Implant Management - EP Lab Digest · 2020. 4. 1. · transvenous (TV) ICD implants. • System...
Transcript of Implant Management - EP Lab Digest · 2020. 4. 1. · transvenous (TV) ICD implants. • System...

Module 2Implant Management
Including advanced implant techniques
Physician Training Implant Management Workbook
EMBLEMTM MRI S-ICD System Implant Management

CRM-349606-AC
Instructions
Module 1: Implant Management
Module 2: Anatomic Considerations
EMBLEMTM MRI S-ICD System Brief Summary
For more information:
• AccesstheInstructionsforUseatbostonscientific.com/IFU
• Call 1-800 CARDIAC
• Contact your BSC representative
Workbook Contents
Contents EMBLEMTM MRI S-ICD System

CRM-349606-AC
EMBLEMTM MRI S-ICD System Instructions
This workbook provides information about the EMBLEMTMMRIS-ICDSystemimplantprocedure.Topics include patient screening, implant planning and preparation, implant steps, and anatomic considerations.
To use the workbook:
• Study the content and refer to the images provided.
• Review the Key Concept listed in the righthand column.
• Read the Notestolearnmore.
The concepts in this workbook build from page to page allowingyoutosystematicallyaddtoyourknowledge.Workatyourownpace.Reviewconceptsasneeded.
NOTES
KEY CONCEPT
Review the key concept before goingtothenextpage.
Read Notes to learn more about the topic.
Workbook Instructions

CRM-349606-AC
EMBLEMTM MRI S-ICD System
Description
Automated Screening Tool (AST)
Description
ECGScreeningConfiguration
ECG Signal Quality
AST Setup
Automated ECG Tests
Sensing Vector Acceptability
Troubleshooting Tips Anesthesia and Pain Control
Considerations
Serratus Anterior Plane Block (SAPB)
Procedure Planning and Preparation
Patient Markup
Arm Positioning
DefibrillationProtection/Draping
Implant Procedure
Pocket Formation
Xiphoid Incision
Proximal Electrode Positioning
Distal Electrode Positioning
Device Positioning
Optimal Placement
Implant Management l Page 1
Contents
Induction Testing
Prepare Patient
Perform Induction Test
Post-Implant Considerations
Wound Closure
Patient Care
Challenges
High BMI Patients
Addendum
Monitored Anesthesia Care (MAC)
Non-Anesthesiologist Administered Sedation and Analgesia (NASA)
Module 1: Implant Management

CRM-349606-AC
Implant Management Learning Objectives
After completing this module, you should be able to:
• Identify EMBLEMTMMRIS-ICDSystemcomponents.
• Describe how to screen patients before EMBLEMTM MRIS-ICDSystemimplant.
• Discussoptionsforsedationandpaincontrol.
•Liststepsforproceduralplanningandpreparation.
• Describe basic EMBLEMTM MRI S-ICD System implantsteps.
•Describeinductiontesting.Troubleshootissuesthatariseduringinductiontesting.
Implant Management l Page 2

CRM-349606-AC
Description
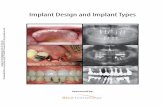
The EMBLEMTM MRI S-ICD System consists of the S-ICD device and electrode, Electrode Delivery System (EDS),andLATITIUDEcommunicator.
• The device is implanted in a pocket between the latissimus dorsi and serratus anterior muscles at the mid-axillaryline.
• The electrode is inserted via an incision just left of the xiphoid process, then passed through a subcutaneous tunnel to the device pocket and superiorsternum.Theproximal sensing ring isplacednearthexiphoid.Thedistal electrode tip is placed in the upper sternum, 14 cm from theproximalsensingring.Thedefibrillationcoilispositioned parallel to and 1 to 2 cm from the sternal midline.FigureA.
• The Model 4712 Electrode Delivery System (EDS) is used to create lateral and superior tunnels forproximalanddistalelectrodeimplant.TheEDSincludes two tunneling tools pre-loaded onto 14 cm and21cmsheaths.FigureB.
• The EMBLEM MRI S-ICD System is enabled for remote patientmanagementviaLATITUDENXT.
The EMBLEMTM MRI S-ICD System consists of the device and electrode, Electrode Delivery System (EDS), and LATITUDE communicator.
To ensure appropriate sensing, avoid the pectoralis muscle when positioningthedistalelectrode.
Figure A: Sensing configuration Figure B: EMBLEMTM MRI S-ICD System
KEY CONCEPT
NOTES
EMBLEMTM MRI S-ICD System
Implant Management l Page 3
Distal electrode tip
Proximal electrode
Device/electrode
LATITUDE
Electrode Delivery System (EDS)

CRM-349606-AC
Automated Screening Tool (AST) Description
The Model 2889 Automated Screening Tool (AST)may improve the selection of suitable candidates for EMBLEMTMMRIS-ICDSystemimplant.1 The AST is available for use with the Model 3120 ZOOM LATITUDETM programmer.
• The AST may reduce the: - Inappropriate exclusion of patients with largeT-waves.Example: Brugada syndrome, congenital heart disease (CHD)1,2
- Inappropriate exclusion of patients with large R-waveamplitudes.Example: hypertrophic cardiomyopathy(HCM).3,4
- Inappropriate selection of patients with small R-waves.1
Subcutaneous cardiac signals (S-ECGs) are similar to surfaceECGsignals.TheASTverifiestheacceptabilityofthesurfaceECGforS-ICDSystemimplant.
The Automated Screening Tool (AST) may improve the selection of suitable candidates for EMBLEMTM MRIS-ICDSystemimplant.
KEY CONCEPT
NOTES
Implant Management l Page 4
Figure A: Programmer Home screen Figure B: Model 3120 programmer
The S-ICD System interprets S-ECG signals using three sensing vectors:- proximal sensing ring to device (primary)- distal sensing ring to device (secondary)- distal to proximal sensing ring (alternate)

CRM-349606-AC
ECG Screening Configuration
To screen the patient, use a three-lead ECG configuration that represents the intended location of thedeviceandelectrode.
ThetypicalECGscreeningconfigurationisdepictedinFigure B and described here:
• ECG electrode LL - at the 5th intercostal space along the mid-axillary line to represent the intended locationofthedevice.
• ECG electrode LA - 1 cm left lateral of the xiphoid midline to represent the intended location of the proximalsensingring.
• ECG electrode RA - 14 cm superior to the LA electrode to represent the intended location of the distalsensingtip.
• ECG electrode RL - at the desired location to serve asagroundelectrode.
Collect the screening ECG in the intended location of the device and electrode.
Location changes may be considered if the patient fails screening.SeeTroubleshootingTips at the end of this section for details.
KEY CONCEPT
NOTES
Automated Screening Tool (AST)
Implant Management l Page 5
FigureB:TypicalscreeningconfigurationFigure A: S-ICD System placement

