HemorrhoidGEN0113 WM
-
Upload
fachry-muhammad -
Category
Documents
-
view
214 -
download
0
Transcript of HemorrhoidGEN0113 WM
-
8/11/2019 HemorrhoidGEN0113 WM
1/4
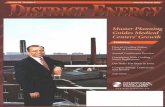
Approach to HemorrhoidsA Primer for Gastroenterologists
A good medical history and physical examination,
including anoscopy or office proctoscopy, should guide
the physician to the correct diagnosis; in cases of bleed-
ing, a colonoscopy or sigmoidoscopy in addition to ano-
scopy is necessary to verify the source of the bleeding.
It is the intent of this review to provide gastroentertolo-
gists with a general introduction to the nonsurgical man-
agement of hemorrhoids.
AnatomyThomson, in his description of hemorrhoidal anatomy,
noted a series of 3 cushions in the anal canal, located in
the left lateral, right anterior, and right posterior posi-
tions. These hemorrhoidal cushions receive their blood
supply primarily from the superior and middle hemor-
rhoidal arteries; the superior, middle, and inferior hem-
orrhoidal veins provide venous drainage. A sinusoidal
pattern of arteriovenous communication is formed within
the cushions, which explains why hemorrhoidal bleeding
is arterial, rather than venous in nature.1
In addition to the vessels noted above, the hemor-
rhoidal cushions are also rich in muscular fibers, arising
from the internal sphincter and the conjoined longitudi-nal muscle. These fibers help to anchor the cushions to
the underlying muscular layer of the anorectum, and it is
the breakdown of these supporting fibers that eventually
leads to the changes that can cause hemorrhoidal symp-
toms.1,2The cushions play an important role in the main-
tenance of rectal continence, as they provide 15% to 20%
of the resting pressure at the anal verge.3
The epithelial layer of the anorectum is characterized
by the relatively insensate columnar epithelium, which
covers the internal hemorrhoidal cushions (mucosa) an
the extremely sensitive squamous epithelium, whic
extends up into the anus (anoderm). The junction o
these 2 epithelial layers is known as the dentate line
and is typically located approximately 3 cm inside th
anal verge. This line marks the transition between th
columnar epithelialcovered internal hemorrhoids an
the squamous epithelialcovered external hemorrhoida
vessels.4-6
Pathophysiology
There are a number of proposed mechanisms t
explain the development of symptomatic hemorrhoid
including abnormal venous dilatation, abnormal disten
sion of the arteriovenous anastomoses, downward dis
placement or prolapse of the hemorrhoidal tissue, or
breakdown of the connective tissue anchoring the hem
orrhoidal cushions. Prolapse of hemorrhoidal tissue
what appears to lead to the development of symptoms
This prolapse allows for mucous deposition on the per
anal skin, which causes itching, and leads to tissue fria
bility and bleeding. Other symptoms include swelling o
associated external disease and fecal soiling when thprolapsing tissue precludes complete closure of the ana
opening.1,7
Internal hemorrhoids are covered by the mucosa
they reside proximal to the dentate line and are gener
ally painless. External hemorrhoids are located distal t
the dentate line and are covered by squamous epithe
lium; patients who experience pain as a result of hemor
rhoids often have a thrombosed external hemorrhoid o
an anal fissure.
Hemorrhoids are normal vascular structures of the
anal canal. Often, they are the source of a variety of
troublesome symptoms, including bleeding, anal pruritus,
prolapse, and pain due to thrombosis of external hemorrhoids.
Patients often mistake other anal or perianal problems for
hemorrhoids, such as anal fissures, skin tags, hypertrophied analpapillae, anal cancer, and anal condylomata, as well as other infections.
