hmo membership information - Blue Cross Blue Shield of ...HMO Membership Information BCBSIL Provider...
Transcript of hmo membership information - Blue Cross Blue Shield of ...HMO Membership Information BCBSIL Provider...

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 1
Membership Information..........................................................................................................2
IPA Selection .................................................................................................................. 2 Identification Cards ......................................................................................................... 2
Eligibility List ............................................................................................................................3
How To Read the Eligibility List ..............................................................................................4
Sample Benefit Plan Listing ............................................................................................ 5 Explanation of Eligibility List Codes on Alphabetical Listing............................................ 6 Sample Member Eligibility List ........................................................................................ 7 Explanation of Eligibility List Codes on Capitation Reconciliation Report........................ 8 Sample Capitation Reconciliation Report........................................................................ 9 Explanation of Eligibility List Codes on the Capitation Summary Report ...................... 10 Sample Capitation Summary ........................................................................................ 11 Explanation of Eligibility List Codes on the Activity Counts Page.................................. 12 Sample Activity Counts Report ..................................................................................... 13 Sample Explanation of the Member Counts and Capitation by Benefit Plan................. 14 Explanation of the Age and Gender Counts Page ........................................................ 15 Explanation of New Members Address List Page ......................................................... 16
Procedure If a Member Does Not Appear On the Eligibility List ........................................17
When the Member Has a Question About a Membership Issue .........................................18
Unassigned Members (597/598 Clinic)..................................................................................19
IPAs Request for Member Transfer (Ask Out Policy) ..........................................................19
Discontinuance and Replacement Policy.............................................................................20
Transition Policy for New and Prospective Members .........................................................22
Transition Policy for Current Members ................................................................................22
Retroactive IPA Member Changes ........................................................................................22
Verifying Membership ............................................................................................................22

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 2
Membership Information IPA Selection
The HMO requires that all members enrolled with the HMO select an IPA site. Dependents (a spouse and/or children) can choose a different IPA than the subscriber. The provision of the Woman’s Principal Health Care Provider (WPHCP) legislation allows a female member to have direct access to an OB/GYN physician within her Primary Care Physician’s IPA. Identification Cards
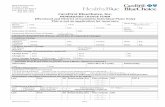
All eligible HMO members are issued an Identification Card.
IN CASE OF EMERGENCY -- CALL YOUR MEDICAL GROUP/PRIMARYCARE PHYSICIAN PHYSICIAN
TO HOSPITALS OR PHYSICIANS: The enrollee named on the face of the card, while currentlyenrolled, is entitled to benefits. All medical and hospital services, except emergencies, must be pre-authorized by the Medical Group/Individual Practice Association (IPA) named on the face of this card.
TO HOSPITALS OR PHYSICIANS: Please file claims with your local BlueCross BlueShield Plan.
TO MEMBER: If a provider does not submit your claim on your behalf, please file the claim to theaddress listed below. To locate a provider when you are out of your service area or when traveling callthe BlueCard Access number listed below.
Customer Service #: 1-800-892-2803
Blue Cross and Blue Shield of IllinoisP.O. Box 805107Chicago, Illinois 60680-4112
Chemical Dependency Network #: 1-800-346-3986
HMO-WPHCP-w/Rx
BlueCard Access #: 1-800-810-BLUEPharmacy Program #: 1-800-423-1973BlueCard Provider Eligibility #: 1-800-676-BLUEQB4103
An Independent Licensee of theBlue Cross and Blue Shield Association
SMITH, MarySubscriber
Participant's Name
Identification No.
125 ABC MEDICAL CENTERMedical Group Number & Name
Group No.
Benefit Plan:Plan Codes: 621/121
Mary SmithXOH851234435
H12345
HMO IllinoisA Blue Cross HMO
(708) 444-4444 01-01-08
125 ABC MEDICAL CENTERWPHCP
(708) 444-4444 01-01-08
3DK20
www.bcbsil.com
Office Visit $20Wellness Copay $20Specialist Copay $20Emergency $90
RPRIMEBIN: 011552PCN: ILDR
Identification cards are generated when:
The member becomes eligible Employer changes the contract Member changes his/her name Member changes IPA IPA Administrative Change, such as name or phone number
If a member has the Prescription Drug benefit, that will be reflected in the lower right hand corner of the identification card.
Each identification card contains the following information:
Subscriber Name - Employee Participant’s Name - Each member will receive their own card Benefit Plan - The code assigned for the member’s benefits Effective Date - The member’s most current effective date (If a member has a status
change, or IPA change - the date will reflect the date of the change - not the original effective date with the HMO)
IPA Name and Number - the unique number of the IPA that is assigned by the HMO and selected by the member.
IPA Phone Number Prescription Drug Benefit Information (if the member has this benefit)

