Heart Failure Dz
-
Upload
immanuel-jeffri-paian -
Category
Documents
-
view
11 -
download
0
description
Transcript of Heart Failure Dz

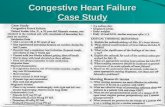
HEART FAILURE
Dr. Dian Zamroni, Sp.JP, FIHA

Definition of heart failure
• Clinical syndrome that can result from any structural or
functional cardiac disorder that impairs the ability of the
ventricle to fill with or eject blood
• A syndrome caused by cardiac dysfunction
- Generally resulting from myocardial muscle dysfunction or loss
- Characteristic by left ventricular dilatation or hypertrophy
- Leading to neurohormonal and circulatory abnormalities and
characteristic symptoms :
- fluid retention
- shortness of breath
- fatique, especially on exertion
AHA / ACC HF guidelines 2001
HFSA guideline 2006

EPIDEMIOLOGY

EPIDEMIOLOGY


Definition of heart failureCriteria 1 and 2 should be fulfilled in all cases
1. Symptoms of heart failure(at rest or during exercise)
And
2. Objective evidence of cardiac
dysfunction(at rest)
And
(in case where the diagnosis is in doubt)
3. Response to treatment directed
towards heart failure

SYMPTOM & SIGN HEART FAILURE

Framingham Criteria for Dx of
Heart Failure• Major Criteria:
– PND
– JVD
– Rales
– Cardiomegaly
– Acute Pulmonary Edema
– S3 Gallop
– Positive hepatic Jugular reflex
– ↑ venous pressure > 16 cm H2O

Dx of Heart Failure (cont.)
• Minor Criteria
LL edema,
Night cough
Dyspnea on exertion
Hepatomegaly
Pleural effusion
↓ vital capacity by 1/3 of normal
Tachycardia 120 bpm
Weight loss 4.5 kg over 5 days management

DIAGNOSTIC• Suspected Heart Failure because of
SYMPTOMS and/or SIGNS
Assess presence of CARDIAC DISEASE
by ECG, X-Ray or BNP (if available)
VENTRICULAR FUNCTION Imaging by ECHO-Doppler,
Nuclear angiography or MRI if available
Heart Failure: Systolic / DiastolicIdentify etiology, evaluate severity, choose therapy
ESC HF guidelines 2001
Tests abnormal
Tests abnormal
NORMAL
No Heart Failure
NORMAL
No Heart Failure

Heart Failure
• What Causes Heart Failure?
– Coronary artery disease
• Cholesterol and fatty deposits build up in
the heart’s arteries
• Less blood and oxygen reach the heart
muscle
• This causes the heart to work harder and
occasionally damages the heart muscle

Heart Failure
• What Causes Heart Failure?
– Heart attack
• An artery supplying blood to the heart
becomes blocked
• Loss of oxygen and nutrients damages
heart muscle tissue causing it to die
• Remaining healthy heart muscle must pump
harder to keep up

Heart Failure
• What Causes Heart Failure?– High blood pressure
• Uncontrolled high blood pressure doubles a
persons risk of developing heart failure
• Heart must pump harder to keep blood
circulating
• Over time, chamber first thickens, then gets
larger and weaker

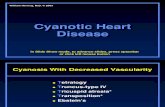
Heart Failure
• What Causes Heart Failure?– Abnormal heart valves
– Heart muscle disease
• Damage to heart muscle due to drugs,
alcohol or infections
– Congenital heart disease
– Severe lung disease

Heart Failure
• What Causes Heart Failure?– Diabetes
• Tend to have other conditions that make the
heart work harder
• Obesity
• Hypertension
• High cholesterol

Heart Failure
• What Causes Heart Failure?– Severe anemia
• Not enough red blood cells to carry oxygen
• Heart beats faster and can become overtaxed with
the effort
– Hyperthyroidism
• Body metabolism is increased and overworks the
heart
– Abnormal Heart Rhythm
• If the heart beats too fast, too slow or irregular it may
not be able to pump enough blood to the body

