Induced pluripotent stem cell-derived hepatocytes and endothelial cells in multi-component hydrogel...
Transcript of Induced pluripotent stem cell-derived hepatocytes and endothelial cells in multi-component hydrogel...

lable at ScienceDirect
Biomaterials xxx (2014) 1e9
Contents lists avai
Biomaterials
journal homepage: www.elsevier .com/locate/biomater ia ls
Induced pluripotent stem cell-derived hepatocytes and endothelialcells in multi-component hydrogel fibers for liver tissue engineering
Chan Du, Karthikeyan Narayanan*, Meng Fatt Leong, Andrew C.A. Wan*
Institute of Bioengineering and Nanotechnology, 31 Biopolis Way, The Nanos 138669, Singapore
a r t i c l e i n f o
Article history:Received 12 March 2014Accepted 7 April 2014Available online xxx
Keywords:Multi-component fibersLiver tissue engineeringVascularizationInduced pluripotent stem celldifferentiationHepatocyteEndothelial cell
* Corresponding authors. Tel.: þ65 6824 7134; fax:E-mail addresses: [email protected] (
star.edu.sg (A.C.A. Wan).
http://dx.doi.org/10.1016/j.biomaterials.2014.04.0110142-9612/� 2014 Elsevier Ltd. All rights reserved.
Please cite this article in press as: Du C, ethydrogel fibers for liver tissue engineering,
a b s t r a c t
Liver tissue engineering requires a suitable cell source, methodologies to assemble the cells withintheir niche microenvironments in a spatially defined manner, and vascularization of the constructin vivo for maintenance of hepatocyte viability and function. Recently, we have developed methods ofencapsulating cells within separate domains in multi-component hydrogel fibers and methods ofassembling fibers to form 3D-patterned tissue constructs. In the present work, we have combinedthese approaches to encapsulate hepatocytes and endothelial cells within their specific niches, and toassemble them into endothelialized liver tissue constructs. The hepatocytes and endothelial cells wereobtained in parallel by differentiating human recombinant protein-induced human pluripotent stemcells, resulting in a construct which contained genetically identical endothelial and parenchymal el-ements. We were able to demonstrate that the presence of endothelial cells in the scaffold signifi-cantly improved hepatocyte function in vitro and facilitated vascularization of the scaffold whenimplanted in a mouse partial hepatectomy model. The in vivo studies further asserted that integrationof the scaffold with host vasculature had occurred, as demonstrated by the presence of human al-bumin in the mouse serum.
� 2014 Elsevier Ltd. All rights reserved.
1. Introduction
There is a high demand for liver transplantation treatment dueto its success; however, the scarcity of donor organs means that itcannot be available for every patient. Hepatocyte transplantation isan alternative method that holds great promise for the treatment ofliver disease, where the transplanted cells reduce the load on theexisting host cells and help in the recovery or regeneration of thehost liver.
Many approaches have been studied for the rescue of liverfailure such as extracorporeal devices (reviewed in Refs. [1,2]) andcell-based therapies [3,4]. Cell-based therapies have a great po-tential to treat acute and chronic liver failure and the cell source forthe therapies could be from adult stem cells or pluripotent stemcells. Mesenchymal stem cells from bone marrow and umbilicalcord blood [5], as well as human embryonic stem cells [6e8] havebeen successfully differentiated into functional hepatocytes.Induced pluripotent stem cells (iPSCs) generated by
þ65 6478 9081.K. Narayanan), [email protected]
al., Induced pluripotent stemBiomaterials (2014), http://dx
reprogramming fibroblasts [9] have been postulated to be anexcellent cell source for liver tissue engineering [10] and have beendifferentiated to hepatocytes by several groups [11e13].
In addition to the issue of cell source, delivery of hepatocytes tothe liver requires the appropriate vehicle and form. One of thesystems that has gained attention is the implantable tissue engi-neered liver construct. Hepatocytes have a self-assembling prop-erty that helps them to form spheroids. The formation of spheroidson low-attachment surfaces and on Matrigel enhanced the func-tional characteristics of the hepatocytes when compared to 2Dcollagen surface [14e18]. Similarly, hepatocyte spheroids culturedin 3D biomaterial constructs showed better functionality than cellsgrown on 2D substrate [19e24]. Encapsulation of hepatocytes inalginate [20,21], methylated collagen [22,23] or synthetic materials[24] formed spheroids with improved cellecell interactions andhepatocyte functions. Thus, hepatocytes were encapsulated in thepermissive matrix of polyelectrolyte complex hydrogel fibers in thepresent work, to allow them to self assemble into 3D structures fortheir optimal function.
The liver contains several cell types, the majority being hepa-tocytes and endothelial cells. Co-cultures of hepatocytes with non-parenchymal cells have been reported to improve hepatocytefunction by means of reciprocal signaling interactions between the
cell-derived hepatocytes and endothelial cells in multi-component.doi.org/10.1016/j.biomaterials.2014.04.011

Table 1List of antibodies and PCR assays used in the study.
(A) List of antibodies
Antibody Source
Sox17 R&D Systems, MN, USAGATA4 Abcam, Cambridge, UKFOXA2 Abcam, Cambridge, UKE-CAD Abcam, Cambridge, UKAFP Abcam, Cambridge, UKALB Sigma-Aldrich, MO, USAvWF Abcam, Cambridge, UKCD-31 Abcam, Cambridge, UK
(B) List of Taqman assays
Gene Assay#
GAPDH Hs99999905-M1GATA4 Hs00171403-m1SOX17 Hs00751752-s1HNF4a Hs00604435-m1ALB Hs00910225-m1V-ECAD Hs00901463-m1PECAM-1 Hs00169777-m1
C. Du et al. / Biomaterials xxx (2014) 1e92
two cell types [25e28]. The effectiveness of these interactionsrelied on spatial patterning of the cells with respect to each other[26]. Based on our earlier work with interfacial polyelectrolytecomplex (IPC) fiber scaffolds, where fibers are drawn from theinterface between two oppositely charged polyelectrolytes [29,30],we recently established proof-of-concept for co-culture of cellswithin multi-interfacial polyelectrolyte complex (MIPC) fibers[31,32]. MIPC fibers are drawn from two or more interfaces,resulting in segregated domains within single fibers. In the currentwork, these multi-component fibers allowed us to spatially definehepatocytes and endothelial in separate compartments, with theobjective of reproducing the ideal 3D microenvironment for theirreciprocal interactions.
