Hepatitis C Research Paper Denise Final
-
Upload
denise-t-robinson -
Category
Documents
-
view
22 -
download
3
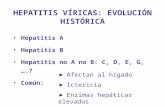
Transcript of Hepatitis C Research Paper Denise Final

Denise RobinsonLake Worth High School
April 10, 2010
FAU Medical Outreach Program
Hepatitis C “The Silent Epidemic”

Table of Contents
Basic Anatomy of Effected Organs and Basic Structure of A Virus 3
Etiology 6
Signs and Symptoms 7
Diagnosis 8
Treatment 11
Prognosis 12
Prevention……………………………………………………………………………………......15
2

Hepatitis C is a spherical, single-stranded RNA virus that, over a long period of time,
affects the entire body. Before giving an explanation of the virus and how it works, a breakdown
of the anatomy of the affected organs must be given. First of all, the word “Hepatitis” means
inflammation of the liver which makes the liver, not only a perfect place to start, but also the
basis of the disease. Weighing about three pounds in an adult, the liver is located in the upper
third of the abdomen, resting “on the stomach, the intestines, and the right kidney” (Horn, 2005,
p. 25). “About 13% of the body’s blood is in the liver” (Horn, 2005, p. 29). Eighty percent of
the blood that travels from the heart into the liver goes through the portal veins; the other twenty
percent enter through the hepatic artery. The deoxygenated blood is then returned to the heart
through the hepatic vein (Horn, 2005).
“The liver performs more than 500 important functions” (Horn, 2005, p. 30). One of its
most important jobs is to be the body’s filter. Without it, our blood would be clogged with fats;
there would be no way to get rid
of the toxins in our body, and the
breaking down of food wouldn’t
even be possible. Edible
products that have the ability to
travel within the bloodstream,
“must first flow through the
liver” (Horn, 2005, p. 27). The
liver produces a greenish
substance called bile which carries toxins away from the liver. Bile is efficiently collected from
the liver cells through the hepatic bile duct system. About half of the bile that is produced is
3

delivered by the common bile duct to the small intestine. The other half is sent straight to the
gallbladder which acts as a storage unit for the bile (Horn, 2005, p. 29). Once fatty foods are
consumed, the gallbladder “squirts” bile into the small intestine so it can help break down the
fats (Zein and Edwards 3).
The liver has other important functions as well. For one thing, it helps fight off infection
by “secreting some immune factors that help the cells of the immune system fight infections”.
Removing and killing bacteria within the blood and producing certain chemicals used for
coagulation or blood clotting when tissue is destroyed are essential functions as well (Horn,
2005, p. 31).
The liver is divided into right and left lobes. These main lobes are divided into two more
lobes which are then “further subdivided
into many thousands of basic functional
units or small lobes called lobules” (Horn
29). The lobules appear to be in a
hexagonal shape and at each corner of the
hexagon are “a cluster of three vessels: very
small branches of the hepatic artery, the
portal vein, and a small bile duct” (Horn
29). A central axle lies in the center of the lobule and branching out from it are spokes. These
spokes are made up of hepatocytes or liver cells. The hepatocytes are the workers of the liver.
Their job is to take certain substances from the blood, modify them, and put these modified
substances either back into the blood or into the bile ducts (Horn, 2005, p. 29).
4

Not only is the anatomy an important part of understanding the overall damage that is
caused by a virus, but also an understanding of the term, virus, in general must be met. What is a
virus? A virus is a microscopic parasite that is dependent on a host cell in order to replicate and
survive. The virus first attaches to the host cell, penetrates it, and inserts nucleic acid which
initiates the reproduction process, but instead of replicating the cell, the cell will make copies of
the virus. Once the new viruses are produced, they leave the host cell and search for new cells to
infect. The virus takes over the metabolic functions of the host cell and uses that energy to stay
alive. This energy that would normally be used to meet the needs of the host cell and the needs of
other cells, is now being used as a deadly weapon and “the whole organism may develop
symptoms that are caused by the loss of important cell functions” (Horn, 2005, p. 44-45).
“Viruses have relatively simple structures” (Horn
45). They have nucleic acids and one way that scientists
classify viruses is whether they have DNA or RNA.
These nucleic acids usually have about 20 or fewer genes.
Another way to classify viruses is the number of strands
they have: a single or a double (Horn, 2005, p. 45). The
nucleic acid of a virus encased in a capsid is called a
nucleocapsid and the capsid protects the virus from
enzymes (Horn 45, 48). “Many viruses have spikes of
protein that make the capsid look like a pincushion”
(Horn 47). These spikes contain the special sites that allow it to recognize a host cell and “bind
to the surface” (Horn 47). When the virus is ready to leave the host cell, it exits through a
process called budding. This is when the virus comes out of the cell and the cell membrane
5