HARRYSARLESJR., MD
GastroenterologistDigestive Health Associates of Texas
Dallas, Texas
PRINTER-FRIENDLY VERSION AVAILABLE AT GASTROENDONEWS.COM
1INDEPENDENTLY DEVELOPED BY MCMAHON PUBLISHING GASTROENTEROLOGY & ENDOSCOPY NEWS JANUARY 2013
-
8/11/2019 HemorrhoidGEN0113 WM
2/4
The causes of symptomatic hemorrhoids are not com-
pletely clear, but a number of factors, including a lack of
dietary fiber, constipation, straining on defecation, diar-
rhea, pregnancy, obesity, a sedentary lifestyle, spending
excess time on the commode, spinal cord injuries, and
family history all have been suggested.8
Epidemiology
It is difficult to quantify the incidence of hemorrhoidal
disease, in large part because many patients do not seek
medical care for their condition; additionally, some attri-
bute almost any anorectal symptom to hemorrhoids.
Estimates of the prevalence of hemorrhoidal disease
in the United States range from 4.4% to 40%.9Some
research suggests that 75% of the population will expe-
rience symptomatic hemorrhoid disease at some point
in their lives.10Although these estimates vary widely, it
seems clear that symptomatic hemorrhoids have a sig-
nificant effect on health and well-being.
Grading of Hemorrhoidal Disease
Banov et al11developed a grading system for inter-
nal hemorrhoids based on the degree of prolapse. The
grade of hemorrhoidal disease has some bearing on the
treatment options available to a patient with internal
hemorrhoids: grade I: non-prolapsing internal hemorrhoids
grade II: prolapse of internal hemorrhoids during defeca-
tion with spontaneous reduction
grade III: prolapse of internal hemorrhoids during defeca-
tion that requires manual reduction
grade IV: prolapse and incarceration of internal hemor-
rhoids; hemorrhoids cannot be reduced
Diagnosis
PATIENTHISTORY
As previously stated, patients often attribute any ano-
rectal symptom to hemorrhoidal disease, and althoughthis may partly explain symptoms, it is important for the
physician to determine whether there are other issues
involved as well.5,12
Internal hemorrhoids are associated with pain-
less bleeding, prolapse, mucus discharge, soiling, and
symptoms of pruritus ani; these symptoms rarely cause
significant pain. External hemorrhoids usually are
asymptomatic, unless they become thrombosed. Pain
with defecation is commonly due to the presence of an
anal fissure, which is found in up to 20% of patients with
hemorrhoids.13
The relationship between symptoms, defecation habits,
bleeding, and a description of factors that might relieveor exacerbate a patients symptoms are important to
consider in the medical history.
PHYSICALEXAMINATION
A visual inspection of the perianal area will allow for
the discovery and description of rashes, tags, fissures,
fistulae, abscesses, neoplasms, condylomata, some cases
of prolapse, and so forth. The left lateral decubitus posi-
tion is preferred for the examination, as this position
seems to be better tolerated than the prone, jack-knife
position.14
A digital rectal examination will identify such things
scars, small fissures, and the origins of fistulae. These
clinical findings will be important in formulating a com-
prehensive treatment plan for the symptomatic patient.15
ENDOSCOPICEXAMINATION
Anoscopy is an accurate, efficient, inexpensive way
to evaluate the anal canal quickly, with minimal discom-
fort to the patient. Flexible endoscopy frequently is
performed to evaluate patients with symptoms of hem-
orrhoids, however, it is not as accurate as anoscopy. A
prospective study showed that anoscopy revealed 99% of
anorectal lesions, whereas endoscopy revealed 78% when
performed with straight withdrawal of the endoscope,
and 54% with retroflexion.16 The limitations of flexible
endoscopy, along with increased cost and inconvenience
to the patient, stress the need to consider anoscopy in
the evaluation of hemorrhoidal disease.
Treatment
CONSERVATIVEMEDICALTREATMENT
There are a number of over-the-counter prepara-
tions intended to treat patients with symptomatic hem-
orrhoids. These compounds contain ingredients such as
antiseptics, astringents, topical anesthetics, and cortico-
steroids. There is not a lot of evidence to support the use
of many of these products, and the potential negative
effects of the long-term use of topical steroids should
be considered.17
Common dietary and behavioral recommendations
for patients with hemorrhoids include increasing the
intake of dietary fiber, minimizing the amount of time
spent on the commode, avoiding straining during defe-
cation, and taking sitz baths several times a day. There
is evidence to support these recommendations both forthe treatment of symptomatic disease and in limiting the
risk for recurrence.18These measures are a reasonable
first-line approach for patients with mild symptoms.