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 3
Eligibility List
Prior to the first of each month, the HMO will provide the IPA with an alphabetical listing of all members enrolled at that facility. This list will be electronically posted to the secure internet site. This list is referred to as the Eligibility List. This List details the members who are eligible to receive services at the IPA during the month.
A member may have an ID card and not appear on the Eligibility List. This will occur when the membership application is processed after the Eligibility List cut-off date. It is also possible that members may have ID cards after their eligibility has ended, since the HMO does not retract ID cards from cancelled members.
If a member has an ID card, but does not appear on the Eligibility List, you should call the HMO Membership Department at (800) 892-2803. There is a Voice Response Unit for Eligibility Verification or if you have access, you can check NDAS Online or our secured internet membership system for eligibility.
Note: You should verify membership every visit prior to services being provided.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 4
How To Read the Eligibility List
It consists of several different parts:
The Member Eligibility List provides the alphabetical listing of enrolled members. This listing will indicate any member changes processed since the last monthly listing.
The Capitation Reconciliation Report indicates the current and/or retro PCP
capitation being paid to or deducted from the IPA.
The Capitation Summary Page provides a summary of the total monthly capitation paid to the IPA by category.
The Activity Counts Page provides a summary of monthly enrollment data and
changes.
The Member Counts and Capitation by Benefit Plan pages provide a detailed summary of monthly enrollment by Benefit Plan. Refer to the next page for a sample Benefit Plan listing.
The Age and Gender Counts Page that provides a summary of monthly enrollment data
based on the age and gender.
The New Member Address Listing provides an address listing for all new members to your IPA.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 5
Sample Benefit Plan Listing

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 6
Explanation of Eligibility List Codes on Alphabetical Listing Refer to page 7 for a sample Member Eligibility List report. 1. Medical Group Number A unique number assigned by the HMO to each IPA.
2. Medical Group Name The name of the IPA.
3. Eligibility Period The period which the Eligibility List covers.
4. Member Name Name of the member: all dependents are listed under the
subscriber’s last name.
5. Relationship Indicates relationship of the member to the subscriber
6. Gender Sex of the member
7. Birth Date The birth date of the member.
8. Group Number Identifies the subscriber's employer number.
9. Subscriber Number Member's identification number (which is usually the Subscriber's social security number, but may not be).
10. Pln Cov Desc A five-character code indicates the benefit plan for the member.
11. Office Co-pay A specified charge that a member pays for a specified PCP service.
12. PCP – Effective Date The member’s effective date with the IPA for PCP selection.
13. Alternative PCP – Clinic
The member’s effective date with the different IPA for PCP selection that differs from your WPHCP IPA.
14. WPHCP Effective Date The female member’s effective date with the IPA for WPHCP selection.
15. Alternative WPHCP – Clinic The female member’s effective date with the different IPA for WPHCP selection that differs from your PCP IPA.
16. MSG - (Special Message Field) Indicates that a change has been made in the status of the member’s contract since the last eligibility list ran. This special message will only appear on the Eligibility List once – printed on the month immediately following the change. This field is also used to communicate a special membership status. If MP is listed, indication that member is Medicare Primary. If OD is listed, indication that member is an over-age dependent.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 7
Sample Member Eligibility List

