Global INitiative for Asthma Guidelines 2006 - The … · History 1993 Global Initiative for Asthma...
Transcript of Global INitiative for Asthma Guidelines 2006 - The … · History 1993 Global Initiative for Asthma...
History History
1993 Global Initiative for Asthma (GINA) 1993 Global Initiative for Asthma (GINA) formedformed1995 goals and objectives were 1995 goals and objectives were described in NHLBI/ WHO workshop described in NHLBI/ WHO workshop reportreport2002 revised2002 revised11stst update in 2003 October, 2update in 2003 October, 2ndnd 2004 , 32004 , 3rdrd
2005 and latest in 2006 November2005 and latest in 2006 November
Definition Definition A chronic inflammatory disorder of the A chronic inflammatory disorder of the airwaysairwaysMany cells and cellular elements play a roleMany cells and cellular elements play a roleChronic inflammation is associated with Chronic inflammation is associated with airway hyperresponsiveness that leads to airway hyperresponsiveness that leads to recurrent episodes of wheezing, recurrent episodes of wheezing, breathlessness, chest tightness, and breathlessness, chest tightness, and coughingcoughingWidespread, variable, and often reversible Widespread, variable, and often reversible airflow limitationairflow limitation
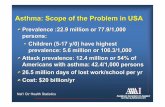
Burden of asthmaBurden of asthmaAsthma is one of the most common chronic Asthma is one of the most common chronic diseases worldwide with an estimated 300 diseases worldwide with an estimated 300 million affected individualsmillion affected individualsPrevalence increasing in many countries, Prevalence increasing in many countries, especially in children and range from 1% to especially in children and range from 1% to 18%18%A major cause of school/work absenceA major cause of school/work absence1% of the total global disease burden *1% of the total global disease burden *
*Masoli et al. Allergy2004;59(5):469-78
Factors that Influence Asthma Factors that Influence Asthma Development and ExpressionDevelopment and Expression
Host FactorsHost FactorsGeneticGenetic
-- AtopyAtopy -- IgEIgE , cytokine, cytokine-- Airway hyperresponsiveness Airway hyperresponsiveness --chromosome 5 chromosome 5 ##
GenderGender-- childhood <14 year M>F, adult childhood <14 year M>F, adult F>MF>MObesityObesity –– LeptinLeptin**
#Postma et al. N Engl J Med1995;333(14):894-900 *Beuther et al. Am J Respir Crit Care Med2006;174(2):112-119
Environmental factorsEnvironmental factorsIndoorIndoor allergensallergens-- mites, cockroaches, mites, cockroaches, house dusthouse dustOutdoorOutdoor allergensallergensOccupationalOccupational sensitizerssensitizers-- >300 >300 substances substances egeg. Isocyanates, platinum . Isocyanates, platinum salts, plants and animal products. High salts, plants and animal products. High risk in farming and agricultural workers, risk in farming and agricultural workers, painting, cleaning, plastic manufacturingpainting, cleaning, plastic manufacturingAir PollutionAir Pollution
Tobacco smokeTobacco smoke-- accelerated decline in accelerated decline in lung function. >4 times in infant of lung function. >4 times in infant of smoking mothers smoking mothers ##
Respiratory InfectionsRespiratory Infections-- RSV, Para influenza RSV, Para influenza produce symptoms similar to asthmaproduce symptoms similar to asthma$$
Measles protect against asthmaMeasles protect against asthma**DietDiet-- breast feeding protect against breast feeding protect against asthmaasthma****Hygiene hypothesis Hygiene hypothesis ####
#Dezateux et al. Am J Respir Crit Care Med1999;159(2):403-10
$ Sigurs et al. Am J Respir Crit Care med2000;161(5):1501-7
*Shaheen et al. Lancet1996;347(9010):1792-1796
** Friedman et al. J Allergy Clin Immunol2005;115(6):1238-48
##Meer et al. Allergy2005;60(5):619-625
HistoryHistoryRecurrent episodes of wheezingRecurrent episodes of wheezingTroublesome cough at nightTroublesome cough at nightCough or wheeze after exerciseCough or wheeze after exerciseCough, wheeze or chest tightness after Cough, wheeze or chest tightness after exposure to airborne allergens or exposure to airborne allergens or pollutantspollutantsColds Colds ““go to the chestgo to the chest”” or take more or take more than 10 days to clearthan 10 days to clear
Cough variant asthmaCough variant asthmaChronic cough , more at nightChronic cough , more at nightVariability in lung function or airway Variability in lung function or airway hyperresponsivenesshyperresponsivenessD/D D/D eosinophiliceosinophilic bronchitis where LFT bronchitis where LFT normalnormalOther D/DOther D/DACE inhibitorsACE inhibitorsGERDGERDPost nasal dripsPost nasal dripsChronic sinusitisChronic sinusitisVocal cord dysfunctionVocal cord dysfunction