closes around the capsid until “until finally the membrane breaks free of the cell and closes up
with the virus inside” (Horn 50). However, some viruses have another exit strategy: they break
or rupture the membrane by releasing certain enzymes. “The completer virus structure that exits
a host cell and can infect other cells is referred to as a virion” (Horn 52).
Etiology
Having explained the basics, it’s best to start talking about the actual disease: Hepatitis C,
also known as the Silent Epidemic. Believed to have begun infecting humans as early as 1960,
HCV was formerly called non-A, non-B hepatitis and labeled as a “unique virus” (Fabry and
Narasimhan, 2007, p. 4). 170 million individuals worldwide have HCV and 4 million of those
are in the United States, most with chronic HCV (Fabry and Narasimhan, 2007, p. 8). Hepatitis
C primarily attacks the liver meaning that “roughly over half of all liver transplants in the United
States now involve patients with hepatitis C” ((Fabry and Narasimhan, 2007, p. 8).
Contracting the HCV begins with a simple transmission (Horn 86). HCV is a bloodborne
virus; therefore, the most common way to become infected with HCV is by it being directly
introduced into the bloodstream. “A history of Intravenous Drug Use (IVDU) is the most likely
cause of the infection in 60 percent of newly identified cases” (Fabry and Narasimhan, 2007, p.
16). IVDU, or intravenous drug use, is when the drug is injected directly into the bloodstream by
use of a needle. As the history of injections
lengthens and the sharing of needles increases, so
does that person’s risk of becoming infected (Fabry
and Narasimhan, 2007, p. 16). Until HCV was
discovered in 1989, blood transfusions were “a
6

common route of transmission” (Fabry and Narasimhan 16). However once the virus was
identified, scientists began to do routine screening tests on donated blood. Due to the tests and
new technology, the risk of contraction has decreased from 1 in 100,000 to 1 in 1,000,000 (Fabry
and Narasimhan 16).
The most common ways of transmission are IVDU and blood transfusions, but according
to Zein and Edwards (2008), “intranasal drug use, as in the snorting of cocaine” (p. 29) is also a
common transmission. There are tiny blood vessels in the nose and when cocaine is snorted,
those vessels rupture giving the virus a perfect portal of entry. Some less common factors were
“infusion of clotting factor concentrates before 1987” (Fabry and Narasimhan, 2007, p. 16) and
“organ transplantation prior to 1992” (Fabry and Narasimhan, 2007, p. 16).
Signs and Symptoms
Signs are the things the doctor sees while symptoms are what the patient experiences
(Fabry and Narasimhan, 2007, p. 27). Sixty percent of patients around the world had no idea that
they even had the disease. The fact that these people didn’t know they even had the disease is
pretty common since most patients have no signs or symptoms of liver disease which is why it’s
called the Silent Epidemic (Fabry and Narasimhan, 2007, p. 27). Many people have no
symptoms for up to thirty years which is why numerous amounts of HCV patients are left
untreated; they don’t think there’s anything wrong. When someone thinks of liver disease, they
automatically think of the yellowing of the skin, or jaundice, which is due to the buildup of
bilirubin (Bruce and Montanarelli, 2007, p. 44), however, only about 20 to 30 percent of HCV
patients experience this symptom.
7