CRM-349606-AC
ECG Signal Quality
Ensure each collected ECG has a stable baseline and isfreeofnoiseandartifacts.
To obtain a stable ECG baseline:
•Removechesthair.Cleanthepatient’sskinusinganon-alcoholwipeorprepgel.
•Usenewelectrodesfromanunopenedpackage.
• Use enough gel to ensure good skin-electrode contact.
•Addagroundelectrode(RL)topreventinterference.FigureA.
• Ask the patient to inhale; then exhale and hold his orherbreathwhilerecordinga10-secondECG.
Correct a wandering baseline by replacing the ECG cable or using a gauze pad to create light skin abrasion forimprovedcontactattheelectrodesite.
Ensure each collected ECG has a stable baseline and is free of noise andartifacts.
ECG markers:S = sensed beatT = tachy detectionC = charge startE = charge endN = noise• = discard ♥ = event end
KEY CONCEPT
NOTES
Automated Screening Tool (AST)
Implant Management l Page 6
Figure B: Wandering baseline Figure A: Add ground electrode (RL)

CRM-349606-AC
Automated Screening Tool (AST) Set-up Automated Screening Test
To set up the automated ECG screening test:
1.Positionsurfaceelectrodes.*
2.SelecttheEMBLEM S-ICD Automated Screening Tool fromtheprogrammerhomescreen.FigureA.
3.ConnecttheECGcablestotheprogrammer.
4.SelecttheInformation tab to enter or edit patient information(FigureB).
5.VerifytheECGsignal:**- Ensure each ECG signal has a stable baseline and isfreeofnoiseandmotionartifacts.
- Select MagnifytozoominontheECGsignal.-AdjustsignalGainasneeded.
*RefertotheECGScreeningConfigurationpage.
**RefertotheECGSignalQualitypage.
To set up automated screening test:
1.Positionsurfaceelectrodes.
2.SelecttheEMBLEMS-ICDAutomatedScreeningTool.
3. ConnectECGcables.
4.Recordpatientinformation.
5. VerifyECGsignal.
KEY CONCEPT
NOTES
Implant Management l Page 7
Figure A: Programmer home screen
The required patient information fieldsare:- Patient Name or ID- Date of Birth
Figure B: Patient information screen

CRM-349606-AC
Automated Screening Tool (AST)
A patient is considered suitable for an S-ICD System implant if at least one sensing vector is acceptable in all tested patient postures. Required postures are supine andstandingorsitting.
To run automated ECG tests:
1.SelecttheScreening tab; then select the intended Sternal Lead Positionofthedistalelectrode.Menuoptions are left sternal margin (default), right sternal margin,andmedial.FigureA(1).
2. RunECGtestsforrequiredpostures:- Place patient in supineposition.SelectcorrespondingRunbutton(arrow)tocollectECG.FigureA(2).
- Select Magnify button to view ECG test results fromtheSnapshotscreen.SelectClose. FigureB.
- Place patient in standing or sittingposition.FigureA(3).
- Runtestandviewresults.SelectClose.
3.RunECGtestsforadditionalpostures:-Placepatientindesiredposture.- Select Other; type posture in corresponding text field(e.g.,leftlateral,rightlateral).FigureA(4).
- Select Capture ECG.Viewresults.-ConsidercollectingECGduringexercisetesting.
4.Savescreeningreport:- Select Save Reporttosavetoharddrive.- Select Print Reporttosendtoexternalprinter.
5.SelectEnd Screening Session.
To run automated ECG tests:
1.SelectSternalLeadPosition.
2.RunECGtestsforrequiredpostures.
3.Reviewtestresults(Snapshot).
4.Savescreeningreport.
5.Endscreeningsession.
To repeat an ECG test, select Run; thenselectProceed.Thepreviousresultsareoverwritten.
To run more than six ECG tests, save the screening report and start anewsession.
KEY CONCEPT
NOTES
Implant Management l Page 8
Automated ECG Tests
Figure B: Snapshot view Figure A: ECG Test screen
1
4 2 3

CRM-349606-AC
Automated Screening Tool (AST)
The ECG screening report summarizes results for eachleadandposturetested.
To identify a sensing vector:
• Ensure the QRS morphology is consistent for all tested postures (similar peak amplitudes and QRS widths).Fornotchedorclippedsignals,ensurelargepeaksareconsistentinrelationtosmallpeaks.
• Verify the acceptability of at least one common ECG surface lead in all tested postures.
Unacceptable or marginal sensing vectors may result in failedorinappropriatetherapy.
Use the ECG screening report to evaluate QRS morphology and identify an acceptable sensing vector.
ToexportreporttoUSBflashdrive:- SelectEndScreeningSession.- InsertUSB.- Select Patient Data
Management; then the Export ScreeningDatatab.
- Select Export and follow prompts.
KEY CONCEPT
NOTES
Implant Management l Page 9
Sensing Vector Acceptability

CRM-349606-AC
Fail Test Result
If the patient fails the screening test, select Advanced View toviewthefilteredsignalandtroubleshootreasonsforscreeningfailure.Consider altering the intended location of the device or electrode as follows:
• If the R-wave amplitude is too low, consider placing the device posterior to the mid-axillary line.
• If the R-wave amplitude is too high, consider moving the electrode to the right side of the sternum.
• If the ECG shows elevated T-waves, consider moving the electrode 1 cm up or down, placing the electrode on the right side of the sternum, or placing the device posterior to the mid-axillaryline.
Automated Screening Tool (AST) Troubleshooting Tips
Implant Management l Page 10

CRM-349606-AC
Considerations
An S-ICD System implant requires anesthesia and pain control strategies that differ from traditional transvenous(TV)ICDimplants.
• System implant involves dissection within the highly innervated intercostal region (T2 to T9), subcutaneoustunnelling,anddefibrillationtesting.The use of general anesthesia allows the implanter to focus on the technical aspects of the procedure, butincreasesproceduraltime,cancausesignificantbradycardia or hypotension in heart failure patients, andmayprolongrecovery.16
• A recent expert panel has recommended sedation strategies that limit the use of general anesthesia, and pain control strategies that reduce the need foropioids.6 These strategies are described on the next three pages.
S-ICD System implant requires anesthesia and pain control strategies that differ from transvenous(TV)ICDimplants.
Strategies that limit the use of general anesthesia and opioids are recommended.
It is the responsibility of the implanting physician to ensure all decisions regarding anesthesia and pain control are appropriate for the patient.
KEY CONCEPT
NOTES
Anesthesia and Pain Control
Implant Management l Page 11

CRM-349606-AC
Serratus Anterior Plane Block (SAPB)
Ultrasound-guided serratus anterior plane block (SAPB) provides long-acting anesthesia to the lateral branchesoftheintercostalnervesfromT2toT9.Itmaybe an option for patients who cannot tolerate general anesthesiaorwhorequiremorelocalanesthesia.8
•Theplaneblocktakesaboutfivetotenminutesto administer, anesthetizes the nerves that supply the left chest for up to eight hours, and can be usedwithanticoagulants.6,8 Studies show that serratus anterior plane block along with monitored anesthesia care may eliminate the need for post-implantopioids.6,8
• The images in Figure A show injection sites for serratusanteriorplaneblock.Ahighfrequencyultrasound transducer permits visualization of fascial layers.Thered starshowsthespaceinjected.16
Basic technique:
• The transducer is placed on the mid-axillary line inthetransverseplaneatthelevelofthefifthrib.After applying a topical anesthetic, the needle is advanced in-plane at a 45o towardthefifthrib.Theentireneedleisvisualizedtoavoidbloodvessels.
• Once the needle tip is in place, a small amount of local anesthetic is injected to hydrodissect fascial layersandopenthefascialplane.Alargervolumeoflocalanesthetic(e.g.,30to40mLof0.25%bupivaciane)isgraduallyinjected.Theneedleisremovedandthepatient’spainlevelassessed.
Ultrasound-guided serratus anterior plane block provides long-acting anesthesia to the lateral branches of the intercostal nerves from T2 to T9.
Plane blocks have historically been used for breast and thoracic surgery.Publishedreportsshowexcellent results using plane block forS-ICDSystemimplant.8,16
Figure A: Ultrasound-guided serratus anterior plane block8
KEY CONCEPT
NOTES
Anesthesia and Pain Control
Implant Management l Page 12
Space injected

