Helping Kids to Health The role of Iowa public schools.
-
Upload
eustace-griffith -
Category
Documents
-
view
214 -
download
0
Transcript of Helping Kids to Health The role of Iowa public schools.
Collaborators• Iowa Dietetic Association• Iowa Dental Hygienists Association• Iowa School Food Service
Association• Iowa Fit Kids Coalition• ISU Extension
Discussion Objectives
To understand and describe Three examples of health problems
that can be prevented How the school environment
impacts health and nutrition Policy changes that can impact
health of students
Invest in a Child’s Health
To help his/her… Ability to learn Physical ability Appearance Social opportunities Success in school and future employment
Health is key to a long and productive life!
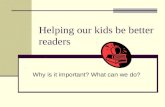
Trends in Overweight
0.0%
2.0%
4.0%
6.0%
8.0%
10.0%
12.0%
14.0%
16.0%
18.0%
1963-65 1971-74 1976-80 1988-91 1999
NHANESBoys
NHANESGirls
Overweight and Obesity
Obesity has been related to changes in our lifestyle, including diet and physical activity
Efforts to lose weight have proven unsuccessful for many adults.
Obese children are 43.5 times more likely to have at least 3 cardiovascular risk factors. Nicklas, 2001
As many as 45% of children newly diagnosed with diabetes have type 2 diabetes.
The Problem of Childhood Overweight
Complex …but simple Cannot ignore that one cause is
caloric intake that exceeds caloric expenditure.
Experts recommend that we concentrate on preventing overweight.
No Simple Answer to the Obesity Epidemic
ObesityEpidemic
Food Industry
Candy
Genes
Soft Drinks
Pouring Contracts
Junk Food
Restaurants
Fast Food Computer
s
Working Mothers Povert
y
Poor Parenting
School Feeding
TV
Decreasing Physical Activity
Decreased PE in Schools
Sugar
Glycemic Index
Energy Density
Nicklas, TA, 2003
Genetic vs. Environmental
Obesity gene Children have higher risk of obesity when
either one or both parents are obese. Obesity associated with genetic syndromes
What has changed? … “Gene pool” has not changed Environment: has changed
Dental Health Tooth decay is the most common chronic
disease among children--5 times more common than asthma.
An estimated 51 million school hours per year are lost due to dental related illness
Children with chronic dental pain are unable to attend to school work. (Oral Health in America: A Report of the Surgeon General, 2000)
Poor oral health tied to decreased school performance, poor social relationships and less success later in life
Dental Health
20% of low income children in Iowa have untreated decay in permanent teeth.
68% of low income children have a history of decay compared to 52% of higher income children.
56% of children participating in the IDPH dental sealant programs have a history of decay.
Bone Health Bones are formed during childhood and
adolescence. Milk and dairy products are the best
sources of calcium needed to form bones.
Lack of calcium in adolescence could lead to bone health in later years.
Weight bearing exercise is an important factor in bone formation and retention.
Bone Health Osteoporosis is “a pediatric disease
with a geriatric outcome” Physically active girls who consume
soft drinks have more bone fracturesWyshak, G, Arch Pediatr. Adolesc. Med, 2000; 154:610-613.
Over 10 million men & women are estimated to have osteoporosis in 2002; another 33.6 million have low bone mass and are at risk for osteoporosis.
National Osteoporosis Foundation http://www.nof.org/osteoporosis/state.htm
Psychosocial Concerns of Poor Health
Lowered self esteem Body image disturbances Depression Poor academic performance Increased behavior problems
Why be Concerned?
70 to 80% of overweight teens become overweight as adults.
Poor diet/inactivity in adults causes 300,000+ deaths annually.
Osteoporosis decreases mobility and increases pain and has been reported in women.
What has Changed? Physical Activity
22% children did not participate in moderate or vigorous physical activity
20% were not enrolled in physical education class
86% did not attend physical education class daily
(Youth Risk Behavior Survey, CDC, 2000)
Physical Activity
Physically fit children perform better academically – California schools
NASPE recommends 150 minutes/week of physical education
Qualified teachers can ensure safety and teach appropriate activities that are enjoyable, develop motor skills and maintain health related fitness.