Signs and Symptoms of
Heart Failure
Shortness of Breath (dyspnea)
• WHY?
– Blood “backs up” in the pulmonary
veins because the heart can’t keep up
with the supply an fluid leaks into the
lungs
• SYMPTOMS
– Dyspnea on exertion or at rest
– Difficulty breathing when lying flat
– Waking up short of breath

Persistent Cough or Wheezing
• WHY?
– Fluid “backs up” in the lungs
• SYMPTOMS
– Coughing that produces white or pink blood-tinged
sputum
Signs and Symptoms of
Heart Failure

– Edema
• WHY?
– Decreased blood flow out of the weak heart
– Blood returning to the heart from the veins
“backs up” causing fluid to build up in tissues
• SYMPTOMS
– Swelling in feet, ankles, legs or abdomen
– Weight gain
Signs and Symptoms of
Heart Failure

– Tiredness, fatigue
• WHY?
– Heart can’t pump enough blood to meet needs of
bodies tissues
– Body diverts blood away from less vital organs
(muscles in limbs) and sends it to the heart and
brain
• SYMPTOMS
– Constant tired feeling
– Difficulty with everyday activities
Signs and Symptoms of
Heart Failure

– Lack of appetite/ Nausea
• WHY?
– The digestive system receives less blood
causing problems with digestion
• SYMPTOMS
– Feeling of being full or sick to your stomach
Signs and Symptoms of
Heart Failure

– Increased heart rate
• WHY?
– The heart beats faster to “make up for” the loss
in pumping function
• SYMPTOMS
– Heart palpitations
– May feel like the heart is racing or throbbing
Signs and Symptoms of
Heart Failure

Heart Failure
• New York Heart Association (NYHA)
Functional Classification
Class % of
patients
Symptoms
I 35% No symptoms or limitations in ordinary physical
activity
II 35% Mild symptoms and slight limitation during
ordinary activity
III 25% Marked limitation in activity even during minimal
activity. Comfortable only at rest
IV 5% Severe limitation. Experiences symptoms even at
rest

Treatment Objectives
Survival
Morbidity
Exercise capacity
Quality of life
Neurohormonal changes
Progression of CHF
Symptoms

Heart Failure
• Treatment Options
– The more common forms of heart failure
cannot be cured, but can be treated
• Lifestyle changes
• Medications
• Surgery

Heart Failure
Management
• Lifestyle changes
– Stop smoking
– Loose weight
– Avoid alcohol
– Avoid or limit caffeine
– Eat a low-fat, low-sodium diet
– Exercise

Heart Failure
• Lifestyle changes
– Reduce stress
– Keep track of symptoms and weight and
report any changes or concern to the
doctor
– Limit fluid intake
– See the doctor more frequently

Physiology - Treatment

Treatment
Pharmacologic Therapy
•ACE inhibitors
•Diuretics
•Beta Blockers• Digitalis
• Spironolactone
• Other

Heart Failure
• Medications used to treat Heart
Failure
– ACE Inhibitors
• Cornerstone of heart failure therapy
• Proven to slow the progression of heart
failure
• Vasodilator – cause blood vessels to
expand lowering blood pressure and the
hearts work load

VASOCONSTRICTION VASODILATATION
Kininogen
Kallikrein
Inactive Fragments
Angiotensinogen
Angiotensin I
RENIN
Kininase IIInhibitor
ALDOSTERONE
SYMPATHETIC
VASOPRESSIN
PROSTAGLANDINS
tPA
ANGIOTENSIN II
BRADYKININ
ACE-i. Mechanism of Action
A.C.E.

