that your patient has sepsis
Turn over page for sepsis resuscitation guideline
Does your patient have any RED ZONE observations or
additional criteria? NB: LACTATE > 4mmol/L
= Rapid Response
Look for other common causes of deterioration
New arrhythmia Hypovolaemia/haemorrhage Pulmonary embolus/DVT Atelectasis AMI Stroke Overdose/over sedation
• Initiate appropriate clinical care
• Repeat observations within 30 minutes AND increase the frequency of observations as indicated by the patient’s condition
• Re-evaluate for sepsis if observations remain abnormal or deteriorate
PLUS
YES
Discuss management plan with patient and family
OR
DOES YOUR PATIENT HAVE A KNOWN OR SUSPECTED INFECTION?
Have a higher level of suspicion of sepsis for patients age > 65 years
YES
Does your patient have any of the following sepsis risk factors, signs or symptoms present?
Clinical Excellence Commission © Released May 2014
SEPSIS PATHWAY – ADULT – INPATIENT
This pathway is intended for the recognition and immediate management of sepsis
Use relevant febrile neutropenia guidelines if the patient has haematology/oncology diagnosis

REF
ER
This patient may need transfer to an Intensive Care Unit • Discuss the patient’s condition with the Attending Medical Officer • Consider a higher level of care as per local CERS • Discuss management plan with patient and their family/carers
THIS PATIENT HAS SEVERE SEPSIS OR SEPTIC SHOCK ESCALATION IN LEVEL OF CARE IS REQUIRED
RES
USC
ITAT
E &
REA
SSES
S
Large bore intravenous access, collect and check results: Lactate Blood cultures x 2 FBC
Call for expert assistance after two failed IVC attempts
Maintain patent airway
Give oxygen Aim SpO2 ≥ 95% (or 88-92% for COPD & chronic type II respiratory failure)
IV Fluid Resuscitation Give initial 250-500mL 0.9% sodium chloride bolus STAT: aim for SBP > 100mmHg If no response, repeat 250-500mL 0.9% sodium chloride boluses STAT until SBP > 100mmHg unless there are signs of pulmonary oedema Escalate to Rapid Response if no response in SBP after 1000mL of fluid
Adapt treatment to the patient’s Resuscitation Plan if applicable
PRESCRIBE and ADMINISTER ANTIBIOTICS WITHIN 60 MINUTES Do not delay for investigations or results
If patient already on antibiotic therapy this MUST be reviewed by the Attending Medical Officer
Blood gas Coags LFTs
EUC CRP Glucose
Procalcitonin if available
Assess level of consciousness (LOC) using Alert, Verbal, Pain, Unresponsive (AVPU) If V or less conduct a GCS If P or U reassess Airway, Breathing and Circulation
Fluid balance Monitor and document fluid input & output - consider IDC Maintain urine output > 0.5 mL/kg/hour
Continue monitoring and assess for signs of deterioration: • Respiratory rate in the Red or Yellow Zone • SBP < 100mmHg • Decreased or no improvement in level of consciousness • Urine output < 0.5mL/kg/hour • Increasing or no improvement in serum lactate
Examine patient for source of sepsis Collect appropriate swabs, cultures, chest X-ray, ECG if indicated
Check Blood Glucose Level: if > 12mmol/L consider glycaemic control
Clinical Excellence Commission © Released May 2014
MONITOR &
REASSESS
A
B
C
D
E
F
G
SEPSIS PATHWAY – ADULT – INPATIENT
SEPSIS RESUSCITATION GUIDELINE

SEPSIS PATHWAY – PAEDIATRIC – INPATIENT
This pathway is intended for the recognition and immediate management of sepsis
Use relevant febrile neutropenia guidelines if the patient has haematology/oncology diagnosis
Patient may have SEPSIS • Obtain early senior clinician
review within 30 minutes
• Consider and review blood gas
Does senior clinician consider
patient to be septic?
.
Commence treatment as per sepsis resuscitation guideline (over page)
Ensure the Attending Medical Officer/Paediatrician/NETS is aware (as per local CERS)
RES
PON
D &
ESC
ALA
TE
ARE YOU CONCERNED THAT YOUR PATIENT COULD HAVE EARLY SEPSIS?
PLUS
YES NO
Does your patient have TWO or more YELLOW ZONE observations OR additional criteria OR clinician
concern? NB: Three Yellow Zone Criteria = Rapid Response
*Persistent tachycardia is consistent with sepsis
Look for other common causes of deterioration • Initiate appropriate clinical
care
• Repeat observations within 30 minutes AND increase the frequency of observations as indicated by the patient’s condition
• Re-evaluate for sepsis if observations remain abnormal or deteriorate
YES
YES
YES
NO
Discuss management plan with patient and family
REC
OG
NIS
E
Patient has SEVERE SEPSIS or
SEPTIC SHOCK until proven otherwise
• Sepsis is a medical emergency
• Call for a Rapid Response (as per local CERS) unless already made
Any of these values are significant in sepsis
• Lactate > 2 mmol/L • BE < - 5 • Procalcitonin (PCT) > 0.5
Clinical Excellence Commission ©, Released May 2014
Deterioration despite treatment New or persistent signs of toxicity:
Alertness, arousal or activity decreased; colour pale or mottled; cool peripheries; cry weak; grunting; rigors; bounding pulses; wide pulse pressure
New onset of fever ≥38.50c (neonates ≥380c) High level parental concern Blood WCC outside normal range
Recent surgery/cellulitis/wound infection
Line associated infection/redness/ swelling/pain
Central line in-situ
Chronic illness or immunocompromised
3 months of age or younger (corrected)
Does your patient have any of the following sepsis risk factors, signs or symptoms present?
Does your patient have any RED ZONE observations OR additional criteria OR
serious clinician concern?
Ensure senior clinician review to confirm
likelihood of sepsis

