Heese 2009 Current Strategies in the Mgt of Lysosomal Storage Diseases
-
Upload
bolicious8 -
Category
Documents
-
view
7 -
download
2
Transcript of Heese 2009 Current Strategies in the Mgt of Lysosomal Storage Diseases

CMB
Tgilompt(go
emmcNbs(asja
F
D
A
1d
urrent Strategies in theanagement of Lysosomal Storage Diseases
ryce A. Heese, MA, MD
Lysosomal storage diseases (LSDs) comprise a diverse group of over 40 clinically distinctinherited disorders. LSDs are progressive and may present at any age affecting any numberof tissues and organ systems. They result from a genetic defect in cellular transport ormetabolism of molecules within the lysosome. Treatment is directed toward symptomaticcare of secondary complications for most of these diseases. For some individuals, hema-topoietic stem cell transplantation or enzyme-replacement therapy can be effective. How-ever, limitations in these therapies still exist. To date, there is no cure for any of the LSDs.Early diagnosis and treatment is essential for optimal treatment; this lends support toimplementing mass newborn screening for LSDs.Semin Pediatr Neurol 15:119–126 © 2008 Elsevier Inc. All rights reserved.
zAef(wmoc
mctdtdcsto
n(lhsmlfu
he lysosome is an intracellular organelle essential for thebiochemical breakdown of several molecules, such as
lycosaminoglycans (GAGs), oligosaccharides, sphingolip-ds, and other lipids. Defects of lysosomal metabolism, orysosomal storage diseases (LSDs), comprise a diverse groupf over 40 inherited disorders. These disorders are caused byutations in genes that code for lysosomal enzymes, trans-ort proteins, or other gene products essential for a func-ional lysosomal system. As a result, abnormal accumulationor storage) of substrates within the lysosome leads to pro-ressive cellular impairment and dysfunction of numerousrgans and systems.The genes that code for lysosomal proteins are present in
very cell. However, because of unique metabolic require-ents of different cell types, a defect in a lysosomal enzymeay have a significantly greater impact in a certain tissue
ompared with other tissues. For example, the enzyme-acetyl-galactosamine-6-sulfate is critical in the lysosomalreakdown of keratin sulfate, primarily found in the skeletalystem. A defect in this enzyme, as in mucopolysaccharidosisMPS) type IVA (Morquio syndrome), causes abnormal stor-ge of keratin sulfate in the skeletal system, thus resulting inevere skeletal growth problems, dysostosis multiplex, andoint disease. Cardiac valve disease and corneal clouding arelso features of Morquio syndrome, but, in general, this en-
rom the Department of Pediatrics, Division of Genetics and Metabolism,University of Florida, Gainesville, FL.
r Heese is supported in part by an educational grant from Genzyme Cor-poration.
ddress reprint requests to Bryce A. Heese, MA, MD, Department of Pediatrics,
sPO Box 100296, Gainesville, FL 32610. E-mail: [email protected]071-9091/08/$-see front matter © 2008 Elsevier Inc. All rights reserved.oi:10.1016/j.spen.2008.05.005
yme defect relatively spares most nonskeletal organ systems.lternatively, the lysosomal enzyme, galactocerebrosidase, isssential for metabolizing galactosylceramide, a sphingolipidound in myelin. Individuals with a defect in this enzymeKrabbe disease [globoid cell leukodystrophy]) will presentith progressive neuroregression. Other defects of sphingo-yelin degradation, such as metachromatic leukodystrophy
r GM2 gangliosidosis, also have predominantly abnormalentral nervous system (CNS) findings.
LSDs typically are not evident at birth, and they are com-only progressive in nature. Diagnosis can be difficult be-
ause of the marked variability in clinical presentation amonghe group and the subtle progressive nature of many of theseisorders. An astute pediatrician may be able to quickly iden-ify problems in an infant with classic MPS IH (Hurler syn-rome) with coarsening features and neurodegenerative de-line. However, more attenuated forms of MPS I (Scheieyndrome), with slowly progressive mild coarsening of fea-ures and normal cognition, may go unnoticed for years withnly vague nonspecific symptoms being reported.Among specific enzyme defects, marked variability in phe-
otypic presentation also exists. For example, Pompe diseaseacid maltase deficiency) is a disorder of glycogen metabo-ism that manifests as severe infantile onset with hypotonia,ypertrophic cardiomyopathy, and failure to thrive. Theame enzyme defect can also result in adult-onset proximaluscle weakness, respiratory insufficiency, and complete
ack of cardiac findings. Of note, Pompe disease is also re-erred to as glycogen storage disease (GSD) type II. However,nlike other GSDs, Pompe disease is functionally a lysosomal
torage disease and thus is the only GSD considered in this119

rscdpcdaaccftot
sdtte
sho(LmeTpahwlbs
HHdhf
shdHKosKnltla
asAi
tftdpt1mraaap
ETwtzbdmtbmttmec
Fcubmsdti
spltbfatat
120 Bryce A. Heese
eview. Niemann Pick disease type C typically presents withignificant hepatosplenomegaly, ataxia, and dystonia in earlyhildhood. However, a late-onset variant of Niemann Pickisease can present in adolescence or even adulthood withrogressive behavioral and psychiatric problems without vis-eral manifestations. Cystinosis is a unique LSD caused by aefect in a lysosomal (anion) transporter that results in theccumulation of cystine crystals, particularly in renal tissuesnd in the cornea. This disorder generally presents in earlyhildhood with significant growth failure, rickets, renal Fan-oni syndrome, and photophobia. Individuals are often re-erred to and/or diagnosed by pediatric nephrologists andypically progress to renal failure. However, an adult variantf this disorder can present with only photophobia caused byhe accumulation of crystals within the cornea.