NONSURGICALTREATMENT
Sclerotherapy
Sclerotherapy uses the injection of a sclerosant into
the submucosa, beneath the hemorrhoid, to create an
inflammatory reaction in the soft tissue that affixes the
loose hemorrhoidal mucosa back to the underlying mus-
culature. The procedure dates back to the 1800s. Some
research shows sclerotherapy to be beneficial in patients
with grade I and II hemorrhoids,19whereas other researchshows it to be no more beneficial than bulk laxatives.20
Potential complications of sclerotherapy include pain,
urinary retention, abscess, and impotence. Avoidance of
these complications depends on precise placement of
the injection.21
Rubber Band Ligation
Rubber band ligation (RBL) is the most commonly
performed nonsurgical procedure used in the treatment
of hemorrhoids; it is performed in up to 80% of patients
INDEPENDENTLY DEVELOPED BY MCMAHON PUBLISHING2
-
8/11/2019 HemorrhoidGEN0113 WM
3/4
with hemorrhoids.22,23Blaisdell first described a ligation
technique using a silk suture in 1958,24with Barron begin-
ning to use rubber bands in 1963.25Barron treated one
column of hemorrhoids per session to minimize pain and
post-banding complications. The process causes the
banded tissue to necrose and slough, with the resultant
inflammatory reaction causing refixation of the mucosa
to the underlying tissue, eliminating hemorrhoidal pro-
lapse. This mechanism of action is common among the
nonsurgical treatments for hemorrhoids, stressing the
importance of hemorrhoidal prolapse in the etiology of
symptoms.
RBL is a simple, inexpensive procedure, effective for
grade I to III hemorrhoids.2Patients undergoing RBL typ-
ically do not require bowel preparation, sedation, nar-
cotics, or a significant recovery period; they are able to
return to work immediately.5One of the disadvantages
of earlier RBL procedures was the need for 2 operators
to perform the procedure, but this has since been over-
come with the development of single-use, disposable
devices that do not require an assistant.6,7
RBL leads to reconfiguration and reduction in the size
of hemorrhoidal cushions, resulting in symptom resolu-
tion. Short-term success rates of up to 99% and long-
term success rates of up to 80% have been described;
however, there is a large range in the reported incidence
of complications. The predominant issue in patients
undergoing RBL is significant pain, with the incidence
rates ranging from less than 1% to 50%, in some series.6,26
Other reported complications include bleeding, urinary
retention, vasovagal reactions, and the very rare compli-
cation of sepsis. Based on the literature, the incidence of
complications appears to be related to the techniques
that are used to perform the banding.
Endoscopic RBL has been shown to have excellent
results, however, the method is more expensive than the
others and requires patient preparation as well as anes-thesia.27Endoscopic RBL also has been reported to be
more painful than other banding techniques.28 Other
common techniques use an anoscope to gain access to
the hemorrhoids. There also is a procedure that allows
for a blind placement of the band, obviating the need
for an anoscope.