Intravenous access, collect and check results:
SEPSIS RESUSCITATION GUIDELINE R
EFER
Blood gas Blood culture(s) FBC
Consider intraosseous access after two failed attempts or 60 seconds
This patient may need transfer to a Paediatric Intensive Care Unit • Update the Attending Medical Officer on patient’s condition • Seek advice from local/regional paediatric experts and/or NETS Tel: 1300 36 2500 • Early inotropes and intubation may be necessary • Discuss management plan with patient and their family/carers
THIS PATIENT HAS SEVERE SEPSIS OR SEPTIC SHOCK ESCALATION IN LEVEL OF CARE IS REQUIRED
Maintain patent airway
Give oxygen Aim SpO2 ≥ 95%
IV Fluid Resuscitation Give 20mL/kg 0.9% sodium chloride bolus STAT Repeat 20mL/kg 0.9% sodium chloride bolus if no improvement in heart rate, capillary refill, colour
Adapt treatment to the patient’s Resuscitation Plan if applicable
PRESCRIBE and ADMINISTER ANTIBIOTICS WITHIN 60 MINUTES Do not delay for investigations or results
If patient already on antibiotic therapy this MUST be reviewed by the Attending Medical Officer
Consider alternate source of infection and/or resistance
Lactate Coags LFTs
EUC CRP Glucose
Procalcitonin if available
Assess level of consciousness (LOC) using Alert, Verbal, Pain, Unresponsive (AVPU) If V or less conduct a GCS If P or U reassess Airway, Breathing and Circulation
Fluid balance Monitor and document fluid input & output - consider IDC Maintain urine output > 1mL/kg/hour
MONITOR &
REASSESS
Continue monitoring and assess for signs of deterioration: • Persistent tachycardia, slow capillary refill and hypotension • Colour pale and mottled • Drowsiness or abnormal LOC • Urine output < 1mL/kg/hour • Acidosis, increasing serum lactate or procalcitonin • Hypoglycaemia, leukopenia or abnormal coagulation
Examine patient for source of sepsis Collect appropriate swabs, cultures, chest X-ray if indicated
Check Blood Glucose Level: if less than 3mmol/L treat with 2mL/kg 10% Dextrose
RES
USC
ITAT
E &
REA
SSES
S
Monitor: Respiratory rate Respiratory distress, SpO2
Monitor: Temp
Monitor: Urine output
Monitor: BGL
Clinical Excellence Commission ©, Released May 2014
A
B
C
D
E
F
G
Monitor: LOC
Monitor: Heart rate, BP, capillary refill, colour
SEPSIS PATHWAY – PAEDIATRIC – INPATIENT

SEPSIS 48 HOUR MANAGEMENT PLAN
Time Action Criteria
0 –
2 H
ours
Communication
Attending Medical Officer (AMO) informed that patient is on sepsis pathway Clinical handover must inform the receiving team that the patient was treated for sepsis
� �
Monitor and reassess
Monitor and reassess for sepsis deterioration which may include one or more of the following:
Respiratory rate in the Red or Yellow Zone Systolic blood pressure < 100mmHg Decreased or no improvement in level of consciousness Urine output less than 0.5mL/kg/hr No improvement in serum lactate level
If deteriorating, activate local CERS and inform AMO � If improving, continue observations every 30 minutes for 2 hours, then hourly for 4 hours �
Sepsis screen
Head to toe assessment for infection source and initiate investigations which may include:
• Diagnostic imaging � • Urine MSU (or CSU) for MCS � • Sputum for MCS � • Faeces for C.difficile and MCS (if diarrhoea) � • Wound swab for MCS � • Nasopharyngeal swabs � • Lumbar puncture (if indicated) �
Antibiotics
Medical officer to consult with AMO on appropriate antibiotic prescribing � Prescribe antibiotics in the medication chart and indicate the appropriate time for dosing �
IV Fluids Prescribe IV fluids as appropriate Monitor haemodynamic observations �

Time Action Criteria 2
– 24
Hou
rs
Continue monitoring
Monitor and reassess for sepsis deterioration which may include one or more of the following:
Respiratory rate in the Red or Yellow Zone Systolic blood pressure < 100mmHg Decreased or no improvement in level of consciousness Urine output less than 0.5mL/kg/hr No improvement in serum lactate level
If deteriorating, activate local CERS and inform AMO � If improving, continue observations every 30 minutes for 2 hours, then hourly for 4 hours �
Repeat lactate
Lactate level 4 hours post recognition
Date -- /--/ ---- Time --:-- ��.� mmol/L � Lactate level 4 hours post recognition
Date -- /--/ ---- Time --:-- ��.� mmol/ L �
Fluid Resuscitation
Prescribe IV fluids as appropriate Monitor haemodynamic observations
�
Reassess Check preliminary blood counts � If patient is neutropenic, review antibiotics and change if needed �
Review treatment
Review need for advanced care directives and ceiling of care if appropriate � Are any other causes of deterioration likely? �
• Discuss with AMO and treat accordingly • Cease antibiotics if appropriate • Continue monitoring for deterioration including urine output
24 –
48
Hou
rs
Reassess
Repeat biochemistry as indicated � Review results of tests and investigations �
• Discuss with AMO and treat accordingly • Cease antibiotics if appropriate • Continue monitoring for deterioration including urine output
Confirm diagnosis and document source of sepsis in medical record � This document is intended for patients who have been recognised as having sepsis and have started on a sepsis pathway. The Sepsis 48 Hour Management Plan aims to guide clinical staff using a step by step process which ensures that the patient monitoring and treatment is appropriate.

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 1 of 9
SEPSIS INTRAVENOUS ANTIBIOTIC GUIDELINE
ADULT - INPATIENT
The Clinical Excellence Commission (CEC) Adult Inpatient Sepsis Intravenous Antibiotic Guideline aims to guide the prescription and timely administration of antibiotics for adult inpatients that have a diagnosis of sepsis, severe sepsis or septic shock and have been admitted to hospital for 48 hours or more.
The guideline is based on the recommendations in Therapeutic Guidelines: Antibiotic version 14, 20101. It is intended to provide an accessible resource, which can be adapted to suit individual facility preferences in liaison with the antimicrobial stewardship team and local antimicrobial susceptibility patterns. Antimicrobial stewardship teams may wish to refer to their latest hospital cumulative antibiogram, if available, when modifying the guideline.
Prompt administration of antibiotics and resuscitation fluids is vital in the management of the patient with sepsis. The goal is to commence antibiotic therapy within the first hour of the recognition and diagnosis of severe sepsis.
The selection of appropriate antimicrobial therapy is complex and this guideline is not intended to cover all possible scenarios.
Clinicians must review antimicrobial therapy within 24 hours of commencement, and change or cease antibiotics as required once microbiology results are available.
This guideline is not intended for:
- patients with FEBRILE NEUTROPENIA who should be managed using local febrile neutropenia guidelines
- small hospitals and multi-purpose services where it would be more appropriate to use the Sepsis Adult FIRST DOSE Empirical Intravenous Antibiotic Guideline – Emergency Department
- patients who are deemed to have had incubating or unrecognised community acquired sepsis on admission. Use the Sepsis Adult FIRST DOSE Empirical Intravenous Antibiotic Guideline – Emergency Department
Obtain at least two sets of blood cultures from separate venepuncture sites before antibiotic administration.
Obtain other clinical specimens as appropriate but do not delay administration of antibiotics or wait for results of investigations.
The antimicrobial treatment indication and plan should be documented in the patient record.