Other common, obvious symptoms are dark urine and/or a light stool due to the fact that
the liver is not filtering properly. Some patients will have symptoms like “fatigue, mild
discomfort over the liver, nausea, and a poor appetite” (Fabry and Narasimhan, 2007, p. 27),
however, these symptoms are vague and could be any number of things. Other reported
symptoms include “depression, joint pains, Irritable Bowel Syndrome, bloating, menstrual
difficulties, bruising and bleeding easily, itchy skin” (Bruce and Montanarelli, 2007, p. 43).
Individuals with chronic hepatitis C commonly experience inflammation of the liver
which leads to scarring. This permanent scarring of the tissue is called cirrhosis. Twenty
percent of chronic HCV patients who have progressed to cirrhosis have had the terrible fate of
liver failure and/or liver cancer, however, it is not immediate and might not even occur; the risk
is a 3 to 4 percent chance. “This risk is significantly higher in people who consume excessive
amounts of alcohol.”
Diagnosis
As previously stated, once HCV was identified and isolated, scientists began to do
routine screenings on donated blood in 1990 (Horn 88).
When it is apparent that the liver is not working properly, doctors will put the patient
through a series of liver function tests (LFTs) to measure “the levels of liver proteins, liver
enzymes (called transaminases, and cholestatic live enzymes), and bilirubin” (Edwards and Zein,
2008, p. 136). “Doctors
usually order a standard
group of tests called a
liver panel that includes
8

aspartate aminotransferase (AST), alanine aminotransferase (ALT), bilirubin, alkaline
phosphatase, and albumin” (Fabry and Narasimhan, 2007, p. 41). To find any inflammation or
injury in the liver, AST and ALT levels are tested. Elevated AST levels alone could mean
there’s an issue a few places in the body, however, if there are elevated ALT levels as well, there
is definitely an issue with the liver (Edwards and Zein, 2008, p. 136). Race and sex play a role in
the transaminase levels and just transaminase levels alone do not necessarily tell of the extent of
the liver damage; “they are only the first clues along a path of diagnostic tests employed to
pinpoint what is wrong” (Edwards and Zein, 2008, p. 136.) Bilirubin and albumin just measure
the level of liver function. When the bile ducts are clogged, alkaline phosphatase levels elevate.
Though liver function tests aren’t perfect, they do help to identify issues that the patient might
not have suspected (Fabry and Narasimhan, 2008, p. 41).
If HCV is already suspected to have infected a patient, then a direct test, also called
hepatitis C RNA tests, is usually given. This test looks for even the smallest amount of the
actual virus in the patient’s blood (Fabry and Narasimhan, 2007, p. 38). Hep C RNA tests are
either qualitative, declared as positive or negative, or quantitative, measuring the “amount of
virus in the blood”, depending on how it is reported (Fabry and Narasimhan, 2007, p. 39). The
quantitative tests are more helpful when deciding whether to continue treatment or not.
Currently the most common of the RNA tests is the polymerase chain reaction (PCR). The
results of the test are usually reported in international units per milliliter; “one international unit
is roughly equivalent to two copies” (Fabry and Narasimhan, 2007, p. 39).
When a patient is infected, HCV attacks the immune system (Fabry and Narasimhan,
2007,p. 40). As HCV is passed on from patient to patient, the virus evolves, meaning there are
numerous amounts of strands or genotypes of the virus which is “determined through a blood
9

test” (Fabry and Narasimhan, 2007, p. 40). “There are 6 major HCV genotypes and more than
50 subtypes” (Fabry and Narasimhan, 2007, p. 40) and these play a big part in predicting a
response to certain treatments. In the United States, 75 percent of HCV patients have genotype 1
and the most difficult to treat; the remaining 25 percent having genotypes 2, 3, or occasionally 4
which have more of a positive response to treatment. Genotype 5 is more prevalent in South
Africa and genotype 6 is commonly found in Southeast Asia (Fabry and Narasimhan, 2007, p.
40).
To further increase their knowledge of the patient’s condition, doctors will order an array
of radiological tests, the most common being an ultrasound. This produces an image of the
“gallbladder, kidneys, spleen, pancreas, and blood vessels” and allows the doctor to see the
severity of the liver’s abnormalities (Fabry and Narasimhan, 2007, p. 45). Though an ultrasound
isn’t flawless, if used in along with other patient information, it can be very useful for
determining the severity of the patient’s condition; it is also able to sometimes detect liver cancer
if it exists within the patient (Fabry and Narasimhan, 2007, p. 45).
In order to fully understand the liver’s degree of damage, doctor’s will ask for a liver
biopsy to be performed. A liver biopsy is when a physician sticks a needle into the liver and
extracts a small sample of the liver tissue. Once removed, the tissue is examined under a
microscope. If the ultrasound is not specific enough
and the LFTs were inconclusive, a liver biopsy has
the ability to clear things up and help eliminate other
sources of liver disease off the list (Fabry and
Narasimhan, 2007, p. 46). When interpreting a liver
biopsy, doctors will use a scale from 0 to 4 for the
10