The ability to describe each LSD in detail is beyond thecope of this review. Table 1 lists over 40 known lysosomalefects and their classic phenotype, with the understandinghat most of these diseases can have quite variable presenta-ions. Diagnostic testing and treatments specific to each dis-ase are also listed in Table 1.
Classically, the treatment of LSDs has been limited toymptomatic care of disease manifestations. Recent decadesave observed the development and continual improvementf therapies such as hematopoietic stem cell transplantationHCT) and enzyme-replacement therapy (ERT) for selectSDs. For many, this has led to significant clinical improve-ent and enhanced quality of life. It has been shown that
arlier diagnosis and treatment improves overall outcome.1
herapy should, ideally, be initiated presymptomatically torovide the best outcome. This may be possible for ansymptomatic patient diagnosed because of a known familyistory; however, most patients who are diagnosed clinicallyill be symptomatic by the time therapy is initiated, regard-
ess of how astute the clinician may be. This underscores theenefits to developing and introducing mass newborncreening for LSDs.
CTCT is an important treatment in several inherited metaboliciseases including LSDs. The objective of HCT is to engraftealthy cells (without genetic defect) into a patient withoutunctional enzyme.
The first HCT for an LSD was in an individual with Hurleryndrome in 1980.2 The relative success of this procedureas been followed by over 900 HCTs for inherited metaboliciseases with mixed results.3 Most clinical information onCT in LSDs comes from patients with Hurler syndrome andrabbe syndrome, but there is limited experience in manyther conditions within this group.4-8 For disease types withignificant CNS deterioration, such as MPS type I (Hurler) orrabbe disease, HCT is known to only be effective in theeonatal or presymptomatic stage of the disease. Another
imitation of HCT is that skeletal disease is not affected byreatment. The greatest challenge to HCT is transplant-re-ated mortality rate, which has been reported between 10%
nd 25%.9 Continually improving techniques and the use of slternative stem cell sources, such as umbilical cord bloodtem cells, will likely lead to better outcomes in the future.10
ll things considered, HCT remains a viable option for somendividuals with LSDs.
Based on clinical experience with transplant in LSDs, Pe-ers and Steward1 suggest that HCT be considered in theollowing diseases: MPS type IH (Hurler syndrome), MPSype VI (Marateaux-Lamy syndrome), MPS type VII (Sly syn-rome), Krabbe disease, metachromatic leukodystrophy, al-ha-fucosidosis, alpha-mannosidosis, Gaucher disease (al-hough ERT is available and is the first-line treatment for type), and Niemann-Pick disease type B. For most other lysoso-al defects, there are either limited or discouraging data to
ecommend HCT. Because of the progressive nature and vari-bility of each disease, a comprehensive, multidisciplinarypproach should be used in each case to determine whetherpatient is a good candidate for HCT.1 Ideally, this should beerformed in a center with experience in LSDs.
RThe concept of enzyme replacement was realized decades agoith observations in experimental fibroblast cell lines of MPS
ype I and MPS type II patients in whom the respective en-yme defect in either cell type was corrected by culturingoth cells together.11 Lysosomal enzymes and proteins pro-uced in the cell are posttranslationally modified with certainarkers, such as a mannose-6-phosphate moiety. These pro-
eins are directed to the lysosome in which specific mem-rane receptors (in this instance, a mannose-6-phosphateembrane receptor) help endocytose the protein for use in
he lysosome. Lysosomal proteins may also be excreted out ofhe cell and taken up by other cells and specific lysosomalembrane receptors within that cell, as was observed by the
arly studies of mixing MPS I and MPSII cell lines.12 Thisoncept is the basis for current ERT for 6 of the LSDs (Fig 1).