We first differentiated human iPSCs to hepatocytes and endo-thelial cells, by adapting the existing differentiation strategies[5,8,12,13,33e37]. These differentiated cells were encapsulated infibers drawn by interfacial polyelectrolyte complexation (IPC) thatwere subsequently assembled to form tissue-like constructs. Wethen characterized the performance of these constructs, in terms ofhepatocyte function and integration with host tissue, in a mousepartial hepatectomy model.
2. Materials and methods
2.1. iPSCs culture
iPSCs used in this report were generated by reprogramming human foreskinfibroblasts with recombinant proteins as described earlier [38]. hESC-qualifiedMatrigel (BD Biosciences, NJ, USA) was used as the substrate for the maintenanceof the iPSCs culture.
2.2. Differentiation of human iPSCs to hepatic cells
Hepatocyte differentiation was carried out according to the three-stageprotocol reported by Takata et al. [39], with slight modifications. iPSCs wereseeded at 70e80% confluence and were cultured in serum-free RPMI 1640 me-dium (Invitrogen, CA, USA) supplemented with B-27 (Invitrogen, CA, USA) andrh-activin-A (100 ng/mL) (R&D systems, MN, USA) for 3 days. Subsequently,differentiated mesendodermal cells were treated with HGF (20 ng/mL) (R&Dsystems, MN, USA) for 5 days to generate hepatic cells. To achieve final hepaticcell maturation, cells were cultured for 5 days in hepatocyte culture medium(HCM; Lonza, Walkersville, MD) supplemented with oncostatin M (10 ng/mL)(OSM; R&D systems, MN, USA). Cells were maintained in HCM with no oncostatinM after hepatic cell maturation.
2.3. Differentiation of human iPSCs to endothelial cells
We designed a two-step protocol to differentiate the stem cells into endo-thelial cells. The first stage involved differentiation of the stem cells to themesodermal lineage. In the second stage, the mesodermal cells were differenti-ated into endothelial cells. During the first stage, iPSCs were cultured for 7 dayswith RPMI 1640 media supplemented with insulinetransferrineselenium A (1%v/v) (Invitrogen, CA, USA), non-essential amino acids (0.1 mM) (Invitrogen, CA,USA), L-glutamine (2 mM) (Invitrogen, CA, USA), 2-mercaptoethanol (0.1 mM)(Invitrogen, CA, USA), penicillin and streptomycin (each 100 U/mL) (Invitrogen,CA, USA), rh-activin-A (100 ng/ml), rh-BMP-4 (25 ng/ml) (R&D systems, MN,USA), rh-bFGF (4 ng/ml) (R&D systems, MN, USA), rm-Wnt-3a (50 ng/ml) (R&Dsystems, MN, USA) and 10 mM SB431542 (Tocris Bioscience, MO, USA). Themesodermal cells were further differentiated to endothelial cells for 7 days withEndoGro media (Millipore, MA, USA). The EndoGro media contains rh-VEGF(5 ng/ml) and rh-FGF (5 ng/ml). We supplemented the second stage of differ-entiation with VEGF (50 ng/ml) (Millipore, MA, USA) and rh-bFGF (10 ng/ml)(R&D systems, MN, USA). The differentiated cells were maintained with EndoGromedia without excess VEGF and FGF. Human umbilical vascular endothelial cells(HUVEC) were obtained from ATCC (CRL-1730).
2.4. Encapsulation of cells in multi-component hydrogel fibers
Water soluble chitin (WSC), prepared from crab chitin (SigmaeAldrich), andsodium alginate (SigmaeAldrich) were used at a concentration of 10 mg/ml aspolycation and polyanion, respectively. WSC containing galactose (WSC-Gal) andcollagen (WSC-Col) were used to provide niche microenvironments for the hepa-tocytes and endothelial cells respectively (see Supplementary Information forpreparation of WSC-Gal and WSC-Col).
The hydrogel was formed by assembly of polyelectrolyte fibers as describedpreviously [40]. Each polyelectrolyte fiber, formed by multi-interfacial poly-electrolyte complexation (MIPC) [31], consisted of four separate domains.
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://d
Differentiated hepatocytes and endothelial cells were suspended in WSC-Gal andWSC-Col solutions at a density of 1 � 104 cells/ml, respectively. The solutions weredispensed in the layout of WSC-Col solution flanked by two 20 ml droplets of sodiumalginate solution, which were in turn flanked by two 20 ml droplets of WSC-Galsolution on the outside. Each polyelectrolyte droplet was brought to meet its adja-cent droplets, creating four interfaces which were fused to create a nascent poly-electrolyte fiber with four domains. Consequently, this led to the formation of a fiberwith endothelial cells in the two center domains, flanked by hepatocytes in the outerdomains. Multiple polyelectrolyte fibers were drawn simultaneously, fused andspooled to make a hydrogel. The resulting hydrogel was fused further by immersingsequentially in 0.5% WSC in PBS, 0.5% alginate in PBS, and the process was repeated.Finally, the fused hydrogel was removed from the spooling device and transferred tothe culture medium. For single culture control, WSC-Col solution was used withoutthe endothelial cells.
2.5. Immunostaining
Cells grown on coverslips were fixed with 4% paraformaldehyde for 15 min. Thecells were permeabilized with PBS containing 0.1% triton X-100 (SigmaeAldrich,MO, USA) for 10 min and used as described earlier [41]. Suitable secondary anti-bodies conjugated with a fluorophore were used and the samples were visualizedunder a fluorescence microscope.
Mice liver slices containing the implanted cell/scaffold constructs were fixedwith 4% paraformaldehyde solution overnight at 4 �C, dehydrated sequentially in15% (w/v) sucrose solution in PBS overnight, followed by 30% sucrose in PBS over-night, embedded in Tissue-Tek Optimal Cutting Temperature (O.C.T.) compound(Sakura, The Netherlands) and cryosectioned. Liver sections were immunostainedwith specific antibodies as described earlier [41]. The list of antibodies used in thestudy is given in Table 1A.
