Hypertension Presentation
Transcript of Hypertension Presentation
HYPERTENSIONDetection, Evaluation
and Non-pharmacologic Intervention
Misbah Keen, MD, FAAFPAct. Asst. Professor Family MedicineUniversity of Washington School of MedicineSeattle WA
Problem Magnitude Hypertension( HTN) is the most common
primary diagnosis in America. 35 million office visits are as the primary
diagnosis of HTN. 50 million or more Americans have high BP. Worldwide prevalence estimates for HTN may
be as much as 1 billion. 7.1 million deaths per year may be attributable to
hypertension.
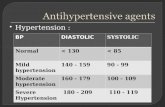
Definition
A systolic blood pressure ( SBP) >139 mmHg and/or
A diastolic (DBP) >89 mmHg. Based on the average of two or more
properly measured, seated BP readings.
On each of two or more office visits.
Accurate Blood Pressure Measurement
The equipment should be regularly inspected and validated.
The operator should be trained and regularly retrained. The patient must be properly prepared and positioned
and seated quietly for at least 5 minutes in a chair. The auscultatory method should be used. Caffeine, exercise, and smoking should be
avoided for at least 30 minutes before BP measurement.
An appropriately sized cuff should be used.
BP Measurement
At least two measurements should be made and the average recorded.
Clinicians should provide to patients their specific BP numbers and the BP goal of their treatment.
Follow-up based on initial BPmeasurements for adults*
*Without acute end-organ damagewww.nhlbi.nih.gov
Prehypertension SBP >120 mmHg and <139mmHg and/or
DBP >80 mmHg and <89 mmHg.
Prehypertension is not a disease category rather a designation for individuals at high risk of developing HTN.
Pre-HTN Individuals who are prehypertensive are not
candidates for drug therapy but Should be firmly and unambiguously advised to
practice lifestyle modification Those with pre-HTN, who also have diabetes
or kidney disease, drug therapy is indicated if a trial of lifestyle modification fails to reduce their BP to 130/80 mmHg or less.
Isolated Systolic Hypertension
Not distinguished as a separate entity as far as management is concerned.
SBP should be primarily considered during treatment and not just diastolic BP.
Systolic BP is more important cardiovascular risk factor after age 50.
Diastolic BP is more important before age 50.
Frequency Distribution of Untreated HTN by Age
Isolated Systolic HTN
Isolated Diastolic HTN
Systolic Diastolic
HTN
Hypertensive Crises
Hypertensive Urgencies: No progressive target-organ dysfunction. (Accelerated Hypertension)
Hypertensive Emergencies: Progressive end-organ dysfunction. (Malignant Hypertension)
Hypertensive Urgencies
Severe elevated BP in the upper range of stage II hypertension.
Without progressive end-organ dysfunction.
Examples: Highly elevated BP without severe headache, shortness of breath or chest pain.
Usually due to under-controlled HTN.
Hypertensive Emergencies Severely elevated BP (>180/120mmHg). With progressive target organ dysfunction. Require emergent lowering of BP.
Examples: Severely elevated BP with: Hypertensive encephalopathy Acute left ventricular failure with pulmonary
edema Acute MI or unstable angina pectoris Dissecting aortic aneurysm
Types of Hypertension Primary HTN: also known as
essential HTN. accounts for 95%
cases of HTN. no universally
established cause known.
Secondary HTN: less common cause
of HTN ( 5%). secondary to other
potentially rectifiable causes.
Causes of Secondary HTN Common
Intrinsic renal disease Renovascular disease Mineralocorticoid
excess Sleep Breathing
disorder
Uncommon Pheochromocytoma Glucocorticoid excess Coarctation of Aorta Hyper/hypothyroidism
Secondary HTN-Clues in Medical History
Onset: at age < 30 yrs ( Fibromuscular dysplasi) or > 55 (athelosclerotic renal artery stenosis), sudden onset (thrombus or cholesterol embolism).
Severity: Grade II, unresponsive to treatment. Episodic, headache and chest pain/palpitation
(pheochromocytoma, thyroid dysfunction). Morbid obesity with history of snoring and
daytime sleepiness (sleep disorders)
Secondary HTN-clues on Exam
Pallor, edema, other signs of renal disease.
Abdominal bruit especially with a diastolic component (renovascular)
Truncal obesity, purple striae, buffalo hump (hypercortisolism)
Secondary HTN-Clues on Routine Labs
Increased creatinine, abnormal urinalysis ( renovascular and renal parenchymal disease)
Unexplained hypokalemia (hyperaldosteronism)
Impaired blood glucose ( hypercortisolism)
Impaired TFT (Hypo-/hyper- thyroidism)
Renal Parenchymal Disease
Common cause of secondary HTN (2-5%)
HTN is both cause and consequence of renal disease
Multifactorial cause for HTN including disturbances in Na/water balance, vasodepressors/ prostaglandins imbalance
Renal disease from multiple etiologies.
