Hypertension
-
Upload
dhavalshah4424 -
Category
Health & Medicine
-
view
5 -
download
0
description
Transcript of Hypertension

Hypertension in Diabetes Mellitus

Hypertension: The Silent KillerFacts & Figures
50 million Americans & 1 billion worldwide affected
Most common primary care diagnosis (35 million visits annually)
Normotensive at age 55 have 90% lifetime risk of Hypertension
Continuous & consistent relationship with CVD Between ages 40-70, starting from 115/75 CVD risk doubles with each increment of 20/10

Data from King H et al. Diabetes Care. 1998;21:1414-1431.
Top Three Countries for Diabetes

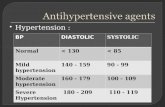
Blood Pressure (mm Hg) Category
Systolic Diastolic
<120 and <80 Normal
120-139 or 80-89 Prehypertension
140-159 or 90-99 Stage 1 hypertension
≥160 or ≥100 Stage 2 hypertension
JNC 7 Definition
Hypertension 2003;42:1206-52
What is Hypertension?

Types of Hypertension
Essential hypertension
90%
No underlying cause
Secondary hypertension
Underlying cause

Causes of Secondary Hypertension
Renal Parenchymal Vascular Others
Endocrine Neurogenic Miscellaneous Unknown

Hypertension: Predisposing factors
Age > 60 years Sex (men and postmenopausal women) Family history of cardiovascular disease Smoking High cholesterol diet Co-existing disorders such as diabetes, obesity and
hyperlipidaemia High intake of alcohol Sedentary life style

National High Blood Pressure Education Program Working Group. Arch Intern Med. 1993;153:186-208.
Hypertension: A Significant CV and Renal Disease Risk Factor

CV Mortality Risk Doubles with Each 20/10 mm Hg BP Increment*
*Individuals aged 40-69 years, starting at BP 115/75 mm Hg.CV, cardiovascular; SBP, systolic blood pressure; DBP, diastolic blood pressureLewington S, et al. Lancet. 2002; 60:1903-1913.JNC VII. JAMA. 2003.
CVmortality
risk
SBP/DBP (mm Hg)
0
1
2
3
4
5
6
7
8
115/75 135/85 155/95 175/105

Pathophysiology of hypertension in DM
The derangements in glucose, lipid, and protein metabolism lead to
functional abnormalities in autonomic nerves
overproduction of vasoconstrictor factors that increase vascular tone
concomitant reductions in the biologic actions of vasodilators
resulting in an increase in BP

Vasoactive substancesCause structural changes in the CV system and in the kidney through effects on:
Vascular smooth muscle cell hypertrophy
Hyperplasia, angiogenesis, cellular apoptosis, macrophage/fibroblast activation with augmented formation of extracellular matrix
Adhesive interactions of circulating leukocytes and platelets with the vessel wall

Processes important in the development or perpetuation of hypertension in diabetics
Alterations in the balanced production of vasodilator & vasoconstrictor substances from the endothelium
Altered vascular smooth muscle responses to these substances
Resistance of peripheral tissues & selected lipid metabolic processes to the actions of insulin
Alterations in the cellular & extracellular elements that comprise the vessel wall

Reactive oxygen species (ROS)
Diabetics—increased metabolic processes that produce reactive oxygen species (ROS)
ROS serve as signaling mechanisms mediate many of the functional & structural vascular abnormalities observed in diabetics
Thus, hypertension in diabetics probably results from a series of interrelated, complex functional and structural abnormalities

Management: JNC 7 GUIDELINES

What are the goals of therapy?
<140/90 for patients without diabetes or renal disease
Most patients who achieve their systolic goal will also achieve their diastolic goal
<130/80 for patients with diabetes or renal disease
JNC VII Guidelines

But… There are Reasons for Inadequate BP Control
Poor compliance to lifestyle modifications
Acceptance of inadequate control by physician
Difficulty achieving BP control with one agent/suboptimal regimens
BP goals are more aggressive than in previous years
Lack of compliance due to: Perceived side effects of antihypertensive medication(s) Frequency of dosing/multiple agents to attain control
JNC VI. Arch Intern Med. 1997

And that leads to…
Refractory hypertension –
Defined by a blood pressure of at least 140/90 or at least 130/80
in patients with diabetes or renal disease despite adherence to
treatment with full doses of at least three antihypertensive
medications, including a diuretic.
JNC VII Guidelines

Refractory hypertension is primarily a systolic and age related problem
It affects 5-30% of the general population with hypertension
Patients with refractory hypertension have an increased risk of Stroke, Aortic Dissecting Aneurysm, Myocardial Infarction, Congestive Heart Failure and Renal failure compared to other hypertensive patients
J Hypertens. 2005;23(8):1441-4, Hypertension. 1988;11(3 Pt 2):II71-5, Minerva Med. 2003;94(4):201-14.
Refractory Hypertension leads to

Causes of Refractory Hypertension
The main reasons why hypertension may be unresponsive to a standard antihypertensive treatment include:
Incorrect diagnosis, Secondary forms of hypertension, Inadequate antihypertensive drug regimen, Associated factors or diseases, Use of non-steroidal anti-inflammatory drugs, Non-compliance with antihypertensive treatment.
Although non-compliance may also be common in patients with well-controlled blood pressure, poor compliance with drug treatment is generally recognized as a major cause of unsatisfactory blood pressure control.