Enzyme replacement first became clinically available withood and Drug Administration approval in 1991.13 Imiglu-erase is a recombinant enzyme for the treatment of individ-als with nonneuronopathic (type 1) Gaucher disease. It haseen reported to reduce hepatosplenomegaly, improve ane-ia and thrombocytopenia, and reduce episodes of pain cri-
es in these patients.13,14 Because the recombinant enzymeoes not cross the blood-brain barrier, it is not effective inype 2 Gaucher disease patients with severe CNS abnormal-ties.15
Fabry disease is an X-linked disorder that typically pre-ents in adolescent or adult males with acroparesthesia, hy-ohidrosis, and vague gastrointestinal symptoms and often
eads to progressive renal failure and cardiomyopathy. Un-reated, the life expectancy for males with Fabry is reported toe 40 to 55 years. Although this is an X-linked disorder,emales are indeed symptomatic.16 ERT using recombinantlpha-galactosidase A has been clinically available for pa-ients with Fabry disease since 2003. Improvement in painnd gastrointestinal symptoms has been reported, but long-erm studies are required for evaluating its efficacy with re-
pect to life-threatening complications.17,18
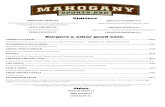
Table 1 LSDs, Typical Presentation, Unique Diagnostic Features, and Disease-Specific Treatments and Investigational Therapies
Disorder (enzyme or defect) Clinical Manifestations Diagnostic Features Specific Treatment
Defects in Glycosaminoglycan DegradationMPS type I; Hurler & Scheie s. (alpha-L-
iduronidase)Coarse, hydrocephalus, dysostosis multiplex,
valve, airway obst; cornea; MR in Hurler,milder in Scheie s.
Urine GAG screen; enzyme (leuk, fibr);molecular
ERT; HCT for Hurler Investigational:intrathecal ERT
MPS type II; Hunter syndrome(iduronate-2-sulfatase)
X-linked; MR, coarse, hydrocephalus,dysostosis multiplex, airway obstruction,valve
Urine GAG screen; enzyme (leuk, fibr);molecular
ERT; investigational: intrathecalERT
MPS type III; Sanfilippo syndrome (typesA-D; different enzymes)
MR, behavior and aggression probs., seizures Urine GAG screen; enzyme (leuk, fibr);molecular
MPS type IV; Morquio syndrome (typesA & B; different enzymes)
Normal cognition, coarse, dysostosismultiplex
Urine GAG scrn; Enzyme (leuk, fibr);Molecular
MPS type VI; Maroteaux-Lamy s.(arylsulfatase B)
Normal cognition, coarse, dysostosismultiplex, HSM, valve
Urine GAG scrn; Enzyme (leuk, fibr);Molecular
ERT; HCT for severe form
MPS type VII; Sly syndrome (beta-glucuronidase)
MR, coarse, dysostosis multiplex, HSM,Hydrops fetalis
Urine GAG screen; enzyme (leuk, fibr);molecular
MPS type IX; Natowicz syndrome(hyaluronidase)
Skeletal problems, periarticular soft-tissuemasses (single patient)
Molecular
Defects in Glycoprotein (oligosaccharide; carbohydrate side-chain) Degradationalpha-Mannosidosis (alpha-
mannosidase)MR, coarse, cerebellar ataxia, psychiatric,
dysostoses multiplex, corneal, HSMVacuo lymph; urine oligo screen; enzyme
(leuk fibr); molecularHCT
beta-Mannosidosis (beta-mannosidase) MR, coarse, hypotonia, spasticity, neuropathy Urine oligo screen; enzyme (leuk fibr);molecular
Fucosidosis (alpha-fucosidase) MR, coarse, spasticity, cardiomegaly,myoclonic
Urine oligo screen; enzyme (leuk fibr);molecular
HCT (limited experience)
Sialidosis; Mucolipidosis type I (alpha-N-acetyl neuraminidase)
(type I) Vision, myoclonic, spasticity,neuropathy; (type II) coarse, dysostosismultiplex, cherry red
Urine oligo screen; enzyme (fibr);molecular
Aspartylglucosaminuria(aspartylglucosaminidase)
MR, coarse, behavioral, HSM Vacuo lymph; urine oligo screen; enzyme(leuk fibr); molecular
HCT (limited experience)
Schindler disease (alpha-N-acetyl-galactosaminidase)
MR, spasticity, myoclonic; adult onset(Kanzaki d.) milder, angiokeratoma corporisdiffusum
Vacuo lymph; urine oligo screen; enzymestudies (leuk fibr); molecular testing