CRM-349606-AC
Patient Mark-up
Refer to anatomic landmarks to mark-up the implant area as follows:
• Mark incision sites. FigureA.- Xiphoid: 1 cm left and 1 cm above the xiphoid
midline- Pocket: between the 5th and 6th intercostal
space at the left mid-axillary line
• In females, mark the bottom of the bra line when thepatientissittingorstanding.Ensurethemarkedpocketincisionsiteisoutsidethebraline.
• Draw the lateral tunnel line between the xiphoid andpocketincisionsites.Markthepositionoftheintegratedsuturesleeveatthexiphoid.
• Draw the superior tunnel line between the xiphoid incision site and position of the distal electrode tip inuppersternum(14cm).Placeelectrodeoverskintodeterminepositionofdistaltip.Take tissue depth into account to avoid underestimating length of superior tunnel. FigureB.
• Draw the mid-axillary reference line starting at thedeepestpartofthearmpit.
Use anatomic landmarks to clearly mark incision sites, the device pocket, tunnel lines, and reference lines.
Figure A: Mark-up implant area Figure B: Determine distal electrode position
KEY CONCEPT
NOTES
Procedure Planning and Preparation
Implant Management l Page 13
Other implant equipment:- Sterile drapes, incision drape - Marker pen- Surgical set with scalpel, surgical tweezers, surgical scissors, needle driver, large retractor-Sutures:twoforelectrodefixation, one for anchoring device in pocket, 2.0Vicrylforclosingsubcutaneouslayers,4.0Vicrylforskinlayer- Needles: Small half circle for electrodefixation,largerhalfcircleforanchoringdevice.

CRM-349606-AC
Arm Positioning
Secure the patient’s left armbeforedraping.
•Positionandstrapthepatient’sleftarmonapaddedextensionboard,palmfacingup.Anglethearmno more than 60o to prevent injury to the brachial plexusandulnarnerve.FigureA.
•Ensuretheleftshoulderisrelaxed.Askthepatienttoconfirmthearmpositioniscomfortable.
• In some patients, it may be helpful to slightly rotatethepatient’storsotobettervisualizepocketformation.Useablanketrollorwedgetosupportthe patient at a 25o to 30oangle.
• Usetapetomanagebreastandlooseadiposetissue.
Strapthepatient’sleftarmonapaddedboardwithpalmfacingup.Angle the arm no more than 60o to improvecomfortandpreventinjury.
Figure A: Arm position during implant
KEY CONCEPT
NOTES
Procedure Planning and Preparation
Implant Management l Page 14
Refer to Anatomic Considerations (Module 2 of this workbook) for more information about the brachialplexusandulnarnerve.

CRM-349606-AC
Defibrillation Protection / Draping
Defibrillation protection
•Backupdefibrillationprotectionisnecessaryduringimplantandinductiontesting.Typicallyonedefibrillationpadisplacedonthepatient’schestbelowtherightclavicle;theotheronthepatient’sbackbelowtheleftscapula.
• To accommodate the larger implant area required for an S-ICD System implant, shift the front pad to the right (right anterior pectoral placement) and the corresponding back pad to the left (left posterior scapularplacement).FigureA.
Use four sterile drapes to create a surgical window withfullexposuretotheimplantarea.Securedrapes.FigureB.
• Placethefirstdrapeonthelowerbodyandextendabovetheumbilicalline,halfwaytothexiphoid.
•Placetheseconddrapealongthepatient’sleftsidetomeetthetablesurface(orsupportwedge).Extendthedrapefromtheaxillatothefirstdrape.
•Placethethirddrapetotherightofthepatient’smidline.Extendthedrapefromtheclavicletothefirstdrape.Ensurethedrapeisnocloserthan2cmfromthemidline.
• Placethefourthdrapeacrossthepatient’snecktomeetthedrapesonbothsides.
Providedefibrillationprotectiontoaccommodatetheimplantarea.Drape the patient to create a surgical window with full exposure totheimplantarea.
Compared to a TV-ICD implant, the S-ICD requires a larger implant area with exposure of the left lateralthorax.
A number of the infections that occurred during early S-ICD System implants were related to suboptimal draping.9
Figure A: Defibrillation pad placement Figure B: Patient draping
KEY CONCEPT
NOTES
Procedure Planning and Preparation
Implant Management l Page 15

CRM-349606-AC
The intermuscular device pocket is formed in the space between the serratus anterior and latissimus dorsi muscles. The intermuscular pocket places the deviceposteriortothemidaxilla.
• To form the pocket, make a 6 cm incision at the markedincisionsite.Dissecttothemuscularfasciaandfollowthecontourofthechestwall.Theexactanatomic plane depends on the size of the lattisimus dorsi.FigureA.
• Place the device in the pocket to test the fit. When positioned, the inferior device margin is parallel tothexiphoidorslightlymorecranial.Inpatientswith a prominent lattisimus dorsi, the muscle partly coversthedevice.10FigureB.
• Place an anchoring suture in the fascia covering the serratusanterior.
•Cauterizeallvesselstokeepthepocketdry.
The intermuscular pocket is formed in the space between the serratus anterior and latissimus dorsi muscle.Thepocketplacesthedeviceposteriortothemid-axilla.
An intermuscular pocket may:- Reduce the DFT in high BMI
patients.- Improve comfort and cosmetic
appearanceinlowBMIpatients.
Figure A: Pocket formation Figure B: Test device fit
KEY CONCEPT
NOTES
Implant Procedure
Implant Management l Page 16
Pocket Formation

CRM-349606-AC
Xiphoid Incision
Xiphoid incision
• Make a 2 to 3 cm horizontal incision about 1 cm aboveand1cmleftoftheinferiorxiphoidprocess.FigureA.In high BMI patients, a wider incision may be needed to access the fascial plane and place the anchoring sutures.
•Dissecttothefascialplanetofacilitatetunnelling.
• Place at least two anchoring sutures within the incision, spacing them to match the grooves of the integratedsuturesleeve.
Standard of patient care
• Flush all incisions thoroughly, using an antibiotic solutionperstandardofcare.
• Usesterilesalinetokeepincisionsmoist.
• Managepainperplannedprotocol.
Make a 2 to 3 cm horizontal incision 1 cm above and 1 cm left of the inferiorxiphoidprocess.Dissecttothefascialplane.
The size and orientation of the xiphoid incision depends on the patient’sbodyhabitus.
Figure A: Xiphoid incision
KEY CONCEPT
NOTES
Implant Procedure
Implant Management l Page 17