2.6. RNA extraction, reverse transcription, polymerase chain reaction (PCR) and real-time PCR
Total RNA from the cells were extracted using RNeasy Mini Kit (Qiagen, CA, USA)or with TRIZOL reagent (Invitrogen, CA, USA). The RNA concentration was deter-mined using NanoDrop 2000 (Thermo Scientific, MA, USA). For real-time PCR,Taqman assays (Life Technologies, NY, USA) were used, as listed in Table 1B.
2.7. Flow cytometry
Flow cytometry was carried out as described earlier [41]. Briefly, a suspension ofsingle cells was fixed with formaldehyde and permeabilized with PBS containing0.1% Triton X-100. The specific antibodies used for flow cytometry are listed in thetable. The stained cells were analyzed in a BD LSRII flow cytometry analyzer at theBiopolis Shared Facility, Singapore.
2.8. Human albumin ELISA
The concentration of albumin secreted into the media was assayed using thehuman albumin enzyme linked immunosorbent assay (ELISA) kit. The assay wascarried out as described in the manufacturer’s instructions (Cygnus Technologies,NC, USA). Assays were performed on samples obtained from three independentcultures and were performed in duplicate. A standard curve was prepared for thedetermination of the albumin concentration in the samples.
cell-derived hepatocytes and endothelial cells in multi-componentx.doi.org/10.1016/j.biomaterials.2014.04.011

Day 0 3 8 13
iPSCs Mesendoderm Hepatic Iineage Hepatic cells(Stage-I) (Stage-II) (Stage-III)
Activin A HGF OSM
E-Cad/HNF4a ALB/DAPI E-Cad/ALB
300
200
100
0
Fold
cha
nge
Stage-I Stage-II Stage-III Stage-I Stage-II Stage-III Stage-I Stage-II Stage-III Stage-I Stage-II Stage-III
12
8
4
0
8
6
3
0
15
10
5
0
GATA 4 SOX17 HNF4ɑ Albumin
Stage-IIStage-III
AFP ALB E-CAD
E-CADStage-I
SOX17 GATA4 FOXa235.1 ± 2.7% 28.4 ± 2.7%
28 ± 2.7% 30.9 ± 2.7%
26 ± 2.5%
23.8 ± 2.7%
43.1 ± 2.6% 47.7 ± 2.5%
24.1 ± 2.7% 31.8 ± 2.8%
40
30
20
10
0Alb
umin
/DN
A (n
g/ng
)
Stage-I Stage-II Stage-III
A
B
C
D E
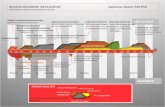
Fig. 1. Differentiation of iPSCs to hepatocytes. A three-stage differentiation protocol was adopted as described in the methods, and illustrated in scheme (A). Immunostaining of thedifferentiated cells derived from Stage III was performed with antibodies against E-Cad, HNF4-a (HNF4a) and human albumin (ALB) (B). Gene expression analysis was done on theRNA obtained from different stages of differentiation. Real-time PCR was carried out with gene specific Taqman assays (C). The fold changes were calculated with the expressionlevels in the undifferentiated iPSCs as control. Flow cytometry was done to identify the percentage of differentiated cells at different stages of differentiation (D). Albumin secretedby the differentiated cells into the media was measured using specific antibody against human albumin. The amount of albumin was calculated with the help of a standard curve.The amount of the albumin secreted was normalized against the total DNA (E). Scale bar in (B) ¼ 50 mm.
C. Du et al. / Biomaterials xxx (2014) 1e9 3
2.9. In vivo implantation of scaffolds
Animal experiments reported in this manuscript conformed to the guidelinesof the National Advisory Committee on Laboratory Animal Research (NACLAR)and were approved by the Institutional Animal Care and Use Committee (IACUC).The mice were anesthetized and underwent 70% partial hepatectomy. Cell-loaded scaffold constructs were implanted into livers of partially hepatecto-mized SCID mice. The mice were sacrificed 2 weeks and 4 weeks after implan-tation, and sites containing the cell-scaffold constructs were excised forcharacterization. Serum samples from these animals were also collected foranalysis.
2.10. Dot-blot of serum samples
5 ml of the serum samples was spotted onto a nitrocellulose membrane (Bio-Rad,CA, USA) and allowed to air-dry. For the positive control, human reference serum(Bethyl Laboratories Inc., TX, USA) containing w9.0 mg/mL albumin was used. Themembranewas treatedwith 5% (w/v) skimmilk (SigmaeAldrich, MO, USA) in TBS for1 h at room temperature followed by incubation with the primary antibody. Horse-radishperoxidase conjugated secondary antibodyandECL based chemiluminescencesystem (GE Lifesciences, PA, USA) was used to detect the samples. Images of themembrane were obtained using a ChemiDoc MP system (Bio-Rad, CA, USA).
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://dx
3. Results
3.1. Strategy
We took advantage of the availability of human iPSCs developedusing a non-viral and non-genetic method [38], and differentiatedthem to hepatocytes for use in our study. Parallel experiments wereconducted to differentiate these same iPSCs into endothelial cells.We utilized MIPC fibers to encapsulate the differentiated hepato-cytes and endothelial cells in individual fibers as illustrated in Fig. 3.MIPC fibers allowed co-patterning of the differentiated hepatocytesand endothelial cells in their niche microenvironments, for whichwe incorporated galactose and collagen type I, respectively. At thesame time, we could ensure that the differentiated hepatocyteswere in close proximity to the endothelial cells, and that this closeassociation was uniformly repeated within the 3D hydrogel.Consequently, we anticipated that co-patterning would lead to animproved, functional liver tissue construct as (i) non-parenchymal
cell-derived hepatocytes and endothelial cells in multi-component.doi.org/10.1016/j.biomaterials.2014.04.011

Day 0
iPSCs Mesoderm Endothelial cells
7 13
(Stage-1) (Stage-2)
BMP4 VEGF
CD-31/DAPI V-ECAD/DAPI
18
12
6
0
Fold
cha
nge
V-ECAD
Stage-1 Stage-2 HUVEC Stage-1 Stage-2 HUVEC
300
200
100
0
PECAM-1
400
300
200
100
0
Cel
l cou
nt
400
300
200
100
0
Cel
l cou
nt
vWF+ (96%) CD-31+ (96%)
A
B
C
D E
Fig. 2. Differentiation of iPSCs to endothelial cells. A two-step protocol was developed for the differentiation of iPSCs to endothelial cells as illustrated in the scheme (A). Im-munostaining (B) was carried out for differentiated cells with endothelial specific antibodies such as CD-31 (i) and V-ECAD (ii). DAPI was used to stain the nuclear compartment ofthe cell. Total RNA was isolated from the differentiated cells at different stages of differentiation and real-time PCR was done with gene specific Taqman assays (C). Flow cytometrywith endothelial specific antibodies such as vWF and CD-31 was done on the differentiated cells obtained from step-2 of the differentiation protocol (D). Tubule formation assay onMatrigel was performed to demonstrate the functionality of the differentiated endothelial cells (E). Scale bar in (E) ¼ 200 mm.
