Gut 1999 Van Erpecum 435 8
Transcript of Gut 1999 Van Erpecum 435 8
-
8/11/2019 Gut 1999 Van Erpecum 435 8
1/5
Review
Gallstones: an intestinal disease?
During the first half of this century, cholelithiasis was
regarded as a disease of the gall bladder, with inflammationof the wall as the primary defect and exfoliated cells as thesource of biliary cholesterol.1 2 During the 1960s, Smalland Rapo elucidated the physicalchemical basis of biliarycholesterol supersaturation and demonstrated that exces-sive hepatic cholesterol secretion is the underlying defect.3
Cholesterol gallstones were then considered to be the con-sequence of a metabolic defect of the liver. The importanceof the gall bladder during gallstone formation wasresurrected during the 1980s, when impaired gall bladderemptying was identified as a factor contributing togallstone formation.4 5 During the past 10 years, a thirdorgan has been proposed as an important player in gallsto-ne pathogenesisthe intestine. Several recent observationsindicate slow intestinal transit in gallstone patients andanimal models. Impaired intestinal transit might promotegallstone formation by increasing the amounts of thehydrophobic bile salt deoxycholate or by other mecha-nisms. In this review, we shall evaluate critically the prosand cons of the intestinal hypothesis.
Cholesterol supersaturation and crystal formationCholesterol is a relatively insoluble amphiphile. Its solubil-ity in water is only 20 109 M, but in gall bladder bile,20 103 M of the sterol can be kept in solution.6 Thismillionfold increase in solubility is explained by incorpora-tion of cholesterol into micelles, together with bile salts andphospholipids (mainly phosphatidylcholine). Whereascholesterol is soluble only to a limited extent in micellesthat contain exclusively bile salts (simple micelles),addition of phosphatidylcholine leads to strongly enhanced
solubility in mixed micelles, provided that this phos-pholipid contains unsaturated acyl chains at the sn-2position.7 Supersaturation occurs when either too muchcholesterol or not enough bile salts and phosphatidylcho-line are secreted to allow complete micellar solubilisationof all cholesterol in bile. Current thought is that increasedbiliary cholesterol secretion rather than decreased bile saltor phospholipid secretion is the primary cause of biliarycholesterol supersaturation.8 Excessive cholesterol may besolubilised in vesicles (spherical bilayers of cholesterol andphospholipids, without bile salts). As these vesicles areoften cholesterol-rich, they maypossibly after aggrega-tion and fusionnucleate cholesterol crystals, an essentialstep in gallstone formation.9 10 A large number of proteinsare secreted in bile, among them apolipoproteins A1 and
A2, anionic polypeptide fraction, aminopeptidase N,
1acid glycoprotein, mucin, haptoglobin, immune globulins,phospholipases A2 and C, and others. Based on in vitrostudies, several of these proteins may either promote orinhibit crystallisation by stabilising or destabilisingcholesterol-rich vesicles.