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 8
Explanation of Eligibility List Codes on Capitation Reconciliation Report
Refer to page 9 for a sample Capitation Reconciliation Report.
Field Name Data Type Length Description PROV_ID Number 3 Contracting Entity Number PROV_SEQ_NBR Number 3 Medical Group Number GRP_NBR Character 6 Group Number SUB_LAST_NM Character 20 Subscriber("Family")Last Name SUB_ID_NBR Character 12 Subscriber Number LAST_NM Character 20 Member Last Name -Could differ from subscriber Last Name FIRST_NM Character 20 Member First Name BEN_PLAN_ABBR_CD Character 6 HMO/BlueAdvantage Benefit Plan OFFC_CPAY_AMT Decimal 6 Office Copay ELIG_DET_PCP_EFF_DT Character 10 PCP Effective Date(MM-DD-YYYY) ALT_PCP_CLC_ID Number 3 Alternate PCP Medical Group Number(Optional) ELIG_DET_WPHCP_EFF_DT Character 10 WPHCP Medical Group Effective Date (MM-DD-YYYY) ALT_WPHCP_CLC_ID Number 3 Alternate WPHCP Medical Group Number(Optional) ELIG_CAT_CD Character 2 Eligibility Category Code: MP- Medicare Primary, OD-Overaged Dependent PCP_RETRO_CAP_AMT Decimal 9 PCP Retroactive Cap Amount PCP_CURR_CAP_AMT Decimal 9 PCP Cap Amount for current Elig Period WPHCP_RETRO_CAP_AMT Decimal 9 WPHCP Retroactive Cap Amount WPHCP_CURR_CAP_AMT Decimal 9 WPHCP Cap Amount for current Elig Period ELIG_PCP_CHG_CD Character 2 PCP Change Code: MA-Add, MC-Cancel, TI-Transfer In, TO-Transfer Out, RI-Reinstate, NN-Name Change, etc. ELIG_WPHCP_CHG_CD Character 2 WPHCP Change Code: MA-Add, MC-Cancel, TI-Transfer In, TO-Transfer Out, RI-Reinstate, NN-Name Change, etc. ELIG_PCP_CLC_END_DT Character 10 PCP End Date(Cancel or Transfer Out)(MM-DD-YYYY)(Optional) ELIG_WPHCP_CLC_END_DT Character 10 WPHCP End Date(Cancel or Transfer Out)(MM-DD-YYYY)(Optional) DOB Character 10 Date of Birth of Member(MM-DD-YYYY) REL_CD Character 3 Member Relationship Code (SUB-Subscriber, SPS-Spouse, DEP-Dependent) GNDR_CD Character 1 Member Gender Code (F-Female, M-Male) AGE Number 3 Member Age STR_ADDR_LN_1 Character 40 Member Street Address 1 (Populated only for new Member) STR_ADDR_LN_2 Character 40 Member Street Address 2 (Populated only for new Member) APARTMENT_UNIT_NBR Character 5 Optional Apt Unit Number (Populated only for new Member) CTY_NM Character 25 Member City Name (Populated only for new Member) ST_CD Character 2 Member State (Populated only for new Member) ZIP_CD Character 9 Member Zip Code (Populated only for new Member) PGM_ID Character 2 Member Managed Care Program/Network "01" = HMOI; "02" = BlueAdvantage BEN_PLAN_CHG_IND Character 1 Benefit Plan Change Indicator SUB_SSN Character 12 Subscriber SSN MEM_PROV_ID Number 9 Member Provider Number MEM_PROV_SEQ_NBR Number 5 Member Provider Sequence Number WPHCP_PROV_ID Number 9 Women's Principle Health Care Provider Number WPHCP_PROV_SEQ_NBR Number 5 Women's Principle Health Care Provider Sequence Number PROV_NM Character 50 Provider Name WPHCP_NM Character 50 Women's Principle Health Care Provider Name ELIG_PER_FR_DT Character 10 Eligibility List From Date (MM-DD-YYYY) ELIG_PER_TO_DT Character 10 Eligibility List To Date (MM-DD-YYYY)

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 9
Sample Capitation Reconciliation Report

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 10
Explanation of Eligibility List Codes on the Capitation Summary Report
Refer to page 11 for a sample Capitation Summary Report.
1. Current Capitation The amount of monthly capitation paid for members assigned to IPA for PCP.
2. Retroactive Capitation The amount of retro monthly capitation paid or deducted for member activity with a prior month effective date.
3. Total Capitation The amount of the total monthly capitation for PCP & WPHCP for IPA HMO members.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 11
Sample Capitation Summary

