Hypertension 2016: Are we Hypertension up or down? Peter ...
Hypertension
-
Upload
deepak-solanki -
Category
Documents
-
view
436 -
download
12
Transcript of Hypertension

Blood pressure : • Pressure exerted by the blood column on the
lateral walls of the arteries.
Factors affecting arterial B.P.:• Age• Sex• Habitus• Climate• Diurnal variation• Exercise, emotions, meals, heredity, gravity,
posture and regional variation.

Determinants of blood pressure :
1. Cardiac output
×
2. Peripheral resistance
Peripheral resistance Viscosity of blood
Peripheral resistance 1/ Velocity of blood

Measurement of blood pressure
Non invasive Invasive methodsmethod
By mercury Aneroid Electronic BPSphygmomanometer meter Meter
Palpatory Auscultatory Oscillatory method method method
Kortkoffs soundNote: • Resting adults : DBP Disappearance of Kortkoffs sound• Adults after exercise children, pregnancy hyperthyroidism DBP
Muffling• Keep the arm at the level of the heart• Appropriate cuff size.

Regulation of blood pressure
Various interconnected mechanism work together to maintain normal MAP
1. Rapidly acting mechanisms
• Acts within seconds to minutes
• Loose their capacity after few hours
• Circulatory reflexes
• Main center is VMC

Receptors Operates Stimulation Afferents Cent-re
Efferent Effects
(a) Baroreceptor reflex
Stretch receptor- Carotid sinus & aortic arch- atria
60-20 mmHg of MAP
Distension IX & X nerve
VMC Sympathetic and vagus
VasodilationVenodilatation BP HR
(b) Chemoreceptor reflex
Carotid & aortic bodies
40-100 mmHg of MAP
PCO2/H+ /
pH Sinus nerve VMC Sympathetic
and vagusPeripheral vasoconstriction BP HR
(c) Bezold Jarisch/Coronary chemoreflex
Left ventricle MI Substance from infracted tissueSeratonin, capsasin etc
Vagus Apnoea f/b rapid breathing BP HR

(d) Pulmonary chemoreflex
Juxtracapillary in walls of alveoli
Hyper-inflation of lug
Seratonin, capsacin etc.
- do -
(e) Somatosympathetic reflex
Muscles Exercise surgery
Pain Somatic nerve
VMC Sympathetic nerve
BP
(f) Cushings reflex
VMC ICT Hypoxia Hypercapnia
Direct stimulation
symp-discharge
BP HR (reflexly)
(g) Bain Bridge reflex
Increased venous return Increase heart rate

2. Moderately acting mechanisms • Hormones : Epinephrine, Nor epinephrine, AVP,
angiotensin I, histamine, ANP, VIP,• Endothelin products: Endothelin-1, NO, kinins,
TxA2
3. Long term regulatory mechanisms • Slow to begin• Comes to equilibrium in 3-10 days
1. Direct mechanism: by kidneys call as renal fluid mechanism
2. Indirect mechanism: aldosterone and renin angiotensin system.

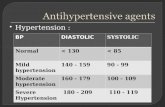
Hypertension
• An adult is considered to manifest hypertension when SBP/DBP are 140/90 mmHg or more on at least 2 occasions measured at least 1-2 weeks apart.
• For anaesthetists: on the basis of 2/3 readings taken over a period of hours.

Classification of hypertension
JNC VI classification:Category SAP (mmHg) DAP (mmHg)
Optimal < 120 < 80
Normal 120-129 80-84
High normal 130-139 85-89
Hypertension
Stage 1 140-159 90-99
Stage 2 160-179 100-109
Stage 3 > 180 > 110
Note: Where patients SBP and DBP falls into 2 different categories, the higher category is selected.