Postprandial gall bladder motilityIngestion of a meal induces considerable gall bladderemptying, up to 7080% of fasting gall bladder volume, byreleasing the hormone cholecystokinin (CCK) from theduodenal wall. Apart from biliary cholesterol supersatura-tion and proteins, gall bladder motility may also influencegallstone formation. The basic concept is relatively simple:
impaired gall bladder emptying prolongs residence of bile in
the gall bladder, thus allowing more time for nucleation ofcholesterol crystals from supersaturated bile. Furthermore,in the case of adequate gall bladder emptying, cholesterolcrystals that have nucleated are ejected to the duodenum,whereas in the case of impaired gall bladder emptying, thesecrystals aggregate into macroscopic gallstones. Indeed, stud-ies in patients with gallstones by either scintigraphic orultrasonographic methods have identified a subgroup withimpaired emptying, as defined by a low percentage decreasein fasting volumes or low amounts of ejected bile after con-sumption of a meal.4 Even in patients with normal gall blad-der emptying according to these criteria, there are oftenincreased fasting and residual gall bladder volumes, despitenormal amounts of bile ejected after feeding.11 12 Tradition-ally, it has been assumed that after a meal, the gall bladderempties in a steady, progressive fashion and that gall bladderrefill occurs only in the fasting state, between meals. Thisassumption has been challenged by studies using combinedduodenal perfusion and scintigraphy13 or minute by minuteultrasound14: there seems to be very frequent, short periodsof gall bladder emtying and refilling (bellow concept), thebalance between them determining whether net emptyingsuch as in the immediate postprandial periodor net refill-ing occurs. One should realise that, strictly speaking,ultrasound measures only gall bladder volumes (which areinfluenced by refilling), and HIDA scintigraphy measuresthe reduction in total gall bladder isotope counts (which areindependent of refilling). Jazrawi and colleagues15 recentlyintroduced a method of combined scintigraphy andultrasound that enables simultaneous, accurate quantitationof gall bladder emptying and refilling, as well as bile turno-
ver. Interestingly, postprandial gall bladder emptying, refill-ing and bile turnover were all strongly depressed in patientswith gallstones, thus suggesting a reduced postprandialwashout eVect. Nevertheless, one may argue that abnormalgall bladder motility in these patients could be secondary tothe presence of stones or supersaturated bile in the gall blad-der, with no relevance for gallstone formation. Indeed, stud-ies in gallstone forming animal models have shown that, afterits absorption by the gall bladder wall from supersaturatedbile, excess cholesterol is incorporated within the sarcolem-nal plasma membrane of the gall bladder muscle cell, withdecreased membrane fluidity, impaired contractility andimpaired relaxation as a result.1618 Although impaired motil-ity could be in many cases secondary to biliary cholesterolsupersaturation, it may still facilitate the process of gallstoneformation: in the prairie dog model19 and in humans,20
impaired gall bladder motility occurs in the earliest stage ofgallstone formation, before stones have formed. Gall bladdermotility is also often impaired in many high risk situations forgallstone formation, such as pregnancy, obesity, diabetesmellitus, treatment with the somatostatin analogue octre-otide, very low calory diets, and total parenteral nutrition.Prospective studies indicate that impaired gall bladdermotility is also an independent risk factor for gallstonerecurrence after extracorporeal shockwave lithotripsy.21
Daily CCK injection during total parenteral nutrition22 or
Abbreviations used in this paper: CCK, cholecystokinin; MMC,
migrating motor complex.
Gut1999;44:435438 435
group.bmj.comon September 12, 2014 - Published bygut.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://gut.bmj.com/http://gut.bmj.com/http://group.bmj.com/http://gut.bmj.com/ -
8/11/2019 Gut 1999 Van Erpecum 435 8
2/5
inclusion of small amounts of fat in the diet during rapidweight loss23 restore normal gall bladder motility and avoidthe risk of gallstone formation. All these data suggest a role
for gall bladder motility in gallstone formation.
The intestine: its relation to bile composition and gallbladder motility in the fasting (interdigestive) stateRecent data indicate that, along with the liver and the gallbladder, the intestine might also be involved in gallstoneformation. The gall bladder and the small intestine deter-mine enterohepatic cycling of bile salts and their fluxthrough the liver. In patients with gallstones, both smallintestinal24 and whole gut25 transit times are prolonged.What explanations could be oVered for the associationbetween prolonged intestinal transit and gallstone disease?One should remember one potential caveat: gallstones arerather frequent in the western world and the symptomsoften attributed to them, such as right upper quadrant
painwith or without radiation to the backor nausea,are not specific to gallstones.26 These symptoms can also becaused by constipation as they often disappear uponchanges in diet or pharmacological intervention. Aspecificabdominal symptoms may have led to ultrasonographicdetection of gallstones and clinicians with special interestin gallstone research may have measured intestinal transitand included these patients in their case-control studies.Nevertheless, one study explicitly states that patients wereunaware of the presence of stones.25 One could alsohypothesise that impaired intestinal motility is somehowcausally related to gallstone formation. Indeed, the hydro-phobic bile salt deoxycholate could be the link betweenimpaired intestinal motility and lithogenic bile. The mainbile salts in humans are cholate and chenodeoxycholate,