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 12
Explanation of Eligibility List Codes on the Activity Counts Page
Refer to page 13 for a sample Activity Counts Report.
1. Total Subscribers Total number of subscribers effective with IPA for each category for the month.
2. Total Dependents Total number of dependents effective with IPA for each category PCP, WPHCP and Medicare Primary for the month.
3. New Additions Total number of new additions with IPA for each category PCP, WPHCP and Medicare Primary effective for the current month.
4. Cancellations Total number of cancellations with IPA for each category effective for current month.
5. Transfer In Total number of members transferred in from other IPA’s effective for the current month.
6. Transfer Out Total number of members transferred to another IPA for the current month.
7. Reinstates Total number of members reinstated effective for the current month.
8. Totals Members Total active members. This count constitutes PCP & WPHCP members.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 13
Sample Activity Counts Report

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 14
Sample Explanation of the Member Counts and Capitation by Benefit Plan
This page provides a detailed summary of monthly enrollment by Benefit Plan, age & sex. See page 5 of this section for a sample of the Benefit Plan listing.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 15
Explanation of the Age and Gender Counts Page
This page breaks down the total number of Non-Medicare Primary and Medicare Primary members into Age and Gender categories.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 16
Explanation of New Members Address List Page
Each month the IPA receives a listing of all new HMO members and their home addresses. This list is updated by HMO only when a member sends in current address information. Therefore, the information on the list may not be correct. The IPA should use the active member list in conjunction with the IPA’s address information to insure an accurate member address.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 17
Procedure If a Member Does Not Appear On the Eligibility List
Occasionally, an eligible member will not appear on the Eligibility List. This can be for a variety of reasons. If this occurs, the IPA should do the following:
1. Verify the subscriber’s name. The member’s surname may be different. Look on the list
under the subscriber’s last name.
2. Check the online membership system. Or if applicable call HMO Membership Department at (800) 892-2803.
If membership is verified, the IPA should perform services for the member, and should check the next month’s Eligibility List to verify capitation was received for the member. (See Retroactive Capitation in the Payment/Compensation to the IPA Section of this manual) If it is not, the IPA should contact the HMO Membership Department - see the Contacts Section for more information.
If membership cannot be verified, the IPA should:
1. Explain this to the member and have the member check with his/her employer to verify
coverage, and
2. The IPA should either:
Perform services and charge the member at the time of service. Refund the money to the member if he/she appears on the Eligibility List, or
Perform services and bill the member if he/she does not appear on the
next Eligibility List.
Note: You should call the HMO Membership Department if the member does not appear on the next eligibility list.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 18
When the Member Has a Question About a Membership Issue
If the member loses or needs a new ID card the member should call the HMO at (800) 892-2803 or go online to www.bcbsil.com.
If the member wants to change their Primary Care Physician, the member should contact
the IPA directly.
If the member wants to change IPAs: the member should call the HMO at (800) 892-2803.
If the member wants to add/delete a dependent: the member should contact the Benefits
office of their Employer. The member will fill out a request form. Generally, the contract change must be made within 30 days of the qualifying event.
Typically, a subscriber may not add a dependent of a dependent (e.g., a grandchild) to the contract, unless he/she has legally adopted, or obtained an interim court order of adoption for that dependent. If the IPA becomes aware that this has occurred, or if they have knowledge that an individual listed as a dependent does not meet the definition of a dependent, the IPA should notify the HMO Membership Department - see the Contacts Section of this manual. Services should not be denied until such time as the individual has been removed from the Eligibility List.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 19
Unassigned Members (597/598 Clinic)
There are occasions where a member will be eligible with the HMO but does not have a valid IPA assignment. The HMO will place these members in the 597 or 598 IPA.
A member may be placed in a 597 Status if:
1. The member does not indicate an IPA selection on the enrollment application.
2. If the member is asked out of an IPA and fails to select a new IPA in the designated time
frame.
3. The HMO can not decipher the IPA selection on the enrollment application.
4. The member chooses an invalid IPA selection.
A member may be placed in a 598 Status if the member chooses a closed or non-affiliated IPA.