C. Du et al. / Biomaterials xxx (2014) 1e94
cells such as endothelial cells have been reported to promote he-patocyte function [25e28], and, (ii) endothelial cells facilitate theformation of vasculature which can anastomose with the host[37,42e44].
3.2. Generation of hepatocytes from iPSCs
We followed a three-stage protocol to induce the differentiationof the human iPSCs to hepatocytes (Fig. 1A). Morphological obser-vation of the cells during differentiation showed that the compactiPS cells became more ‘honeycomb’ shaped at the end of differen-tiation (Supplementary Fig. 1A and B). At Stage I, iPSCs were primedto undergo differentiation towards mesoendoderm in the presenceof Activin-A (100 ng/ml). At Stage II, the cells were further differ-entiated to the hepatic lineage in the presence of HGF (20 ng/ml). AtStage III, mature hepatocytes were derived, upon completing thedifferentiationwith the addition of oncostatinM (10 ng/ml). Cells at
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://d
the end of Stage I were positively stained with antibodies against E-CAD, GATA-4 and FOXA2 (Supplementary Fig. 2), indicating thatthey had differentiated towards the mesendodermal lineage. StageII cells were stained positive with E-CAD and AFP antibodies(Supplementary Fig. 3). Hepatic cells at the end of Stage III werecharacterized by positive immunostaining against E-CAD, HNF-4aand albumin, markers that distinguish hepatic cells (Fig. 1B).Quantitative PCR analysis confirmed the transient expression ofGATA-4 and SOX-17 at Stage I during Activin-A treatment. On theother hand, the expression of hepatic genes such as HNF-4a andalbumin increased progressively during differentiation (Fig. 1C).Next, we estimated the percentage of cells positive for the stagespecific markers by flow cytometry. The numbers indicated inFig. 1D reflects the average percentile of the cells positive for thespecific antigen among three independent experiments. We wereable to achieve 43.1�2.6% and 47.7� 2.5% positive cells for AFP andalbumin respectively. From FACS analysis, 42% of cells were found
cell-derived hepatocytes and endothelial cells in multi-componentx.doi.org/10.1016/j.biomaterials.2014.04.011

Fig. 3. Schematic diagram indicating the fiber drawing process (A). iPSCs were differentiated into hepatocytes and endothelial cells as mentioned earlier. The differentiated cellswere mixed either with chitin (WSC-Gal) for hepatocytes or with chitin (WSC-Col) for endothelial cells and droplets were placed with respect to droplets of alginate solution asillustrated in (A). iPSC-derived hepatocytes or endothelial cells were encapsulated in the MIPC fibers that were drawn from the interfaces between alginate and chitin. The fiberswere fused to form a multi-component fiber. The collected fibers were cultured for up to 8 days in static culture with media replenished every day. Albumin secretion assay wasperformed for the hepatocytes encapsulated in the scaffold in the presence (grey) or absence (white) of endothelial cells derived from iPSCs. * represents P < 0.001 among thegroups. The amount of albumin secreted was calculated using standards and monitored for up to 8 days in culture (B).
C. Du et al. / Biomaterials xxx (2014) 1e9 5
to stain positive for HNF4-a, which is one of the markers for maturehepatocytes. We also measured human albumin secretion atdifferent stages of differentiation. Results indicate that the secre-tion of human albumin increased 20-fold from Stage I to Stage II,further increasing to 28-fold at Stage III. The hepatic cells weremeasured to secrete human albumin in vitro at about 28 ng/ng ofDNA (Fig. 1E).
3.3. Differentiation of iPSCs to endothelial cells
We established a two-step differentiation protocol to deriveendothelial cells from the iPSCs (Fig. 2A). In the first step, the iPSCswere differentiated to the mesodermal lineage by the addition ofActivin-A (100 ng/ml), BMP-4 (25 ng/ml) and TGF-beta inhibitorSB431542 (10 mM) for 7 days. Following mesoderm differentiation,the cells were exposed to a high concentration of VEGF (at a finalconcentration of 55 ng/ml) to direct their differentiation towardsendothelial cells. Immunostaining of the differentiated cells withCD-31 and V-ECAD antibodies suggested that the cells weredifferentiated towards the endothelial phenotype (Fig. 2B). Thekinetics of gene expression during differentiation showed that theexpression of V-ECAD and PECAM-1 increased upon addition ofVEGF. The expression of V-ECAD was noted to be comparable to theexpression level in HUVECs. However, the expression of PECAM-1was about 6-fold lower than the expression level in HUVECs(Fig. 2C). Flow cytometry with antibodies against Von Willebrandfactor (vWF) and CD-31 was used to estimate the percentage ofendothelial phenotype cells. About 90% of the cells were identifiedpositive for the expression of vWF and CD-31 (Fig. 2D). Culture ofthe endothelial cells on Matrigel, whereupon tubule formation
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://dx
occurred, further confirmed the functional characteristics of thedifferentiated endothelial cells (Fig. 2E).
3.4. Encapsulation of cells in multi-component hydrogel fibers
Differentiated hepatocytes and endothelial cells were encapsu-lated within MIPC fibers in galactose- and collagen-containingdomains respectively. The MIPC fibers were subsequently assem-bled to form a polyelectrolyte hydrogel (Fig. 3). For controls, onlydifferentiated hepatocytes were encapsulated. In a separate set ofexperiments we analyzed the mechanical stability of the IPChydrogels by carrying out rheological analyses to characterize thedynamic modulus of the hydrogels. For constructs that werecultured for 3 days, we found that the shear storage modulus, G0, ofconstructs encapsulating hepatocarcinoma, HepG2 cells, weresignificantly higher than the acellular constructs (SupplementaryFig. 4A). These results seem to suggest that the encapsulatedHepG2 cells may have deposited new extracellular matrix materialswhich increased the G0 of the cellular hydrogels.