Exercise induced asthmaExercise induced asthma
55--10 min after completing exercise10 min after completing exerciseResolve spontaneously within 30Resolve spontaneously within 30--45 45 minminSymptoms similar to asthma Symptoms similar to asthma 8 min running protocol is use for 8 min running protocol is use for diagnosisdiagnosis**
*Anderson et al; Med J Aus2002:117Suppl:s61-63
Examination Examination
May beMay be normalnormal
MostlyMostly wheezingwheezing on auscultationon auscultationExacerbationExacerbation –– cyanosis, drowsiness, cyanosis, drowsiness,
difficulty in speaking, tachycardia, difficulty in speaking, tachycardia, hyperinflated chest, use of hyperinflated chest, use of accessory muscles and accessory muscles and intercostalintercostalrecessionrecession
Investigation Investigation Lung function test by spirometry or peak Lung function test by spirometry or peak expiratory flow meterexpiratory flow meterMeasurement of airway responsiveness Measurement of airway responsiveness
Measurements of allergic status to Measurements of allergic status to identify risk factorsidentify risk factors
Extra measures may be required to Extra measures may be required to diagnose asthma in children 5 years and diagnose asthma in children 5 years and younger and the elderlyyounger and the elderly
Pulmonary function testPulmonary function test continue to be continue to be recommended as an aid to diagnosis and recommended as an aid to diagnosis and monitoring. Show obstructive pattern monitoring. Show obstructive pattern
ReversibilityReversibility –– rapid improvement in FEVrapid improvement in FEV1 1 or PEF measured within minutes after or PEF measured within minutes after inhalation of SABA or more sustained inhalation of SABA or more sustained improvement over days or weeks after improvement over days or weeks after effective controller treatment like inhaled effective controller treatment like inhaled glucocorticoids. Significant glucocorticoids. Significant -- >12% or > >12% or > 200ml but not always200ml but not always
Variability Variability –– improvement or improvement or deterioration in symptoms and lung deterioration in symptoms and lung function over time e.g. Over days, function over time e.g. Over days, day to day, month to month or day to day, month to month or seasonal. PEF >20% significantseasonal. PEF >20% significantMeasure of variability of airflow Measure of variability of airflow limitation is given increase limitation is given increase prominence rather than reversibilityprominence rather than reversibilityAs, most asthma patients will not As, most asthma patients will not exhibit reversibility at each exhibit reversibility at each assessment assessment
Measurement of airway Measurement of airway responsivenessresponsiveness
MethacholineMethacholine, histamine, , histamine, mannitolmannitol or or exercise challenge testexercise challenge test##
Fall in FEVFall in FEV1 1 > 20% is diagnostic> 20% is diagnosticLimitationLimitation--
Limited specificity, positive in allergic Limited specificity, positive in allergic rhinitis, cystic fibrosis, bronchiectasis rhinitis, cystic fibrosis, bronchiectasis and COPD, fatal reactionand COPD, fatal reaction
#Cockroft et al; Clin Rev Allergy Immunol2003;24(1):19-26
NonNon--invasive markers of airway invasive markers of airway inflammationinflammation
Sputum Sputum eosinophileosinophil and and neutrophilneutrophilExhaled nitric oxide and carbon Exhaled nitric oxide and carbon monoxidemonoxide
Measurement of allergic statusMeasurement of allergic statusSkin testSkin testSpecific Specific IgEIgE
Look for alternative diagnosisLook for alternative diagnosis
In case of adult and older children In case of adult and older children Upper airway obstruction and FBUpper airway obstruction and FBHyperventilation syndrome and panic attackHyperventilation syndrome and panic attackVocal cord dysfunctionVocal cord dysfunctionOther obstructive lung diseases particularly Other obstructive lung diseases particularly COPDCOPDNon obstructive lung diseases e.g. DPLDNon obstructive lung diseases e.g. DPLDNon respiratory causes of symptoms e.g. Non respiratory causes of symptoms e.g. LVFLVF
New approach New approach
GINA 2006 emphasize asthma GINA 2006 emphasize asthma management based onmanagement based on
clinical controlclinical controlRather than classification of patient by Rather than classification of patient by
severityseverity