The member will not receive an ID Card. The member will receive a package of information requesting them to choose an IPA. No ID card will be issued until an IPA has been chosen.
If a member does not choose an IPA within 30 days, the subscriber’s HMO will assign the subscriber and dependents, if applicable to an IPA based on geographic location. If a member wishes to change the IPA assignment, the member should call HMO membership at (800) 892-2803.
IPAs Request for Member Transfer (Ask Out Policy)
Refer to the HMO Policy and Procedure Section of this manual for information on requesting that a member be transferred out of the IPA.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 20
Discontinuance and Replacement Policy
The HMO Administrative office will be notified by the HMO Marketing Department when a member has Discontinuance and Replacement benefits. The HMO Administrative office will notify the IPA.
1. Discontinuance of Blue Cross/Blue Shield HMO Coverage
Under this employer group coverage benefit, if the entire employer group cancels its HMO policy, and there is a totally disabled subscriber, or totally disabled dependent of an eligible subscriber, the totally disabled member will be considered still eligible for HMO benefits. This policy only applies when the entire employer group cancels its Blue Cross/Blue Shield HMO policy, and not when an individual subscriber or family is terminated.
The member should have a statement completed by an attending physician
identifying the total disability. The member will keep their same group number and will be assigned section #7777. The HMO is responsible for providing services rendered in connection with the
disability, until the person is no longer disabled, or until the end of the prior policy’s discontinuance of coverage extension of benefits provision or for a one (1) year period, whichever comes first.
The HMO Network Consultant will notify the IPA that the member is eligible for limited benefits for a one-year period.
The HMO will pay the IPA monthly capitation for a one year period (no exceptions). 2. Replacement of Discontinued Group Coverage
When the HMO is replacing another carrier’s group policy, persons who are totally disabled on the effective date of this coverage will be eligible for coverage under the Blue Cross/Blue Shield of Illinois HMO plan.
Such totally disabled persons will be entitled to all of the benefits under the HMO plan, to be coordinated with benefits under the prior group policy. The prior group policy will be considered the primary coverage for all services rendered in connection with the disability, until the person is no longer totally disabled, or until the end of the prior policy’s discontinuance of coverage extension of benefits provision, or the end of twelve months, whichever occurs first. Primary Care Physician referral remains in effect for such totally disable persons.
Blue Cross/Blue Shield of Illinois HMOs is responsible for providing all medically necessary services to the member, with the exception of those services previously identified under the disabling illness, injury or condition clause.
If the dependent of an eligible member is still totally disabled at the end of the prior policy’s discontinuance of coverage extension of benefits period, the dependent’s coverage under the HMO will not be terminated. Should a subscriber continue to be totally disabled at the end of the prior policy’s discontinuance of coverage of benefits periods, such person’s coverage and the coverage of his/her dependents under the HMO plan will be terminated at that time.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 21
Discontinuance and Replacement Policy (cont.) 3. If a member changes the Insurance Policy
If an eligible HMO member’s policy is terminated on the date in which the member is hospitalized, the member’s coverage will be terminated on that date, unless the member’s employer group has purchased Extension of Benefits coverage.
Likewise, if a new HMO member becomes effective on the date he/she is undergoing hospitalization, the IPA will be responsible for coordination of care at the time of notification to the IPA by the HMO of the member’s status.

HMO Membership Information
BCBSIL Provider Manual—Rev 10/08 22
Transition Policy for New and Prospective Members
Please refer to the HMO Policy and Procedure Section of this manual for detailed information on this policy.
Transition Policy for Current Members If a physician leaves an IPA, the IPA must notify the members in writing who are currently seeing that physician. The letter must include the following Transition of Care language: If you and /or one of your family members are currently in an ongoing course of treatment and wish to receive transition of care services, you may request that you continue seeing your current physician for up to 90 days from the date of this notification. To receive this transition of care service you must submit a request in writing within 30 days of this notification or call: Blue Cross and Blue Shield of Illinois Consumer Affairs Unit 300 East Randolph, 27th Floor Chicago, Illinois 60601 (312) 653-6600
Retroactive IPA Member Changes
Please refer to the HMO Policy and Procedure Section of this manual for detailed information on retroactive IPA member changes.
Verifying Membership Call (800) 892-2803 to verify membership. Remember to always check the member’s ID card.