amount of inflammation and scarring in the liver where 0 is acknowledged as normal and 4 is
classified as cirrhosis (Fabry and Narasimhan, 2007, p. 48).
Prothrombin time (PT), yet another blood test, “reflects coagulation or the body’s ability
to clot” (Fabry and Narasimhan, 2007, p. 43).
Treatment
“The goal of treatment for hepatitis C is to prevent the development of cirrhosis and the
complications of cirrhosis including liver cancer and liver failure” (Fabry and Narasimhan, 2007,
p. 63).
Deciding whether or not to proceed with treatment, let alone choosing which treatment
would produce the best results is a delicate process and should not be rushed. It takes several
years for HCV to take its full affect and there is never a reason to start treatment in a hasty
manner. By the time the doctors have identified the true severity of the disease and begin
discussing different forms of treatment, patients have a definitive attitude about how they want to
handle their situation.
However, many people are
just as confused as ever and
spend a great deal of their
time throwing ideas around
in their heads, trying
desperately to make a
decision that is right for their
life style and family (Fabry and Narasimhan, 2007, p. 60).
11

One treatment is therapy with interferon and ribavirin, however, due to the many
uncomfortable side affects this treatment is usually not recommended and/or most patients aren’t
candidates for it. The patients that do choose this treatment will have to “take an interferon shot
once a week and ribavirin tablets twice a day” (Fabry and Narasimhan, 2007, p. 61). Some of
the risks of this treatment are “depression, birth defects, infection, severe anemia, bone marrow
depression, thyroid disease, and worsening of an underlying autoimmune disease” (Fabry and
Narasimhan, 2007, p. 67). The length of time at which this treatment lasts is determined by the
genotype of the virus particular to the patient and the “amount of disease found on the initial
liver biopsy” (Fabry and Narasimhan, 2007, p. 61); it also depends on the genotype of the virus.
Once treatment begins, certain goals that have been set previously must be achieved as the doctor
checks the patient’s viral levels regularly (Fabry and Narasimhan, 2007, p. 70). If these targets
are not hit, the doctor will stop the treatment, reassess the situation and the patient’s condition,
and suggest alternate options. Patients infected with genotype 1 HCV are treated with 1,000 to
1,200 milligrams of peginterferon and weight-based ribavirin for 48 weeks, but will be halted if
the patient’s viral levels do not fall 100-fold by the 12-week mark or if the virus is still found in
the blood at the 24-week mark. Genotype 2 or 3 patients will receive 800 milligrams daily for 24
weeks and viral levels for these patients are not really checked since there is such high cure rate
for these genotypes (Fabry and Narasimhan, 2007, p. 71).
Many of the symptoms can be relieved by doing simple things like stress reduction and
having a healthier diet (Bruce and Montanarelli, 2008, p. 44).
Prognosis
12

Now what the future holds for those with Hepatitis C depends upon the treatment and the
patient’s response to said treatment. There is a fine line between a treatment and a cure;
treatment is the process and the cure is the “destination”. Once HCV is no longer detected
during a number of blood tests 6 months after treatment has been stopped, “the outcome is
termed a sustained virological response (SVR)” (Fabry and Narasimhan, 2007, p. 62). Studies
show that once SVR has been achieved, there is a low chance that there will be a relapse or that
complications will develop (Fabry and Narasimhan, 2007, p. 62). If for some reason the patient
wants to stop treatment at any time, there really isn’t a risk. Obviously, continuing treatment for
the full length of time and taking the dosage prescribed by the doctor will increase the chance
that the patient will be cured. Occasionally, unwanted or risky side effects will become present
during treatment and at that time, the doctor may make the decision to cease treatment (Fabry
and Narasimhan, 2007, p. 76).
According to a study by Manns and colleagues, published between 2001 and 2004, (p.
72) the safety and efficacy of peginterferon alfa-2b with ribavirin was compared to interferon
alfa-2b and ribivirin; the cure rate was 54 percent. For patients with genotype 1 is 40 to 45
percent and 70 to 80 percent of those with genotype 2 or 3 (Fabry and Narasimhan, 2007, p. 72).
However, treatment protocols were different back during those years then they are now,
therefore, it is difficult to compare those results to this day and age. In another study by Fried
and colleagues in 2002, peginterferon alfa-2a and ribavirin combination was compared to
peginterferon alfa-2a; placebo showed similar results (Fabry and Narasimhan, 2007, p. 73).
“Genotype is clearly the most important predictor of a response to combination therapy” (Fabry
and Narasimhan, 2007, p. 74).
13