The literature is confusing when it comes to where
the band should be placed, as descriptions vary from
a few millimeters above the dentate line29to at least
2 cm proximal to the dentate line.30,31 I prefer a tech-
nique that involves placing the band at least 2 cm above
the dentate line, as this technique has been associated
with less pain.6
Controversy exists regarding the number of hemor-
rhoids to treat during a single session. In the time since
Barrons original work was published,25most research-
ers have recommended treating only one column of
hemorrhoids per session in order to minimize the rate
of complications. Other authors have suggested band-
ing 2 or more columns per session in order to minimize
the number of patient visits required; however, compli-
cation rates are higher when more bands are placed.32
I recommend banding a single hemorrhoid per session
Endoscopic band placement is effective but is mor
costly and is associated with higher rates of post-proce
dural pain compared with in-office band placement.24,3
Personally, I prefer the blind touch techniqu
described by Cleator and Cleator.6This technique allow
placement of the band without an anoscope at 2 cm abov
the dentate line. Using this technique, the researcher
demonstrated a 1% complication rate (primarily pain
and successful treatment of up to 99% of patients, wit
a recurrence rate of 5% at 2 years.5
Infrared Coagulation
Neiger first described infrared coagulation (IRC) i
1979.34 The infrared coagulator is placed through a
anoscope while infrared light is converted to heat in th
hemorrhoidal tissue. The heat produces tissue destruc
tion, protein coagulation, and inflammation, leading t
scarring and tissue fixation. During the procedure, 3 to
pulses of energy are applied to the mucosa at the ape
of the hemorrhoid, and 1 to 2 columns of hemorrhoid
are treated at a time. Treatment is repeated every 2 t
4 weeks.24
Advantages of IRC include a relative lack of signif
icant complications. Disadvantages include equipmen
costs, the need for repeated treatments, higher recu
rence rates, and its ineffectiveness in patients with mor
advanced disease.24,34
Direct Current Electrotherapy
Direct current electrotherapy also uses a device that
inserted through an anoscope (Ultroid, Ultroid Technolo
gies, Inc).35This procedure uses direct current and doe
not create heat but rather produces sodium hydroxide
creating the submucosal reaction that leads to scarring
which helps to eliminate the hemorrhoidal prolapse.7
Limitations of direct current electrotherapy includ
the cost of the technology and the amount of tim
required to treat the involved tissue. The length of thprocedure depends on the grade of hemorrhoidal dis
ease and the amount of current that the patient can to
erate, which ranges from 4:45 to 19:45.35The procedur
has been reported to cause significant pain in up to 20%
of patients, resulting in termination of therapy; 16% o
patients have prolonged post-procedural pain.36
Bipolar Diathermy and Heater Probe Coagulatio
These technologies may be used by way of anoscop
in order to control chronic hemorrhoidal symptoms. Bot
procedures generate heat, which causes coagulation o
the target tissue leading to a fibrotic reaction with fixa
tion of the treated tissue.32
The procedures have similar efficacy for the treatment of bleeding. In one study, the heater probe con
trolled the bleeding more quickly (76.5 vs 120.5 days
at the expense of more pain.37The bipolar technolog
was associated with a higher overall rate of complica
tions (11.9% vs 5.1%), including pain, bleeding, fissure fo
mation, and spasm of the internal sphincter. Anothe
study demonstrated symptomatic mucosal ulceration i
24% of patients treated with bipolar electrocoagulation
significant bleeding in 8%, and prolonged pain in 4%.3
GASTROENTEROLOGY & ENDOSCOPY NEWS JANUARY 2013 3
-
8/11/2019 HemorrhoidGEN0113 WM
4/4
Neither technology was able to reliably eliminate pro-
lapsing tissue.29,36,37
Cryosurgery and Lords Stretch Procedure
These techniques are mentioned for historical refer-
ence only, as neither is recommended. Cryosurgery is
associated with significant post-procedure pain, along
with foul-smelling discharge and prolonged recovery in
several series.36The Lords Stretch, a forceful dilatation
of the anus in order to reduce elevated sphincter pres-
sures was found to result in incontinence in a significant
number of patients.38Some have recommended that the
procedure be abandoned.39
SURGICALTREATMENTOPTIONS
This review is intended to discuss nonsurgical options
available for the treatment of symptomatic hemorrhoidal
disease, and these approaches have been shown to be
effective in 80% to 99% of patients. A number of surgical
options are available as well, but because of increased
cost, pain, disability, recuperation time, risk for complica-
tions, and so on, surgical options should be reserved only
for nonresponders and for patients with grade IV hemor-
rhoids or hemorrhoids with both internal and external
components.40
Conclusions
Symptomatic hemorrhoids are common and patients
frequently visit a gastroenterologist for diagnosis and
treatment. A number of effective nonsurgical approaches
are available for these patients. RBL is the most com-
monly used office-based hemorrhoidal therapy. Informa-
tion is presented here to aid the gastroenterologist in the
evaluation and definitive treatment of patients with hem-
orrhoidal disease.
References
1. Thomson WH. The nature of haemorrhoids. Br J Surg. 1975;62(7):542-552.
2. Sardinha TC, Corman ML. Hemorrhoids. Surg Clin North Am. 2002;
82(6):1153-1167, vi.