ACE-I. Clinical Effects
• Improve symptoms
• Reduce remodelling / progression
• Reduce hospitalization
• Improve survival

• Symptomatic heart failure
• Asymptomatic ventricular dysfunction
- LVEF < 35 - 40 %
• Selected high risk subgroups
ACE-i. Indications
AHA / ACC HF guidelines 2001
ESC HF guidelines 2001

ACE-i. Practical Use
•Start with very low dose
• Increase dose if well tolerated
•Renal function & serum K+ after 1-2 w
•Avoid fluid retention / hypovolemia (diuretic use)
•Dose NOT determined by symptoms
•Combine to overcome “resistance”
•Do not use alone


ACE-I. Adverse Effects
• Hypotension (1st dose effect)
• Worsening renal function
• Hyperkalemia
• Cough
• Angioedema
• Rash, ageusia, neutropenia, …

ACE-I. Contraindications
• Intolerance (angioedema, anuric renal fail.)
• Bilateral renal artery stenosis
• Pregnancy
• Renal insufficiency (creatinine > 3 mg/dl)
• Hyperkalemia (> 5,5 mmol/l)
• Severe hypotension

RENIN
Angiotensinogen Angiotensin I
ANGIOTENSIN II
ACE
Other pathways
Vasoconstriction Proliferative
Action
Vasodilatation Antiproliferative
Action
AT1 AT2
AT1
Receptor
BlockersRECEPTORS
Angiotensin II Receptor Blockers (ARB)

•Candesartan, Eprosartan, Irbesartan
Losartan, Telmisartan, Valsartan
•Efficacy not equal / superior to ACE-I
•Not indicated with beta blockers
• Indicated in patients intolerant to ACE-I
Angiotensin II Receptor Blockers (ARB)
AHA / ACC HF guidelines 2001
ESC HF guidelines 2001

Diuretics
• Essential to control symptomssecondary to fluid retention
• Prevent progression from HT to HF
• Spironolactone improves survival
• New research in progress

Cortex
Medulla
Thiazides
Inhibit active exchange of Cl-Na
in the cortical diluting segment of the
ascending loop of Henle
K-sparing
Inhibit reabsorption of Na in thedistal convoluted and collecting tubule
Loop diuretics
Inhibit exchange of Cl-Na-K inthe thick segment of the ascending
loop of Henle
Loop of HenleCollecting tubule
Diuretics

Diuretics. Indications
1.Symptomatic HF, with fluid retention
• Edema
• Dyspnea
• Lung Rales
• Jugular distension
• Hepatomegaly
• Pulmonary edema (Xray)
AHA / ACC HF guidelines 2001
ESC HF guidelines 2001

Loop Diuretics / Thiazides. Practical Use
•Start with variable dose. Titrate to achieve dry weight
•Monitor serum K+ at “frequent intervals”
•Reduce dose when fluid retention is controlled
•Teach the patient when, how to change dose
•Combine to overcome “resistance”
•Do not use alone

Loop diuretics. Dose (mg)
Initial Maximum
Bumetanide 0.5 to 1.0 / 12-24h 10 / day
Furosemide 20 to 40 / 12-24h 400 / day
Torsemide 10 to 20 / 12-24h 200 / day
AHA / ACC HF guidelines 2001

Thiazides, Loop Diuretics. Adverse Effects
• K+, Mg+ (15 - 60%) (sudden death ???)
• Na+
• Stimulation of neurohormonal activity
• Hyperuricemia (15 - 40%)
• Hypotension. Ototoxicity. Gastrointestinal.
Alkalosis. Metabolic
Sharpe N. Heart failure. Martin Dunitz 2000;43
Kubo SH , et al. Am J Cardiol 1987;60:1322
MRFIT, JAMA 1982;248:1465
Pool Wilson. Heart failure. Churchill Livinston 1997;635

ß-Adrenergic BlockersMechanism of action
• Density of ß1 receptors
• Inhibit cardiotoxicity of catecholamines
• Neurohormonal activation
• HR
•Antiischemic
•Antihypertensive
•Antiarrhythmic
•Antioxidant, Antiproliferative

ß-Adrenergic BlockersClinical Effects
• Improve symptoms (only long term)
• Reduce remodelling / progression
• Reduce hospitalization
• Reduce sudden death
• Improve survival