Renovascular HTN Atherosclerosis 75-90% ( more common in
older patients) Fibromuscular dysplasia 10-25% (more
common in young patients, especially females) Other
• Aortic/renal dissection• Takayasu’s arteritis• Thrombotic/cholesterol emboli• CVD• Post transplantation stenosis• Post radiation
Complications of Prolonged Uncontrolled HTN
Changes in the vessel wall leading to vessel trauma and arteriosclerosis throughout the vasculature
Complications arise due to the “target organ” dysfunction and ultimately failure.
Damage to the blood vessels can be seen on fundoscopy.
Effects On CVS
Ventricular hypertrophy, dysfunction and failure.
Arrhithymias Coronary artery disease, Acute MI Arterial aneurysm, dissection, and
rupture.
Effects on The Kidneys
Glomerular sclerosis leading to impaired kidney function and finally end stage kidney disease.
Ischemic kidney disease especially when renal artery stenosis is the cause of HTN
The Eyes
Retinopathy, retinal hemorrhages and impaired vision.
Vitreous hemorrhage, retinal detachment Neuropathy of the nerves leading to
extraoccular muscle paralysis and dysfunction
Retina Normal and Hypertensive Retinopathy
Normal Retina Hypertensive Retinopathy A: HemorrhagesB: Exudates (Fatty Deposits)C: Cotton Wool Spots (Micro Strokes)
A B
C
Stage III- Hemorrhages (H), Cotton Wool Spots and Exudats (E)
H
E
Stage IV- Stage III+Papilledema
Patient Evaluation Objectives (1) To assess lifestyle and identify other
cardiovascular risk factors or concomitant disorders that may affect prognosis and guide treatment
(2) To reveal identifiable causes of high BP (3) To assess the presence or absence of
target organ damage and CVD
(1) Cardiovascular Risk factors Hypertension Cigarette smoking Obesity (body mass index 30 kg/m2)≥ Physical inactivity Dyslipidemia Diabetes mellitus Microalbuminuria or estimated GFR <60 mL/min Age (older than 55 for men, 65 for women) Family history of premature cardiovascular disease (men
under age 55 or women under age 65)
(2) Identifiable Causes of HTN Sleep apnea Drug-induced or related causes Chronic kidney disease Primary aldosteronism Renovascular disease Chronic steroid therapy and Cushing’s
syndrome Pheochromocytoma Coarctation of the aorta Thyroid or parathyroid disease
(3) Target Organ Damage Heart Left ventricular hypertrophy Angina or prior myocardial infarction Prior coronary revascularization Heart failure Brain Stroke or transient ischemic attack Chronic kidney disease Peripheral arterial disease Retinopathy
History Angina/MI Stroke : Complications of HTN,
Angina may improve with b-blokers Asthma, COPD: Preclude the use of b-
blockers Heart failure: ACE inhibitors indication DM: ACE preferred Polyuria and nocturia: Suggest renal
impairment
History-contd. Claudication: May be aggravated by b-
blockers, atheromatous RAS may be present Gout: May be aggravated by diuretics Use of NSAIDs: May cause or aggravate HTN Family history of HTN: Important risk factor Family history of premature death: May
have been due to HTN
History-contd.
Family history of DM : Patient may also be Diabetic
Cigarette smoker: Aggravate HTN, independently a risk factor for CAD and stroke
High alcohol: A cause of HTN High salt intake : Advice low salt intake
Examination Appropriate measurement of BP in both arms Optic fundi Calculation of BMI ( waist circumference also
may be useful) Auscultation for carotid, abdominal, and femoral
bruits Palpation of the thyroid gland.
Examination-contd.
Thorough examination of the heart and lungs
Abdomen for enlarged kidneys, masses, and abnormal aortic pulsation
Lower extremities for edema and pulses Neurological assessment
Routine Labs EKG. Urinalysis. Blood glucose and hematocrit; serum
potassium, creatinine ( or estimated GFR), and calcium.
HDL cholesterol, LDL cholesterol, and triglycerides.
Optional tests urinary albumin excretion. albumin/creatinine ratio.
Goals of Treatment Treating SBP and DBP to targets that are
<140/90 mmHg Patients with diabetes or renal disease, the BP
goal is <130/80 mmHg The primary focus should be on attaining the
SBP goal. To reduce cardiovascular and renal morbidity
and mortality
Benefits of Treatment
Reductions in stroke incidence, averaging 35–40 percent
Reductions in MI, averaging 20–25 percent
Reductions in HF, averaging >50 percent.
Lifestyle Changes Beneficial in Reducing Weight
Decrease time in sedentary behaviors such as watching television, playing video games, or spending time online.
Increase physical activity such as walking, biking, aerobic dancing, tennis, soccer, basketball, etc.
Decrease portion sizes for meals and snacks.
Reduce portion sizes or frequency of consumption of calorie containing beverages.
Other Resources
Chronic Kidney Disease Information GFR Calculator www.nephron.com
Hyperlipedemia Information Adult Treatment Panel 3 Guidelines www.nhlbi.nih.gov/guidelines/cholesterol/index.htm