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 2 of 9
*Examples of MROs include methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), extended-spectrum beta-lactamase (ESBL) producing organisms and carbapenem-resistant Gram negative organisms
Patient meets sepsis pathway criteria
Yes No
Does the patient have febrile neutropenia?
Consult immediately with the Attending Medical
Officer regarding antibiotic choice. Advice from the
designated infectious diseases and/or clinical microbiology services
may be required
Follow antibiotic regimen outlined in Table 1 or
local guideline if available in your facility
Consult immediately the Attending Medical
Officer and manage according to febrile
neutropenia guideline relevant for your facility
Yes No No
• antibiotic therapy within the last 7 days • had a recent infection with a multi-resistant organism (MRO)* or is known to
be colonised with an MRO • contra-indications to specific antimicrobial therapy recommended in the
guideline • multiple possible sources of infection • acute renal and/or hepatic failure • risk factors for an antibiotic resistant infection due to time spent in
hospital(s), overseas hospitalisation or residential care in previous 12 months
• surgical procedures that may influence the likely source of infection (e.g. urological surgery).
Does the patient have one or more of the following?
Does the patient have febrile neutropenia?

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 3 of 9
TABLE 1: ANTIBIOTIC PRESCRIBING (review after 24 hours)
Apparent source of sepsis Sepsis antibiotic regimen Penicillin allergic not immediate hypersensitivity
Penicillin or cephalosporin allergic
Immediate hypersensitivity or severe prior reaction
Sepsis secondary to hospital acquired pneumonia, low risk of MRO (generally patient who has been in hospital < 5 days who does not have risk factors for MRO)
ceftriaxone 1 g IV, daily
ceftriaxone 1 g IV, daily moxifloxacin 400 mg IV, daily
OR
OR
benzylpenicillin 1.2 g IV, 6-hourly PLUS gentamicin 4 to 6 mg/kg IV, for 1 dose (severe sepsis 7 mg/kg)
cefotaxime 1 g IV, 8-hourly
OR
cefotaxime 1 g IV, 8-hourly OR
piperacillin+tazobactam 4+0.5 g IV, 8-hourly OR
ticarcillin+clavulanate 3+0.1 g IV, 6-hourly
Sepsis secondary to hospital acquired pneumonia, high risk of MRO
piperacillin+tazobactam 4+0.5 g IV, 6-hourly
cefepime 2 g IV, 8-hourly Seek expert advice
If the patient is ventilated ADD gentamicin 4 to 6 mg/kg IV, for 1 dose (severe sepsis: 7 mg/kg)
OR
ticarcillin+clavulanate 3+0.1 g IV, 6-hourly
OR
cefepime 2 g IV, 8-hourly If the patient is ventilated ADD gentamicin 4 to 6 mg/kg IV, for 1 dose (severe sepsis: 7 mg/kg) If MRSA prevalent in your hospital ADD vancomycin 1.5g IV, 12-hourly
If MRSA prevalent in your hospital ADD vancomycin 1.5g IV, 12-hourly

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 4 of 9
TABLE 1: ANTIBIOTIC PRESCRIBING (review after 24 hours)
Apparent source of sepsis Sepsis antibiotic regimen Penicillin allergic not immediate hypersensitivity
Penicillin or cephalosporin allergic
Immediate hypersensitivity or severe prior reaction
Severe sepsis with an apparent urinary tract source
gentamicin 4-7 mg/kg IV, for 1 dose PLUS ampicillin 2 g IV, 6-hourly
gentamicin 4-7 mg/kg IV, for 1 dose
gentamicin 4-7 mg/kg IV, for 1 dose
OR
ceftriaxone 1 g IV, daily if gentamicin is contraindicated OR
cefotaxime 1 g IV, 8-hourly if gentamicin is contraindicated
Severe sepsis with an apparent biliary or gastrointestinal tract source
ampicillin 1 g IV, 6-hourly PLUS gentamicin 4 to 7 mg/kg IV, for 1 dose PLUS metronidazole 500 mg IV, 12-hourly
metronidazole 500 mg IV, 12-hourly PLUS ceftriaxone 1 g IV, daily
gentamicin 4 to 7 mg/kg IV, for 1 dose AND seek expert advice OR
metronidazole 500 mg IV, 12-hourly PLUS cefotaxime 1 g IV, 8-hourly
Severe sepsis resulting from a skin infection (including cellulitis) or surgical site infection
flucloxacillin 2 g IV, 6-hourly cephazolin 2 g IV, 8-hourly
clindamycin 450 mg IV, 8-hourly
If MRSA prevalent in your hospital ADD vancomycin 1.5g IV, 12-hourly
If MRSA prevalent in your hospital ADD vancomycin 1.5g IV, 12-hourly
OR
vancomycin 1.5 g IV, 12-hourly
Maternal sepsis (peri or post-partum) if source unclear
piperacillin+tazobactam 4+0.5 g IV, 8-hourly
ceftriaxone 1g IV, 24-hourly PLUS metronidazole 500mg IV 12-hourly
Seek expert advice
If patient meets criteria for toxic shock ADD clindamycin 600mg IV, 8-hourly If likely to be MRSA colonized ADD vancomycin 1.5g IV, 12-hourly
If patient meets criteria for toxic shock ceftriaxone 1g IV, 24-hourly PLUS clindamycin 600mg IV, 8-hourly in place of above regimen