There are several possible outcomes of treatment. The first, discussed earlier, is SVR.
Another is relapse where at the time that treatment ended, the virus was not detected within the
blood, however, six months later, it was present when blood tests were performed. This response
to treatment shows that the patient’s body was only able to rid itself of the virus temporarily.
Third, a patient has a huge drop in viral levels, but the virus is still detected in the bloodstream;
this patient is called a partial responder.
Finally, a rare but possible result is a nonresponder who is simply an HCV patient who is
not responding to the treatment that was given. In this case, the patient’s situation must be
reassessed because the treatment given was not able to clear the virus from the patient’s system.
It is important to acknowledge that though the virus isn’t gone, it’s promising that treatment has
slowed the virus’ journey through the body (Fabry and Narasimhan, 2007, p. 76-77).
Patients with mild scarring of the liver are not recommended any further treatment
because there is a little to no chance of developing cirrhosis. Appropriate lifestyle changes,
follow-up care every 6 to 12 months, and a liver biopsy every 3 to 5 years would benefit the
patient immensely (Fabry and Narasimhan, 2007, p. 77).
Those with more severe scarring or cirrhosis have a higher risk of developing
complications like liver cancer. There are really only two options for patients with this much
damage to the liver and are not responding to normal treatment. The first option is to consume a
“low dose of interferon is used indefinitely in an attempt to control (but not cure) the infection”
(Fabry and Narasimhan, 2007, p. 78). The other option is to use consensus interferon which is
under the brand name Infergen. It is a synthetic interferon made by combining natural
interferons and using the most common amino acid (Fabry and Narasimhan, 2007, p. 80). Since
2002, The North Dakota Department of Corrections and Rehabilitation has been using this type
14

of therapy on the prison populations where the HCV numbers are so high. The cure rate overall
was 54.2 percent with genotype 1 and 75 percent of those who had genotypes 2 or 3 (“New
Opportunities for the Management and Therapy of Hepatitis C in Correctional Settings.”).
Maintenance therapy is when peginterferon is used at a low dose indefinitely. It controls
the viral level which will reduce inflammation and stop the progression of fibrosis (Fabry and
Narasimhan, 2007, p. 78). In this way, in the minds of the doctor, HCV is no longer thought of
as a disease but more as a chronic illness. Patients who should consider this option are those
with “advanced fibrosis or compensated cirrhosis” (Fabry and Narasimhan, 2007, p. 79).
Prevention
“Hepatitis C is spread through blood-to-blood contact” (Fabry and Narasimhan, 2007, p.
17). Those with HCV must be extremely careful not to spread it
to anyone else and those without HCV must be careful not to
come into contact with another person’s blood if it is exposed.
A major way not to transmit hepatitis C is to not engage in any
drug activity whatsoever. Drugs are naturally contaminated with
a number of chemicals and poisons. Drug dealers are not known
for being very careful; therefore, anything could be in the drug being purchased, including HCV.
If an HCV patient has a drug problem, it’s
best to enroll in a substance abuse program so
that they may receive help in order to stop
using drugs.
15

Though it’s rare to transmit HCV through sexual activity, it is in the patient’s best
interests to inform their partner of any infections that they have; it is also recommended to use a
“new latex condom with lubricants to reduce the risk of bleeding” (Fabry and Narasimhan, 2007,
p. 18).
Other preventative precautions: “do not donate sperm, ova, or blood; clean blood spills
appropriately; do not share razor blades, toothbrushes, nail clippers, etc; dispose of feminine
hygiene products in plastic bags” (Fabry and Narasimhan, 2007, p. 19). Another way to prevent
HCV transfer is to not become pregnant while viral levels in the blood are high.
In summary, hepatitis C mainly attacks the liver. HCV was not identified until 1989 and
from then on, special screenings have been done on donated blood in order to reduce the risk of
transmission. It is transmitted through blood-to-blood contact. The most common way of HCV
transmission is intravenous or intranasal drug use. Most patients with this disease don’t show
any symptoms for years after receiving
the virus. RNA tests and a liver biopsy
are the best ways to test for the disease
and see how much damage it has been
done. Treatment includes different kinds
of therapy. The prognosis for HCV
patients is that they will either be cured,
have a relapse, or have to take a low dose of interferon for the rest of their lives. Preventing
transmission of the virus to yourself or anyone else is important and must be taken seriously to
16
Figure 1 Scientists are working on a vaccination.