3. Lestar B, Penninckx F, Kerremans R. The composition of
anal basal pressure. An in vivo and in vitro study inman. Int J
Colorectal Dis. 1989;4(2):118-122.
4. Wexner SD, Jorge JMN. Anatomy and embryology of the anus, rectum,
and colon. In: Corman ML, ed. Colon and rectal surgery. 4th ed. Philadel-
phia, PA: Lippincott-Raven; 1998.
5. Guttenplan M, Ganz RA. Hemorrhoidsoffice management and review
for gastroenterologists. Touchgastroentorology.com; December 2011.
6. Cleator IGM, Cleator MM. Banding hemorrhoids using the ORegan
disposable bander. US Gastroenterology Review. 2005:69-73.
7. Corman ML. Hemorrhoids. In: Corman ML, ed. Colon and rectal surgery.
4th ed. Philadelphia, PA: Lippincott-Raven; 1998:147-205.
8. Loder PB, Kamm MA, Nicholls RJ, Phillips RK. Haemorrhoids: pathology,
pathophysiology and aetiology. Br J Surg. 1994;81(7):946-954.
9. Ohning GV, Machicado GA, Jensen DM. Definitive therapy for internal
hemorrhoidsnew opportunities and options. Rev Gastroenterol Disord.
2009;9(1):16-26.
10. Baker H. Hemorrhoids. In: Longe JL, ed. Gale encyclopedia of medicine.
3rd ed. Detroit: Gale; 2006:1766-1769.
11. Banov L Jr, Knoepp LF Jr, Erdman LH, Alia RT. Management of hemor-
rhoidal disease.J S C Med Assoc. 1985;81(7):398-401.
12. Halverson A. Hemorrhoids. Clin Colon Rectal Surg. 2007;20(2):77-85.
13. Schubert MC, Sridhar S, Schade RR, Wexner SD. What every gastroen-
terologist needs to know about common anorectal disorders. World J
Gastroenterol. 2009;15(26):3201-3209.
14. Alonso-Coello P, Castillejo MM. Office evaluation and treatment of hemor-
rhoids.J Fam Pract. 2003;52(5):366-374.
15. Beck DE. Evaluation of the anorectum during endoscopic examinations.
Tech Gastro Endoscopy. 2004;6:2-5.
16. Kelly SM, Sanowski RA, Foutch PG, Bellapravalu S, Haynes WC. A pro-
spective comparison of anoscopy and fiberendoscopy in detecting anal
lesions.J Clin Gastroenterol. 1986;8(6):658-660.
17. Chong PS, Bartolo DC. Hemorrhoids and fissure in ano. Gastroenterol Clin
North Am. 2008;37(3):627-644, ix.
18. Moesgaard F, Nielsen ML, Hansen JB, Knudsen JT. High-fiber diet reduces
bleeding and pain in patients with hemorrhoids: a double-blind trial of
Vi-Siblin. Dis Colon Rectum. 1982;25(5):454-456.
19. Khoury GA, Lake SP, Lewis MC, Lewis AA. A randomized trial to compare
single with multiple phenol injection treatment for haemorrhoids. Br J
Surg. 1985;72(9):741-742.
20. Senapati A, Nicholls RJ. A randomised trial to compare the results of
injection sclerotherapy with a bulk laxative alone in the treatment ofbleeding haemorrhoids. Int J Colorectal Dis. 1988;3(2):124-126.
21. Pilkington SA, Bateman AC, Wombwell S, Miller R. Anatomical basis for
impotence following haemorrhoid sclerotherapy.Ann R Coll Surg Engl.
2000;82(5):303-306.
22. Kann BR, Whitlow CB. Hemorrhoids: diagnosis and management. Tech
Gastro Endoscopy. 2004;6(1):6-11.
23. Corman ML, Veidenheimer MC. The new hemorrhoidectomy.Surg Clin
North Am. 1973;53(2):417-422.
24. Blaisdell PC. Prevention of massive hemorrhage secondary to hemor-
rhoidectomy. Surg Gynecol Obstet.1958;106(4):485-488.
