Genetic Alliance UK Autumn newsletter
-
Upload
genetic-alliance -
Category
Documents
-
view
227 -
download
1
description
Transcript of Genetic Alliance UK Autumn newsletter

Genetic Alliance UK
We’ve joined the party at the European
Medicines Agency
Page 3
The imminent launch of the rare
disease plan
Pages 4 & 5
Annual
conference and
AGM 2013
Pages 6 & 7
Want to get
involved in our
work in the
devolved nations?
Pages 11 & 12
In this
issue As we move into Autumn the shape of the UK Strategy for Rare Diseases becomes clearer. As a high level strategic document for the whole of the UK it will not contain too many details about how improved services and support will be delivered on the ground. This is the responsibility of the NHS in each of the four countries of the UK, but it will provide a series of yardsticks against which the implementation
strategies can be measured.
Headlines in the plan include better access to diagnosis, improved information to patients, more and better rare disease research, greater patient engagement and empowerment and a commitment to reconvene the stakeholder group set up to support the development of the plan as a monitoring group; the group will have a duty to report to ministers on progress every two years. This should help ensure that the plan is a living document that
does not gather dust on the shelf.
Following the Prime Minister’s announcement last Christmas that 100,000 NHS patients would have their genomes sequenced for research and clinical use the Department of Health has set up Genomics England. As a wholly owned company its mission is to secure the delivery of the benefits from this pledge for the NHS and promote opportunities for the development of innovations through effective multi stakeholder working
including the private sector.
This is a bold step. We are watching with interest to see how it will work in practice, and that the interests of
patients and families are front and centre in the planning and execution of this venture. The focus of this initiative is cancer, rare diseases and infectious diseases, all of which pose significant challenges for the NHS now
and for the future.
Closer to home we were delighted that our project SWAN UK was shortlisted by the Big Lottery as one of the best projects of the year. We did not win, (you can see the winners on page three) but we were a very creditable runner up and were featured on the lottery programme in August. You can view the film on YouTube - www.youtube.com/watch?
v=QuBA5fPItxo.
I was delighted to be asked to propose the motion “This House would Engineer its Babies” at the St Andrew’s University Union. This is one of the oldest university debating societies in the UK, and it was a great opportunity to tackle some of the myths and wilder assertions about genetics, and remind those attending about the realities for families at risk of having children affected by life limiting genetic
disorders.
Finally, I know you will want to join us in celebrating the safe birth of a daughter, Emmeline, to our Assistant Director, Melissa Hillier. Mother and baby are doing well, and her little boy seems delighted to have a baby sister to play with. Alastair Kent, Director
Autumn 2013
The first UK strategy for rare diseases,
new projects and new opportunities to
get involved this Autumn!

Genetic Alliance UK Newsletter Autumn 2013
2
We will soon have a new section on our website focusing on preimplantation genetic diagnosis (PGD). This is the result of a great deal of work over the past year to gather and prepare information on PGD for all those that may be interested in it. This will include the history of PGD, information for couples who may wish to access PGD, information on funding for
PGD and much more.
This process has been a fascinating experience for us. Do you know when the first PGD birth was? It was in 1990 in London. That was for sex selection for a couple at risk of having a child with an X-linked
condition.
As Policy Analyst, the part of the new site which interests me the most will perhaps come as a surprise. We will for the first time publish our condition by condition statements that comment on licence applications to the HFEA. This will be a resource, which for the first time in the UK (that we are aware of!) will list on a condition by condition basis the reason why PGD should be available to help couples at risk of having a child affected by the condition. For me, this will allow us to move from the theoretical debates and hand-wringing that can often surround the issue in the UK, and move towards discussing the ability for couples to avoid the birth of children affected by specific
conditions, for specific reasons.
Being able to take an overview of the 124 statements that we have submitted to the HFEA, plus the additional statements that we have produced with members to cover
collected. These include stories from those that have used PGD and those
that have chosen not to.
The alternatives to PGD are not
equivalent to PGD
There are many options available to couples at risk of having a child affected by a genetic condition. These are all equally valid, and appropriate to different couples for different reasons. However there is only one option that allows a couple to have a child, who is biologically their own and free from a genetic condition, without having to contemplate a termination of pregnancy, and that is PGD. Some of our couples’ stories focus on why they have chosen PGD and one of the key points they make is this one: PGD is the only way to have a child
in the way they wish to.