both primary bile salts synthesised from cholesterol inthe liver, and the secondary bile salt deoxycholateformed in the distal small intestine and colon by bacterial7-dehydroxylation of cholate. Deoxycholate is partlyabsorbed from the intestinal lumen and joins the enterohe-patic circulation of bile salts after taurine or glycine conju-gation in the liver. Prolonged intestinal transit timeprobably enhances formation of deoxycholate by increas-ing the intestinal residence time of bile salts, whereasdecreasing intestinal transit time may have the oppositeeVect. As a result amounts of deoxycholate vary consider-ably in humans, between 10 and 30% of the total bile saltpool. Preliminary data from Dowling and coworkers27 haverevealed that patients with gallstones have increased
amounts of Gram positive anaerobic bacteria and in-creased 7-dehydroxylating activity in their caecumcompared with controls. In these patients, slowness ofcolonic transit correlates with increased caecal pH andwater solubility of deoxycholate (factors promoting intesti-nal absorption of the bile salt). What eVects do increasedamounts of biliary deoxycholate in bile have on lithogenic-ity? Several studies in patients with gallstones have found apositive correlation between the amount of biliarydeoxycholate on the one hand and the cholesterol
saturation index24 28 or the speed of cholesterolcrystallisation28 on the other. In acromegalics, octreotidetreatment induces a similar combination of increasedintestinal transit times, more biliary deoxycholate, in-creased biliary cholesterol saturation index and fastcrystallisation.29 30 In contrast, treatment with ampicillinleads to decreased faecal 7-dehydroxylation activity,decreased amounts of biliary deoxycholate and a lower bil-iary cholesterol saturation index.31 In the ground squirrel32
and in the C57L inbred mouse,33 a cholesterol-rich dietinduces a significant increase in the proportion of biliarydeoxycholate, cholesterol supersaturation and gallstoneformation. Furthermore, in the ground squirrel model,small intestinal transit is prolonged.32 Thus, data frompatients with gallstones and acromegalics on octreotide as
well as animal models suggest an association between slowintestinal transit, high deoxycholate, cholesterol supersatu-ration and gallstone formation. One should realise,however, that this association is not universal: in humanson oral contraceptives (another risk factor for gallstoneformation), cholesterol supersaturation and slow intestinaltransit are associated with a decreased rather thanincreased deoxycholic acid pool size.34 Furthermore, inboth the ground squirrel and the C57L inbred mousemodels on lithogenic diets, there is an increased pro-portion, not only of biliary deoxycholate, but also of theprimary bile salt chenodeoxycholate. This might beexplained by negative feedback suppression through thehydrophobic deoxycholate on hepatic cholesterol 7-hydroxylase (the rate controlling enzyme in the classicpathway of bile salt synthesis) and a higher contribution to
bile salt synthesis of the alternative or acidic pathwaythrough the mitochondrial enzyme sterol 27-hydroxylaseas the alternative pathway has a preference for chenodeoxy-cholate over cholate synthesis.35 36
Increased deoxycholate could promote lithogenic bileand gallstone formation through several mechanisms.Firstly, deoxycholate itself can slow down intestinaltransit,37 thereby allowing more time for intestinalcholesterol absorption and exerting a positive feedback onits own formation. The mechanism for this eVect is notentirely clear: although in in vitro studies, bile salts seem toexert a depressant eVect on intestinal muscle contractility,38
increased maximal contractile responses of intestinalcircular and longitudinal smooth muscle strips on bethan-echol stimulation have been reported in ground squirrels
on a lithogenic diet, associated with slow small intestinaltransit and biliary deoxycholate enrichment.32 Moredeoxycholate could theoretically also increase intestinalcholesterol absorption by means of enhanced micellarsolubilisation of the sterol. This eVect, however, is probablymore relevant in animal models with rather hydrophilicendogenous bile salts32 33 than in humans with a relativelyhydrophobic endogenous bile salt pool. Secondly, deoxy-cholate could enhance biliary cholesterol secretion by aneVect on the hepatocytic canalicular membrane. The outerleaflet of the membrane contains large amounts of choles-terol and the phospholipid sphingomyelin (associated inlaterally separated domains), which confers resistance tothe detergent action of bile salts by decreasing membrane
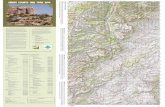
Figure 1 The intestinal migrating motor complex occurs periodically(12 hour cycle) during the fasting state and is characterised by three
phases: contractile activity is absent during phase I; irregular activityoccurs during phase II; and there are intense, regular coordinatedcontractions during phase III. Significant periodic gall bladder contractionoccurs before phase III and is associated with a rise in plasma motilinconcentrations.