Defects of Glycolipid Degradation (particularly, sphingolipids found in nervous tissue)Globoid cell leukodystrophy or Krabbe
disease (galactocerebrosidase)MR, leukodystrophy, spasticity, neuropathy,
(late-onset variants too)Enzyme (leuk fibr); molecular HCT Investigational: ERT, small
molecule therapyMetachromatic leukodystrophy
(arylsulfatase A)MR, leukodystrophy, spasticity, neuropathy,
(late onset variants too)Urine sulfatides, Ultrastructure lipid
deposits (bx); enzyme (leuk, fibr);molecular
HCT Investigational: ERT
GM1-gangliosidosis (beta-galactosidase) MR, coarse, hypotonia, cherry red, dysostosismultiplex, HSM, hydrops fetalis, (latevariants too)
Urine oligo screen; enzyme (leuk fibr);molecular
HCT (limited experience)
Lyosomalstorage
diseases121

Table 1 Continued
Disorder (enzyme or defect) Clinical Manifestations Diagnostic Features Specific Treatment
GM2-gangliosidosis; Tay-Sachs (alpha-hexosaminidase A; beta-subunit)
MR, spasticity, myoclonic, cherry red, (lateronset variants too)
Urine oligo screen; enzyme (leuk fibr);molecular
Investigational: small-moleculetherapy
GM2-gangliosidosis; Sandhoff d. (beta-hexosaminidase A & B; alpha subunit)
MR, spasticity, myoclonic, cherry red Urine oligo screen; enzyme (leuk, fibr);molecular
Gaucher disease types I, II, III (beta-glucocerebrosidase)
(Type I) later onset, HSM, anemia,thrombocytopenia, bone pain (Type II)MR, spasticity, myoclonic, HSM, hydropsfetalis
Ultrastructure lipid storage in macrophages(bone marrow); enzyme (leuk, fibr);molecular
ERT; HCT type I; Small moleculetherapy
Fabry disease (alpha-galactosidase A) X-linked; pain crises, acroparesthesia,hypohidrosis, angiokeratoma, corneal,kidney, cardiovascular; females affected
Enzyme (leuk, fibr); molecular ERT
Farber disease (ceramidase) MR, neuropathy, hoarse, skin nodules Cellular ultrastructure (nodule bx); enzyme(fibr); molecular
HCT (limited experience)
Niemann-Pick type A & B (sphingomyelinase) Type A (neuropathic): MR, myoclonic,cherry red, cornea, lung disease, HSMType B: HSM, lung disease
Vacuo lymph; Ultrastructure (bone marrowbx); enzyme (leuk, fibr); molecular
For type B: HCT (limitedexperience); Investigational:ERT
Defect in Glycogen DegradationPompe disease; GSD type II (alpha-
glucosidase)Infantile: hypotonia, myopathy, hypertrophic
cardiomyopathy, FTT, Adult: proximalmuscle weak, no cardiac
Creatine kinase; vacuo lymph; Urine oligoscreen; enzyme (fibr); molecular
ERT
Defect in Polypeptide DegradationPycnodysostosis (cathepsin K; cysteine
protease)Skeletal deformation, fractures Radiologic; molecular
Cholesterol and Lipid Transport DefectsCeroid lipofuscinosis CLN1 (palmitoyl
protein thioesterase 1) CLN2 (tripeptidylpeptidase 1) CLN3 (membrane protein)
Psychomotor regression, myoclonic,blindness CLN1, CLN2, CLN3 and others
Vacuo lymph; Ultrastructure deposits (skin,nerve bx, leuk); enzyme (leuk fibr forCLN1); molecular
HCT for CLN1 & CLN2 (limitedexperience)
Niemann-Pick d. type C (intracellularcholesterol esterification & transport)
Psychomotor regression, hypotonia, liverdisease, vertical supranuclear palsy,dystonia, seizures; later onset variantswith psychiatric and dementia
vacuo lymph; ultrastructure (bone marrowbx); in vitro cholesterol esterification(fibr); molecular
Investigational: small moleculetherapy
Wolman disease (acid lipase; cleavecholesterol esters from LDL)
Psychomotor regression, FTT, diarrhea,stearrhea, HSM, adrenal calcifications;adult variants with atherosclerosis
Serum cholesterol; vacuo lymph; enzyme(leuk)
Defects in Multiple Lysosomal EnzymesMultiple sulfatase deficiency (sulfatase-
modifying factor 1)Features of MLD, and MPS types II, III, IV,
& VI, as well as ichthyosis and proptosisUrine GAG screen, enzyme (numerous
sulfatase deficiencies); molecularGalactosialidosis (protective
protein/cathepsin A)(early severe) MR, coarse, spasticity,
cherry red, cornea, dysostosis multiplex,HSM, hydrops fetalis, (late onset var.)