Cost dependsCost depends on individual patients on individual patients level of control and extent of level of control and extent of exacerbationexacerbationEmergency care is more Emergency care is more expensiveexpensivethan planned treatmentthan planned treatmentGuideline determined asthma care Guideline determined asthma care can be can be cost effectivecost effectiveWell control asthma reduce socioWell control asthma reduce socio--economic burden economic burden
more streamlined document that will more streamlined document that will be useful for busy cliniciansbe useful for busy clinicians
Updated epidemiological dataUpdated epidemiological data
Introduction of concept of difficult to Introduction of concept of difficult to treat asthmatreat asthma
Difficult to treat asthmaDifficult to treat asthma
Some patient develop asthma that is Some patient develop asthma that is difficult to manage difficult to manage Relatively insensitive to Relatively insensitive to glucocorticosteroidsglucocorticosteroidsMost of them have difficult to treat asthma Most of them have difficult to treat asthma from the onset rather than progressing from the onset rather than progressing from milder asthma from milder asthma Poor compliance, psychological and Poor compliance, psychological and psychiatric disorderspsychiatric disorders
Classification based on severity Classification based on severity ( intermittent, mild , moderate and ( intermittent, mild , moderate and severe ) is now recommended only for severe ) is now recommended only for research purposeresearch purpose
Present classification is controlled, Present classification is controlled, partly controlled and uncontrolledpartly controlled and uncontrolled
Emphasis is placed on the concept that Emphasis is placed on the concept that the goal of asthma treatment is to the goal of asthma treatment is to achieve and maintain controlachieve and maintain controlAsthma controlAsthma control is defined asis defined as
No ( twice or less/week) No ( twice or less/week) day time day time symptomssymptoms
No limitation of No limitation of daily activitiesdaily activitiesNo No nocturnal symptomsnocturnal symptoms or awakening or awakening No ( No ( ≤≤2/week) need for 2/week) need for reliever medicationreliever medicationNormal or near normal Normal or near normal lung functionlung functionresultsresults
No exacerbationNo exacerbation
TreatmentTreatment
Role of several medications have Role of several medications have evolved since previous version of the evolved since previous version of the report report
Medications Medications Controller
Inhaled glucocorticosteroidsLeukotriene modifiersLong-acting inhaled β2-agonistsSystemic glucocorticosteroids TheophyllineCromonesLong-acting oral β2-agonistsAnti-IgE(omalizumab)
Reliever•Rapid-acting inhaled β2-agonists- salbutamol, terbutaline, fenoterol, reproterol and pirbuterol•Systemic glucocorticosteroids•Anticholinergics –ipratropium bromide and oxitropium bromide•Theophylline•Short-acting oral β2-agonists
Oral anti allergic compoundsOral anti allergic compoundsE.g. E.g. tranilasttranilast, , repirinlastrepirinlast, , tazanolasttazanolastVery limited roleVery limited role
Other controller therapiesOther controller therapiesMethotrexateMethotrexateCyclosporinCyclosporinGoldGoldMacrolideMacrolidetroleandromycinetroleandromycine
Allergen-specific ImmunotherapyGreatest benefit of specific immunotherapy using allergen extracts has been obtained in the treatment of allergic rhinitisThe role of specific immunotherapy in asthma is limitedSpecific immunotherapy should be considered only after strict environmental avoidance and pharmacologic intervention, including inhaled glucocorticosteroids, have failed to control asthmaPerform only by trained physician
Recent data indicating an increase risk Recent data indicating an increase risk of asthma related death associated of asthma related death associated with long acting with long acting ββ2 2 agonists agonists (salmeterol) and should not be used (salmeterol) and should not be used as monotherapy. Only be used with as monotherapy. Only be used with an appropriate dose of inhaled an appropriate dose of inhaled corticosteroid corticosteroid
Leukotriene modifier now have a more Leukotriene modifier now have a more prominent roleprominent role
Changes in medication approach
Monotherapy with Monotherapy with cromonescromones is no is no longer an alternative to low dose longer an alternative to low dose inhaled glucocorticoids to adultsinhaled glucocorticoids to adults