436 van Erpecum, van Berge-Henegouwen
group.bmj.comon September 12, 2014 - Published bygut.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://gut.bmj.com/http://gut.bmj.com/http://group.bmj.com/http://gut.bmj.com/ -
8/11/2019 Gut 1999 Van Erpecum 435 8
3/5
fluidity. Particularly hydrophobic bile salts such asdeoxycholate can release cholesterol from the sphingomy-elin domains (most likely by decreasing the activationenergy necessary for desorption of the sterol from themembrane), thus allowing its secretion into bile.7 Thirdly,in vitro studies have revealed that deoxycholate enhancesbiliary cholesterol crystallisation by destabilising choleste-rol-rich vesicles.39 This eVect (paradoxical if one wouldonly consider the enhanced micellar cholesterol solubilisa-tion in deoxycholate-rich biles) can be nicely explained by
the elegant model studies performed by Wang and Carey40:deoxycholate leads to a rightward shift in the ternary(cholesterol-phospholipid-bile salt) phase diagram, withinherent faster cholesterol crystallisation.
Apart from the eVects on biliary deoxycholate another,possibly complementary, link between the intestine and gall-stone formation could be the relation between intestinal andgall bladder motility in the fasting (also called interdiges-tive) state. As fig 1 shows, significant periodic gall bladderemptying occurs during this period (2030% emptying inthe fasting state compared with 7080% emptying after ameal) at one to two hour intervals, associated with the cycleof the intestinal migrating motor complex (MMC) and witha rise in plasma motilin concentrations.41 42 The MMC, apattern of cyclic contractile activity displayed in the fasting
state by the upper intestinal tract, is characterised by threephases: during phase I, contractile activity is absent; irregu-lar activity occurs during phase II; and during phase III thereare intense, regular coordinated contractions. In healthypeople, significant gall bladder emptying and high plasmamotilin concentrations are observed before phase III.4244 Wefound that patients with gallstones have less frequent MMCcycles, absent interdigestive gall bladder emptying and analtered pattern of motilin release compared with controls. 45
A similarly prolonged MMC cycle has been found in theground squirrel model of gallstone formation.46 The fastingstate, namely the night, would seem to be the mostvulnerable period for gallstone formation. During thisperiod, biliary cholesterol saturation is highest as a result ofrelatively low bile salt secretion and relatively high choles-terol secretion. There is also a progressive concentration of
gall bladder bile during this period, which is partially coun-teracted by periodic interdigestive gall bladder contractionsin association with phase III of the MMC.47 Bile concentra-tion has important consequences: it leads to higher micellarcholesterol (and phospholipid) solubilisation by increasingthe micellar phase boundary.40 As phospholipids are muchmore easily solubilised in micelles than cholesterol, there is amuch larger shift of phospholipid than cholesterol from vesi-cles to micelles. The remaining vesicles should therefore beenriched in cholesterol and prone to nucleate cholesterolcrystals.48 49 According to this concept, the reduced fre-quency of phase III and absent interdigestive gall bladdercontractility, as found in our patients with gallstones, couldpromote bile concentration, crystallisation and gallstone for-mation. During the earliest stages of gallstone formation in
the prairie dog model there is also excessive concentration ofbile within the gall bladder50 and prevention of excessive bileconcentration with the aid of the drug amiloride preventsgallstone formation.51 Interestingly, cholesterol absorptionby the gall bladder wall seems to function as a protectivemechanism against cholesterol crystallisation under thesecircumstances, because it leads to a lower biliary cholesterolsaturation. Using the isolated pig gall bladder model,Corradini and colleagues52 have confirmed earlier reports53 54
that significant cholesterol absorption as well as some phos-pholipid absorption occurs from supersaturated biles. Incontrast, there is virtually no bile salt absorption. Thisdefence mechanism may be operating particularly in the caseof impaired gall bladder emptying.55 Based on indirect
evidence (comparison of protein concentrations in hepaticand associated gall bladder biles), Groen and coworkers56
have postulated a similar absorption of pronucleatingproteins by the gall bladder wall as an additional defence
mechanism against crystallisation.