Vacuo lymph; Urine oligo screen; Enzyme(fibr); increased serum lysosomalenzymes; molecular
122Bryce
A.Heese

Table 1 Continued
Disorder (enzyme or defect) Clinical Manifestations Diagnostic Features Specific Treatment
Mucolipidosis type II (I-Cell d.) & typeIII (pseudo Hurler disease) (N-acetylglucosamine 1-phospotransferase)
Similar to MPS I: MR, hydrocephalus, coarse,dysostosis multiplex, valve, HSM Type III ismilder disease
Vacuo lymph; urine oligo screen;enzyme (fibr);increased several serumlysosomal enzymes; molecular
Lysosomal transport defectsCystinosis (cystosin; lysosomal
membrane transporter)Renal tubular fanconi, FTT, rickets, corneal
crystals Non-nephrotic/adult–photophobiaonly
Corneal crystals (slit lamp);Ultrastructure crystals (bone marrow,conjunctiva, renal); leukocyte cystine;molecular
Oral cysteamine, renal transplant;investigation: cysteamine eyedrops
Cobalamin F Defect (lysosome releaseof Vit B12)
MR, FTT, seizures, rash, stomatitis, Serum/urine methylmalonic acid, Plasmahomocysteine
Vitamin B12
Mucolipidosis IV (mucolipidin;receptor-stimulated cation channel)
MR, spasticity, cornea, retinopathy Plasma gastrin; vacuo lymph;ultrastructure inclusions (skin, cornealbx); molecular
Sialic acid storage disease (sialin;lysosomal anion transporter)
MR, coarse, hypotonia, cerebellar ataxia HSMAdult (Salla d.) slow progressive onset
Sialic acid in urine; molecular
Sialuria (UDP-N-acetylglucoamine-2-epimerase)
MR, coarse, hypotonia, myoclonic, HSM Sialic acid in urine; molecular
Chediak-Higashi syndrome (lysosomaltrafficking regulator)
Psychomotor regression, oculocutaneousalbinism, bleeding diathesis, recurrentinfection
Ultrastructure granules (leuk, bonemarrow)
HCT
Danon disease (lysosome-associatedmembrane protein-2)
X-linked, MR, cardiomyopathy, muscle weak,retinopathy
Creatine kinase; vacuoles (muscle);molecular
Heart transplant
Unknown mechanism (speculated lysosomal storage disease)Marinesco-Sjögren syndrome (ER
glycoprotein enhances proteinsynthesis)
MR, microcephaly, FTT, cerebellar ataxia,weakness, spasticity, cataracts, skeletal,hypogonadotropic hypogonadism
Ultrastructure inclusion bodies (leuk);molecular
Hermansky-Pudlak syndrome (severalgenes implicated)
Oculocutaneous albinism, bleeding diathesis,pulmonary fibrosis, granulomatous colitis
Ultrastructure absent dense bodies inplatelets; Molecular
Geleophysic dysplasia (not known) MR, seizures, happy-nature appearance,skeletal, cardiac valve, hepatomegaly
Ultrastructure storage vacuoles (live,cartilage, heart)
Defects of Activator ProteinsGM2-gangliosidosis AB-variant (beta-
hexosaminidase activator)Features of GM2 gangliosidosis: MR,
hypotonia, cherry redEnzyme (leuk, fibr); molecular
Saposin A; Krabbe variant Features of Krabbe (single case report) Enzyme; molecularSaposin B; MLD variant Features of MLD Enzyme; molecularSaposin C; atypical Gaucher Features of Gaucher types II/III Ultrastructure (nerve); molecular
Many lysosomal storage diseases have a wide clinical spectrum; however, only common features are noted here.Abbreviations: MR � mental retardation, includes developmental delay and developmental regression; myoclonic � myoclonic seizures; HSM � hepatosplenomegaly; valve � cardiac valve disease;
FTT � failure to thrive; cornea � corneal clouding or crystals; cherry red � cherry red macular spot; GAG � glycosaminoglycans; oligo � oligosaccharides; vacuo lymph � vacuolatedlymphocytes; leuk � leukocytes; fibr � fibroblasts; bx � biopsy; ER � endoplasmic reticulum; GSD � glycogen storage disease; MLD � metachromatic leukodystrophy.
Lyosomalstorage
diseases123

rtgtt
ibja
pwatrfo
ipmc
sd
ldifairrttlmmitdib
td
(smt
s avail
124 Bryce A. Heese
Laronidase was approved in 2003 for use in MPS I witheported improvements in hepatosplenomegaly and respira-ory disease and showing a decrease in urinary glycosamino-lycan excretion.19 However, HCT remains the mainstay ofherapy for MPS I but at the risk of HCT-related complica-ions.
Recombinant arylsulfatase B was approved for clinical usen MPS VI (Maroteaux-Lamy syndrome) in 2005 and haseen associated with improvements in hepatosplenomegaly,
oint movement, cardiopulmonary function, and pain as wells reduced excretion of urinary glycosaminoglycans.20
Alglucosidase alpha is Food and Drug Administration ap-roved for use in infantile Pompe disease. A portion of infantsho are diagnosed and treated with ERT before 6 months of
ge had improved survival and quality of life compared withhe observed natural history of the disease, yet, for unknowneasons, a subset of the treated cohort did not show effectsrom ERT.21 ERT studies for late-onset Pompe disease arengoing.The latest recombinant human enzyme available clinically
s idursulfase for the treatment of MPS II (Hunter syndrome)atients. Clinical trials showed improvement in cardiopul-onary disease and hepatosplenomegaly and decreased ex-
retion of urinary glycosaminoglycans.22
There are a number of challenges to ERT. ERT has beenhown to halt progression and even reduce the disease bur-
Figure 1 A depiction of ERT. A cell with a dysfunctiowith abnormal accumulated storage material (bottom lmodified with a mannose 6-phoshate group, is (1) targeendosome combines with a dysfunctional lysosome, andfunctional exogenous enzymes. The accumulated storagand structure of the lysosome. (Color version of figure i
en in certain tissues. However, it is apparent that ERT has v
ittle effect on the brain, skeletal tissue, and valvular heartisease in LSDs. Infusion-related events have been noted in
ntravenous ERT. Mild allergic reactions, such as urticaria,ever, and chills, are typically treatable with antihistaminesnd nonsteroidal antiinflammatory drugs and reduction innfusion rate. The development of neutralizing antibody toecombinant enzyme followed by clinical decline has beeneported; however, most patients who seroconvert developolerance to the enzyme. Rarely, a patient will have to discon-inue therapy because of adverse infusion reactions.23,24 Life-ong, frequent infusions are another challenge of ERT that
ust be weighed against the burden of disease. Current treat-ent protocols consist of frequent intravenous access and
nfusion, which vary from weekly to monthly depending onhe protocol.25 In some instances, this may require long-istant travel to an infusion facility. However, local and even
n-home infusions are available and can alleviate some of theurden of infusion therapy.Alternative delivery of recombinant enzymes, such as in-
rathecal injection of recombinant enzymes in Hurler syn-rome, has been proposed and is currently investigational.26
The estimated cost of ERT is between $90,000 to $565,000US), depending on the disease (therapy) and patientize.25,27 Costs are driven by extraordinary financial invest-ent in research and development taken on by pharmaceu-
ical companies who take a risk in developing therapies for
somal enzyme is shown exhibiting swollen lysosomesxogenous enzyme (or recombinant enzyme), which iscellular membrane receptors and endocytosed. (2) Thedefective enzymes within the lysosome are replaced by
rial can be metabolized, improving the overall functionable online.)