As I write this, Alastair Kent OBE, our Director, has recently debated (and won) in favour of PGD at St. Andrew’s University, and next week I will be part of a panel discussion of the topic at the British Library. It’s inevitable that a ground breaking technique such as this will continue to gather significant attention (and policy people love to debate!); but reading the information we have put together for this project has shown me that when you see the value of PGD through the eyes of our members, the points for debate
seem to fade into the background.
Nick Meade, Policy Analyst,
conditions that were not licensed through the current route, has made
a few things clear to me:
Couples are making an informed
choice
In the vast majority of cases of PGD in the UK, couples are asking for PGD because they have experience of the condition they would like to avoid. One member of the couple may be affected by the condition, as is the case with autosomal dominant conditions. They may have lived through one of their parents dealing with the disease, as is the case with late-onset autosomal dominant conditions. The first they may have heard of the condition is when a previous pregnancy was diagnosed, or when their child began developing symptoms. In all these cases, the family has had direct experience of the condition. This is an informed choice based on evidence and experience that very
few of us have.
There is no spectrum of severity
The way the HFEA must judge PGD licence applications is to consider whether the condition is "serious" or not. This requirement was made during the most recent revision of the Human Fertilisation and Embryology Act in 2008. This concept brings to mind a line in the sand of severity which all conditions must be able to get to when arguing their case. Of course, this is not how the process works, but it was only when we considered all the statements that we have prepared that the breadth of types
of severity become clear.
Another wonderful piece of this project is the stories we have
Patients’ stories bring meaning and weight
to the preimplantation genetic diagnosis
policy debate

Genetic Alliance UK Newsletter Autumn 2013
3
We’ve joined the party! I have just joined the Patient and Consumer’s Working Party (PCWP) at the European Medicines Agency (EMA). This will allow us to have a stronger voice in issues related to medicines regulation in Europe, as this is the group EMA turns to if it requires advice from
patients and patient groups.
To finish off the acronym heavy beginning to this article, EGAN, the Patient’s Network for Medical Research and Health, is a European patient organisation of which Genetic Alliance UK are members. EGAN stands for European Genetic Alliances’ Network. This is the main vehicle through which we can represent our members in Europe, and this is the group I
will be representing at the Agency.
A new three-year term of the PCWP has just started, and we have been accepted as members in an expansion of the group. This is an exciting time for medicine regulation, so we are pleased to be able to have a voice in the EMA’s ear. It seems that finally the products of many years of research into our members’ conditions is beginning to bear fruit, as potential treatments for muscular dystrophy and polycystic kidney disease amongst others both make their way through the regulatory process. The regulation of these treatments brings certain challenges that we hope the
PCWP will be able to assist the Agency in solving.
Of course this is only one way we’re involved in the work of EMA. In the past Alastair Kent OBE and I have been member and alternate member respectively of the Committee for Advanced Therapies, which advises on gene therapies and stem cell therapies for EMA. Some of you will also know about the work we do to
review package leaflets of new medicines to ensure this information is clearly presented. We have also arranged for some of our members to participate in a Scientific Advice Group at EMA, but the secrecy that surrounds that work is such that I’m not sure if I can even
say that here!
The work of the PCWP over the next year will be broad. We will continue the bread and butter work of the group in working with the EMA to review information for communication with the public, including an interesting piece of work on risk communication, and work on communicating shortage of medicines. There will be an element of work that contributes to ongoing discussions
on access to clinical trial data in Europe.
The most exciting thing that may happen over the next three years are the first steps towards a new model for regulating medicines, that is more capable of reacting to patient views, and better equipped to judge the effectiveness of medicines in the real world. It won’t
necessarily be a party, but it will be interesting!
Nick Meade, Policy Analyst,
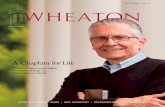
Nick with Kaisa from the European
Patients' Forum.
Picture taken by Lise Murphy
We’re delighted for the Icthyosis Support Group (ISG) and are pleased their excellent work has been recognised by their members in voting for them in this
award and by the National Lottery.
Liz Dale from the Icthyosis Support Group (ISG) said: “This is such an amazing achievement for our small charity and is already raising the profile of ichthyosis and the ISG, helping to highlight the condition in the public eye. We never thought we would win such a prestigious award but thanks to all of your hard work
we managed to pull in the votes - a staggering 4,882 -
which would have won any of the 6 other categories too! We managed to get 730 more votes than the runner up in the health category, which just
shows the amazing support we have had.“
Congratulations to the ISG on
winning the National Lottery
Awards!