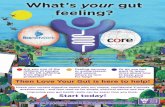
SummaryCurrent evidence suggests that impaired intestinal motilitymay facilitate gallstone formation by influencing biliarydeoxycholate levels or by modulating interdigestive gallbladder motility (fig 2), although a primary intestinaldefect in gallstone pathogenesis has not yet beendemonstrated. In the cold war period, most interestingevents, from a political point of view, occurred at the bor-der between capitalist and communist systems, near theiron curtain. Similarly, the gall bladder and biliary tract canbe viewed as the border between liver and intestinal tract,where many interesting things occur with profound impacton both systems. Combined eVorts by researchers in thefield of hepatology and gastrointestinal motility shouldbrake down the Berlin wall of ignorance of one of the mostcommon diseases in the Western world.
K J VAN ERPECUMG P VAN BERGE-HENEGOUWEN
Department of Gastroenterology,
University Hospital Utrecht,
Postbox 85500,
3508GA Utrecht,
The Netherlands
Correspondence to: Dr van Erpecum.
1 Naunyn B.A treatise on cholelithiasis.New Syndenham Society, 1896.2 ShaVer EA. Abnormalities in gall bladder function in cholesterol gallstone
disease: bile and blood, mucosa and musclethe list lengthens.Gastroenterology1992;102:180812.
3 Small DM, Rapo S. The source of abnormal bile in patients with cholesterolgallstones. N Engl J Med1970;283:537.
4 Pomeranz IS, ShaVer EA. Abnormal gall bladder emptying in a subgroup ofpatients with gallstones.Gastroenterology 1985;88:78791.
5 Forgacs IC, Maisley MN, Murphy GM,et al. Influence of gallstones andursodeoxycholic acid therapy on gall bladder emptying. Gastroenterology1984;87:299307.
6 Cabral DJ, Small DM. Physical chemistry of bile. In: Schultz SG, Forte JG,Rauner BB, eds. Handbook of physiologyThe gastrointestinal system III.Sec-tion 6. Baltimore: Waverly Press, 1989:62162.
7 van Erpecum KJ, Carey MC. Influence of bile salts on molecularinteractions between sphingomyelin and cholesterol: relevance to bileformation and stability.Biochim Biophys Acta1997;1345:26982.
8 Carey MC. Formation and growth of gallstones: the new synthesis. In:Fromm H, Leuschner U, eds. Bile acids,cholestasis and gallstones. Dordrecht:Kluwer, 1995:14775.
9 Holan KR, Holzbach RT, Hermann RE, et al. Nucleation time: a key factorin the pathogenesis of cholesterol gallstone disease. Gastroenterology1979;77:61117.
10 Halpern Z, Dudley MA, Kibe A, et al. Rapid vesicle formation and aggrega-tion in abnormal human biles: A time-lapse video-enhanced contrastmicroscopy study.Gastroenterology 1986;90:87585.
Figure 2 Potential mechanisms of cholest erol gallstone formation.
Frequency of intestinal migrating motor complex
Intestinal transit time
Deoxycholic acid pool size
Biliary cholesterol secretion
Bile concentration
Gall bladder hypomotilityDestabilisation of biliary vesicles
Cholesterol crystallisation
Gallstone formation
Are gallstones an intestinal disease? 437
group.bmj.comon September 12, 2014 - Published bygut.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://gut.bmj.com/http://gut.bmj.com/http://group.bmj.com/http://gut.bmj.com/ -
8/11/2019 Gut 1999 Van Erpecum 435 8
4/5
11 van Erpecum KJ, van Berge-Henegouwen GP, Stolk MFJ,et al. Fasting gallbladder volume, postprandial emptying and cholecystokinin release in gall-stone patients and normal subjects.J Hepatol1992;14:194202.