• Symptomatic heart failure
• Asymptomatic ventricular dysfunction
- LVEF < 35 - 40 %
• After AMI
AHA / ACC HF guidelines 2001
ESC HF guidelines 2001
ß-Adrenergic BlockersIndications

•Patient stable
• No physical evidence of fluid retention
• No need for i.v. inotropic drugs
•Start ACE-I / diuretic first
•No contraindications
• In hospital or not
ß-Adrenergic BlockersWhen to start

Initial Target
Bisoprolol 1.25 / 24h 10 / 24h
Carvedilol 3.125 / 12h 25 / 12h
Metoprolol tartrate 6.25 / 12h 75 / 12h
Metoprolol succinnate 12,5-25 / 24h 200 / 24h
• Start Low, Increase Slowly• Increase the dose every 2 - 4 weeks
ß-Adrenergic BlockersDose (mg)

•Hypotension
•Fluid retention / worsening heart failure
•Fatigue
•Bradycardia / heart block
ß-Adrenergic BlockersAdverse Effects
•Review treatment (+/-diuretics, other drugs)
•Reduce dose
•Consider cardiac pacing
•Discontinue beta blocker only in severe cases

ß-Adrenergic Blockers
Contraindications
•Asthma (reactive airway disease)
•AV block (unless pacemaker)
•Symptomatic hypotension / Bradycardia
•Diabetes is NOT a contraindication

ALDOSTERONE
• Retention Na+
• Retention H2O
• Excretion K+
• Excretion Mg2+
• Collagen
deposition
Fibrosis- myocardium
- vessels
Spironolactone
Edema
Arrhythmias
Competitive antagonist of the
aldosterone receptor
(myocardium, arterial walls, kidney)
Aldosterone Inhibitors
-

Spironolactone. Indications
• Recent or current symptoms despite
ACE-i, diuretics, dig. and b-blockersAHA / ACC HF guidelines 2001
• Recommended in advanced heart failure
(III-IV), in addition to ACE-i and diuretics
• HypokalemiaESC HF guidelines 2001

Spironolactone. Practical use
• Do not use if hyperkalemia, renal insuf.
• Monitor serum K+ at “frequent intervals”
• Start ACE-i first
• Start with 25 mg / 24h
• If K+ >5.5 mmol/L, reduce to 25 mg / 48h
• If K+ is low or stable consider 50 mg / day

Digitalis. Mechanism of Action
Blocks Na+ / K+ ATPase => Ca+ +
• Inotropic effect
• Natriuresis
• Neurohormonal control- Plasma Noradrenaline
- Peripheral nervous system activity
- RAAS activity
- Vagal tone
- Normalizes arterial baroreceptors
NEJM 1988;318:358

Digitalis. Clinical Effects
• Improve symptoms
• Modest reduction in hospitalization
• Does not improve survival

Digitalis. Indications
• When no adequate response to
ACE-i + diuretics + beta-blockers
AHA / ACC Guidelines 2001
• In combination with ACE-i + diuretics
if persisting symptoms
ESC Guidelines 2001
• AF, to slow AV conduction
Dose 0.125 to 0.250 mg / day

• Digoxin toxicity
• Advanced A-V block without pacemaker
• Bradycardia or sick sinus without PM
• PVC’s and VT
• Marked hypokalemia
• W-P-W with atrial fibrillation
Digoxin. Contraindications

Other Drugs. (only in selected patients)
• Inotropics: refractory HF
• Nitrates: ischemia, angina, pulmonary congestion
• ARB: Contraindications to ACE-i
• Antiarrhythmics: (only amiodarone) H risk arrhyth.
• Anticoagulants: High risk of embolysm
• Ca channel blockers: (only amlodipine) ischemia

Heart Failure
• Treatment options– Surgery and other Medical Procedures
• Not often used in heart failure unless there
is a correctable problem
• Coronary artery bypass
• Angioplasty
• Valve replacement
• Defibrillator implantation
• Heart transplantation
• Left ventricular assist device (LVAD)

“The very essence of cardiovascular practice is
the early detection of heart failure”
Sir Thomas Lewis, 1933