Len Goodman presents the award to families

Genetic Alliance UK Newsletter Autumn 2013
4
The imminent launch of the UK rare disease strategy
and what is a Centre of Excellence? advocate for country-specific
strategies across the devolved
nations of the UK;
work alongside government and NHS officials to achieve effective implementation in all four home
nations.
At our Westminster reception it was announced by Earl Howe, the minister in charge of rare diseases, that the Department of Health in England would establish a Rare Disease Stakeholder Forum to develop the National Strategy for Rare Diseases. This Forum has fulfilled that responsibility and will now focus its efforts on monitoring; RDUK is pleased to have representatives attending the Forum from all four
home nations.
Rare Disease Advisory Group
Chair of Rare Disease UK, Alastair Kent, has been appointed to NHS England's Rare Disease Advisory Group (RDAG). This new body will advise NHS England and the
After five years of campaigning we are now weeks away from the publication of the National Strategy
for Rare Diseases in November.
RDUK has worked tirelessly to ensure that the voice of the rare disease community has been heard and represented in the development of the National Strategy. We know that an effective strategy for rare diseases would not only improve the quality of services and health outcomes for people with rare diseases, but would also ensure a
more efficient use of NHS resources.
However, our work does not end here. RDUK will now campaign for the effective implementation of the National Strategy for Rare Diseases to ensure high quality services and better health outcomes for people
with rare diseases. We will:
work towards clear policies to ensure accountability for its implementation in practice and
that the outcomes are measured;
Rare Disease UK (RDUK) was established by Genetic Alliance UK in 2008 following the European Commission’s Communication on Rare Diseases: Europe’s Challenges. On the back of this Communication, RDUK successfully campaigned for the adoption of the Council of the European Union’s Recommendation on an action in the field of rare diseases (June 2009). The Recommendation outlines how EU Member States should develop and implement plans or strategies for rare diseases by the end of
2013.
Since the adoption of the Council Recommendation, RDUK has been actively ensuring that the UK’s health departments act on their obligation to develop a plan for rare diseases and we have been instrumental in engaging the rare disease community to shape the
content of the proposed plan.
From our members ALD Life: Highlighting the links between ALD and Addison’s Disease ALD Life is the main UK charity supporting patients and families affected by ALD and Adrenomyeloneuropathy (AMN). www.aldlife.org. ALD Life project managers Karen Harrison and Angela Kateley have recently embarked on a project, partially funded by the Mrs Smith and Mount Trust, to highlight the link between X- linked Adrenoleukodystrophy
(ALD) and Addison’s disease.
Karen’s father had Addison’s disease with symptoms of AMN; he was not diagnosed with either ALD or AMN and died at a young age from an adrenal crisis. Karen went on to have identical twin sons, and all was well until they were six years old, at which point one of the twins started to lose his eyesight and hearing. He was eventually diagnosed with X- linked Childhood Onset Cerebral ALD. He continued to deteriorate at an alarming rate, and within a year was blind, deaf, had no speech, was tube fed and wheelchair-bound. He died 18
months after diagnosis. His twin brother needed to have a bone marrow transplant (BMT) without delay, a procedure which can halt the progression of ALD if undertaken early on in the course of the disease. Even though his BMT was carried out within weeks of diagnosis he has continued to deteriorate, and now, at 17, is severely disabled. There are many success stories where BMT has been timely and the boys are now
well, with little or no disability.
Angela’s story is slightly different in that her father was diagnosed with Cerebral ALD aged 40 and died aged just 45. His brother in Canada had been diagnosed with Addison’s Disease several years prior and was then tested and was found to have AMN. Angela took the difficult decision to not have children, having seen the devastating
deterioration in her father.

Genetic Alliance UK Newsletter Autumn 2013
5
devolved administrations of NHS Scotland, NHS Wales and NHS Northern Ireland on developing and implementing the strategy for rare diseases and highly specialised
services.
Highly specialised services are provided to a smaller number of patients compared to specialised services; usually no more than 500 patients per year. For this reason they are typically best delivered nationally through a very small
number of centres of excellence.