JNCDET VII classification
Category SAP (mmHg) DAP (mmHg)
Normal < 120 < 80
Pre Hypertensive 120-139 80-89
Hypertensive
Stage 1
Stage 2
140-159
> 160
90-99
> 100

Terminologies used for hypertension
1. Isolated systolic hypertension: SBP > 140 mmHg, DBP < 90 mmHg, elderly
2. Essential hypertension : No cause found
3. Secondary hypertension
4. Accelerated hypertension : Markedly elevated (recent over previous episodes) associated with retinal damage. But without papilledema.
5. Malignant hypertension: Markedly elevated hypertension (diastolic > 140 mmHg) + retinopathy + hypertensive encephalopathy.
6. Complicated hypertension : Hypertension + end organ damage
7. White coat hypertension

Classification of hypertension according to etiology
1. Primary/essential/idiopathic hypertension : • 95% of all cases • No cause found
Possible factors : • Multifactorial genetic defects• Environmental : salt intake, obesity, smoking,
alcohol, tobacco, occupation, large family size, inadequate intake of K and Ca.
• Generalized cell membrane defect

• Increased sympathetic activity• Sleep disorders• Hypercholesterolemia, diabetes, insulin
resistance• Increased renin secretion• Deficiency of vasodilators such as PG, NO
2. Secondary hypertension • < 5% of all the cases• Etiology is present

Types
(A) Systolic and diastolic hypertension with increased PVR.
(1) Renal• Renal vascular disease e.g. renal artery stenosis.• Renal parenchymal diseases e.g. GN
(acute/chronic), pyelonephritis• Renal transplantation• Renin secreting tumors• Other e.g. PCK, diabetic nephropathy, arterial
nephrosclerosis.

(2) Endocrine• Cushings syndrome (excessive glucocorticoid)• Congenital adrenal hyperplasia• Conns syndrome (primary hyperaldosteronism)• Pheochromocytoma• Myxedema• Acromegaly
(3) Neurogenic• Psychogenic• Spinal cord injuries• GBS• Dysautonomia• Increased ICT• Diencephalic syndrome.

(4) Drugs• OCP• Glucocorticoids• Mineralocorticoids• Cyclosporine• Tyramine• Sympathomimetics
(5) Miscellaneous• Toxemia of pregnancy• Coarctation of aorta• PAN• Hypercalcemia• Increased intravascular volume• Acute intermittent porphyria

(B) Systolic hypertension with wide pulse
pressure
1. Decreased compliance of aorta
(arteriosclerosis; aortic rigidity)
2. Increased stroke volume : AR, thyrotoxicosis,
fever, AV fistula, PDA

PATHOPHYSIOLOGY OF ESSENTIAL HYPERTENSION
1. CVS
systemic BP
after load
acceleration ofatheromatous Concentric LVH Endomyocardial plaque fibrosis
Myocardial O2 requirement
Coronary insufficiency myocardial compliance
Infarction CCF COdysrrythmia
Pulmonary oedema

2. Peripheral blood vessels
Arterial and arteriolar wall thickening
Decreased internal diametre
• Vascular contraction leads to abnormally large increase in BP
• Vascular relaxation leads to greater than expected decrease in BP.
• Relative hypovolumia ( intravascular volume)• Rehydration following relaxation causes rebound
hypertension.

3. Nervous system• Cerebral haemorrhage• Encephalopathy• Atherosclerosis in cerebral blood vessels • Cerebra infarcts TIA• Chronic hypertension causes a shift to the right
in cerebral and renal autoregulation• Decrease in cerebral blood flow and cerebral
ischaemia occurs at higher BP than in normal patients.
Clinical pearls:1. 25% decrease in MAP reaches the lower limit of
autoregulation.2. A 55% decrease in MAP reaches symptomatic
brain hypoperfusion.

4. Fundus changes: Retinal haemorrhages, exudates + papilloedema
5. Renal system:
Arteriosclerotic lesions of the arterioles and glomerulus
Decrease GFR and tubular dysfunction
Proteinuria and microscopic hematuria
• Adversely affects renal autoregulation • End organ damage to kidneys. • Prerenal hypoperfusion due to sudden and
sustained decreased in BP.