nal lysoeft). Eted to(3) thee mate
ery rare disorders. A small portion of those developmental

cltugttpfi
SFifptor(aczpr
tiftCtmfodDus
cfwaTgibaddotla
GGaiLboahifrd
NAvlgipf
dvlpsatsttripvpsobwK
SLrasHumr
Lyosomal storage diseases 125
osts and Food and Drug Administration approval fees areessened by the Orphan Drug Act of 1983, without whichhere may not have been incentive to develop ERT for clinicalse. However, it has also been argued that this act, whichrants 7 years exclusivity, also eliminates competition in set-ing costs.27 To the credit of the respective ERT pharmaceu-ical companies, each has set up some form of patient-sup-ort system to help gain coverage and access and to take thenancial stress off of the clinical staff and patients.
mall-Molecule Therapyor many LSDs, there is a promise of continual technical
mprovements in existing therapies. However, even success-ul HCT and ERT will likely continue to have limitations,articularly in the treatment of CNS and skeletal manifesta-ions that occur in most of these disorders. A significant fieldf research deals with small-molecule therapies that could beelevant to LSDs. The hope of this treatment is to offer simplelikely oral) medication that can cross the blood-brain barriernd be more readily distributed throughout the body. Theseompounds are directed at either enhancing the existing en-yme function, as in chaperone molecules, or by limiting theroduction-offending substrate (or abnormal storage mate-ial), as in substrate-reduction therapy.
Chaperones are small molecules whose role is to enhancehe formation of protein products of a cell. Because a proteins transcribed from RNA, it must be correctly folded into aunctional product. Misfolded proteins are likely nonfunc-ional and more rapidly degraded by cellular proteases.haperone therapy may be beneficial in inherited diseases
hat are caused by genetic mutations causing small confor-ational changes in the protein, often missense mutation or
rame-shift deletions.28 In this treatment modality, a chaper-ne would assist a protein in folding and help avoid degra-ation to produce a (at least partially) functional enzyme.iseases caused by null mutations, resulting in no gene prod-ct, would not be expected to be aided by chaperone therapyo this type of therapy would be mutation dependent.
Substrate-reduction therapy is directed at reducing the ac-umulation of storage molecules by inhibiting their initialormation. N-Butyldeoxynojirmimycin is the only drugithin this category that is Food and Drug Administration
pproved for use in an LSD, specifically Gaucher disease.29
his compound works by inhibiting the enzyme ceramidelucosyltransferase from producing glucosylceramide, whichs accumulated in this disease. The recommended use of N-utyldeoxynojirmimycin would include the treatment ofdults with mild or moderate Gaucher disease who cannot oro not wish to be on ERT or Gaucher patients with persistentisease despite ERT.30 Trials are also ongoing for the efficacyf N- butyldeoxynojirimycin in patients with Niemann-Pickype C because this condition is also associated with accumu-ation of glucosylceramide.31 Another trial using isoflavone as
substrate inhibitor in MPS type III is being evaluated.32 sene Therapyene therapy is the insertion of a functional gene to produceworking enzyme and replace the defective one and prom-
ses a potential cure for many inherited diseases includingSDs. Currently, several different LSD animal models areeing studied by either direct gene transfer using viral vectorsr by genetically altering defective hematopoietic stem cellsnd then returning them to the donor.24 A small (n � 3)uman clinical trial in Gaucher disease did not show signif-
cant clinical improvement.33 Since that time, clinical trialsor gene therapy have been limited because of safety concernsesulting from a few case reports of complications in otheriseases.34,35
ewborn Screenings treatment options for LSDs improve, there is a clear ad-antage for early, preferably presymptomatic, diagnosis. Thisends support to developing newborn screening for thisroup of disorders. Since its inception in the early 1960s,ndividuals with inborn errors of metabolism, particularlyhenylketonuria, and other inherited diseases have benefitedrom early, presymptomatic treatment.36