RDAG will receive recommendations from Clinical Reference Groups set up by NHS England, and in addition will formulate its advice by calling on sources of sound evidence from outside the NHS, such as professional bodies and patient groups to create a coherent strategic plan. For more information on RDAG please visit: www.england.nhs.uk/ourwork/d-
com/rdag/
Centres of Excellence
We have previously mentioned that RDUK has been working on a project looking into Centres of Excellence. We are now at the final stages and our report 'Centres of Excellence for Rare Diseases' will be launched in
mid-October. The main aim of the report is to develop a broader understanding of what a Centre of Excellence should be and establish criteria under which a centre can be
classed as a Centre of Excellence.
Having examined the concept of a Centre of Excellence, it is apparent to RDUK that the absence of a concrete definition of a Centre of Excellence in the UK limits the value that the rare disease community and health services can gain from exploiting the concept. We believe it is vital that a definition be
agreed.
The criteria from the Department of Health in England make a useful starting point for this definition. They
recommend:
coordinated care for patients;
an adequate caseload for
clinicians’ expertise;
ensuring the centre is not
dependent on a single clinician;
that there are arrangements for transition from children’s to
adults’ services;
ensuring the centre is engaged with people with rare conditions;
and
keeping research active at the
centre of excellence.
ALD is a rare, terminal, x-linked degenerative metabolic disorder. In short it causes demyelination of the brain due to the accumulation of very long chain fatty acids in the blood which in turn attack the myelin sheath in the brain. The most common and serious form of the disease is childhood onset cerebral ALD,
affecting boys aged between 4 and 10 years.
AMN is the adult form of the disease and mainly affects the spinal cord, although in some cases it can also cause severe neurological damage. All forms of ALD and AMN will probably feature adrenal failure and it is often the first
symptom.
The primary aim of this project is to raise awareness of the studies which suggest that 60-80% of all boys, and 10-35% of adolescent or adult males, presenting with adrenal failure/
Addison’s Disease will, on testing, be found to have ALD.
ALD/AMN is an important cause of adrenal failure in males. Failure to carry out these further tests often results in missed or delayed diagnosis which can have catastrophic results. The window of opportunity for treatment is very small and so the patient or their relatives need to be treated quickly to avoid needlessly suffering the devastating consequences of this illness. The diagnosis does not just affect the patient with Addison’s; it has far reaching consequences for the wider family, and genetic counselling should be offered to ensure
that all affected males and carrier females are identified.
By the end of the project we will have compiled a complete database of all the Endocrinologists in the UK, with a sub database which will detail all those with a special interest in Adrenal problems. In doing so we hope this will ultimately result in saving lives. If you have a special interest in Adrenal problems or would like to know more about the project please contact either of the project officers by email:
[email protected] or [email protected].
Minesh Gokal, Fundraising Manager, ALD Life
Our findings have supported these criteria and suggest two additional areas for inclusion, these focus on education and training for medical professionals and international
networks of excellence.
We will use this report to influence policy in this area and push for the findings and recommendations to be recognised by the health departments in the development of the country specific implementation
plans. In particular we will:
campaign for stronger links between education providers
and Centres of Excellence; and
advocate for the establishment for international networks of excellence so that Centres of Excellence do not work in
isolation (where applicable).
The report will be available online from Monday October 14 2014. You can view this online at www.raredisease.org.uk or if you would like a hard copy, please
contact me.
Farhana Ali, Public Affairs Officer and Rare Disease UK Secretariat,
Karen
and her
son

Genetic Alliance UK Newsletter Autumn 2013
6
Thank you to everyone who came along to our annual conference and AGM on 10th July. It was great to see so many of you; to meet some new faces and to catch up with some of the more familiar ones. We had a great turn out this year with over 70 representatives from our member organisations attending alongside researchers, clinicians and industry representatives. The diversity of our attendees was encouraged by the
breadth of the talks on the day.
To cover all of the topics, we had a broad range of speakers from the Department of Health, NHS England, NICE, Public Health England as well as a speaker from
one of our members.
After a welcome from our Director, Alastair Kent, we opened the conference with the first session of the day on the subject of rare diseases and, more specifically, the progress that the rare disease plan is making in the
UK.
The UK Strategy for Rare Diseases
Titled, ‘how will the implementation of the rare disease plan and reorganisation of the NHS in England affect rare disease patients?’ this was our first session of the day. In order to tackle this subject from a number of directions we had Dr Colin Pavelin from the Department of Health, Kate Caston from NHS England and Meindert
Boyson from NICE.
Dr Pavelin opened the session by informing our audience of the likely impact of the implementation of the rare disease plan before handing over to Kate Caston. Kate explained how the changes to the NHS
and the new rare disease plan will affect the commissioning of specialised services. In order to try and reduce the ‘postcode lottery’ for patients, more services are being commissioned nationally to ensure
equity in services; no matter where a patient lives.