CRM-349606-AC
Lateral tunnel - xiphoid to pocket
• Stay on the deep fascial plane when tunneling from the xiphoidincisiontothepocketincision.GuidetheEDS towardinferiorsideofpocket.FigureA(top).
• Remove tunneling tool from the sheath and insert theelectrodeintosheath.Passtheelectrodethrough the sheath from the pocket to the xiphoid incision.FigureA(bottom).
Proximal electrode positioning
• Secure the integrated suture sleeve to the deep fascia using at least two ofthefoursuturegrooves.The suture sleeve may be anchored in a horizontal, vertical, or curved position. FigureB.
• Pullonthetwoendsofthesuturetoconfirmadequatetissuefixation.Thesutureissecureifitdoes not pull out as the tissue tents.
• Alternative technique: To gain more room to maneuver, create the superior tunnel before securingtheintegratedsuturesleeveatthexiphoid.
Stay on the deep fascial plane when creatingthelateraltunnel.Tunnelfrom the xiphoid to the inferior pocket.
Secure the integrated suture sleeve to deep fascia using at least two suturegrooves.
KEY CONCEPT
NOTES
Implant Procedure
Implant Management l Page 18
Proximal Electrode Positioning
Figure A: Create lateral tunnel / Insert proximal electrode Figure B: Secure integrated suture sleeve
Directing the EDS toward the inferior side of the pocket may protect the electrode from being inadvertentlycutwhenit’stimefordevicereplacement.
Appropriate anchoring techniques preventelectrodemovement.9
Use caution when tunneling near breastimplant.

CRM-349606-AC
Superior tunnel - xiphoid to upper sternum
• Tunnel from the xiphoid incision to the 2nd inter-costalspace(sternomanubrialjunction).Remainparallel toand1to2cmfromthesternalmidline.Ensure the tunnel is long enough to accommodate thedistalelectrode(14cm).
• Angle the EDS 10o to 20o toward sternal bone to stay close to the deep fascia. UsefingerstoguidetheEDSalongthecurvatureofthesternum.FigureB.
•Standatthepatient’smidlineforagoodviewofthetunnelingprocess.Ifthetunnelpositionissuboptimal,removetheEDSandstartover.
Distal electrode positioning
•Removetunnelingtoolfromsheath.Crackthesheath hub, then advance the electrode through the sheath.
•Palpatethedistalelectrodetiptoconfirmitisatthesternomanubrialjunction.Thensplitthesheathandcarefullyremoveit.
• Massage along the length of the distal electrode and overtheincisionstoremovetrappedair.
• Usefluoroscopytoconfirmtheelectrodeiscorrectlypositioned,withnobucklingalongitslength.
Stay parallel to and 1 to 2 cm from the sternal midline when creating thesuperiortunnel.AngletheEDStoward the sternal bone to stay closetothedeepfascia.
Palpatetoconfirmthedistalelectrodetipiscorrectlypositioned.
KEY CONCEPT
NOTES
Implant Procedure
Implant Management l Page 19
Distal Electrode Positioning
Figure A: Create superior tunnel Figure B: Position distal electrode
In a patient with sternal wires, use fluoroscopytoensuresufficientseparation between the wire and sensingrings.Metal-to-metalcontactcancompromisesensing.9
In some patients, right parasternal positioning may improve sensing and involve more muscle mass in theshockvector.9

CRM-349606-AC
Electrode connection to device:
• Insert the torque wrench at a 90o angle into the centerdepressionofthesealplug.Thisopenstheseal plug and provides a path for the release of air and fluidfromtheconnectorport.
• With the torque wrench in place, fully insert the electrodepinstraightintotheconnectorport.Confirm electrode tip is visible past the connector block. FigureA.
• Apply gentle downward pressure on the torque wrenchtoensureitisfullyengagedinthesetscrew.Turn the setscrew clockwise until it clicks.
• Removetorquewrench.Gently tug on the electrode toensureitissecurelyconnected.FigureA.
Pulse generator positioning
• Thread a nonabsorbable suture through each of the two suture holesinthedeviceheader.Placethedeviceinthepocket,thensutureittothefascia.FigureB.
• Keep the suture loose to:-Permitfullrangeofmotion.- Keep device from leaning too tightly against ribcage.
-Preventskinerosion.- AvoidhighshockimpedanceandahighDFT.
•Coilexcesselectrodelengthunderdevice.
Open seal plug to release trappedair.Insertelectrodepininto connector port and tighten setscrew.
Anchor device in pocket, ensuring it isnottootightagainsttheribcage.
KEY CONCEPT
NOTES
Implant Procedure
Implant Management l Page 20
Device Positioning
Figure B: Secure device in pocket
A slightly loose setscrew or seal plug puncture may cause inappropriatetherapy.9
Appropriate anchoring techniques prevent device movement and erosion.9
Figure A: Check electrode connection
Suture holes

CRM-349606-AC
Implant Procedure Optimal Placement
After implant and before hospital discharge, obtain chestx-raystoassessdeviceandelectrodepositioning.Recall that in the optimal sensing configuration, the heart is between the device and the distal coil.
Example:
• In the AP view, the sensing rings are parallel and about1cmfromthesternalmidline.Thedeviceisatthemid-axillaryline.
• In the left lateral view, the sensing rings appear to lieonthesternalsurface.Thedeviceisatthemid-axillary line, in a position that is neither too anterior ortooposterior.
Usex-raystoconfirmdeviceandelectrodepositioning.
The device can be placed with the logo facing inward or outward and orientedverticallyorhorizontally.Avertical orientation is typically more comfortableforthepatient.
KEY CONCEPT
NOTES
Implant Management l Page 21
AP view Left lateral view

CRM-349606-AC
Before induction testing:
•Useanatomiclandmarkstoconfirmthedeviceispositioned as planned between the 5th and 6th intercostal space at or posterior to the left mid-axillary line.
• Loosen the left arm restraint and lower arm to the patient’sside,palmfacinginward.Thisrelaxesthearm and helps protect the ulnar nerve and brachial plexus.FigureA.
• Removethewedgesupport(ifused).
• Close the deep tissue layer to ensure good tissue-electrodecontact.FigureB.
• Administer long-acting local anesthesia in device pocketandelectrodetunnel.
• Confirmsensingbeforedefibrillationtesting(DFT).
Before induction, loosen arm restraints, close the deep tissue layer,andconfirmsensing.
KEY CONCEPT
NOTES
Induction Testing
Implant Management l Page 22
Prepare Patient
Figure A: Arm position during DFT
Figure B: Close inner tissue layer before DFT5

CRM-349606-AC
Programmed settings:*
• Conditional Shock Zone: OFF• Shock Zone: 170 bpm• Shock Therapy: ON• Shock energy: 65J • Post Shock Pacing: per physician discretion
Induction
• Press Hold to Induce to deliver a 50 Hz, 200 mApulse.ObservetheECGtracingandcalloutinductionprogress.NotethesensingmarkersastheS-ICDdetectsVF.Capacitorchargingbeginswhendetectioncriteriaaremet.
• Upon induction, watch for capture of the pectoralis majormuscleandabductionoftheleftarm.Ifnoobviouscaptureisobserved,it’spossiblethereisnotelemetrylinkorthedeviceanddefibrillationcoilarenotoptimallypositioned.
*Programmingisusuallytheroleofthetechnicalrepresentativeinthelab.
Press Hold to Induce and observe inductionprogress.IfDFTfails,checkdeviceandelectrodeposition.
Plan with staff how long to wait for theS-ICDtodelivershocktherapy.Be prepared to deliver an external rescueshockifneeded.
KEY CONCEPT
NOTES
Induction Testing Perform Induction Test
Implant Management l Page 23
Figure A: Induction screen Figure B: Induction progress