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 5 of 9
TABLE 1: ANTIBIOTIC PRESCRIBING (review after 24 hours)
Apparent source of sepsis Sepsis antibiotic regimen Penicillin allergic not immediate hypersensitivity
Penicillin or cephalosporin allergic
Immediate hypersensitivity or severe prior reaction
Maternal sepsis likely to be due to Group A streptococcal infection
benzylpenicillin 2.4g IV, 4-hourly PLUS clindamycin 600mg iv 8-hourly
cephazolin 2 g IV, 6-hourly PLUS clindamycin 600mg iv 8-hourly
Seek expert advice
OR
OR
benzylpenicillin 2.4g IV, 4-hourly PLUS lincomycin 600 mg IV 8-hourly
cephazolin 2 g IV, 6-hourly PLUS lincomycin 600 mg IV 8-hourly
Severe sepsis, unknown source or focus, including possible IV line-associated sepsis Removal of the infected IV device is usually required
flucloxacillin 2 g IV, 6-hourly PLUS gentamicin 4-7 mg/kg IV, for 1 dose
cephazolin 2 g IV, 8-hourly PLUS gentamicin 4-7 mg/kg IV, for 1 dose
vancomycin 1.5 g IV, 12-hourly PLUS gentamicin 4-7 mg/kg IV, for 1 dose
If MRSA prevalent in your hospital ADD vancomycin 1.5g 12-hourly
If MRSA prevalent in your hospital ADD vancomycin 1.5g 12-hourly
NOTES FOR TABLE 1 Definitions of penicillin hypersensitivity
Immediate hypersensitivity involves the development of urticaria, angioedema, bronchospasm or anaphylaxis within one to two hours of drug administration.
Severe prior reaction involves a history of drug rash eosinophilia and systemic symptoms (DRESS) or Stevens-Johnson Syndrome following administration of a penicillin or cephalosporin.
All penicillin and cephalosporin class antibiotics are contraindicated in patients with history of drug rash eosinophilia and systemic symptoms (DRESS), Stevens-Johnson Syndrome or IgE-mediated immediate penicillin or cephalosporin allergy.
Refer to Therapeutic Guidelines: Antibiotic for more information
http://etg.hcn.com.au/desktop/tgc/abg/1315.htm
Definitions of low risk and high risk of MRO
Refer to Therapeutic Guidelines: Antibiotic for more information
http://etg.hcn.com.au/desktop/tgc/abg/5313.htm
Doses for renal impairment
(creatinine clearance ≤ 60mL/min)
Consult AMO (who may request referral to ID/Microbiology) in conjunction with guidance provided in Therapeutic Guidelines: Antibiotic
http://etg.hcn.com.au/desktop/tgc/abg/8571.htm

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 6 of 9
Gentamicin and vancomycin dosing and frequency
Refer to Therapeutic Guidelines: Antibiotic for more information
http://etg.hcn.com.au/desktop/tgc/abg/7823.htm
http://etg.hcn.com.au/desktop/tgc/abg/7971.htm
Criteria for toxic shock Refer to Therapeutic Guidelines: Antibiotic for more information
http://etg.hcn.com.au/desktop/tgc/abg/6225.htm
Notes for gentamicin
One dose of gentamicin is recommended; for subsequent doses, assess renal function and adjust frequency accordingly
Use for a maximum of 48 hours as empirical therapy pending outcome of investigations; monitoring of plasma concentrations NOT required if gentamicin is not used beyond 48 hours
Directed therapy (beyond 48 hours, based on microbiology results) should be used on the advice of infectious diseases physician or clinical microbiologist only
Dose should be based on ideal body weight or actual body weight – whichever of the two is lower
The maximum dose of gentamicin in severe sepsis is 640 mg
For other indications, the maximum dose is lower. Refer to Table 2.24 in Therapeutic guidelines: Antibiotic, version 14, 2010.
Contraindications:
Previous vestibular or auditory toxicity due to an aminoglycoside
Serious hypersensitivity reaction to an aminoglycoside
Precautions:
Pre-existing significant hearing problems
Pre-existing vestibular problems
Neuromuscular disorders, including myasthenia gravis
Chronic liver disease or severe cholestasis (bilirubin above 90 micromol/L)
Chronic renal failure or deteriorating renal function – consult AMO

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 7 of 9
TABLE 2: ANTIBIOTIC ADMINISTRATION 2,3
• Reconstitute antibiotics with sterile water for injection (WFI) unless stated otherwise.
• If further dilution is required for IV injection or infusion, use sterile sodium chloride 0.9% or sterile glucose 5% unless stated otherwise.
• Where possible use separate dedicated lines for resuscitation fluid and for medications. When injecting antibiotics directly into an IV injection port which has resuscitation fluid running:
- clamp the infusion fluid line and flush with 20 mL sterile sodium chloride 0.9% solution - administer antibiotic over the required time - flush the line with 20 mL sterile sodium chloride 0.9% solution and recommence resuscitation fluid.
Antibiotic Presentation (adult)
Reconstitution fluid/volume
Final volume Minimum administration time
Notes
ampicillin Vial 1 g 10 mL WFI 10 - 20 mL 3 – 5 minutes Penicillin class antibiotic
benzylpenicillin Vial 600 mg 2 mL WFI 10 mL 3 – 5 minutes Penicillin class antibiotic
Doses ≥ 1.2 g must be administered over 30 minutes
Vial 1.2 g 4 mL WFI
cefepime Vial 1 g 10 mL NS 10 mL 3 - 5 minutes Cephalosporin class antibiotic
Doses ≥ 2 g must be administered over 20 minutes
ceftriaxone Vial 1 g 10 mL WFI 10 mL 2 – 4 minutes Cephalosporin class antibiotic incompatible with calcium containing solutions, flush thoroughly before and after with sodium chloride 0.9%
cefotaxime Vial 1 g 10mL WFI 10 mL 3 – 5 minutes Cephalosporin class antibiotic
cephazolin Vial 1 g 10 mL WFI 10 mL 3 – 5 minutes Cephalosporin class antibiotic
clindamycin Ampoules
300 mg/2 mL
600 mg/4 mL
N/A 600 mg in 50 mL 20 minutes Check product is clear of any crystals prior to administration
900 mg in
100 mL
30 minutes