Upon encapsulation of cells in the MIPC fibers, liveedead assaywas conducted to confirm the viability of the cells in the scaffolds.Liveedead assay indicated that the cells were viable after encap-sulation (Supplementary Fig. 4B). Encapsulation of mature hepa-tocytes and endothelial cells in the MIPC fibers brings them intoclose proximity, which enhances the function of the hepatocytes.This was demonstrated by the albumin secretion assay. Humanalbumin secreted into the media was measured by ELISA, for 8 daysof culture in vitro. Albumin secretion was compared between he-patocytes and hepatocytes co-cultured with endothelial cells. Thekinetics of the assay indicated that albumin production increasedsteadily for the first 4 days of culture, followed by a gradual
cell-derived hepatocytes and endothelial cells in multi-component.doi.org/10.1016/j.biomaterials.2014.04.011

C. Du et al. / Biomaterials xxx (2014) 1e96
decrease in the next 4 days. We believe that this was due to thestatic culture conditions that limited nutrient and gas exchangebetween the media and cells embedded in the scaffold. Hence, weimplanted the cell-scaffold construct 4 days after seeding the cellsin the scaffold. However, at any given time point, the amount ofalbumin secreted in the co-culture group was noted to be w2e4� that of the single culture group. The maximum difference inalbumin secretion between the hepatocytes ‘alone’ group andhepatocyte-endothelial co-culture group was recorded on day 7 ofculture, when the co-culture group secreted approx. 4-fold morealbumin (Fig. 3B).
3.5. In vivo implantation
We next sought to investigate the development of the tissueconstructs comprised of iPS cell-derived hepatocytes and endo-thelial cells, when implanted in a liver regenerative environment.For this, the cell laden fibrous scaffolds were implanted in the liverof mice that underwent 70% partial hepatectomy. We segregatedthe study into 2 groups; one group received only the hepatocytes,while the other group received hepatocytes and endothelial cells.The animals were sacrificed at either 2 weeks or 4 weeks of thestudy. Serum samples were collected separately for human albumindetection. From H&E stainings of the explants, we noticed the lackof blood vessels in the group that received only hepatocytes(Fig. 4A) However, the group that received the 3D-patterned he-patocytes and endothelial cells showed the presence of bloodvessels and red blood cells (Fig. 4B and C). To further confirmendothelial tube formation, we used CD31 antibodies to identifythe endothelial cells. Immunostaining with CD31 antibodies clearlyshowed the presence of tubular structures made up of the endo-thelial cells. Double immunostaining with human albumin anti-body and CD31 antibody showed that the explants fromhepatocytes alone group had no human CD31 positive cells or bloodvessels even at 4 weeks of implantation (Fig. 5Ai, ii). On the otherhand, human CD31-stained blood vessel structures were observedfor the explants from the hepatocytes-endothelial co-culture group,
Fig. 4. Histological analysis was done on the cryosections derived from the explants of hepadotted line indicates the boundary of the fibrous scaffold implanted in the partially hepatsections derived from hepatocytes ‘alone’ group and (B) indicates the sections derived fromof the boxed region in (B). Arrows in B and C show the presence of blood vessels in this grouthe reader is referred to the web version of this article.).
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://d
where the hepatocytes were in close proximity with the endothe-lial cells (Fig. 5Aiiievi).
To investigate the functionality of the implanted hepatocytes,serum was collected from the animals from the hepatocytes groupand co-culture group. Dot-blots were performed on the serumcollected from the animals after 2 weeks and 4 weeks of the study.As presented in Fig. 5B, human albumin could be detected as earlyas 2 weeks for the group which included both hepatocytes andendothelial cells. The detection of human albumin in the serum ofthe animals suggests that the hepatocytes were functional and thatthe newly-formed blood vessels in the scaffold had anastomosedwith the host liver tissue. Establishing vascular networks as early as2 weeks, as demonstrated in Fig. 5A, helped in the circulation of thehuman albumin secreted by the differentiated cells. On the otherhand, wewere barely able to detect human albumin in the serum ofthe group that received only hepatocytes, even after 4 weeks ofimplantation. This further confirms the necessity of endothelialnetworks within the scaffold to establish a viable connection withthe host blood circulation.
4. Discussion
The success of liver tissue engineering would depend on theability to address the pressing issues applicable to the engineeringof any tissue or organ e the practical availability of a cell source foreach of the cell types that make up the organ, a methodology tocombine the cells three-dimensionally in a way that recapitulatesthe structure and function of the native tissue, and the generationof structures necessary for the vascularization of the construct.Prior to this work, our laboratory has endeavored to address thesevery issues of cell source [38,41], 3D-cell patterning [31,32] andvascularization [40]. The relevant methodologies are combined inthe present work, to realize a potentially workable platform tomake tissue constructs for liver therapy.
We had previously used recombinant protein methodology toderive iPSCs [38], and these cells were further differentiated intohepatocytes and endothelial cells for the purpose of the present
tocytes ‘alone’ group and hepatocytes co-cultured with endothelial cells group. The redectomized host liver. H&E staining was carried out on the sections. (A) indicates thehepatocytes co-cultured with endothelial cells. (C) represents the higher magnificationp. Scale bar ¼ 100 mm (For interpretation of the references to color in this figure legend,
cell-derived hepatocytes and endothelial cells in multi-componentx.doi.org/10.1016/j.biomaterials.2014.04.011

Fig. 5. (A) Explants were collected after 2 weeks and 4 weeks of implantation. Immunostaining was done on the cryosections from hepatocytes ‘alone’ group and hepatocytes co-cultured with endothelial cells. The sections were immunostained against CD-31 (green) and human albumin (red). (i) and (ii) represent the sections from hepatocytes ‘alone’ groupharvested at 2 weeks and 4 weeks, respectively. (iii) and (iv) represent the sections from hepatocytes co-cultured with endothelial cells group harvested at 2 weeks and 4 weeks,respectively. (v) and (vi) represent the magnified view of the boxed regions in (iii) and (iv), respectively. Scale bar in (i), (ii), (iii) and (iv)¼ 100 mm; in (v) and (vi) ¼ 50 mm. (B) Serumwas collected from the animals implanted either with hepatocytes ‘alone’ or with hepatocytes co-cultured with endothelial cells at 2 weeks and 4 weeks of the study. The serumwas adsorbed onto nitrocellulose membrane and probed with anti-human albumin antibody. Chemiluminescence system was used to detect the samples and the membrane wasimaged in a ChemiDoc MP system. The bottom panel in (B) represents the layout of the samples. PC and NC represent the positive control and negative control, respectively. H andH þ E represent the serum from hepatocytes ‘alone’ group or hepatocytes co-cultured with endothelial cells group, respectively (For interpretation of the references to color in thisfigure legend, the reader is referred to the web version of this article.).