TREATMENT OF HYPERTENSION
1. Life style modifications:• Salt restriction• Stop smoking• Limit alcohol intake• Reduce weight• Relaxation • Regular exercise

2. Pharmacological treatment
Site of action
Drug & Dose Indications Contraindications Side effects
Diuretics
Renal tubule ThiazidesO : 12.5-25 mg daily
Mild hypertension As adjunctElderlyheart failure
GOUT, DM, Primary aldosteronism, dyslipidemia
HypokalemiaHyepruricemiaHypercalcemiaHypercholestrolemiaHyperglycemia
Loop diureticsO : 20-80 mg BD/TDS
Mild hypertensionAs adjunctParticularly with renal failure
- do - HypokalemiaHyepruricemiaHypocalcemiaHypercholestrolemiaHyperglycemia
Potassiumsparing SpironolactoneO : 25 mg BD/QIDAmilorideD : 5-10 mg OD
Hypertension due to hyper mineralo-corticoid
Renal failure HyperkalemiaDiarrheaGynecomastia

Anti-adrenergic agent
Central ClonidineD : 0.005-0.6 mg OD
Renal disease with hypertension Premedication
Bradycardia Sedation XerostomiaRebound hypertension
Methyl dopaD : 250-1000
mg BDD : IV 250-1000
mg every 4-6 hours
Malignant hypertension
PheochromocytomaHepatic disease
Drowsiness Dry mouthFatiguePositive coombs test
Autonomic ganglia
TrimethaphanD : IV 1-6 mg/ min
- do - DMCoronary artery disease
Postural hypotension Constipation Visual symptoms
Nerve endings
GuanethidineD: O 10-150 mg OD

Alpha receptors25
PrazosinD : O 1-10 mg OD
Mild to moderate hypertensionProstatism
Caution in the elderly First dose syncope Orthostatic hyportension Fluid retention Sedation
TerazosinD: 1-20 mg OD
- do - - do - - do -
PhentolamineD: IV 30 mcg/
kg
Pheochromo-cytoma
Severe CA disease TachycardiaDizziness
Beta receptors
Propanolol D: O 10-20 mg BD/QID ; IV 10-25 mcg/kg.MetaprololAtenololEsmolol D: bol. IV .2-.5mg/kg
Mild to moderate hypertension specially with hyperdynamic circulation
CHF Heart blockDM
Bradycardia BronchospasmCHFMask hypoglycemia
Alpha/Beta receptors
Labetalol D : IV 0.1-0.25 mg/kgD : O 100-600 mg BDCarvedilol
- do - - do - - do -

Vasodilators
Vascular smooth muscle
Hydralazine D : IV 10-50 mg every 6 hrs
Malignant hypertension
Lupus TachycardiaAnginaLupus like syndrome
MinoxidilD : 2.5-40 mg BD
Severe hypertension
Severe CA disease Tachycardia Hair growth Pericardial effusions
NitroprussideD : 0.5-8 g/ kg/min
Malignant hypertension
DiphoresisNauseaCyanide toxocity
ACE inhibitors
Captopril EnalprilFisinoprilBenazipril
Mild to severe hypertension Heart failureLV dysfunctionDiabetic retinopathy
Renal failurePregnancy B/L Renal artery Stenosis
CoughAngioedemaHyperkalemiaLoss of tasteProteinuria

Angiotensin receptor antagonist
Losartan Valsartan
Mild to severe hypertension Renal arteryStenosis
Renal failurePregnancy B/L Renal artery Stenosis
HyperkalemiaHypotension
Calcium channel blockers
Vascular smooth muscle
VerapamilNifedipineFelodipine
Mild to moderate hypertension
Heart failure 2o or 3o block
HypercalemiaTachycardia GIT disturbances

ANAESTHETIC MANAGEMENT
For elective surgery
• DBP > 110 mmHg should not undergo elective surgery until there hypertension has been corrected over few days.
For emergency surgery
• Treat pain and anxiety
• Reduce BP to around 160/100 mmHg
• Careful fluid replacement

PREOPERATIVE EVALUATION
Aims of preoperative evaluation:
1. To determine whether hypertension is primary or secondary
2. Evaluate end organ damage : LVH, CHF, angina, CVA, PVD, renal insufficiency
3. Determine adequacy of systemic blood pressure control
4. Review pharmacology of drugs

HISTORY AND EXAMINATION
(A) Whether hypertension is primary/secondary
• H/o repeated UTI : suggests renal origin
• H/o weight gain or emotional liability : cushings syndromes
• H/o weight loss with episodic headaches, palpitation, diaphoresis, postural dizziness : pheochromocytoma
• H/o polyuria, polydipsia, muscle weakness, hypokalemia: primary aldosteronism