12 Portincasa P, Di Ciaula A, Baldassarre G,et al. Gall bladder motor functionin gallstone patients: sonographic and in vitro studies on the role ofgallstones, smooth muscle function and gall bladder wall inflammation. JHepatol1994;21:43040.
13 Lanzini A, Jazrawi RP, Northfield TC. Simultaneous quantitative measure-ments of absolute gall bladder storage and emptying during fasting andeating in humans.Gastroenterology 1987;92:85261.
14 Howard PJ, Murphy GM, Dowling RH. Gall bladder emptying patterns inresponse to a normal meal in healthy subjects and patients with gallstones:ultrasound study.Gut1991;32:140611.
15 Jazrawi RP, Pazzi P, Petroni ML, et al. Postprandial gall bladder motorfunction: refilling and turnover of bile in health and cholelithiasis. Gastroen-
terology1995;109:58291.16 Chen Q, Amaral J, Oh S,et al. Gall bladder relaxation in patients with pig-
ment and cholesterol stones. Gastroenterology1997;113:9307.17 Xu QW, ShaVer EA. The potential site of impaired gall bladder contractility
in an animal model of cholesterol gallstone disease. Gastroenterology 1996;110:2517.
18 Behar J, Rhim B, Thompson WR, et al. Inositol triphosphate restoresimpaired human gall bladder motility associated with cholesterol stones.Gastroenterology1993;104:5638.
19 Fridhandler TM, Davison JS, ShaVer EA. Defective gall bladder contractil-ity in the ground squirrel and prairie dog during the early stages of choles-terol gallstone formation.Gastroenterology 1983;85:8306.
20 Brugge WR, Brand DL, Atkins H,et al. Gall bladder dyskinesia in chronicacalculous cholecystitis.Dig Dis Sci1986;31:4617.
21 Pauletzki J, Althaus R, Holl J, et al. Gall bladder emptying and gallstoneformation: a prospective study on gallstone recurrence. Gastroenterology1996;111:76571.
22 Sitzmann JV, Pitt HA, Steinborn PA, e t al . Cholecystokinin preventsparenteral nutrition induced biliary sludge in humans. Surg Gynecol Obstet1990;170:2531.
23 Gebhard RL, Prigge WF, Ansel HJ,et al. The role of gall bladder emptyingin gallstone formation during diet-induced rapid weight loss. Hepatology1996;24:5448.
24 Shoda J, He B, Tanaka N,et al. Increase of deoxycholate in supersaturatedbile of patients with cholesterol gallstone disease and its correlation with denovo syntheses of cholesterol and bile acids in liver, gall bladder emptying,and small intestinal transit. Hepatology 1995;21:1291302.
25 Heaton KW, Emmett PM, Symes CL, et al. An explanation for gallstones innormal-weight women: slow intestinal t ransit.Lancet1993;341:810.
26 Jrgensen T. Abdominal symptoms and gallstone disease: an epidemiologi-cal investigation.Hepatology1989;9:85660.
27 Thomas LA, Bathgate T, Veysey MJ, et al. Is cholelithiasis an intestinal dis-ease [abstract]?Gut1997;41:A2.
28 Hussaini SH, Pereira SP, Murphy GM, et al. Deoxycholic acid influencescholesterol solubilization and microcrystal nucleation time in gall bladderbile.Hepatology1995;22:173544.
29 Hussaini SH, Murphy GM, Kennedy C,et al. The role of bile compositionand physical chemistry in the pathogenesis of octreotide-associated gallbladder stones.Gastroenterology1994;107:150313.
30 Veysey MJ, Gathercole DJ, Mallet A, e t al . Large bowel transit timeinfluences deoxycholic acid input rate and pool sizerisk factors foroctreotide-induced gallstones [abstract].Gastroenterology 1997;112:A525.