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 8 of 9
Antibiotic Presentation (adult)
Reconstitution fluid/volume
Final volume Minimum administration time
Notes
flucloxacillin Vial 1 g 5 mL WFI 10 mL 3 - 5 minutes
(1 g)
Penicillin class antibiotic
Repeated doses of 2 g via a peripheral line should be further diluted and infused over 20 – 30 minutes
20 mL 10 minutes
(2 g)
gentamicin
Ampoule
80 mg/2 mL
N/A 10- 20 mL (240mg or less)
3 – 5 minutes
Refer to notes for gentamicin
50 mL or
100 mL
(more than 240mg)
30 minutes
lincomycin
Vial 600mg/2mL
N/A 100mL 60 minutes
metronidazole Infusion bag
500 mg / 100 mL
N/A See presentation column
20 minutes
moxifloxacin Infusion bag 400 mg / 250 mL
N/A See presentation column
60 minutes May prolong QT interval and lead to ventricular arrhythmias. May induce seizures in epileptics
piperacillin with tazobactam
Vial 4 g/0.5 g 20 mL WFI 50 mL 30 minutes Penicillin class antibiotic
ticarcillin with clavulanic acid
Vial 3 g/0.1 g 13 mL WFI 50 mL 30 minutes Penicillin class antibiotic
vancomycin Vial 500 mg 10 mL WFI Dilute to maximum concentration of 5mg/mL for peripheral line
Maximum of 10 mg/minute
Infusion related effects are common, decrease infusion rate and monitor closely if these occur
Vial 1 g 20 mL WFI

Sepsis intravenous antibiotic guideline
Adult - Inpatient Page 9 of 9
FURTHER MANAGEMENT
The patient should be reviewed by the Attending Medical Officer within 24 hours of commencing the sepsis pathway and antibiotic therapy, with referral to the infectious diseases and/or clinical microbiology services for specific advice.
Microbiology results are generally available within 48-72 hours, and should be used to guide further management of the patient. This may include de-escalating or ceasing antimicrobial therapy.
Clinicians that are experiencing difficulty in assessing positive or negative microbiology results when rationalising antibiotic therapy at 48-72 hours should contact the designated infectious diseases and/or clinical microbiology services.
Check local instructions regarding referral
References
1. Antibiotic Expert Group. Therapeutic Guidelines: Antibiotic. Version 14. Melbourne: Therapeutic Guidelines Limited; 2010. Accessed through eTG complete (via CIAP).
2. Burridge N (ed). Australian Injectable Drugs Handbook (4th ed). The Society of Hospital Pharmacists Australia; 2008.
3. Rossi S (ed). Australian Medicines Handbook. Chapter 5. Adelaide: Australian Medicines Handbook

ISBAR TOOL
I
Introduction State:
• Your name • Your role/position in the hospital • The ward/unit and hospital/health service you are calling from • I am calling about my patient.....identify the patient (e.g. name, MRN, DOB)
NB: Patients 65+ years of age are at greater risk of sepsis
S Situation
I am concerned they are deteriorating because... • Detail the clinical problem that is prompting the call - I think this patient is septic • The patient is stable/unstable
B
Background • Symptoms - state if symptoms meets the sepsis pathway • Vital signs including any trends • Medical history pertinent to the reason for calling
o Patients who are immune compromised and have a chronic illness are at greater risk of sepsis
o If recently taken or currently on antibiotics • Any initial treatment you have commenced, including whether or not it has worked. Sepsis bundle
commenced oxygen, blood cultures, lactate, IV fluids, antibiotics (if given)
A
Assessment • What do you think the problem is? • Are there any risks you have identified? Any risk factors of sepsis • Clinical signs that support your diagnosis or impression. State if symptoms meets the sepsis
pathway. • Any tests or procedures you think need to be done and blood results including lactate. • Any test(s)/scan(s) results you are waiting for
R
Recommendation Be clear about what you would like to happen, what you want the person you are calling to do and who is responsible for these actions e.g. Urgent review, transfer to another facility or advise on treatment
• I need you to come to review the patient • I need you to authorise transfer of the patient • I need you to authorise the test/scan • I need you to follow up on • I would like some guidance on
• further management of the patient • antibiotic prescribing • further tests or considerations
• I think that this patient would be better managed in a higher level of care

ESCALATION TRIGGERS
FOR CALLING AN AMO FOR PATIENTS WITH SEPSIS
Esc
alat
ion
trigg
ers
Rapid Response call
- including serum lactate > 4mmol/L (adults)
- serum lactate > 2mmol/L is a concern in paediatric patients
3 Clinical Review Calls in an eight hour timeframe
3 simultaneous Yellow Zone criteria in a paediatric patient
Persisting hypotension (SBP less than 90mmHg)
High level of clinician concern
Serious concern by any patient/family member
Significant deterioration in condition and/or admission to ICU
Patient is immunocompromised
Patient with complex antibiotic prescribing requirements
Con
side
ratio
ns fo
r esc
alat
ion
to
ID /
mic
ro s
peci
alis
t
Unfamiliarity with the dosing, efficacy, toxicity, and spectrum of activity of
rarely used and/or newer generation drugs (e.g., meropenem, daptomycin,
linezolid, tigecycline, colistin, amikacin, caspofungin, cefepime)
Patient has had a recent infection with a resistant organism
Pre-existing antibiotics, recent or current antibiotic therapy
Any contradictions to specific antimicrobial therapy
Multiple possible sources of infection
Acute renal failure
Recent travel overseas or to a tropical location
Difficulty in assessing positive or negative microbiology results when
rationalising therapy at 48-72 hours.
Recent candidiasis
The triggers and considerations are suggested as a guide for staff, and can be adapted to suit local facility and LHD requirements.

SEPSIS TROLLEY/PACK
CONTENT LIST
Item Detail Sepsis pathway
Antibiotic guideline
Sepsis 48 hour guideline
Data collection form
Personal protective equipment
Venepuncture / cannulation equipment
Antibiotic vials as per local guidelines
IV resuscitation fluid
Giving sets (including blood pump set)
Blood culture bottles
Pathology tubes
Pathology forms
Syringes

EDUCATION
Sepsis video (available from CEC website)
Sepsis program general presentation (available from CEC website)
Sepsis clinical presentation – adults (available from CEC website)
Sepsis clinical presentation – paediatrics (available from CEC website))
Sepsis multiple choice questions (Toolkit and available from CEC website)
Sepsis multiple choice answers (Toolkit and available from CEC website)