(B) For associated complications
• H/o headache localized especially to occipital regions and occurring on waking up, dizziness, palpitation : severe hypertension
• Episodes of chest pain, dyspnoea, edema : Cardiac failure, angina
• Episodes of weakness/dizziness : TIA
• Episodes of epistaxis : vascular changes
• Episodes of haematuria: Renal vascular changes
• Severe sharp pain : dissection of aorta
• Fundus examination : Hypertensive retinopathy

Preoperative investigations
Always included: • Full blood count, DLC• Blood urea and creatinine• Electrolyte• Hb & haematocrit• Microscopic urinalysis• Blood glucose• Lipid profile• Chest X-ray • 12 lead ECG
Usually but
not always included • TSH• Serum calcium and
phosphate• Echocardiogram

Special studies to screen for secondary hypertension
• Renovascular disease : Renal scan, renal duplex, doppler flow studies, MRI angiosraphy
• Pheochromocytoma: 24 hours urine assay for creatinine, metanephrines and catecholamines
• Cushings syndrome: overnight dexamethasone suppression test, 24 hr urine cortisol and creatinine
• Primary aldosteronism: Plasma aldosterone : renin activity ratio.

Methods to reduce perioperative risks
1. Adequate perioperative BP control • Continue all antihypertensives up to the day of surgery
except diuretics. • Delay elective surgery if SBP> 200mmHg or DBP >
120mmHg until lowered to 140/90 mmHg over several weeks.
• Acute control within hour is not advisable.
2. Measures to prevent hypertensives episodes • Use of agents to attenuate hemodynamic responses to
intubation incision and extubation. • Opioids - fentanly, alfentanyl • Antihypertensive - Esmolol, labetalol, clonidine,
enalpril.• Lignocaine I.V. & spray.

3. Hydration
4. Choice of agents with minimal hemodynamic effects
• Thiopentone over propofol• Pethidine over morphine • Vecuronium and cis atracurium over atracurium.
5. Analgesics

Monitoring • Pulse • BP invasive and non-invasive • ECG• CVP• Urine output • Invasive pulmonary artery catheter if LVF
dysfunction• TEE for LV function
Premedication • Sympathetic activation can cause BP to rise by 20-
30 mmHg & HR by 15-20 BPM. • Aims to avoid hypertension and hypotension,
tachycardia • Benzodiazepines : Lorazepam 2-4mg 2 hours prior
to surgery. • If possible avoid atropine

Induction
• Intravenous agents• Many inducing agents are vasodilators • Avoid propofol and ketamine • Use of opioids reduces dose of inducing
agents. • Thiopentone dose titrated against
response

Intubation
Hypertensive response to laryngoescopy can be reduce by
Use of opioids : Alfentanil : 15-30 g/kg IV at the time of injection Remifentanil : 1 g/kg IV of inducing agent
Fentanyl : 50-150 g/kg IV 3 mins before Sufentanyl : 30 g/kg IV induction
Lignocaine - IV 1.5 mg/kg & spray
Duration should not exceed 15 sec.
If duration likely to exceed 15 sec. sodium nitropusside 1-2 g/kg IV before laryngoescopyesmolol 100-200 g/kg IV 15 sec. before induction

Maintenance
• GOAL: Adjust the depth of anaesthesia to minimize wide fluctuations in blood pressure
• Alpine anaesthesia : Exhibit swings in arterial pressure (graphical presentation)
• Volatile agents : • Cardiovascular depressant • Poorly soluble desflurane and sevoflurane
permit more rapid changes in alveolar concentration and hence depth.
• Opioids reduces the amount of volatile agents required
• N2O can be used safely

Intraoperative hypertension
Causes• Poorly controlled preoperative hypertension • Hypertension secondary to laryngoscopy and
intubation • Hypercapnia : Hypoventilation, depleted
sodalime, CO2 during laparoscpy etc.
• Hypoxemia • Inadequate regional anaesthesia/excessive
surgical site stimulation or light anaesthesia.• Drug related: inadverent infusion of
vasopressors.