What has Changed? Children’s Eating Habits Only 2% of kids meet all Food
Guide Pyramid Recommendations 16% do not meet any
recommendations 12% report skipping breakfast Only 11% eat a breakfast that
contains three food groups and provides >25% of RDA for energy
Compared to Recommendations
84% of kids eat too much fat; 91% eat too much saturated fat Only 15% get enough fruits Only 20% get enough vegetables Only 30% get enough milk Only 19% of girls aged 9 to 19 years
of age meet calcium recommendations
Soft Drinks Cancel Out Milk
Gallons Consumed Per Year
0
10
20
30
40
50
60
1970 1980 1990 1997
milk
soft drinks
Soft Drinks: The Facts
Who drinks soft drinks? 50% of all Americans 65% of adolescent girls 74% of adolescent boys
Borrud, et al., Community Nutrition Inst, 1997
7.0
6.0
5.0
4.0
Plaque pH
critical pH
0 20 40 60 80 100 120 minutes
single glucose rinse
Acidity in the mouth after drinking a sweetened beverage
7.0
6.0
5.0
4.0
Plaque pH
critical pH
0 20 40 60 80 100 120 minutes
First sip
Second sip
Third sip
Fourth sip
Acidity after repeated exposures to a sweetened beverage
Acidity (pH) Sugar (tsp)
Water 7.00 0.0
Diet Coke 3.39 0.0
Mountain Dew 3.22 11.0
Diet Pepsi 3.05 0.0
Gatorade 2.95 3.3
Coke 2.53 9.3
Pepsi 2.49 9.8
Double Trouble: pH and Sugar Content
Challenges for Change
Public Health cannot compete with industry’s advertising budget
Mandated changes are controversial Lifestyle changes are difficult for
individuals
Aim for small improvements over time
Hope for Change
Simple policies can promote health Activity promotion fits in well with
fun school events Alternative fund raisers Children adapt to new ideas and
experiences School provides a venue for
experiencing new tastes and activities
Why Change the School Health Environment?
Education is a process of planning and preparing for a successful future
Why Schools?
Schools play a role in demonstrating to the parents and community the elements that lead to a successful and healthy lifestyle
Children spend time in school
Roles for Schools
Continue to provide nutritionally balanced meals to children Coordinate nutrition education with
opportunities to eat healthy foods. Support nutrition education messages in
the overall school environment. Provide tools for lifelong physical
activity and healthy eating.
Nutrition for Schools in the 21st Century
Budget constraints for schools and school meal programs
Shortened meal times Weak regulations for physical activity
and health in schools School meals must compete with
offerings both on and off campus Foods sold in competition with the
school lunch program for revenue are often of minimal nutritional value
Carbonated Soft Drink Sales• Source of revenue for schools• Competes with goals & revenue of
school lunch• Conflicts with nutrition education
message• USDA regulations only limit
placement & timing of vending machines
Carbonated Soft Drinks in the School
Potential to disrupt the classroom Sugar intake gives children a surge of
energy followed by a drop of energy. More than 51 million school hours are
lost each year to dental-related illness.
American Dental AssociationPolicy: 2000
House of Delegates : oppose contracts that offer
increased access of soft drinks to children and influence their consumption patterns.
calls for continued monitoring of scientific facts and data on the oral health effects of soft drinks.
(2000)
Taking a Position on Healthy School Environments American Dietetic Association American Academy of Pediatrics Society for Nutrition Education Centers for Disease Control and
Prevention Center for Food and Justice American School Food Service
Association
• Create school meal advisory teams of students, parents and teachers to assist in selected menu items.
• Survey students on preferred foods. • Educate students about serving sizes• Employ economies of scale to increase
revenue• Ensure that food sale revenues for
competitive foods are credited to the school food service
Develop positive, healthy options for vending, school stores,
cafeteria environment Ask soft drink companies to
market healthier alternatives. Provide water, 100% juices, milk
and soy drinks
Require closed campuses during lunch periods.
Competitively price healthy foods Sell items that increase physical
activity: pedometers, water bottles. Establish relationships with local
food producers Participate in school gardening
projects
• Ensure that adequate time and space is available for all children to eat comfortably
• Schedule recess before lunch• Encourage teachers and staff to
eat with children
Limit use of food and candy as a reward.
Encourage fund raising efforts associated with healthy lifestyles
Provide daily recess Plan physical education that is
inclusive of all students, including those with disabilities
Fruit & Vegetable Pilot Project 25 schools in Iowa Free fruits & vegetables provided
throughout the day Children learned new foods; enjoyed
them Decreased use of vending machines Positive influence on school
environment
ResourcesSchool Health Index• http://www.cdc.gov/nccdphp/dash• http://www.cdc.gov/nddphp/dnpaChanging the Scene• www.fns.usda.gov/tnFit Healthy & Ready to Learn• http://www.nasbe.org/HealthyScho
ols/healthy_eating.html
More Resources
Team Nutrition• www.fns.usda.gov/tnHealthy Schools Summit• www.actionforhealthykids.orgAlternative ways to raise money
– http://www.scn.org/edu/cccs/– www.commercialfree.org
Conclusions
Schools can positively impact the health of students
A number of options are available to implement school health programs.
A number of tools are available to evaluate environments within schools
AcknowledgementsThanks to the following persons who have
provided expertise and visual support for this presentation
Dr. Michael Kanellis, DDS, MSDr. Jonathan Shenkin, DDS, MPHLinda Snetselaar, RD, PhDEva Tsalikian, MD
University of Iowa School of Dentistry, College of Public Health and College of Medicine