Increase use of Increase use of rapid-acting inhaled β2-agonists is an indication of poor asthma control
Change in equipotent daily dose of inhaled Change in equipotent daily dose of inhaled glucocorticoids for both adults and glucocorticoids for both adults and
childrenchildrenLow Low adult (adult (μμgm )gm )
Low Low childrenchildren
Med. Med. adultadult
Med.Med.childrenchildren
High High adultadult
High High childrenchildren
BeclomethBeclomethasonason
200200--500 500 200200--500500
100100--200200100100--250250
500500--10001000500500--10001000
200200--400400250250--500500
10001000--20002000>1000>1000
>400 >400 newnew>500>500 oldold
BudesonidBudesonidee
200200--400400200200--600600
100100--200200100100--200200
400400--800800600600--10001000
200200--400400200200--600600
800800--16001600>1000>1000
>400>400>600>600
CiclosonidCiclosonidee
8080--160160 8080--160160 160160--320320 160160--320320 320320--12801280 >320>320
FluticasoneFluticasone 100100--250 250 100100--250250
100100--200200100100--200200
250250--500500250250--500500
200200--500500200200--400400
500500--10001000500500--10001000
>500>500>400>400
Change in asthma management Change in asthma management Previous Previous sixsix part asthma part asthma management program is changed to management program is changed to fivefive component component ––
1. Develop Patient/Doctor Partnership2. Identify and Reduce Exposure to
Risk Factors3. Assess, Treat and Monitor Asthma4. Manage Asthma Exacerbations5. Special Considerations
Component 1 reflect that control of Component 1 reflect that control of asthma requireasthma require--
EducationEducation
Include the family and joint setting of goalsInclude the family and joint setting of goals
Provide information about asthmaProvide information about asthma
Provide training on selfProvide training on self--management skillsmanagement skills
Follow up and reviewFollow up and review
Written action planWritten action plan
Improve adherenceImprove adherence
Factors Involved in NonFactors Involved in Non--AdherenceAdherence
Medication UsageMedication UsageDifficulties Difficulties associated with associated with inhalersinhalersComplicated Complicated regimensregimensFears about, or Fears about, or actual side actual side effectseffectsCostCostDistance to Distance to pharmaciespharmacies
Non-Medication FactorsMisunderstanding/lack
of informationFears about side-effects Inappropriate
expectationsUnderestimation of
severityAttitudes toward ill
healthCultural factorsPoor communication
Component 2: Identify and Reduce Exposure to Risk Factors
Indoor allergens Indoor allergens –– domestic mites, furred domestic mites, furred animals, cockroaches and fungianimals, cockroaches and fungiOutdoor allergen Outdoor allergen –– pollens and moldspollens and moldsIndoor air pollutants Indoor air pollutants –– primary/secondary primary/secondary smoke, nitric oxide, carbon monoxide, smoke, nitric oxide, carbon monoxide, carbon dioxide, carbon dioxide, sulphursulphur dioxide, dioxide, formaldehyde etcformaldehyde etcOutdoor air pollutants Outdoor air pollutants –– ozone, nitrogen ozone, nitrogen oxides, acidic aerosols and particulate oxides, acidic aerosols and particulate matter matter Influenza vaccination Influenza vaccination
Cont.Cont.
Occupational exposureOccupational exposureFood and food additives Food and food additives –– sulphitessulphites in food in food and drug preservatives found in processed and drug preservatives found in processed potatoes, shrimp, dried fruits, bear and potatoes, shrimp, dried fruits, bear and wine. Other dietary substances like wine. Other dietary substances like ––yellow dye yellow dye tartazinetartazine, benzoate and , benzoate and monosodium glutamate monosodium glutamate Drugs Drugs –– aspirin and aspirin and NSAIDsNSAIDsObesityObesityEmotional stressEmotional stressOther factors Other factors –– Rhinitis, sinusitis and Rhinitis, sinusitis and polyposis polyposis
Component 3: Component 3: AssessAssess, Treat and , Treat and Monitor AsthmaMonitor Asthma
CharacteristicCharacteristic ControlledControlledPartly controlledPartly controlled(Any one present in (Any one present in
any week)any week)UncontrolledUncontrolled
Daytime Daytime symptomssymptoms
None (2 or less / None (2 or less / week)week)
More than More than twice / weektwice / week
Limitations of Limitations of activitiesactivities NoneNone AnyAny
Nocturnal Nocturnal symptoms / symptoms / awakeningawakening
NoneNone AnyAny
Need for rescue / Need for rescue / ““relieverreliever””treatmenttreatment
None (2 or less / None (2 or less / week)week)
More than More than twice / weektwice / week