Approach to Resistant Hypertension
Establish “true resistance”
Measure BP accurately
Consider “White Coat Hypertension”
Consider “Pseudoresistance”
Medication Adherence
Consider secondary causes

Accurate BP Measurement
“Persons should be seated quietly for 5 minutes with feet on the floor and the arm supported at heart level”
Cuff must be appropriately sized (cuff bladder must encircle 80% of the arm)
Check both arms and a leg (or palpate pulses carefully)
Caffeine and Tobacco can transiently raise BP substantially

Approach to Resistant Hypertension
Establish “true resistance”
Measure BP accurately
Consider “White Coat Hypertension”
Consider “Pseudoresistance”
Medication Adherence
Consider secondary causes

White Coat Hypertension
20-30% of Apparently Resistant Hypertension May be due to “White-Coat Hypertension”
Patients with WCH have an increased risk of CV events and often have some degree of end organ damage
Use home or ambulatory monitoring to sort out

Approach to Resistant Hypertension
Establish “true resistance”
Measure BP accurately
Consider “White Coat Hypertension”
Consider “Pseudoresistance”
Medication Adherence
Consider secondary causes

Pseudoresistance
Pseudohypertension
Non-adherence may account for up to 50% of resistant cases
Inadequate Regimen Especially inadequate diuretic component
Interfering medicines and substances also need to be considered NSAIDs Excessive Alcohol, Caffeine, or Tobacco Excessive Salt Intake Drugs of Abuse Oral contraceptives

Approach to Resistant Hypertension
Establish “true resistance”
Measure BP accurately
Consider “White Coat Hypertension”
Consider “Pseudoresistance”
Medication Adherence
Consider secondary causes

The Importance of Adherence
Only 1/2 to 2/3 of patients take at least 75% of prescribed antihypertensive medicines1
Of those taking < 75%, only 37% achieved BP goal Of those taking ≥ 75%, 81% achieved goal
In a recent BMJ study, the same rate of adherence was found in both responsive and resistant patients (82%)2
1. Arch Int Med 1987; 147:1393-1396
2. BMJ 2001; 323:142

Techniques to Improve Adherence
Education of the patient Increases awareness but less effect on behavior
Minimize the number of pills Combination pills (ACEI/Diuretic, ARB/Diuretic, ARB/Ca-
blocker, etc.)
Increase the frequency of visits Use of care managers

Approach to Resistant Hypertension
Establish “true resistance”
Measure BP accurately
Consider “White Coat Hypertension”
Consider “Pseudoresistance”
Medication Adherence
Consider secondary causes

Secondary Causes of Hypertension
Obstructive Sleep Apnea
Obesity (Metabolic Syndrome)
Endocrinopathies Hyperaldosteronism, thyroid problems,
pheochromocytoma
Kidney Disease Renal Insufficiency and Renal Artery Stenosis

Management of Refractory Hypertension

Management of Refractory Hypertension - 1 The therapeutic outline should be optimized with the different classes of
antihypertensives, including the use of a diuretic in adequate therapeutic doses.
Two different strategies can be used in the attempt of finding an appropriate therapeutic outline for each patient, besides basing it on pathophysiologic knowledge: 1) The empiric approach based on the systematic changes of antihypertensive drugs with the use of associations of two, three or four different pharmacological classes together with adequate dose of thiazide diuretics. The use of loop diuretics follows the same orientation applied to hypertension of other degrees.
2) The rational approach considering the hemodynamic profile and the levels of activity of plasma renin allows to divide this group of patients into volume-dependent and renin-dependent, making it possible to better choose the antihypertensive for each subgroup.
Prevalence of high hyperactivity found in young hypertensive patients and elevation of the levels of activity of renin guide the preferential use of beta-blockers in association with thiazides.
N Engl J Med. 2001;344(1):3-10, Med. 2000;107(5):57-70.

Management of Refractory Hypertension - II
If available, the quantification of plasma renin can address the treatment with drugs.
If the patient presents high plasma renin activity (>0.65 ng/mL/h), the treatment begins with angiotensin converting enzyme (ACEI), AT1 angiotensin II receptor blockers and beta-blockers.
If the plasma renin activity becomes low (<0.65 ng/mL/h), the patient is classified as volume-dependent and should be treated preferentially with a diuretic and calcium channels blockers.

Management of Refractory Hypertension - III
Central nervous alpha-blockers (prazosin, doxazosin, alpha-
metildopa and clonidine), direct vasodilators (hydralazine
and minoxidil) may be used in resistant hypertension when
association with other drugs fails.
In patients with high plasma aldosterone, the associated
use of mineralocorticoid antagonists (spironolactone and
eplerenone) can be effective to reduce the blood pressure
besides delaying the structural alterations that characterize
the cardiovascular remodeling.

Study performed at Mayo Clinics with Refractory Hypertensive patients
A study performed at Mayo Clinics (US) with 104 refractory
hypertensive patients demonstrated that there was a control of
blood pressure and reduction in vascular resistance when the
pharmacological treatment was based on hemodynamic non-
invasive measurements (thoracic bioimpedance) when compared
with the empiric choice of classes of antihypertensives and
adjustments of doses to the specialist's criterion regarding arterial
hypertension.
Hypertension. 2002;39(5):982-8.

Thank You