31 Berr F, Kullak-Ublick G, Paumgartner G,et al. 7-dehydroxylating bacteriaenhance deoxycholic acid input and cholesterol saturation of bile inpatients with gallstones.Gastroenterology1996;111:161120.
32 Xu Q, Scott RB, Tan DTM,et al. Slow intestinal transit: a motor disorder
contributing to cholesterol gallstone formation in the ground squirrel.Hepatology1996;23:166472.33 Wang DQ-H, Paigen B, Carey MC. Phenotypic characterization of Lith
genes that determine susceptibility to cholesterol cholelithiasis in inbredmice: physical-chemistry of gallbladder bile.J Lipid Res 1997;38:1395411.
34 van der Werf SDJ, van Berge-Henegouwen GP, Ruben AT, et al. Biliary lipids,bile acid metabolism, gall bladder motor function and small intestinal transitduring ingestion of a sub-fifty oral contraceptive.J Hepatol1987;4:31826.
35 Vlahcevic ZR, Stravitz RT, Heuman DM, et al. Quantitative estimations ofthe contribution of diVerent bile acid pathways to total bile acid synthesisin the rat.Gastroenterology1997;113:194957.
36 Cooper AD. Bile salt biosynthesis: an alternate synthetic pathway joins themainstream. Gastroenterology 1997;113:20058.
37 Brown HJ, Read NW, Richardson A, et al. Characteristics of lipid substancesactivating the ileal brake in the rat. Gut1990;31:11269.
38 Xu Q, ShaVer EA. The influence of bile salts on small intestinal motility inthe guinea pig in vitro.Gastroenterology 1992;103:2935.
39 Stolk MFJ, van de Heijning BJM, van Erpecum KJ,et al. The eVect of bilesalt hydrophobicity on nucleation of several types of cholesterol crystalsfrom model bile vesicles.J Hepatology 1994;20:80210.
40 Wang DQ-H, Carey MC. Complete mapping of crystallization pathwaysduring cholesterol precipitation from model bile: influence of physical-
chemical variables of pathophysiologic significance and identification of astable liquid-crystalline state in cold, dilute and hydrophilic bilesalt-containing systems.J Lipid Res 1996;37:60630.
41 Ozeki K, Sarna SK, Condon RE, et al. Enterohepatic circulation is essentialfor regular cycling of duodenal migrating motor complexes in dogs. Gastro-enterology1992;103:75967.
42 Stolk MFJ, van Erpecum KJ, Smout AJPM,et al. Motor cycles with phaseIII in antrum are associated with high motilin levels and prolonged gallbladder emptying.Am J Physiol1993;264:G596600.
43 DiMagno EP, Hendricks JC, Go VLW, et al. Relationships among caninefasting pancreatic and biliary secretions, pancreatic duct pressure, andduodenal phase III motor activityBoldireVrevisited. Dig Dis Sci1979;24:68993.
44 Svenberg T, Nilsson I, Samuelson K, et al. Studies on the causal relationshipbetween gall bladder emptying and motilin release in man.Acta Chir Scand1984;520:S5961.
45 Stolk MFJ, van Erpecum KJ, Samson M,et al. Interdigestive gall bladderemptying, antroduodenal motility and motilin release in cholesterolgallstone patients. In: Stolk MFJ, ed. Pathogenesis of cholesterol gallstones.Utrecht: Thesis Universiteit Utrecht, 1993:6578.
46 Xu Q-W, Scott RB, Tan DTM,et al. Altered migrating myoelectrical com-plex (MMC) in an animal model of cholesterol gallstone disease [abstract].
Gastroenterology1997;112:A1417.47 Itoh Z, Takahashi I, Nakaya M, et al. Interdigestive gall bladder bile concen-tration in relation to periodic contraction of gall bladder in the dog. Gastro-enterology1982;83:64551.
48 van Erpecum KJ, van Berge-Henegouwen GP, Stoelwinder B, et al. Bileconcentration is a key factor for nucleation of cholesterol crystals and chol-esterol saturation index in gall bladder bile of gallstone patients.Hepatology1990;11:16.