25. Barron J. Office ligation of internal hemorrhoids.Am J Surg. 1963;
105:563-570.
26. Kumar N, Paulvannan S, Billings PJ. Rubber band ligation of haemor-
rhoids in the out-patient clinic.Ann R Coll Surg Engl. 2002;84(3):172-174.
27. Jutabha R, Jensen DM, Chavalitdhamrong D. Randomized prospective
study of endoscopic rubber band ligation compared with bipolar coagu-
lation for chronically bleeding internal hemorrhoids.Am J Gastroenterol.
2009;104(8):2057-2064.
28. Cazemier M, Felt-Bersma RJ, Cuesta MA, Mulder CJ. Elastic band ligation
of hemorrhoids: flexible gastroscope or rigid proctoscope? World J Gas-
troenterol. 2007;13(4):585-587.
29. Daram SR, Lahr C, Tang SJ. Anorectal bleeding: et iology, evaluation and
management (with videos). Gastrointest Endosc. 2012:76(2):406-417.
30. Madoff RD, Fleshman JW, Clinical Practice Committee, American Gas-
troenterological Association. American Gastroenterological Association
technical review on the diagnosis and treatment of hemorrhoids. Gastro-
enterology. 2004;126(5):1463-1473.
31. Kaidar-Person O, Person B, Wexner S. Hemorrhoidal disease: a compre-
hensive review.J Am Coll Surg. 2007;204(1):102-117.
32. Lee HH, Spencer RJ, Beart RW Jr. Multiple hemorrhoidal bandings in a
single session. Dis Colon Rectum. 1994;37(1):37-41.
33. Cataldo P, Ellis CN, Gregorcyk S, et al. Practice parameters for
the management of hemorrhoids (revised). Dis Colon Rectum.
2005;48(2)189-194.
34. Neiger S. Hemorrhoids in everyday practice. Proctology. 1979;2:22-28.35. Ultroid Model 3053 Operating & Maintenance Manual. Ultroid Technolo-
gies, Inc., Rev 10.5.2010a:17.
36. Yang R, Migikovsky B, Peicher J, Laine L. Randomized, prospective trial
of direct current versus bipolar electrocoagulation for bleeding internal
hemorrhoids. Gastrointest Endosc. 1993;39(6):766-769.
37. Jensen DM, Jutabha R, Machicado GA, et al. Prospective randomized
comparative study of bipolar electrocoagulation versus heater probe
for treatment of chronically bleeding internal hemorrhoids. Gastrointest
Endosc. 1997;46(5):435-443.
38. Lord PH. A new regime for the treatment of haemorrhoids. Proc R Soc
Med. 1968;61(9):935-936.
39. The Standards Task Force. Practice parameters for the treatment of hem-
orrhoids.Dis Colon Rectum. 1990;33(11):992-993.
40. MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a
meta-analysis. Can J Surg. 1997;40(1):14-17.
AUTHOR DISCLOSUREDr. Sarles is a member of the advisory board
of CRH Medical.
DISCLAIMERThis review is designed to be a summary of information
and represents the opinions of the author. Although detailed, the review
is not exhaustive. Readers are strongly urged to consult any relevant
primary literature, the complete prescribing information available in the
package insert of each drug, and the appropriate clinical protocols. No
liability will be assumed for the use of this review, and the absence of
typographical errors is not guaranteed. Copyright 2013, McMahon
Publishing, 545 West 45th Street, 8th Floor, New York, NY 10036.
Printed in the USA. All rights reserved, including right of reproduction,
in whole or in part, in any form.
INDEPENDENTLY DEVELOPED BY MCMAHON PUBLISHING4

















![Soldadoras - pdwatersystems.com · soldadoras wm 140 wm 180 wm 250 características modelo wm 140 wm 180 wm 250 voltaje [ v ] 110 110 / 220 110/220 fases 1 1 1 diametro de electrodo](https://static.fdocuments.us/doc/165x107/5ba485f909d3f2a9218d9d00/soldadoras-soldadoras-wm-140-wm-180-wm-250-caracteristicas-modelo-wm-140.jpg)