CRM-349606-AC
Good closing technique promotes wound healing and preventsairentrapment.Trappedairmayaffectsensingandtheeffectivenessofshocktherapy.
• Use sterile saline to keep incisions moist during and afterimplant.Instill sterile saline around proximal electrodetoreducetheriskofairentrapment.
• To expel trapped air,applyfirmpressureduringinnerlayerclosure.Palpateinalldirectionswhileobservingsensinginthecorrespondingvector.Turn Therapy OFF during palpation to avoid shock delivery.
• To prevent air entry and entrapment, avoid lifting tissueduringclosure.
• Use multiple suture layerstocloseincisions.Use absorbable sutures for skin layer to improve cosmeticappearance.Removesutureendssotheydon’tprotrudefromtheskin.
Air entrapment
• A wandering baseline is indicative of air entrapment (FigureA).Usepost-operativex-rays(PAandlateralviews)toconfirmairentrapment,whichcanoccuraroundthedeviceorsensingrings.FigureB.
KEY CONCEPT
NOTES
Post-Implant Considerations Wound Closure
Figure A: Wandering baseline10 Figure B: Trapped air at proximal electrode11
Air entrapment generally dissipates withintwotothreedaysofimplant.Early recognition and resolution reduces the need for wound exploration.14
Good closing technique promotes wound healing and prevents air entrapment.
Implant Management l Page 24

CRM-349606-AC
After implant:
• ObtainAPandlateralchestx-raysforreference.
• Apply a topical antiseptic along with a compression dressing.
• Administersufficientlocalanesthesiatomanagepost-implantpain.
• Run the automatic setup with the patient in supine anduprightpositionstoensureadequatesensing.
• Advise patient to avoid manipulating the implanted deviceandelectrode.
• Advise patient to perform light activity but refrain from vigorous activity until the incisions are adequatelyhealed.9
KEY CONCEPT
NOTES
Post-Implant Considerations Patient Care
Compression dressing
During a device change out, open thepocketcompletely.Thepocketmay need to be altered as 1st and 2nd generation devices differ in size andshape.
Gen 1 Gen 2
Follow post-implant patient care guidelines.
Implant Management l Page 25

CRM-349606-AC
High BMI Patients
Thefollowingworkflowadjustmentsmayimproveoutcomes in high BMI patients.15
•Identifyandclearlymarkkeyanatomiclandmarks.
•Tapeupbreastsandloosetissue.Uselargerdrapesandcustomizetothepatient.
• Make the xiphoid incision wide enough to access the deepfasciaandanchortheelectrode.FigureA.
• Be prepared for a deep pocket. Use a headlamp to helpvisualizethepocket.FigureB.
• Take care to correctly sizethepocket.Toolargeapocket may cause device movement or electrode dislodgment.
• Considerusingthelabelledthree-incisiontechnique.
• Pocket formation and wound closure take longer, so booktheORlongerandadjustscheduleasneeded.
•Bariatricinstrumentsmaybeuseful.Weitlanderretractors open in two directions for better visualization.
• Protectagainstinfection.
Planning, preparation, and workflowadjustmentsmayimproveoutcomesinhighBMIpatients.
Acquire post-implant AP and lateral chestx-raystoconfirmelectrodeanddeviceposition.
Figure A: Xiphoid incision in high BMI patient Figure B: Deep pocket in high BMI patient
KEY CONCEPT
NOTES
Challenges
Implant Management l Page 26

CRM-349606-AC
Monitored Anesthesia Care (MAC)
Monitored Anesthesia Care (MAC) requires the services of an anesthesia provider who evaluates the patient, manages sedation and pain control, and monitors hemodynamics, respiratory status, and oxygensaturationduringimplantandrecovery.
• MAC strategies range from no sedation to general anesthesia.16 MAC is well suited to an S-ICD System implant because deep sedation may be needed only duringpocketformation,tunneling,anddefibrillationtesting.16 MAC also allows the implanter to focus on the implant procedure.
• MAC providers use multimodal strategies that combine opioids and nonopioids to provide two or moremechanismsofaction.Thisapproachmayenhance analgesic effects and reduce the risk of opioid side effects.6,7
• Experts believe that preventing pain is more effective than treating pain.6 Thus, medications such as acetaminophen or gabapentin may be given pre-implant.Long-actingbupivacaine(0.25%)may be used because it lasts up to eight hours and providespaincontrolpost-implant.Truncalplaneblock and NSAIDs may also be used to reduce opioid use.6,7
*Comparedtolidocaine,bupivacainehasalongeronsetofaction (5 to 10 minutes) and a limited maximum dosage of 175mg.6Intralipid(20%)iskeptonhandforIVinfusionin the event of anesthetic systemic toxicity 6
MAC gives the responsibility for sedation and pain control to the anesthesia provider so the implanter can focus on S-ICD Systemimplant.
It is important for implanters to review the S-ICD System implant procedure with the anesthesia provider so he or she can plan their sedationandpaincontrolstrategy.
Bupivacaine Oxycodone Ibuprofen
KEY CONCEPT
NOTES
Addendum
Implant Management l Page 27
Acetaminophen Long-acting Opioids Truncal plane block NSAIDS
Multimodal Opioid Sparing Analgesia Strategy16
local anesthesia Gabapentin

CRM-349606-AC
Non-Anesthesiologist Administered Sedation and Analgesia (NASA)
For non-anesthesiologist administered sedation and analgesia (NASA), sedation and pain control are managed by the implanting physician or nurse under thesupervisionofthephysician.Itisanoptionforexperienced implanters who do not have access to an anesthesiaprovider.6,7
• NASA has been safely and effectively used in carefully selected patients at implant centers in theU.S.andEurope.6,7 To ensure recognition and treatment of sedation-related complications, the nurse responsible for patient monitoring should be freeofotherduties.Thisisespeciallyimportantwhen using nonreversible agents such as propofol, whichhasanarrowtherapeuticwindow.6,7
• For implanters with deep sedation privileges, small bolusdosesofetomidate(0.1/kg)arerecommendedover propofol to reduce the risk of cardiovascular andrespiratorydepression.16 Reversible sedatives such as midazolam and opioids are recommended asarelong-actingbupivacaine(0.25%)andpre-implantacetaminophenoroxyodone.16
• Experts caution against NASA for high BMI patients and patients who have severe heart failure or pulmonary hypertension, obstructive sleep apnea, a challenging airway, or who use psychoactive drugs oropioidsforchronicpain.6,7
NASA is managed by the implanting physician or a nurse who can give fullattentiontopatientmonitoring.
The administration of procedural sedationrequiresspecificcompetencies, including patient evaluation and education, cardiovascular monitoring, drug selection and administration, and theuseoftechnologies.
Competency requirements are established by health care facilities, with recommendations from organizations such as the American SocietyofAnesthesiologists(ASA).
KEY CONCEPT
NOTES
Addendum
Implant Management l Page 28
Mild Moderate Deep General anesthesia
Sedation Continuum