C. Du et al. / Biomaterials xxx (2014) 1e9 7
study. For differentiation of iPSCs into hepatocytes, we adopted theprotocol of Takata et al. [39]. The differentiated cells showed thefunctional activities of hepatocytes such as albumin secretion, andwe succeeded in obtaining up to 47% of albumin positive cells, asmeasured by FACS. For the case of iPSC differentiation into endo-thelial cells, available protocols were limited to either the embryoidbody formation method or co-culture with OP9 cells [35e37,45e47]. Although both methods have been widely used, they areassociated with the disadvantages of uncontrolled differentiationand the use of undefined factors. These limitations led us toestablish a directed differentiation protocol to differentiate stemcells to endothelial cells following developmental pathways. Weused BMP4 as a stimulator to induce the differentiation of stemcells to the mesodermal lineage [48,49]. We then applied highconcentrations of VEGF to further direct the differentiation ofmesoderm cells towards endothelial cells. In addition to expressionof the relevant markers such as vWF and CD31, the functionality ofthese endothelial cells was ascertained by a tubule formation assay.
The hepatocytes and endothelial cells derived from iPSCs werecultured for up to 3 and 5 passages, respectively. FACS analysis onthese cells revealed that the phenotypes of the cells were main-tained. Supplementary Table S1 shows that 43.8% and 42% of he-patocytes at passage 3 stained positive for AFP and ALB antibodies,respectively. Similarly, 93% and 86% of endothelial cells at passage 5stained positive for vWF and CD-31 antibodies, respectively. We
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://dx
then co-cultured the iPSC-derived hepatocytes and endothelialcells in our 3D-cell-patterned, fiber assembled constructs, with thegoal of improving the functional characteristics of the hepatocytesand achieving vascularization of the tissue constructs whenimplanted in vivo. Co-culture of hepatocytes with endothelial cellshas demonstrated the ability of the latter to prolong the viability ofhepatocytes and enhance their functional capabilities [26,50,51]. Ofparticular relevance, liver-mimetic architectures comprising pri-mary rat hepatocytes and human LSECs have been assembled usingpolyelectrolyte multilayers (PEM), with an intermediate PEMcomprised of chitosan and hyaluronic acid, demonstrating main-tenance of liver-specific functions such as urea and albuminsecretion, as well as cytochrome P450 (CYP1A1/2) enzymatic ac-tivity. In the latter system as well as in ours, the goal was to reca-pitulate key spatial, geometric, and physiological characteristics ofcellular architectures found in vivo, in order to realize optimal he-patic function [50]. As a further aim, we carried out the differen-tiation of hepatocytes and endothelial cells in parallel, using thesame iPSCs as the starting point. In this way, we could engineer athree dimensional, endothelialized liver construct where all thecells were genetically identical (isogenic), a potentially importantpoint in developing future autologous therapies.
The implantation of these constructs in a mouse hepatectomymodel suggested that the presence of endothelial cells hadenhanced the anastomosis of vessels in the constructs with host
cell-derived hepatocytes and endothelial cells in multi-component.doi.org/10.1016/j.biomaterials.2014.04.011

C. Du et al. / Biomaterials xxx (2014) 1e98
tissue. Moreover, we also observed that the secretion of albumin, asdetected in the serum, was dramatically increased in the implantedco-culture constructs. Besides the mentioned benefit of reciprocalsignaling interactions between the two cell types, improved he-patocyte function may have also resulted from enhanced cellviability. A similar result was recently obtained by Baranski et al.,who used microtissue molding to demonstrate that constructscontaining highly aligned “cords” of endothelial cells improve he-patic survival and function when implanted in mice [52].
Based on the dimensions of the fibers and fiber assembly pro-tocol that was used, the spacing of the endothelial units in theconstruct was estimated to be in the range of 200e250 mm, sug-gesting that all the hepatocytes would be within the diffusion limitof oxygen and essential nutrients [53]. In practice, the close prox-imity of the hepatocytes to vasculature was evident in CD31-stained cross sections of the explants (Fig. 5A(iii)e(vi)).
Interestingly, we found that different niche microenvironmentswere required for optimal function of the two cell types in thisstudy, and therefore, they had to be separated in different domainswithin the MIPC fibers. While collagen was needed to align endo-thelial cells for formation of endothelial tubes, we observed that itwas not an optimal microenvironment for functional maintenanceof hepatocytes. We hypothesize that while the presence of collagenmight have provided better adhesion, it also stretched the hepa-tocytes along the fibers and this might have caused the decrease incellular function. A similar observation was made by Du et al.,where hepatocytes grown on galactose-modified substrates hadbetter functional maintenance than on collagen [54]. As such,separate galactose-rich microenvironments were provided for thedifferentiated hepatocytes in domains adjacent to the endothelialcell domains. Patterning of the two cell types in their respectiveniche microenvironments, achieved by assembly of MIPC fibers, ledto improved function of the hepatocytes in the constructs.
5. Conclusion
The results presented here demonstrate the potential applica-tion of multi-component fibers and 3D fiber assembly in liverbioengineering. Additionally, we have reported the completeworkflow for development of a potentially realizable liver tissueengineering platform, from the differentiation of hepatocytes andendothelial cells from iPSCs, to their assembly into tissue constructsand evaluation in a mouse model. This combination of methodol-ogies could be applied towards producing basic units of liver forpatient specific toxicological assays or for patient specific livertissue engineering.
Acknowledgment
This work is funded by the Institute of Bioengineering andNanotechnology (Biomedical Research Council, Agency for Science,Technology and Research, Singapore). Flow cytometry analysis wasperformed at the Biopolis Shared Facility, A*STAR, Singapore.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.biomaterials.2014.04.011.