49 van Erpecum KJ,Stolk MFJ, van den Broek AMWC, et al. Bile concentrationpromotes nucleation of cholesterol monohydrate crystals by increasing thecholesterol concentration in the vesicles. Eur J Clin Invest1993;23:2838.
50 Conter RL, Roslyn JJ, Porter-Fink V, et al. Gall bladder absorption increasesduring early cholesterol gallstone formation. Am J Surg1986;151:18492.
51 Strichartz SD, Abedin MZ, Abdou MS,et al. The eVects of amiloride onbiliary calcium and cholesterol gallstone formation. Ann Surg1989;209:1526.
52 Ginanni Corradini S, Giovannelli L, Elisei W, et al. Cholesterol molar percentof bile influences the rate of phosphatidylcholine but not cholesterol absorp-tion by the gall bladder mucosa [abstract]. Gut1997;41:A32.
53 Ross PE, Butt AN, Gallacher C. Cholesterol absorption by the gall bladder.J Clin Pathol1990;43:5725.
54 Jacyna MR,Ross PE,Bakar MA,et al. Characteristics of cholesterol absorp-tion by human gall bladder: relevance to cholesterolosis. J Clin Pharmacol
1987;40:5249.55 Stolk MFJ,van Erpecum KJ,Renooij W, et al. Gall bladder emptying in vivo,
bile composition and nucleation of cholesterol crystals in patients withcholesterol gallstones.Gastroenterology 1995;108:18828.
56 Keulemans YCA, Mok KS,de Wit LT, et al. Hepatic bile versus gall bladderbile: a comparison of protein and lipid concentration and composition incholesterol gallstone patients.Hepatology1998;28:1116.
438 van Erpecum, van Berge-Henegouwen
group.bmj.comon September 12, 2014 - Published bygut.bmj.comDownloaded from
http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://gut.bmj.com/http://gut.bmj.com/http://group.bmj.com/http://gut.bmj.com/ -
8/11/2019 Gut 1999 Van Erpecum 435 8
5/5
doi: 10.1136/gut.44.3.4351999 44: 435-438Gut
K J VAN ERPECUM and G P VAN BERGE-HENEGOUWENGallstones: an intestinal disease?
http://gut.bmj.com/content/44/3/435.full.htmlUpdated information and services can be found at:
These include:
References
http://gut.bmj.com/content/44/3/435.full.html#related-urlsArticle cited in:
http://gut.bmj.com/content/44/3/435.full.html#ref-list-1
This article cites 51 articles, 6 of which can be accessed free at:
serviceEmail alerting
box at the top right corner of the online article.Receive free email alerts when new articles cite this article. Sign up in the
Notes
http://group.bmj.com/group/rights-licensing/permissionsTo request permissions go to:
http://journals.bmj.com/cgi/reprintformTo order reprints go to:
http://group.bmj.com/subscribe/To subscribe to BMJ go to:
group.bmj.comon September 12, 2014 - Published bygut.bmj.comDownloaded from
http://gut.bmj.com/content/44/3/435.full.htmlhttp://gut.bmj.com/content/44/3/435.full.html#related-urlshttp://gut.bmj.com/content/44/3/435.full.html#ref-list-1http://group.bmj.com/group/rights-licensing/permissionshttp://group.bmj.com/group/rights-licensing/permissionshttp://journals.bmj.com/cgi/reprintformhttp://journals.bmj.com/cgi/reprintformhttp://group.bmj.com/subscribe/http://group.bmj.com/http://group.bmj.com/http://group.bmj.com/http://gut.bmj.com/http://gut.bmj.com/http://group.bmj.com/http://gut.bmj.com/http://group.bmj.com/subscribe/http://journals.bmj.com/cgi/reprintformhttp://group.bmj.com/group/rights-licensing/permissionshttp://gut.bmj.com/content/44/3/435.full.html#related-urlshttp://gut.bmj.com/content/44/3/435.full.html#ref-list-1http://gut.bmj.com/content/44/3/435.full.html