CRM-349606-AC
1.SystemAlgorithmValidationTestReportForProject:S-ICDAutomatedScreeningTool(AS)Product: EMBLEMTMS-ICDSystem.Rev.A
2.OldeNordkampLR,ConteG,RosenmöllerBR,etal.Brugadasyndromeandthesubcutaneousimplantablecardioverter-defibrillator.JACC.2016Aug9;68(6):665-666.Availableat:doi:10.1016/j.jacc.2016.05.058.
3.FranciaP,AdduciC,PalanoF,etal.Eligibilityforthesubcutaneousimplantablecardioverter-defibrillatorinpatientswithhypertrophiccardiomyopathy.JCE.2015Aug;26(8):893-899.
4.MauriziN,OlivottoI,OldeNordkampLR,etal.Prevalenceofsubcutaneousimplantablecardioverter-defibrillatorcandidacybasedontemplateECGscreeninginpatientswithhypertrophiccardiomyopathy.Heart Rhythm.2016Feb;13(2):457-463.
5.EMBLEMS-ICD,EMBLEMMRIS-ICDUser’sManual,359481-019ENEurope2016-11.
6.Essandoh,MK,Mark,GE,Aasbo,JD,etal.,Anesthesiaforsubcutaneousimplantablecardioverter-defibrillatorimplantation:PerspectivesfromtheclinicalexperienceofaU.S.panelofphysicians.PacingClinElectrophysiol,201841:p.807–816.
7.Essandoh,MK,Otey,AJ,Abdel-Rasoul,M,etal.,MonitoredAnesthesiaCareforSubcutaneousCardioverter-DefibrillatorImplantation:ASingle-CenterExperience.JCardiothoracVascAnesth,201630(5):p.1228-33.
8.Droghetti,A,BassoRicci,E,Scimia,P,Harizai,F,andMarini,M,Ultrasound-guidedserratusanterior plane block combined with the two-incision technique for subcutaneous ICD implantation.PacingClinElectrophysiol,2018May;41(5):517-523.
9.KnopsRE,BrouwerTF.Implantationofthesubcutaneouscardioverter-defibrillator. In: EllenbogenKA.Clinical Cardiac Pacing, Defibrillation and Resynchronization Therapy 5th Edition. Philadelphia,PA:Elsevier,Inc. 2017:Chapter28.
10.BrouwerTK,MillerMA,etalImplantationofthesubcutaneousimplantabledefibrillator:anevaluationof4implanttechniques.Circ Arrhythm Electrophysiol.2017Jan;10(1):e004663.
11.KnopsRE,OldeNordkampLR,etal.Two-incisiontechniqueforimplantationofthesubcutaneousimplantabledefibrillator.Heart Rhythm. 2013Aug;10(8):1240-1243.
12.BrouwerTF,DriessenAHG,etal.Surgicalmanagementofimplantationrelatedcomplicationsofthesubcutaneousimplantabledefibrillator.JACC Clin Electrophysiol.2016Feb;2(1):89-96.
13.ChinitzJS,NadrausP,etalInappropriateshockswithin24hoursafterimplantationofasubcutaneousdefibrillatorwithatwo-incisiontechnique. Jrnl of Innovations in Cardiac Rhythm Management. 2016March;7:2295-2298.
14.ZipseMM,SauerWH,etal.Inappropriateshocksduetosubcutaneousairinapatientwithasubcutaneouscardiacdefibrillator.Circ Arrhythm Electrophysiol.2014.Aug;7(4):768-770.
15.DroghettiA,LocatelliA,etal.Totallysubmuscularimplantationofsubcutaneousimplantabledefibrillator:asageandeffectivesolutionforobeseandoversizepatients.Clin Case Rep.2016Sep17;4(10):1009-1011.
16.EssandohMK.AnesthesiaandPainControlConsiderations.BostonScientificCorporation.2019.CRM-594804-AA.
Implant Management References
References: Implant Management

CRM-349606-AC
Anatomic Structures
Fascial Layers
Thoracic Wall
SerratusAnterior/LatissimusDorsi
Axillary Nerves
Anatomic Landmarks
Imaginary Planes
Anterior Thoracic view
Axillary Reference Lines
Anatomic Anomalies
PectusExcavatum/PectusCarinatum
Dextrocardia
Anatomic Considerations l Page 1
Anatomic Considerations Contents

CRM-349606-AC
Anatomic Considerations Learning Objectives
After completing this module, you should be able to:
• Describe anatomic structures relevant to the EMBLEMTM S-ICDSystemimplant.
• Refer to anatomic landmarks to:- Plan EMBLEM S-ICD System positioning - Determine incision locations for the device and electrode.
• Discuss how to adjust the implant procedure to accommodateanatomicanomalies.
Anatomic Considerations l Page 2

CRM-349606-AC
Fascial Layers
The fasciallayersarethesuperficialfasciaanddeepfascia.
• The superficial fascia (subcutaneous tissue) is composed of loose connective tissue with an abundance of blood vessels and adipose (fat) cells. The deep fascia consists of dense connective tissue that surrounds and isolates individual muscles.The fascial layers are easily separated by blunt dissection.
• Adiposetissuehasfivetotentimesmoreelectricalresistancethancardiactissue.*Thus,itisimportantto place the EMBLEMTM MRI S-ICD System below adipose tissue.
*RushS,AbildskovJA,McFeeR.Resistivityofbodytissuesatlowfrequencies.Circulation Research.1963:12:40-50.Availableat:circres.ahajournals.org/content/12/1/40
The EMBLEMTM MRI S-ICD System is implantedbelowadiposetissue.
Fascial layers
KEY CONCEPT
NOTES
Anatomic Structures
Anatomic Considerations l Page 3
Fluoroscopy may be helpful when making incisions in high BMI patients.Ametalinstrumentsuchas a scalpel helps assess the depth ofanincision.
Superficial fascia
Deep fascia

CRM-349606-AC
The thoracic wall consists of skin, fascia, muscles, and rib cage, which is formed by the ribs, spine, sternum,andtheirattachments.
• The manubrium is the broad upper part of the sternum.The superior electrode tunnel extends from the xiphoid process to the sternomanubrial junction parallel to and 1 to 2 cm left of the sternal midline.
• The xiphoid process connects to the sternum at the xiphisternal joint. The xiphoid process is the surface landmark for midline surgical incisions and the primary landmark for positioning the EMBLEMTM MRI S-ICD System.
• The pectoralis major is a thick thoracic muscle that attaches to the sternum and extends to the frontofthearmpit(axilla).Itformsthebulkofthe chest wall in males and lies under the breast in females.Thepectoralis minor is a thin thoracic musclethatliesbelowthepectoralismajor.
• The serratus anterior is a fan shaped muscle that coverstheribsonthelateralthoracicwall.
The xiphoid process is the primary landmark for positioning the EMBLEMTMMRIS-ICDSystem.
Skintensionlines(Langer’slines)correspond to the direction of collagenfibersinthedermis.Surgical incisions that run parallel to skin tension lines heal well because the lines of force pull the cutsurfacestogether. Incisions that run across tension lines split collagenfibers,takelongertoheal,andmayresultinmorescarring.
KEY CONCEPT
NOTES
Anatomic Structures Thoracic Wall
Anatomic Considerations l Page 4
Xiphoid process
Pectoralis major
Manubrium
Serratus anterior
Sternum
Xiphisternal joint
Thoracic wall / rib cage

