Health-Literacy Adapted CBT and Pain Education for Low-SES...
Transcript of Health-Literacy Adapted CBT and Pain Education for Low-SES...

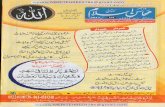
Figure 1. Three graphs showing the change in outcome scores (for BPI-Intensity, BPI-Interference, and Pain Catastrophizing) across the course of the study. * = indicates significant pre–post difference across groups (p < .05) † = significant adjusted between-group difference (ANCOVA) at p < .05.
Health-Literacy–Adapted CBT and Pain Education for Low-SES Individuals
with Chronic Pain: One-Year Follow-up Joshua C. Eyer, Ph.D.,1 Beverly E. Thorn, Ph.D., ABPP;1 & Melissa A. Day, M.A.1,2
1. The University of Alabama; 2. The University of Washington
Select References
Institute of Medicine [IOM]. (2011). Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press.
Thorn, B. E., et al. (2011). Randomized trial of group cognitive behavioral therapy compared with a pain education control for low-literacy rural people with chronic pain. Pain. doi:10.1016/j.pain.2011.07.007
Turk, D. C. (2002). Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clinical Journal of Pain, 18, 355–365.
Method Participants: • 45 individuals with chronic pain, receiving treatment from a federally
qualified (low-income) health center in rural western Alabama • 82% male, 13%white/87% black, aged 56.5 years (SD = 12.4) • 87% at or below poverty threshold • Mean WRAT standard score = 83.4 (SD = 14.9)
Measures: • Brief Pain Inventory–Short Form (BPI) — a validated measure of Pain Intensity
(Range: 0–10) and Pain Interference (range: 0–10). Higher scores = greater dysfunction.
• Pain Catastrophizing Scale (PCS) — a widely used, validated measure of
dysfunction thinking about pain (range: 0–52). Higher scores = greater negative thinking.
• Depression: Center for Epidemiological Studies, Depression (CES-D) — a rigorously validated measure of depressive symptoms (range: 0–60). Greater scores = more depressive symptoms. Cutoff of 27 for clinical depression in chronic pain patients.
• Quality of Life Scale (QLS) — a measure of Quality of Life validated with chronic pain
patients (range: 7-49). Greater scores = more satisfaction with life.
Results • At 12 months, patients endorsed: clinically significant pain (Intensity > 4); moderate life interference (Interference > 4); mostly moderate depression scores (only 8 tested into the clinical range); and moderate–good Quality of Life. (See Table 1 & Figure 1.)
• 12 months compared to pretest: significant decreases in Pain Intensity, Pain Interference, and Pain Catastrophizing (but not for depressive symptoms or quality of life). (See Table 1 & Figure 1.)
• Between-group comparisons: the only significant effect was a greater improvement in PCS scores at 12 months for CBT compared to EDU.
• Follow-up Comparisons: improvement in PCS scores due to treatment with CBT (change at posttest) significantly predicted improvements in pain catastrophizing, depression symptoms, and quality of life at 12 month follow-up. (See Figure 2.)
Discussion
• Results indicated that both treatment were helpful in reducing pain for participants on average.
• Pain relief was modest but clinically meaningful for both groups and resulted in small improvements in pain disruption to daily activities.
• Neither intervention produced broad changes to depressive symptoms or quality of life.
• However, the CBT intervention did result in greater change to PCS scores. Improvement in PCS scores in CBT led to significant improvements in long-term pain catastrophizing, depression symptoms, and quality of life.
• LIMITATIONS: This sample may not be representative of average pain patients as it (a) is limited to only those available at follow-up, and (b) excludes 7 participants with clinically severe depression likely to disrupt pain treatment (CES-D score ≥ 39).
• STRENGTHS: This study represents a strong first step towards the adaptation of cognitive therapy for chronic pain to low-income, multiple disadvantaged people groups. By using an active comparator (EDU), it was able to identify the benefits of simple pain education, in addition to the added benefits of CBT.
CONCLUSION: Results indicate that health-literacy–adapted CBT and Pain Education can both produce important changes in pain experience for individuals with chronic pain and low socioeconomic standing. Furthermore, CBT appears to produce changes in the way patients think about their pain that may lead to long-term benefits.
Acknowledgements — The authors would like to thank the staff and patients of Pine Apple Health Center and the graduate and undergraduate research assistants of the UA Pain Management Team.
For Further Information — For additional information, contact the lead investigator, Dr. Beverly Thorn, at [email protected].
Introduction • 1/3 of Americans (116 million) have chronic pain (IOM, 2011).
• Chronic pain conditions include back pain, arthritis, migraines, fibromyalgia, and diabetes-related pain, among many others.
• Medical treatments for pain are expensive and invasive (Turk, 2002).
• Cognitive-behavioral therapy for chronic pain (CBT) is as effective and cheaper, with fewer side effects (Thorn et al., 2011; Turk, 2002).
• Groups with low SES, such as rural minorities, have a greater risk for chronic pain conditions and greater risk for poor outcomes to pain treatment (IOM).
• Low health literacy is n important factor underlying risks (IOM).
• Treatment and health education materials are difficult for patients to understand.
• Psychosocial treatments are poorly adapted for individuals with low health literacy (IOM).
This poster reports outcomes at 12 months for a randomized,
controlled trial of a health-literacy–adapted cognitive-behavioral pain therapy (CBT) versus a similarly adapted pain-education control.
0
1
2
3
4
5
6
7
8
9
10
Pre Post 6 mos 12 mos
BP
I In
ten
sity
Sco
re (
Me
an)
CBT
EDU
* * * (NS)
0
1
2
3
4
5
6
7
8
9
10
Pre Post 6 mos 12 mos
BP
I In
ten
sity
Sco
re (
Me
an)
CBT
EDU
* * *
(NS)
0
5
10
15
20
25
30
35
40
45
50
Pre Post 6 mos 12 mos
Pai
n C
atas
tro
ph
izin
g Sc
ore
(M
ean
)
CBT
EDU
(NS) * * (NS) (NS)
†
(NS)
Assessment Period
Figure 2. Three graphs showing the regression lines for each condition (unstandardized betas in parentheses). For the CBT condition but not the EDU condition (both in the first graph), the change in PCS scores from pretest to posttest significantly predicted change in Pain Catastrophizing (PCS), depression (CES-D), and quality of life (QLS) by 12 months after treatment. [CBT M = * = indicates significant beta coefficient (p < .05)
PCS Difference Scores, Posttest – Pretest (Centered)
Dec
reas
ing
Path
olo
gy
Dec
reas
ing
Path
olo
gy
Dec
reas
ing
Path
olo
gy
Decreasing Pathology Decreasing Pathology Decreasing Pathology
(.75)* (.44)* (.14)
(-.19)*
(.35)* (-.10)
Pain Intensity
Pain Interference
Pain Catastrophizing
Table 1. Descriptive statistics at 12 months for total sample (N = 45).
Variable
Pre-test M
Pre-test SD
12 mos.
M
12 mos. SD F df p ηp
2
BPI Intensity 5.89 2.27 4.79 1.99 16.69 1, 44 .000 .275
BPI Interference 5.42 2.50 4.25 2.38 11.96 1, 44 .001 .214
PCS 27.16 16.40 20.30 14.15 13.07 1, 44 .001 .229
CES-D 15.38 10.24 14.94 8.35 0.07 1, 44 .787 .002
QLS 32.98 9.64 34.02 8.36 1.16 1, 44 .287 .026