SEPSIS KILLS PROGRAM
MULTIPLE CHOICE QUESTIONS Q1. What is sepsis?
A) Any infection
B) An infection plus hypotension
C) An infection plus systemic inflammatory response syndrome
D) Someone who is on antibiotics
Q2. Which signs and symptoms are most common in adult patients with severe sepsis?
A) Fever > 38deg C
B) Tachycardia
C) Tachypnoea
D) Metabolic acidosis
E) Acute oliguria
Q3. Which of the following criteria present and new in your patient should prompt commencement
of the Sepsis Pathway?
A) RR - 20 breaths/min
B) RR - 20 breaths/min + HR > 122bpm
C) RR > 25 breaths/min + HR > 120bpm + recent surgery
Q4. Patients with severe sepsis and a lactate level ≥ 4 mmol/L have an increased likelihood of
mortality compared to patients with a normal lactate.
A) True
B) False
Q5. In patients with sepsis, which of the following statements is incorrect?
A) Antibiotics should never be delayed while waiting for the results of investigations.
B) Patients with febrile neutropenia should be managed using the local febrile neutropenia guideline
C) Time to first dose antibiotics does not influence outcome
D) The patient should be reviewed by the attending medical officer within 24 hours of starting on sepsis pathway
and antibiotic therapy, with referral to the infectious diseases / clinical microbiology service for specific advice.

Q6. Which signs and symptoms are most common in children and infants with sepsis?
A) Fever >38deg C
B) Persistent Tachycardia
C) Lethargy
D) Metabolic acidosis
E) Lactate >4mmol/L
Q7. During the monitor and reassess phase of resuscitation of the septic child or infant, which of
the following signs of deterioration indicates your patient requires escalation in level of care?
A) Persistent tachycardia, slow capillary refill and hypotension
B) Drowsiness or abnormal LOC and /or urine output<1ml/kg/hr
C) Acidosis, increasing serum lactate or procalcitonin
D) Hypoglycaemia, leukopenia or abnormal coagulation
E) Any of the above
Q8. BP is a reliable parameter in the early recognition of sepsis in paediatric patients
A) True
B) False
Q9. Fluid resuscitation in paediatric sepsis should be given as:
A) 10ml/kg 0.9% sodium chloride over 20minutes
B) 20ml/kg bolus of 0.9% sodium chloride over no more than 10minutes
C) 20ml/kg bolus of 0.9% sodium chloride over 60 minutes
D) 10ml/kg 0.9% sodium chloride over 10minutes
Q10. Key messages are: SEPSIS KILLS & TIME IS LIFE. Fill in the boxes:
risk factors, signs, symptoms of sepsis and have early involvement of senior clinicians
with rapid IV fluids)and administer antibiotics within one hour
to appropriate in hospital teams or retrieval

SEPSIS KILLS PROGRAM
MULTIPLE CHOICE QUESTIONS AND ANSWERS
Q1. What is sepsis?
A) Any infection B) An infection plus hypotension C) An infection plus systemic inflammatory response syndrome D) Someone who is on antibiotics
Answer – C Sepsis occurs when an infection, beginning in any tissue in the body, results in the systemic inflammatory response syndrome (SIRS). The SIRS criteria are heart rate > 90 beats/min, respiratory rate (RR) > 20 breaths/min (or partial pressure of arterial CO2 <32), temperature either > 38°C or < 36°C, and white blood cell count (WBC) either > 12,000 or < 4,000 cells/mm3. For a patient to be diagnosed with sepsis, at least two of the SIRS criteria need to be present with an infection Severe sepsis is defined as sepsis resulting in organ dysfunction. Septic shock occurs when there is sepsis-induced hypotension (where either the systolic blood pressure is < 90 mmHg, 40mmHg below baseline, or the mean arterial pressure (MAP) is < 70mmHg) that persists despite adequate fluid resuscitation Levy MM et al.2001 sccm/esicm/accp/ats/sis international sepsis definitions conference. Intensive Care Conference 2003;29:530-8 Dellinger RP et al. Surviving sepsis campaign: international guidelines for the management of severe sepsis and septic shock, 2012. Intensive Care Med 2013;39:165-228
Q2. Which signs and symptoms are most common in adult patients with severe sepsis?
A) Fever > 38deg C B) Tachycardia C) Tachypnoea D) Metabolic acidosis E) Acute oliguria
Answer – C An increase in respiratory rate is an important early marker of sepsis. Ensure that the clinical observations chart is complete and accurate. In a large prospective cohort study of adult patients with severe sepsis (n=742), 99% had tachypnoea as defined by a respiratory rate >20. Tachycardia occurred in 97%, followed by fever (70%), acute oliguria (54%) and metabolic acidosis (38%). (Brun-Buisson C et al. JAMA 1995)

Q3. Which of the following criteria present and new in your patient should prompt commencement of the Sepsis Pathway?
A) RR - 20 breaths/min B) RR - 20 breaths/min + HR > 122bpm C) RR > 25 breaths/min + HR > 120bpm + recent surgery
Answer - C In NSW any one risk factor, sign or symptom plus 2 Yellow Zone observations or 1 Red Zone observation should prompt obtaining senior clinician review or a Rapid Response call and the consideration of the commencement of the Sepsis Pathway. Sepsis is a medical emergency
Q4. Patients with severe sepsis and a lactate level ≥ 4 mmol/L have an increased likelihood of mortality compared to patients with a normal lactate.
A) True B) False
Answer - True Lactate is a normal product of anaerobic cell metabolism and is released into the blood and metabolised by the liver. Normal lactate levels are less than 1.0 mmol/L in both arterial and venous blood. Elevated serum lactate is strongly associated with morbidity and mortality in critically ill patients. One study showed a level above 4.0 mmol/L was associated with a 27% mortality rate compared with 7% for patients with a lactate of 2.5-4.0mmol/L
(Boschert S. Is it Septic Shock? Check Lactate Level ACEP News 2007) Elevated lactate is typically present in patients with severe sepsis or septic shock and can occur even before patients have a marked acidosis or low blood pressure. Cryptic shock is defined as a serum lactate greater than 4 mmol/L and normotensive. It is therefore important to screen for serum lactate in all patients who are suspected of sepsis irrespective of a normal blood pressure. Elevated lactate is a late sign of sepsis in children. Where lactate is greater than 2mmol/L and sepsis is suspected, it is recommended that immediate treatment is started.
Q5. In patients with sepsis, which of the following statements is incorrect?
A) Antibiotics should never be delayed while waiting for the results of investigations. B) Patients with febrile neutropenia should be managed using the local febrile neutropenia guideline C) Time to first dose antibiotics does not influence outcome D) The patient should be reviewed by the attending medical officer within 24 hours of starting on sepsis pathway
and antibiotic therapy, with referral to the infectious diseases / clinical microbiology service for specific advice.
Answer - C Intravenous antibiotic therapy should be started immediately after obtaining appropriate cultures, since early initiation of antibiotic therapy is associated with lower mortality. The choice of antibiotics should also be guided by the patient's history including recent antibiotic exposure, comorbidities, clinical context (eg, community- or hospital-acquired infection), Gram-stain data and previous resistant bacterial isolates.