References
[1] Allen JW, Hassanein T, Bhatia SN. Advances in bioartificial liver devices.Hepatology 2001;34:447e55.
[2] Strain AJ, Neuberger JM. A bioartificial liverestate of the art. Science2002;295:1005e9.
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://d
[3] Di Campli C, Nestola M, Piscaglia AC, Santoliquido A, Gasbarrini G, Pola P,et al. Cell-based therapy for liver diseases. Eur Rev Med Pharmacol Sci2003;7:41e4.
[4] Lagasse E, Connors H, Al-Dhalimy M, Reitsma M, Dohse M, Osborne L, et al.Purified hematopoietic stem cells can differentiate into hepatocytes in vivo.Nat Med 2000;6:1229e34.
[5] Lee KD, Kuo TK, Whang-Peng J, Chung YF, Lin CT, Chou SH, et al. In vitrohepatic differentiation of human mesenchymal stem cells. Hepatology2004;40:1275e84.
[6] Hamazaki T, Iiboshi Y, Oka M, Papst PJ, Meacham AM, Zon LI, et al. Hepaticmaturation in differentiating embryonic stem cells in vitro. FEBS Lett2001;497:15e9.
[7] Rambhatla L, Chiu CP, Kundu P, Peng Y, Carpenter MK. Generation ofhepatocyte-like cells from human embryonic stem cells. Cell Transpl2003;12:1e11.
[8] Cai J, Zhao Y, Liu Y, Ye F, Song Z, Qin H, et al. Directed differentiation ofhuman embryonic stem cells into functional hepatic cells. Hepatology2007;45:1229e39.
[9] Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouseembryonic and adult fibroblast cultures by defined factors. Cell 2006;126:663e76.
[10] Palakkan AA, Hay DC, A PR, K TV, Ross JA. Liver tissue engineering and cellsources: issues and challenges. Liver Int 2013;33:666e76.
[11] Si-Tayeb K, Noto FK, Nagaoka M, Li J, Battle MA, Duris C, et al. Highly efficientgeneration of human hepatocyte-like cells from induced pluripotent stemcells. Hepatology 2009;51:297e305.
[12] Song Z, Cai J, Liu Y, Zhao D, Yong J, Duo S, et al. Efficient generation ofhepatocyte-like cells from human induced pluripotent stem cells. Cell Res2009;19:1233e42.
[13] Chen YF, Tseng CY, Wang HW, Kuo HC, Yang VW, Lee OK. Rapid generation ofmature hepatocyte-like cells from human induced pluripotent stem cells byan efficient three-step protocol. Hepatology 2011;55:1193e203.
[14] LeCluyse EL, Bullock PL, Parkinson A. Strategies for restoration and mainte-nance of normal hepatic structure and function in long-term cultures of rathepatocytes. Adv Drug Deliv Rev 1996;22:133e86.
[15] Koide N, Sakaguchi K, Koide Y, Asano K, Kawaguchi M, Matsushima H, et al.Formation of multicellular spheroids composed of adult rat hepatocytes indishes with positively charged surfaces and under other nonadherent envi-ronments. Exp Cell Res 1990;186:227e35.
[16] Miranda JP, Leite SB, Muller-Vieira U, Rodrigues A, Carrondo MJ, Alves PM.Towards an extended functional hepatocyte in vitro culture. Tissue Eng Part CMethods 2009;15:157e67.
[17] Peshwa MV, Wu FJ, Sharp HL, Cerra FB, Hu WS. Mechanistics of formation andultrastructural evaluation of hepatocyte spheroids. Vitro Cell Dev Biol Anim1996;32:197e203.
[18] Wu FJ, Friend JR, Remmel RP, Cerra FB, Hu WS. Enhanced cytochrome P450IA1 activity of self-assembled rat hepatocyte spheroids. Cell Transpl 1999;8:233e46.
[19] LeCluyse EL. Human hepatocyte culture systems for the in vitro evaluationof cytochrome P450 expression and regulation. Eur J Pharm Sci 2001;13:343e68.
[20] Yagi K, Tsuda K, Serada M, Yamada C, Kondoh A, Miura Y. Rapid formation ofmulticellular spheroids of adult rat hepatocytes by rotation culture and theirimmobilization within calcium alginate. Artif Organs 1993;17:929e34.
[21] Rowley JA, Madlambayan G, Mooney DJ. Alginate hydrogels as syntheticextracellular matrix materials. Biomaterials 1999;20:45e53.
[22] Chia SM, Leong KW, Li J, Xu X, Zeng K, Er PN, et al. Hepatocyte encapsulationfor enhanced cellular functions. Tissue Eng 2000;6:481e95.
[23] Ng S, Wu YN, Zhou Y, Toh YE, Ho ZZ, Chia SM, et al. Optimization of 3-Dhepatocyte culture by controlling the physical and chemical properties ofthe extra-cellular matrices. Biomaterials 2005;26:3153e63.
[24] Balakrishnan B, Jayakrishnan A. Self-cross-linking biopolymers as injectable insitu forming biodegradable scaffolds. Biomaterials 2005;26:3941e51.
[25] Abu-Absi SF, Hansen LK, Hu WS. Three-dimensional co-culture of hepatocytesand stellate cells. Cytotechnology 2004;45:125e40.
[26] Bhatia SN, Balis UJ, Yarmush ML, Toner M. Effect of cell-cell interactions inpreservation of cellular phenotype: cocultivation of hepatocytes and non-parenchymal cells. FASEB J 1999;13:1883e900.
[27] Seo SJ, Kim IY, Choi YJ, Akaike T, Cho CS. Enhanced liver functions of hepa-tocytes cocultured with NIH 3T3 in the alginate/galactosylated chitosanscaffold. Biomaterials 2006;27:1487e95.
[28] Tukov FF, Maddox JF, Amacher DE, Bobrowski WF, Roth RA, Ganey PE.Modeling inflammation-drug interactions in vitro: a rat Kupffer cell-hepatocyte coculture system. Toxicol Vitro 2006;20:1488e99.
[29] Narayanan K, Leck KJ, Gao S, Wan AC. Three-dimensional reconstitutedextracellular matrix scaffolds for tissue engineering. Biomaterials 2009;30:4309e17.