CRM-349606-AC
Anatomic Structures Serratus Anterior / Latissimus Dorsi
For an intermuscular implant, the S-ICD System device is placed between the anterior surface of the serratus anterior and the posterior surface of the latissimusdorsioverthesixthrib.
• The serratus anterior covers the upper eight or nineribsonthesideoftheribcage.Itinsertsintothevertebralborderofthescapula.Theserratusanterior is innervated by the long thoracic nerve (C5, C6, C7) and receives its blood supply from the circumflex scapular artery. FigureA.
• The latissimus dorsi is a broad back muscle that originates along the spine and extends to the mid-axillaryline.Alongwiththepectoralismajor,thelatissimusdorsiliftsthetrunktothearms.Thelatissimus dorsi is innervated by the thoracodorsal nerve (C6, C7, C8) and supplied by the thoracodorsal artery.FigureA.
• Figure B shows an intermuscular implant.
For an intermuscular implant, the device is enveloped between the latissimus dorsi and serratus anterioratthemid-axillaryline.
Placing the entire device under the latissimus dorsi would compromise sensing as the device would be too posterior.
KEY CONCEPT
NOTES
Anatomic Considerations l Page 5
Figure A Left lateral view Figure B: Intermuscular implant
Latissimus dorsi
Serratusanterior

CRM-349606-AC
The axilla is a pyramid-shaped space at the junction of thethoracicwallandupperarm.Itprovidesapassageforbloodvesselsandnervestravelingtothearm.
• The brachial plexus arises from the cervical spine, extends into the axilla, and branches into the arm andhand.Excessivestretchingorcompressionofthe brachial plexus can cause abnormal sensations, suchastingling,burning,orpain.Severeinjurycanpermanentlyimpairarmorhandmovement. Careful patient prep protects the brachial plexus during EMBLEMTM MRI S-ICD System implant.
• The long thoracic nerve passes behind the brachial plexus and runs along the outer surface of the serratusanterior.Damagetothisnervemayresultin pain, loss of shoulder movement, or scapular winging.Becauseofitslong,fairlysuperficialcourse, the long thoracic nerve may be visualized in thedevicepocket.Careful device placement protects the long thoracic nerve from injury.
Careful patient prep protects the brachialplexus.Attentiontodetailwhen placing the device protects thelongthoracicnerve.
Axillary vessels and nerves
KEY CONCEPT
NOTES
Anatomic Structures Axillary Nerves
Anatomic Considerations l Page 6
Brachial plexus
Long thoracic nerve

CRM-349606-AC
Anatomic Landmarks Imaginary Planes
Clinicians use imaginary planes to visualize and describethepositionofanatomicstructures.
• The median plane passes vertically through the center of the body dividing it into right and left sides. Parasagittal planes are parallel to the median plane.
• Coronal planes pass vertically through the body dividing it into front (anterior) and back (posterior) sections.
• Transverse (axial) planes pass horizontally through the body dividing it into upper (superior) andlower(inferior)sections.
Directional terms, arranged as opposites, are used to compare the relative position of two anatomic structures.Examples:
• Medial (middle); lateral (away from the middle)
• Distal (farther from a reference point); proximal (closer to a reference point)
In practice, radiographic images do not lie precisely in a particular plane,butareslightlyoblique.
KEY CONCEPT
NOTES
Anatomic Considerations l Page 7
The median, parasagittal, coronal, and transverse planes provide points of reference for visualizing anddescribinganatomicstructures.
Median (midsagittal) plane Coronal plane Transverse (axial) plane

CRM-349606-AC
Anatomic Landmarks Anterior Thoracic View
The images show the normal position of the heart in the thoracic cavity and the anatomic landmarks used to position the EMBLEMTMMRIS-ICDSystem.
• The heartisposteriortothesternum.About2/3ofitsmassisleftofmidline.Therightsideoftheheartprojects toward the sternum (anterior location); the leftsidetowardthespine(posteriorlocation).
• The left ventricular (LV) apex rests on the thoracicdiaphragm,superiortothexiphoidprocess.It is posterior to the 5th intercostal space, about ninecmfromthemedianplane.
• The thoracic diaphragm separates the thoracic cavityfromtheabdominalcavity.Becauseofitssize, shape, and location, it serves as an important anatomiclandmark.
• The EMBLEM MRI S-ICD System is positioned superiortothexiphoidprocessanddiaphragm.FigureB.
The position of the EMBLEM S-ICD System is dictated by the position oftheheartinthethoraciccavity.
KEY CONCEPT
NOTES
Anatomic Considerations l Page 8
5th rib
6th rib
FigureA:Anteriorview FigureB:Implanteddevice/electrode
DiaphragmLV apex

CRM-349606-AC
Anatomic Landmarks Axillary Reference Lines
Axillary lines of reference are used to position the S-ICDSystemdevice.
• The mid-axillary line starts at the deepest part of thearmpit.Theanterior axillary line runs along the axillary fold near the thoracic wall; the posterior axillary linealongtheaxillaryfoldneartheback.
• When placed in the intermuscular pocket, the device is posterior to the left mid-axillary line. This position ensuresthereissufficienthearttissuebetweenthedevice and electrode for appropriate sensing and shocking(nottooanterior;nottooposterior).
When placed in the intermuscular pocket, the device is posterior to theleftmid-axillaryline.
The initial pocket incision is made neartheanterioraxillaryline.
KEY CONCEPT
NOTES
Anatomic Considerations l Page 9
Figure A: Axillary lines of reference Figure B: Implanted device
Mid-axillary line A
nter
ior a
xilla
ry li
ne
Post
erio
r axi
llary
line

CRM-349606-AC
Anatomic Anomalies Pectus Excavatum / Pectus Carinatum
Pectus excavatum and pectus carinatum are congenital anomalies that require consideration when implanting the EMBLEMTMMRIS-ICDSystem.
• Pectus excavatum is caused by excessive growth ofconnectivetissuebetweentheribsandsternum.It causes the sternum and anterior ribs to sink inward.TheimagesinFigureAshowhowpectusexcavatumcandisplacetheheart’snormalpositionwithinthethoraciccavity.Thedegreeofdeformityinpectusexcavatumvariesfrompersontoperson.
• Pectus carinatum is caused by the outward growth of connective tissue between the ribs and sternum.Itcausesthesternumtopushforward,givingthechestabird-likeappearance.Pectuscarinatum may be asymmetric, with one side of the chestaffectedmorethantheother.Insomecases,pectus carinatum occurs on one side of the chest andpectusexcavatumontheother.Somepatientsdeveloparigidchestwall.FigureB.
• A pre-implant CT scan and chest x-rays help identify anatomic landmarks and plan placement of the deviceandelectrode.Fluoroscopyensuresgoodvisualizationwhentunnelingalongthefascialplane.
Pectus excavatum can displace theheart’snormalposition.Pectuscarinatum causes the sternum topushforward.Imagingbeforeimplant helps identify landmarks and plan device and electrode placement.
Pectus excavatum occurs in 1 of 400 children with a 3:1 male to femaleratio.Itusuallypresentsinthefirstyearoflifeandworsensasthechildgrows.1
Pectus carinatum occurs in 1 of 1,500 children with a 4:1 male to femaleratio.Itusuallypresentsin childhood and worsens during puberty.2
KEY CONCEPT
NOTES
Anatomic Considerations l Page 10
CT image
X-ray image
Figure A: Pectus excavatum Figure B: Pectus carinatum