Poor outcomes are associated with inadequate or inappropriate antibiotic selection as well as delays in starting antibiotic therapy. A retrospective cohort study of 2,154 patients with septic shock found that each hour of delay in antibiotic administration over the first 6 hours was associated with an average decrease in survival of 7.6%. Therefore statement C is INCORRECT, time to first dose antibiotics DOES significantly influence outcome. (Kumar A, Crit Care Med. 2006)
Q6. Which signs and symptoms are most common in children and infants with sepsis?
A) Fever >38deg C B) Persistent Tachycardia C) Lethargy D) Metabolic acidosis E) Lactate >4mmol/L
Answer - B Persistent tachycardia is a reliable sign in the early recognition of sepsis in children and infants. More specifically persistent tachycardia that is resistant to treatment such as fluid bolus or antipyretics. Not all children with sepsis will have a fever and administering antipyretics pre hospital can mask a high temperature particularly at triage and is therefore not a reliable sign or symptom of sepsis. Children can often compensate very well and relying solely on a patient’s pH again is not a reliable indicator of sepsis in children. Children and infants do not always respond to sepsis in the same way that adults do regarding an elevated lactate. It is therefore important to have a heightened level of concern with a lactate over 2mmol/L with this group.
Q7. During the monitor and reassess phase of resuscitation of the septic child or infant, which of the following signs of deterioration indicates your patient requires escalation in level of care?
A) Persistent tachycardia, slow capillary refill and hypotension B) Drowsiness or abnormal LOC and /or urine output<1ml/kg/hr C) Acidosis, increasing serum lactate or procalcitonin D) Hypoglycaemia, leukopenia or abnormal coagulation E) Any of the above
Answer - E These are all signs suggesting your patient has severe sepsis or septic shock and has not adequately responded to treatment. This patient will require escalation in level of care and may need transfer to a paediatric Intensive Care Unit.
Q8. BP is a reliable parameter in the early recognition of sepsis in paediatric patients
A) True B) False
Answer- False Children are able to maintain their BP despite significant compromise. They can prevent a reduction in their BP by vasoconstriction and increasing their heart rate. Neonates unlike adults cannot change their stroke volume so they increase their heart rate to improve cardiac output. This persistent tachycardia is a valuable sign in identifying sepsis.

Q9. Fluid resuscitation in paediatric sepsis should be given as:
A) 10ml/kg 0.9% sodium chloride over 20minutes B) 20ml/kg bolus of 0.9% sodium chloride over no more than 10minutes C) 20ml/kg bolus of 0.9% sodium chloride over 60 minutes D) 10ml/kg 0.9% sodium chloride over 10minutes
Answer - B Fluid resuscitation should be given as a push of 20ml/kg 0.9% sodium chloride over no more than 10 minutes. Q10. Key messages are: SEPSIS KILLS & TIME IS LIFE. Fill in the boxes:
risk factors, signs, symptoms of sepsis and have early involvement of senior clinicians with rapid IV fluids (20ml/kg 0.9% sodium chloride) and administer antibiotics within one hour
to appropriate in hospital teams or retrieval
Answer RECOGNISE RESUSCITATE, REFER

EVALUATION
Audit tools
Sepsis database and data entry instructions

SEPSIS DATA COLLECTION TOOL ADULT INPATIENT
Service Type
� Critical Care � Medical � Surgical � Oncology / Haematology
� Paediatric � Aged Care � Rehabilitation � Maternity � Other
Time of recognition of sepsis CERS call time / other recognition eg ward round, handover
Rapid Response � Clinical Review � Other � ……………………………………………
Time: ��:�� Date: ��/��/����
Systolic blood pressure ���mmHg
Oxygen administered � YES � NO � Not required Lactate � YES � NO Level ��.�mmol/L Blood cultures One or more sets collected � YES � NO
IV resuscitation fluids* Administered within 60 minutes of CERS call / sepsis recognition. Only record for patients with SBP < 90mmHg and/or lactate > 4mmol/L
� Not given � 250-500 mL
� 500-1000 mL � > 1000 mL
IV antibiotics * Administered within 60 minutes of CERS / sepsis recognition) Do not delay for investigations or results
First IV antibiotic commenced for sepsis:
Time: ��:�� Date: ��/��/����
Transfer of care Use Ward if patient remaining in original ward or transferred to another ward
� Ward
� Other hospital
� HDU / ICU
� Tertiary referral hospital
Comments
Signature ………………………………….. Designation …………………………………………… *Mandatory Field – MRN, DOB, Lactate, IV resuscitation fluids, IV antibiotics
THIS IS NOT A MEDICAL RECORD FORM
FACILITY ………………………………………… WARD ………………........................... For analysis purposes each facility will be able to sort for their own wards

COMPLETING THE DATA COLLECTION TOOL ADULT INPATIENT
1. All dates are in dd/mm/yyyy format
2. All times are in hh:mm 24 hour clock format
3. The MRN is a MANDATORY field and cannot be modified once entered into the database.
4. The facility code originates from NSW Health and is automatically generated with your login
5. The ward code is a free text field and is for the name of the ward. Therefore for analysis of data, each facility will be able to sort on the field and monitor the progress of their own ward.
6. The service type field is used to describe the type of ward eg surgical or medical etc
7. The time and date of time of recognition of sepsis (this is the CERS call time or other method of recognition) is recorded to most accurately reflect how long it takes from time of recognition to the time of administration of the first antibiotic.
8. The Rapid Response / Clinical Review and Other boxes are to be ticked depending the call.
9. The systolic blood pressure field is the reading taken at the time of the CERS call being made / time of sepsis recognition
10. Oxygen administered is recorded as a ‘yes’ or ‘no’ if oxygen is ordered or ‘not required’ if the patient does not need oxygen.
11. Lactate is a MANDATORY field. Lactate is recorded as a ‘yes’ or ‘no’ depending on whether a level is collected. If ‘yes’ the level result is then recorded.
12. Intravenous resuscitation fluids administered if the patient has a systolic blood pressure of
< 90mmHg and/or lactate > 4mmol/L at time of CERS call / sepsis recognition. Record as not given or the amount of bolus fluid given within 60 minutes of the CERS call.
13. The first intravenous (IV) antibiotic time and date is a MANDATORY field. Do not collect or enter
data for patients who do not have intravenous antibiotics.
14. The transfer of care field is for where the patient was managed or was transferred to as a result of the CERS Call
15. Please use the comments box to record information which may assist in the data analysis. This
includes explanations of blank fields, delays in treatment etc. Do not use the comments box as a medication prescribing or pathology record, or a medical record.
16. The signature and designation boxes are to record the name of the person completing the form.