Lung function Lung function (PEF or FEV(PEF or FEV11)) NormalNormal
< 80% predicted or < 80% predicted or personal best (if personal best (if known) on any known) on any
dayday
3 or more 3 or more features of features of partly partly controlled controlled asthma asthma present in present in any weekany week
ExacerbationsExacerbations NoneNone One or more per One or more per One in any One in any
Treat Treat Treatment steps Treatment steps ––
Step 1: as needed reliever medicationStep 1: as needed reliever medicationStep 2: Reliever medication plus a single Step 2: Reliever medication plus a single controllercontrollerStep 3: Reliever medication plus one or two Step 3: Reliever medication plus one or two controllerscontrollersStep 4: Reliever medication plus two or more Step 4: Reliever medication plus two or more controllers controllers Step 5: Reliever medication plus additional Step 5: Reliever medication plus additional controller optioncontroller option
Stepping downStepping down
When controlled on medium- to high-dose inhaled glucocorticosteroids: 50% dose reduction at 3 month intervals *When controlled on low-dose inhaled glucocorticosteroids: switch to once-daily dosing Maintain control at lowest possible step and lowest dose
*Hawkins et al. BMJ 2003; 326(7399): 1115
Stepping upStepping upNeed for repeated dosing over more than one/two days signals need for possible increase in controller therapyUse of a combination rapid and long-acting inhaled β2-agonist (e.g., formoterol) and an inhaled glucocorticosteroid (e.g., budesonide) in a single inhaler both as a controller and reliever is effecting in maintaining a high level of asthma control and reduces exacerbations**Temporarily doubling the dose of inhaled glucocortico-steroids is not effective, and is not recommended. A four fold rise or more is equal to short course of oral steroids *
**Rabe et al.Chest2006;129(2):246-256
*Reddel et al.Eur Respir J2006;28(1):182-199
Component 4: Manage Asthma Component 4: Manage Asthma ExacerbationsExacerbations
Exacerbations of asthma are episodes Exacerbations of asthma are episodes of progressive increase in shortness of progressive increase in shortness of breath, cough, wheezing, or chest of breath, cough, wheezing, or chest tightnesstightness
Patient with high riskPatient with high riskH/O near fatal asthma require intubation and H/O near fatal asthma require intubation and mechanical ventilationmechanical ventilationH/O hospitalization or emergency visit in past H/O hospitalization or emergency visit in past yearsyearsCurrently or recently use oral Currently or recently use oral glucocorticosteroidsglucocorticosteroidsNot currently using inhaled Not currently using inhaled glucocorticosteroidsglucocorticosteroidsOver dependant on SABAOver dependant on SABAPsychiatric disease or psychosocial problemsPsychiatric disease or psychosocial problemsNoncompliance Noncompliance
mildmild moderatemoderate Severe Severe RespiRespi. Arrest. Arrest
breathlessnebreathlessnessss
Can lie downCan lie down sittingsitting Hunch Hunch forwardforward
Talk in Talk in sentencessentences phrasesphrases wordswordsalertnessalertness May be May be
agitatedagitatedUsually Usually agitatedagitated
Usually Usually agitatedagitated
Drowsy / Drowsy / confusedconfused
RRRR increasedincreased increasedincreased > 30/min> 30/minAcc. Muscle Acc. Muscle /retraction/retraction
Usually notUsually not usuallyusually UsuallyUsually ParadoxicalParadoxicalAbdAbd move.move.
wheezewheeze ModerateModerate loudloud Usually loudUsually loud absentabsentPulse/minPulse/min <100<100 100100--120120 > 120> 120 bradycardiabradycardia
PulsusPulsusparadoxusparadoxus
absentabsent May be May be presentpresent
Often +Often + Absent due Absent due to fatigueto fatigue
PEFPEF-- post post bronchodilatorbronchodilator
>80%>80% 6060--80%80% <60% or <60% or response <2hrresponse <2hr
PaO2(on air) PaO2(on air) or PaCO2or PaCO2
NormalNormal< 45mm Hg< 45mm Hg
>60 mm Hg>60 mm Hg<45mm Hg<45mm Hg
<60 mm Hg<60 mm Hg>45 mm Hg>45 mm Hg
SaO2%SaO2% >95%>95% 9191--95%95% <90%<90%
Initial assessmentInitial assessmentHistory, examination, SpOHistory, examination, SpO2 2 , ABG, ABG
↓↓Initial treatmentInitial treatment
O2 to keep saturation >90% (children O2 to keep saturation >90% (children >95%)>95%)Inhaled SABAInhaled SABASystemic glucocorticosteroids (if no rapid Systemic glucocorticosteroids (if no rapid response, pt is on oral steroids or severe response, pt is on oral steroids or severe episodes)episodes)Sedation contraindicatedSedation contraindicated
↓↓Reassess after 1 hrReassess after 1 hr
CCont.ont.