• Surgical causes: use of 10% phenylephrine drops in ophthalmic surgery
• Malignant hyperthermia, thyrotoxicosis, pheoch-romocytoma
• Distended bladder
Treatment • Correct the cause before treating blood
pressure with antihypertensives. • Increase the depth of anaesthesia

Intraoperative hypotension
Causes • Direct effect of anaesthetic agents• Inhibition of the sympathetic nervous system• Loss of the baroreceptor reflex
Treatment • Reduce the depth of anaesthesia• Correct hypovolumia• Small dose vasopressors
EMERGENCE • Avoid pain, hypoxia, coughing • Patient should be returned to ward when
haemodynamically stable

ACUTE POSTOPERATIVE HYPERTENSION
Causes: • Pain• Emergence excitement• Hypercarbia• Intolerance of endotracheal tube• Full bladder• Hypervolaemia• Hypothermia• Withdrawal of chronic therapy• After carotid endarterectomy

Risk associated• Loss of vascular anastomosis• Intracranial bleeding• Myocardial ischaemia
Treatment depends on • The clinical situation • Etiology• Level of analgesia• Degree of hypertension
Drug used• Labetalol 0.1-0.5 mg/kg IV every 10 min• Hydralazine 2.5-10 mg IV every 10-20 min• Nitroprusside 0.5-10 g/kg/min IV

HYPERTENSIVE EMERGENCIES
Common causes of hypertensive crisis• Antihypertensive drug withdrawal (e.g. clonidine)• Autonomic hyperactivity• Collagen-vascular diseases• Drugs (e.g., cocaine, amphetamines)• Glomerulonephritis (acute)• Head trauma• Neoplasias (e.g., pheochromocytoma)• Preeclampsia & eclampsia• Removascular hypertension

Clinical manifestations: • Hypertensive encephalopathy : Headache,
altered consciousness and confusion, CVA, Fundus changes
• Acute aortic dissection• Acute myocardial infarction• Acute cerebral vascular accident• Acute hypertensive renal injury : Renal failure
with oliguria and/or hematuria. • Acute congestive heart failure

Management
Key: prompt recognition and initiation of treatment
• Does the patient have any prior or current complaints and what medications, prescription has the patient taken.
• Palpation of pulses in all extremities
• Fundoscopic examination
• Routine investigations

Drug Dose Length of action
Nitropruside 0.25 mcg/kg/min IV 2-5 minutes
Nitroglycerin 5 mcg/min IV 3-10 minutes
Esmolol 250-500 mcg/min for 1 min, then 50-100 mcg/kg/min
10-20 minutes
Propranolol 1-4 mg IV 1-2 hours
Labetolol 10-200 mg IV (2 mg/min) 1-4 hours
Nicardipine 5-15 mg/hour IV 1-4 hours
Nifedipine 10 mg sublingual or oral 2-5 hours
Diazoxide 30 mg boluses IV (max 300 mg) 4-12 hours
Hydralazine 5-20 mg IV 4-12 hours

REGIONAL ANAESTHESIA
• Hypertension is not a contraindication
• But spinal and epidural causes unpredictable and profound hypotension.
• Hypertensives may have LVH and deranged autoregulation, thus these organs will cope poorly with low perfusion pressure.
• Local blocks should always be considered.

JNCDET Guidelines for anaesthesia in hypertensive patients
• Stage 1 hypertension : little or no increased risk of peri-operative cardiac morbidity, therefore, anaesthesia and surgery can proceed as planned.
• Stage 2 & Stage 3 : • More of a delimma• Balance has to be stuck• Options available: to ignore the elevated arterial BP
to institute acute treatment
to defer surgery for a period of weeks

Various studies• Prys-Roberts & colleagues: demonstrated an
association between poorly controlled hypertension and intraoperative MI and arrythmias.
• Another prospective study: demonstrated an increasing incidence of postoperative myocardial ischaemia with increasing arterial pressure.
• Studies also demonstrate that very rapid control of blood pressure with drugs such as sublingual nifedipine is associated with morbidity and mortality.
• Charleson and colleagues: demonstrated that those with more than 1 hour of a decrease in MAP > 20 mmHg and those with > 15 mins of an increase in MAP > 20 mmHg were at greatest risk of complications. On the basis of these findings; best course for anaesthetists is to defer anaesthesia and surgery in patients with stage 3 hypertension to allow the arterial pressure to be treated.