SEPSIS DATA COLLECTION TOOL PAEDIATRIC INPATIENT
Time of recognition of sepsis CERS call time / other recognition eg ward round, handover
Rapid Response � Clinical Review �
Other � ………………………………………………
Time: ��:��
Date: ��/��/����
Lactate*
� YES � NO Level��.�mmol/L
IV resuscitation fluid bolus* Administered within 60 minutes of CERS call � Not given � 10 mL/kg � 20 mL/kg
IV antibiotics * Administered within 60 minutes Do not delay for investigations or results
First IV antibiotic commenced for sepsis:
Time: ��:��
Date: ��/��/����
Transfer of care Use Ward if patient remaining in original ward or transferred to another ward
� Ward � ICU/HDU
� Other hospital � Tertiary referral hospital
Comments
Signature ……………………………………..
Designation …………………………………….
*Mandatory Field – MRN, DOB, Lactate, IV resuscitation fluids, IV antibiotics
THIS IS NOT A MEDICAL RECORD FORM
FACILITY ………………………………………… WARD ………………............................. For analysis purposes each facility will be able to sort for their own wards

COMPLETING THE DATA COLLECTION TOOL PAEDIATRIC INPATIENT
1. All dates are in dd/mm/yyyy format
2. All times are in hh:mm 24 hour clock format
3. The MRN is a MANDATORY field and cannot be modified once entered on the database
4. The facility code originates from NSW Health and is automatically generated with your login
5. The ward code is a free text field and is for the name of the ward. Therefore for analysis of data, each facility will be able to sort on the field and monitor the progress of their own ward
6. The time and date of time of recognition of sepsis (this is the CERS call time or other method of recognition) is recorded to most accurately reflect how long it takes from time of recognition to the time of administration of the first antibiotic
7. The Rapid Response / Clinical Review and Other boxes are to be ticked depending the call
8. Lactate is a MANDATORY field. Lactate is recorded as a ‘yes’ or ‘no’ depending on whether a level is collected. If ‘yes’ the level result is then recorded
9. Intravenous resuscitation fluid bolus administered within 60 minutes of the CERS call. Record as not given or the amount of fluid bolus given in mL/kg
10. The first intravenous (IV) antibiotic time and date is a MANDATORY field. Do not collect or enter
data for patients who do not have intravenous antibiotics
11. The transfer of care field is for where the patient was managed or was transferred to as a result of the CERS Call
12. Please use the comments box to record information which may assist in the data analysis. This
includes explanations of blank fields, delays in treatment etc. Do not use the comments box as a medication prescribing or pathology record, or a medical record
13. The signature and designation boxes are to record the name of the person completing the form.

SEPSIS DATABASE AND DATA ENTRY INSTRUCTIONS
Step Field Name Issue Solution 1. MRN Cannot delete or change
MRN once record has been generated Using the tab key to move from MRN to DOB wipes out the rest of the data entered
Delete record, then re-enter The MRN field has additional conditions attached to avoid entering duplicate records. You must mouse click - NOT Tab - into the next field from the MRN to allow the duplicate function to be performed
2. Date and time • Date of birth • Time of recognition • IV Antibiotic
Errors in entering date and time
Ensure you enter the date and time in the correct order There are two ways to enter this data: 1. Mouse click into the top area and type the numbers in 2. Use the calendar. Note: you must enter the date before
the time or the date of entry will default into the field Always check the automatically generated time calculation to ensure accuracy of entry
3. Ward No specific list Use the name the ward is usually called
4. Service Type Specific services are not identified in this database
Use the service type that best describes your service or your patient group eg medical, surgical etc Note: all users within your facility can see all data entered by the facility.
5. Time of recognition of sepsis
Variance in time recording
This is the time that either a CERS call is made to escalate care of the patient, or another method of recognition i.e. patient reviewed on a ward round and care escalated after sepsis suspected
6. SBP (Adults only)
Significant indicator of sepsis in adults
Particularly important in adult patients This is a MANDATORY FIELD
7. Oxygen administered (Adults only)
A component of the sepsis care bundle
Not all patients will require administration of oxygen

8. Lactate Significant indicator of sepsis
This is a MANDATORY FIELD
9. Blood cultures (Adults only)
A component of the sepsis care bundle
Record Yes or No depending whether blood cultures are collected.
10. Administration of IV resuscitation fluid
Patient meets the sepsis criteria for CERS call but IV resuscitation fluids are not prescribed / administered
Record as ‘not given’ if resuscitation fluid bolus not administered
11. Administration of IV antibiotics
Patient meets the sepsis criteria for CERS call but the IV antibiotics are not prescribed
If patient has not been given IV antibiotics do not record in database. Note: if the patient has no intravenous (IV) access, and intramuscular (IM) or intraosseous (IO) antibiotics are given instead:
• Record time and date in this field • Record route of administration and reason in the
comments section
12. Transfer of care Ward indicates the patient did not move treatment location as a result of sepsis recognition eg patient on ward stays on ward after sepsis recognition or patient in critical care that remains in critical care after sepsis recognition.
13. Comments Best use of this field This field is not meant to be a medical record Enter concise information that adds value to your data including:
• explanation of missing data • hospital transfers to avoid double entries by two facilities • more information as thought necessary • specific information to identify a subset of your data for
further analysis Use commas and spaces to separate data. Do not use enter key – difficult to read entry in excel spreadsheet

This page has been left intentionally blank