[30] Tai BC, Du C, Gao S, Wan AC, Ying JY. The use of a polyelectrolyte fibrousscaffold to deliver differentiated hMSCs to the liver. Biomaterials 2010;31:48e57.
[31] Wan AC, Leong MF, Toh JK, Zheng Y, Ying JY. Multicomponent fibers by multi-interfacial polyelectrolyte complexation. Adv Healthc Mater 2012;1:101e5.
[32] Lim TC, Leong MF, Lu H, Du C, Gao S, Wan AC, et al. Follicular dermal papillastructures by organization of epithelial and mesenchymal cells in interfacialpolyelectrolyte complex fibers. Biomaterials 2013;34:7064e72.
cell-derived hepatocytes and endothelial cells in multi-componentx.doi.org/10.1016/j.biomaterials.2014.04.011

C. Du et al. / Biomaterials xxx (2014) 1e9 9
[33] Shirahashi H, Wu J, Yamamoto N, Catana A, Wege H, Wager B, et al. Differ-entiation of human and mouse embryonic stem cells along a hepatocytelineage. Cell Transpl 2004;13:197e211.
[34] Hay DC, Zhao D, Ross A, Mandalam R, Lebkowski J, Cui W. Direct differenti-ation of human embryonic stem cells to hepatocyte-like cells exhibitingfunctional activities. Cloning Stem Cells 2007;9:51e62.
[35] Vittet D, Prandini MH, Berthier R, Schweitzer A, Martin-Sisteron H, Uzan G,et al. Embryonic stem cells differentiate in vitro to endothelial cells throughsuccessive maturation steps. Blood 1996;88:3424e31.
[36] LevenbergS,Golub JS,AmitM, Itskovitz-Eldor J, LangerR.Endothelial cellsderivedfrom human embryonic stem cells. Proc Natl Acad Sci U S A 2002;99:4391e6.
[37] Wang ZZ, Au P, Chen T, Shao Y, Daheron LM, Bai H, et al. Endothelial cellsderived from human embryonic stem cells form durable blood vessels in vivo.Nat Biotechnol 2007;25:317e8.
[38] Khan M, Narayanan K, Lu H, Choo Y, Du C, Wiradharma N, et al. Delivery ofreprogramming factors into fibroblasts for generation of non-genetic inducedpluripotent stem cells using a cationic bolaamphiphile as a non-viral vector.Biomaterials 2013;34:5336e43.
[39] Takata A, Otsuka M, Kogiso T, Kojima K, Yoshikawa T, Tateishi R, et al. Directdifferentiation of hepatic cells from human induced pluripotent stem cellsusing a limited number of cytokines. Hepatol Int 2011;5:890e8.
[40] Leong MF, Toh JK, Du C, Narayanan K, Lu HF, Lim TC, et al. Patterned pre-vascularised tissue constructs by assembly of polyelectrolyte hydrogel fibres.Nat Commun 2013;4:2353.
[41] Ng SL, Narayanan K, Gao S, Wan AC. Lineage restricted progenitors for therepopulation of decellularized heart. Biomaterials 2011;32:7571e80.
[42] Levenberg S, Rouwkema J,MacdonaldM,Garfein ES, KohaneDS,DarlandDC, et al.Engineeringvascularized skeletalmuscle tissue.NatBiotechnol 2005;23:879e84.
[43] Rouwkema J, de Boer J, Van Blitterswijk CA. Endothelial cells assemble into a3-dimensional prevascular network in a bone tissue engineering construct.Tissue Eng 2006;12:2685e93.
Please cite this article in press as: Du C, et al., Induced pluripotent stemhydrogel fibers for liver tissue engineering, Biomaterials (2014), http://dx
[44] Yang J, Yamato M, Shimizu T, Sekine H, Ohashi K, Kanzaki M, et al. Recon-struction of functional tissues with cell sheet engineering. Biomaterials2007;28:5033e43.
[45] Li Z, Wilson KD, Smith B, Kraft DL, Jia F, Huang M, et al. Functional andtranscriptional characterization of human embryonic stem cell-derivedendothelial cells for treatment of myocardial infarction. PLoS One 2009;4:e8443.
[46] Vodyanik MA, Bork JA, Thomson JA, Slukvin II. Human embryonic stem cell-derived CD34þ cells: efficient production in the coculture with OP9 stromalcells and analysis of lymphohematopoietic potential. Blood 2005;105:617e26.
[47] Vodyanik MA, Slukvin II. Hematoendothelial differentiation of human em-bryonic stem cells. Curr Protoc Cell Biol 2007;36. 23.6.1-23.6.28.
[48] Maeno M, Mead PE, Kelley C, Xu RH, Kung HF, Suzuki A, et al. The role of BMP-4 and GATA-2 in the induction and differentiation of hematopoietic meso-derm in Xenopus laevis. Blood 1996;88:1965e72.
[49] Zhang P, Li J, Tan Z, Wang C, Liu T, Chen L, et al. Short-term BMP-4 treatmentinitiates mesoderm induction in human embryonic stem cells. Blood2008;111:1933e41.
[50] Kim Y, Larkin AL, Davis RM, Rajagopalan P. The design of in vitro liver sinusoidmimics using chitosan-hyaluronic acid polyelectrolyte multilayers. Tissue EngPart A 2010;16:2731e41.
[51] Rajagopalan P, Shen CJ, Berthiaume F, Tilles AW, Toner M, Yarmush ML.Polyelectrolyte nano-scaffolds for the design of layered cellular architectures.Tissue Eng 2006;12:1553e63.
[52] Baranski JD, Chaturvedi RR, Stevens KR, Eyckmans J, Carvalho B, Solorzano RD,et al. Geometric control of vascular geometry to enhance engineered tissueintegration and function. Proc Natl Acad Sci 2013;110:7586e91.
[53] Jain RK, Au P, Tam J, Duda DG, Fukumura D. Engineering vascularized tissue.Nat Biotechnol 2005;23:821e3.
[54] Du Y, Chia SM, Han R, Chang S, Tang H, Yu H. 3D hepatocyte monolayer onhybrid RGD/galactose substratum. Biomaterials 2006;27:5669e80.
cell-derived hepatocytes and endothelial cells in multi-component.doi.org/10.1016/j.biomaterials.2014.04.011