CRM-349606-AC
Anatomic Anomalies Dextrocardia
Dextrocardia is a congenital anomaly in which the heart is situated right of midline and the apex points to theright.Thegreatvesselsarealsoreversed.
• Isolated dextrocardia is the reversed positioning of theheartandgreatvessels. Dextrocardia with situs inversus is the reversed positioning of all thoracic andabdominalorgans.Otherdefectsmaybepresent.FigureB.
• Dextrocardia requires reversed positioning of the EMBLEMMRIS-ICDSystem.Thedistalelectrodeis placed 1 cm right of the sternal midline and the deviceattherightmid-axillaryline.Pre-implantMRI images and clear labeling of the right and left sideshelpsidentifyanatomiclandmarks.
Dextrocardia requires reversed positioning of the EMBLEM MRI S-ICDSystem.Pre-implantimagesand left-right labelling help identify landmarks and plan device and electrodeplacement.
Dextrocardia occurs in 1 of 10,000 children.Diagnosismaybedelayedifcardiovascularfunctionisnormal.3
KEY CONCEPT
NOTES
Anatomic Considerations l Page 11
Figure A: Normal heart Figure B: Isolated dextrocardia

CRM-349606-AC
Reference: Anatomic Considerations
1.IglesiasJ.Chest Wall Deformities: Pectus Carinatum and Excavatum.Availableat:www.cookchildrens.org/pediatricsurgery.AccessedMay1,2015,
2. UCSFPediatricSurgery.Pectus Carinatum.Availableat:www.pedsurg.ucsf.eduAccessedMay1, 2015,
3.ZahkaKG.Cardiovascularproblemsoftheneonate.In:MartinRJ,FanaroffAA,WalshMC,eds.Fanaroff and Martin’s Neonatal-Perinatal Medicine.9thed.Philadelphia,Pa:MosbyElsevier;2010:part8.
Anatomic Considerations l References

CRM-349606-AC
EMBLEMTM MRI S-ICD Brief Summary
Indications for UseTheS-ICDSystemisintendedtoprovidedefibrillationtherapyforthetreatmentoflife-threatening ventricular tachyarrhythmias in patients who do not have symptomatic bradycardia, incessant ventricular tachycardia, or spontaneous, frequently recurring ventricular tachycardiathatisreliablyterminatedwithanti-tachycardiapacing.
ContraindicationsUnipolar pacing and impedance-based features are contraindicated for use with the S-ICD System.
WarningsRead this manual thoroughly before using the S-ICD System to avoid damage to the pulse generatorand/orsubcutaneouselectrode.Suchdamagecanresultinpatientinjuryordeath.Forsinglepatientuseonly.Donotreuse,reprocess,orresterilize.AllBostonScientificS-ICDimplantablecomponentsaredesignedforusewiththeBostonScientificorCameronHealthS-ICDSystemonly.ConnectionofanyS-ICDSystemcomponentstoanoncompatiblecomponentwillresultinfailuretodeliverlife-savingdefibrillationtherapy.AlwayshaveexternaldefibrillationequipmentandmedicalpersonnelskilledinCPRavailableduringimplantandfollow-uptesting.Using multiple pulse generators could cause pulse generator interaction, resulting inpatientinjuryoralackoftherapydelivery.Testeachsystemindividuallyandincombinationtohelppreventundesirableinteractions.ConcomitantuseoftheS-ICDSystemandimplantedelectromechanical devices (for example a ventricular assistdevice, VAD; or implantable insulin pump or drug pump) can result in interactions that could compromise the function of the S-ICD, the co-implanteddevice,orboth.Electromagnetic(EMI)ortherapydeliveryfromthecoimplanteddevicecaninterferewithS-ICDsensingand/orrateassessment,resultingininappropriatetherapyorfailuretodelivertherapywhenneeded.Inaddition,ashockfromtheS-ICDpulsegeneratorcoulddamagethecoimplanteddeviceandcompromiseitsfunctionality.Tohelppreventundesirable interactions, test the S-ICD system when used in combination with the co-implanteddevice,andconsiderthepotentialeffectofashockonthecoimplanteddevice.Handle the components of the S-ICD System with care at all times and maintain proper sterile technique.Donotmodify,cut,kink,crush,stretchorotherwisedamageanycomponentoftheS-ICDSystem.Usecautionhandlingthesubcutaneouselectrodeconnector.Donotdirectlycontacttheconnectorwithanysurgicalinstrumentssuchasforceps,hemostats,orclamps.Use appropriate anchoring techniques as described in the implant procedure to prevent S-ICD Systemdislodgementand/ormigration.UsecautionwhenplacingamagnetovertheSICDpulsegeneratorbecauseitsuspendsarrhythmiadetectionandtherapyresponse.Inpatientswith a deep implant placement (greater distance between the magnet and the pulse generator) magnetapplicationmayfailtoelicitthemagnetresponse.DonotexposeapatientwithanimplantedS-ICDSystemtodiathermy.DonotexposeapatienttoMRIscanning.Advisepatients to seek medical guidance before entering environments that could adversely affect the operation of the active implantable medical device, including areas protected by a warning noticethatpreventsentrybypatientswhohaveapulsegenerator.Thepulsegeneratormaybemore susceptible to low frequency electromagnetic interference at induced signals greater than 80uV.TheS-ICDSystemhasnotbeenevaluatedforpediatricuse.

CRM-349606-AC
EMBLEMTM S-ICD System Brief Summary
PrecautionsForspecificinformationonprecautions,refertothefollowingsectionsoftheproductlabeling: clinical considerations, sterilization and storage, implantation, device programming, environmental and medical therapy hazards, hospital and medical environments, home and occupational environments, follow-up testing, explant and disposal and supplemental precautionaryinformation.AdvisepatientstoavoidsourcesofEMIbecauseEMImaycausethepulsegeneratortodeliverinappropriatetherapyorinhibitappropriatetherapy.
Potential Adverse EventsPotential adverse events related to implantation of the S-ICD System may include, but are not limitedto,thefollowing:Acceleration/inductionofatrialorventriculararrhythmia,adversereactiontoinductiontesting,allergic/adversereactiontosystemormedication,bleeding,conductor fracture, cyst formation, death, delayed therapy delivery, discomfort or prolonged healingofincision,electrodedeformationand/orbreakage,electrodeinsulationfailure,erosion/extrusion,failuretodelivertherapy,fever,hematoma/seroma,hemothorax,improperelectrode connection to the device, inability to communicate with the device, inability to defibrillateorpace,inappropriatepostshockpacing,inappropriateshockdelivery,infection,keloidformation,migrationordislodgement,muscle/nervestimulation,nervedamage,pneumothorax,post-shock/post-pacediscomfort,prematurebatterydepletion,randomcomponent failures, stroke, subcutaneous emphysema, surgical revision or replacement of thesystem,syncope,tissueredness,irritation,numbnessornecrosis.Patientswhoreceivean S-ICD System may develop psychological disorders that include, but are not limited to, the following:depression/anxiety,fearofdevicemalfunction,fearofshocks,phantomshocks.
Refer to the product labeling for specific indications, contraindications, warnings/precautions and adverse events. Rx only. (Rev. A)