refrain from infecting others. Unfortunately, no vaccine for hepatitis C is available at this time,
however, scientists are still working on this current problem.
17

Resources
“The ABC’s of Viral Hepatitis.” World Book Science Fair. 01. Aug. 2009. eLibrary. Web. 08
Apr. 2010."The A, B, C's of Viral Hepatitis." World Book Science Year. 01 Aug.
2009. eLibrary. Web. 08 Apr. 2010."The A, B, C's of Viral Hepatitis." World Book
Science Year. 01 Aug. 2009. eLibrary. Web. 08 Apr. 2010."The A, B, C's of Viral
Hepatitis." World Book Science Year. 01 Aug. 2009. eLibrary. Web. 08 Apr.
2010."The A, B, C's of Viral Hepatitis." World Book Science Year. 01 Aug. 2009.
eLibrary. Web. 08 Apr. 2010.
“Brandon Hepatitis C Outbreak Traced To Employee Mistakes.” McClatchy – Tribune Business
News. 19 Mar. 2010. eLibrary. Web. 08 Apr. 2010.
Bruce, Cara, and Lisa Montanarelli. The First Year Hepatitis C Second Edition: An Essential
Guide for the Newly Diagnosed. New York: Marlowe & Company, 2007. Print.
Crosta, Peter. “What Is A Virus? What Is A Viral Infection?” Infectious Diseases / Bacteria /
Viruses News. Medical News Today, 20 Jul. 2009. Web. 08 Apr. 2010.
Edwards, Kevin M., Nizar N. Zein. Liver Disorders A Cleveland Clinic Guide. Ohio: Cleveland
Clinic Press, 2008. Print.
Fabry, Stephen C., and Anand Narasimhan. 100 Questions & Answers About Hepatitis C: A
Lahey Clinic Guide. Massachusetts: Jones and Bartlett Publishers, 2007. Print.
18

Hagan, John J., Jeffrey E. Hostetter, C. Kent Martin. “New Opportunities for the Management
and Therapy of Hepatitis C in Correctional Settings.” The American Journal of Public
Health 100 (2010): 13. Health and Wellness Resource Center. Web. 08 Apr. 2010.
“Hepatitis C (non-A, non-B virus, HCV).” The Mosby Medical Encyclopedia. 01. Oct. 1996.
eLibrary. Web. 08 Apr. 2010.
“Hepatitis C Virus; Hepatitis C Virus Replication in Perihepatic Lymph Nodes Contributes to
Viremia.” Science Letter. 09 Jun. 2006: 906. eLibrary. Web. 08 Apr. 2010.
“Hepatitis C Virus Infection; Non-injecting Sexual Partners of HCV- Infected Persons At High
Risk for Infection.” Science Letter. 12 Oct. 20004: 714. eLibrary. Web. 08 Apr. 2010.
“Hepatitis C Virus; Researchers from the United States and Austrailia Report Recent Findings in
Hepatitis C Virus.” Science Letter. 03. Jun. 2007:4406. eLibrary. Web. 08 Apr. 2010.
“Hepatitis C Virus Studies from the United States and Japan Describe New Findings in Hepatitis
C Virus Research.” Obesity, Fitness & Wellness Week. 09 May. 2006: 1464. eLibrary.
Web. 08 Apr. 2010.
Horn, Lyle W. Deadly Diseases and Epidemics Hepatitis. Philidelphia: Chelsea House
Publishers, 2005. Print.
19

Seppa, Nathan. “Keeping Hepatitis C Out.” Science News. 24 Oct. 2009: 11. eLibrary. Web. 08
Apr. 2010.
Worman, Howard J. The Liver Disorders and Hepatitis Source Book. New York: McGraw Hill,
2006. Print.
20