For decades, most states screened for only a handful ofisorders as a result of the complexity of screening for indi-idual disorders. One of the most significant advances in theast decade has been the implementation of a high-through-ut, multiplex technique using tandem mass spectrometry tocreen for dozens of organic acidemias, amino acidopathies,nd fatty acid oxidation defects. Today, almost every state inhe United States and numerous countries have adopted thiscreening modality.37 This has also paved a way for poten-ially adding a multiplex screening technique aimed at de-ecting LSDs. Methods have been developed and are cur-ently being piloted using either tandem mass spectrometrydentification of enzyme reaction products or immunologicrotein assay of several markers. Both methods have beenalidated to detect several different LSDs, and both are re-orted to be capable of being high throughput for masscreening at costs comparable to current screening meth-ds.38-40 It is difficult to determine when/if LSD screening wille adopted by most screening programs; however, it is note-orthy that the state of New York has been screening forrabbe disease since 2006.41
ummarySDs comprise a diverse group of disorders; each is relativelyare, but, as a group, they have an estimated incidence ofbout 1 in 7,000. For most LSDs, management is still re-tricted to treating secondary complications of the disease.owever, within the past decade, treatment options, partic-larly HCT and ERT, have substantially changed manage-ent in a few lysosomal diseases. These therapies are di-
ected at the primary (enzymatic) defect and have been
hown to halt progression and even reverse some features of
tc
R
1
1
1
1
1
1
1
1
1
1
2
2
2
2
2
2
2
2
2
2
3
3
3
3
3
3
3
3
3
3
4
4
126 Bryce A. Heese
he disease. However, limitations exist in treatment, and noure exists for any of these disorders.
eferences1. Peters C, Steward C: Haematopoietic cell transplantation for inherited
metabolic diseases: An overview of outcomes and practice guidelines.Bone Marrow Transplant 31:229-239, 2003
2. Hobbs J, Hugh-Jones K, Barrett A, et al: Reversal of clinical features ofHurler’s disease and biochemical improvements after treatment bybone-marrow transplantation. Lancet 2:709-712, 1981
3. Rovelli A, Steward C: Haematopoietic cell transplantation activity inEurope for inherited metabolic diseases: Open issues and future direct-sions. Bone Marrow Transplant 35:S23-S26, 2005
4. Boelens J: Trends in haematopoietic cell transplantation for inbornerrors of metabolism. J Inherit Metab Dis 29:413-420, 2006
5. Beck M: New therapeutic options for lysosomal storage disorders: En-zyme replacement, small molecules and gene therapy. Hum Genet 121:1-11, 2007
6. Peters C, Balthazor M, Shapiro E, et al: Outcome of unrelated donorbone marrow transplantation in 40 children with Hurler syndrome.Blood 87:4894-4902, 1996
7. Escbolar M, Poe M, Provenzale J, et al: Transplantation of umbilical-cord blood in babies with infantile Krabbe’s disease. N Engl J Med352:2069-2081, 2006
8. Krivit W: Allogeneic stem cell transplantation for the treatment of ly-sosomal and peroxisomal metabolic disease. Semin Immunol 26:119-132, 2004
9. Hoogerbrugge P, Brouwer O, Bordigoni P, et al: Allogeneic bone mar-row transplantation for lysosomal storage diseases. The EuropeanGroup for Bone Marrow Transplantation. Lancet 345:1398-1402, 1995
0. Martin P, Carter S, Kernan N, et al: Results of the cord blood transplan-tation sticy (COBLT): Outcomes of unrelated donor umbilical cordblood transplantation in pediatric patients with lysosomal and peroxi-somal storage diseases. Biol Blood Marrow Transplant 12:184-194,2006
1. Fratantoni J, Hall C, Neufeld E: Hurler and Hunter syndromes: Mutualcorrection of the defect in cultured fibroblasts. Science 162:570-572,1968
2. Van der Ploeg A, Kroos M, Willemsen R, et al: Intravenous administra-tion of phosphorylated acid alpha-glucosidase leads to uptake of en-zyme in heart and skeletal muscle of mice. J Clin Invest 87:513-518,1991
3. Barton N, Brady R, Dambrosia J, et al: Replacement therapy for inher-ited enzyme deficiency—Macrophage-targeted glucocerebrosidase forGaucher disease. N Engl J Med 324:1464-1470, 1991
4. Grabowski G, Barton N, Pastores G, et al: Enzyme therapy in type 1Gaucher disease: Comparative efficacy of mannose-terminated gluco-cerebrosidase from natural and recombinant sources. Ann Intern Med122:33-39, 1995
5. Migita M, Hamada H, Fujimujra J, et al: Glucocerebrosidase level in thecerebrospinal fluid during enzyme replacement therapy—Unsuccess-ful treatment of the neurological abnormality in type 2 Gacucher dis-ease. Eur J Pediatr 162:524-525, 2003