Moderate episodesModerate episodes Severe episodesSevere episodesPEF 60 PEF 60 –– 80% 80% personal bestpersonal bestModerate symptomsModerate symptomsAccessory muscle Accessory muscle useuseTreatment:Treatment:O2 , inhaled O2 , inhaled ββ2 2 agonistagonist & inhaled & inhaled anticholinergicsanticholinergicsevery 60min, oral every 60min, oral glucocorticoicosteroiglucocorticoicosteroidesdescont. for 1cont. for 1--3 hrs3 hrs
Risk factor for near Risk factor for near fatal asthmafatal asthmaPEF <60%PEF <60%Severe symptom at Severe symptom at rest, chest retractionrest, chest retractionNo improvementNo improvementTreatment:Treatment:O2, Inhaled O2, Inhaled ββ2 2 agonist & agonist & anticholinergicsanticholinergics, , systemic systemic glucocortricosteroidsglucocortricosteroids, I.V. MgSO4, I.V. MgSO4Reassess after 1-2 hrs cont.
Good Good response response
Incomplete Incomplete responseresponse
Poor responsePoor response
Normal Normal physical physical examinationexamination>70% , >70% , SpO2>90%SpO2>90%
Risk factor for near Risk factor for near fatal asthma, mild to fatal asthma, mild to mod signs, PEF < 60%, mod signs, PEF < 60%, SpO2 <90%SpO2 <90%
Risk Risk factors+,severefactors+,severesymptomssymptoms--drowsiness, drowsiness, confused, PEF < confused, PEF < 30%, PCO2 > 45, PO2 30%, PCO2 > 45, PO2 <60 <60
Home Home treatmenttreatment
Admit to acute care Admit to acute care settingsettingO2, O2, ββ2 agonist, anti 2 agonist, anti cholinergicscholinergics, systemic , systemic steriodssteriods, I.V.MgSO4, I.V.MgSO4Assess after 6Assess after 6--12 hr12 hr
←←improveimprove//notnot→→
Admit to Admit to intensive careintensive careO2, O2, ββ2 agonist, anti 2 agonist, anti cholinergicscholinergics, , systemic systemic steriods,considersteriods,consider I.V. I.V. ββ2 agonist, I.V. 2 agonist, I.V. theophyllinestheophyllines, , intubation and intubation and
h i lh i l
Component 5:Special considerations are Component 5:Special considerations are required torequired to
manage asthma in relation to:manage asthma in relation to:PregnancyPregnancy-- 1/3 worse, 1/3 less severe and 1/3 1/3 worse, 1/3 less severe and 1/3 unchanged unchanged **. Poor control leads to increase . Poor control leads to increase perinatalperinatal mortality, mortality, prematuarityprematuarity and LBWand LBWMonitored use of theophylline, inhaled Monitored use of theophylline, inhaled glucocorticosteroids, glucocorticosteroids, ββ2 agonist and 2 agonist and leucotriene modifiers are safeleucotriene modifiers are safeSurgerySurgery-- systemic glucocorticoids coverage systemic glucocorticoids coverage during the surgical period and reduce rapidly during the surgical period and reduce rapidly 24hr after surgery for wound healing24hr after surgery for wound healing
*Schatz et al. J Allergy Clin Immunol1999;103(2Pt2):s330-6
Rhinitis, sinusitis, and nasal polypsRhinitis, sinusitis, and nasal polypsOccupational asthmaOccupational asthma-- complete avoidance complete avoidance of the relevant exposureof the relevant exposureRespiratory infectionsRespiratory infectionsGastroesophagealGastroesophageal refluxrefluxAspirinAspirin--induced asthmainduced asthma-- in minute to hrs in minute to hrs patient experience vasomotor rhinitis and patient experience vasomotor rhinitis and rhinorrhoearhinorrhoea, attack of asthma and may lead , attack of asthma and may lead to violent to violent bronchospasmbronchospasm and even and even respiratory arrestrespiratory arrestAnaphylaxis and AsthmaAnaphylaxis and Asthma-- epinephrine is epinephrine is the bronchodilator of choice the bronchodilator of choice
Asthma can be effectively controlled in most patients by intervening to suppress and reverse inflammation as well as treating bronchoconstriction and related symptomsAlthough there is no cure for asthma, appropriate management that includes a partnership between the physician and the patient/family most often results in the achievement of control
Conclusion