6. MacDermot K, Homes A, Miners A, et al: Natural history of Fabrydisease in affected males and obligate female carriers. J Inherit MetabDis 24:24-24, 2001 (suppl 2)
7. Ramaswami U, Wendt S, Pintos-Morell G, et al: Enzyme replacementtherapy with agalsidase alfa in children with Fabry disease. Acta Paedi-atr 96:122-127, 2007
8. Banikazemi M, Bultas J, Waldeck S, et al: Agalsidase-beta therapy foradvanced Fabry disease: A randomized trial. Ann Intern Med 146:77-86, 2007
9. Wraith J, Clarke L, Beck M, et al: Enzyme replacement therapy for
mucopolysaccharidosis I: A randomized, double-blinded, placebo-con-trolled, multinational study of recombinant human alpha-L-iduronidase(laronidase). J Pediatr 144:581-588, 2004
0. Harmatz P, Giugliani R, Schwartz I, et al: Enzyme replacement therapyfor mucopolysaccharidosis VI: A phase 3, randomized, double-blind, pla-cebo-controlled, multinational study of recombinant human N-acetyl-galactosamine 4-sulfatase (recombinant human arylsulfatase B or rhASB)and follow-on, open-label extention study. J Pediatr 148:533-539, 2006
1. Kishnani P, Corzo D, Nicolino M, et al: Recombinant human acidalpha-glucosidase: Major clinical benefits in infantile-onset Pompe dis-ease. Neurology 68:99-109, 2007
2. Muenzer J, Wraith J, Beck M, et al: A phase II/III clinical study ofenzyme replacement therapy with idursulfatase in mucopolysacchari-dosis II (Hunter syndrome). Genet Med 8:465-473, 2006
3. Wraith J: Limitations of enzyme replacement therapy: current and fu-ture. J Inherit Metab Dis 29:442-447, 2006
4. Wilcox W: Lysosomal storage disorders: The need for better pediatricrecognition and comprehensive care. J Pediatr 144:S3-S14, 2004
5. Burrow T, Hopkin R, Leslie N, et al: Enzyme reconstitiution/replace-ment therapy for lysosomal storage diseases. Curr Opin Pediatr 18:628-635, 2007
6. Dickson P, McEntee M, Vogler C, et al: Intrathecal enzyme replacementtherapy: Successful treatment of brain disease via the cerebrospinalfluid. Mol Genet Metab 91:61-68, 2007
7. Beutler E: Lysosomal storage diseases: Natural history and ethical andeconomic aspects. Mol Genet Metab 88:208-215, 2006
8. Bernier V, Lagace M, Bichet D, et al: Pharmacological chaperones: Po-tential treatment for conformational diseases. Trends Endocrinol Metab15:222-228, 2004
9. Aerts J, Hollak C, Boot R, et al: Substrate reduction therapy of glyco-sphingolipid storage disorders. J Inherit Metab Dis 29:449-456, 2006
0. Cox T, Aerts J, Adria G, et al: The role of the iminosugar N-bu-tyldeoxynojirimycin (miglustat) in the management of type I (non-neuronopathic) Gaucher disease: a postion statement. J Inherit MetabDis 26:513-526, 2003
1. Patterson MC, Vecchio D, Prady H, et al: Miglustat for treatment ofNiemann-Pick C disease: A randomized control study. Lancet 6:765-772, 2007
2. Jakobkiewicz-Banecka J, Wegrzyn A, Wegrzyn G: Substrate depriva-tion therapy: A new hope for patients suffering from neuronopathicforms of inherited lysosomal storage diseases. J Appl Genet 48:383-388, 2007
3. Dunbar C, Kohn D, Schiffmann R, et al: Retroviral transfer of theglucocerebrosidase gene into CD34� cells from patients with Gaucherdisease: In vitro detection of transduced cells without myeloablation.Hum Gene Ther 9:2629-2640, 1998
4. Raper S, Chimule N, Lee F, et al: Fatal systemic inflammatory responsesyndrome in a ornithine transcarbamylase deficient patient followingadenoviral gene transfer. Mol Genet Metab 80:148-158, 2003
5. Kohn D, Sadelain M, Glorioso J: Occurrence of leukaemia followinggene therapy of X-linked SCID. Nat Rev Cancer 3:477-488, 2003
6. Marsden D, Larson C, Levy H: Newborn screening for metabolic dis-orders. J Pediatr 148:577-584, 2006
7. National Newborn Screening & Genetics Resource Center: 2008. Avail-able at: http://genes-r-us.uthscsa.edu. Accessed August 30, 2008
8. Gelb M, Turecek F, Scot CR, et al: Direct multiplex assay of enzymes indried blood spots by tandem mass spectrometry for the newbornscreening of lysosomal storage disorders. J Inherit Metab Dis 29:397-404, 2006
9. Meikle P, Grasby D, Dean C, et al: Newborn screening for lysosomalstorage disorders. Mol Genet Metab 88:307-314, 2006
0. Fletcher J: Screening for lysosomal storage disorders—A clinical per-spective. J Inherit Metab Dis 29:405-408, 2006
1. Newborn Screening for Krabbe Disease: Available at http://www.
wadsworth.org/newborn/krabbe.htm. Accessed August 30, 2008