Meindert Boyson was the final speaker from our panel speaking about the effect that the changes in the NHS and the introduction of the rare disease plan will have on the appraisal of new treatments and technologies. We then opened the floor to questions from the audience and enjoyed a lively discussion for the rest of the session. If you would like to see our speakers’ slides from this session, or any other session from our conference, they are all available at
www.geneticalliance.org.uk/latest-events.htm.
Our RAPID project
The next talk of the day was a presentation of the findings from one of our projects; RAPID. Professor Lyn Chitty from University College London and our own Dr Celine Lewis presented the findings of their interviews with parents and parents to be about Non-Invasive Prenatal Testing. This is a new form of testing that offers the possibility of a diagnosis of conditions such as Down’s syndrome from a maternal blood sample early
in pregnancy without the risk of a miscarriage.
Before tests such as this become clinically available in the UK, it is crucial to conduct empirical research to understand public attitudes. It is important that patients’ views and experiences are recorded when new technology is being assessed to see if it is suitable to become clinically available. Genetic Alliance UK’s involvement in the project also illustrates our belief in making sure the patient voice is heard in decisions about cutting edge technology which may affect those affected by genetic conditions. This was the most popular talk of the day with our attendees who responded to our survey who all rated it as ‘good’ or ‘excellent’. You can find out more about the RAPID project on our project pages
www.geneticalliance.org.uk/projects/rapid.htm.
The all-England congenital abnormalities register
In the final session before lunch, Dr Jem Rashbass from Public Health England spoke about the new all-England congenital abnormalities register. This new register will collect data from across England on rare diseases. This will enable the health services to better target interventions for certain rare diseases and to coordinate treatment for the conditions more easily. The large
Genetic Alliance UK
Annual Conference and AGM 2013
From left to right: Meidert Boyson, Kate Caston and Dr Colin
Pavelin share a joke before their panel session

Genetic Alliance UK Newsletter Autumn 2013
7
amount of information gathered will also enable researchers to use the data to find out more about rare diseases which will potentially help develop new
treatments or therapies.
The new register may also offer patients the opportunity to rate the care that they receive from their specialist doctor. This will hopefully increase the quality of care for those affected by rare diseases. Dr Rashbass highlighted these points from the lessons that Public Health England had learnt from the all-England
cancer registry.
Our new trustees
After lunch, thoughts turned briefly to the year which has just passed with our Annual General Meeting (AGM). Unfortunately, our Chair Chris Friend was unable to attend the day but was re-elected as a trustee for the next few years, which meant that Joanie Dimavicius kindly volunteered to act as Chair for the meeting. Our Director Alastair Kent spoke about the achievements of Genetic Alliance UK over the past year which you can catch up with in our annual report at
www.geneticalliance.org.uk/annual-report.htm.
After this, four new trustees were elected to the Genetic Alliance UK trustee board. Ruth Abuzaid (Huntington’s Disease Association), Rebecca Griffiths (UKPIPS), Rae McNairney (PIDUK) and John Mills (Vasculitis UK). With the new elections we unfortunately had to say goodbye to Joanie Dimavicius, Professor Shirley Hodgson, Tessa
Homfrey and Liz Nelson.
What does PGD mean to patients?
Following the conclusion of the AGM, our Policy Analyst Nick Meade and Sarah Dennis from our member organisation the Cardiomyopathy Association talked about Genetic Alliance UK’s project on Preimplantation Genetic Diagnosis (PGD). Nick and Sarah spoke about the work that we have been doing to ensure the regulatory environment for PGD is both effective and
secure while also supporting applications for new licences to be granted for PGD to be available for
those affected by genetic conditions.
The talks highlighted the impact that a genetic condition can have on families and the potential benefits that PGD may offer to families should they wish to pursue it. We are currently finishing our latest work on PGD and will be launching a new section on our website describing the process, how it can be accessed and
including all of our work in the area soon.
Finally, Alastair Kent closed the day by summarising our work ahead for the coming year and the challenges which those affected by genetic conditions may face. As always, we will be working hard to ensure that our members’ voices are heard by health policy makers facing any decision with the potential to affect those
affected by genetic conditions.
As a part of this work, we are delighted to announce that Alastair Kent OBE has been appointed to the Rare Diseases Advisory Group (RDAG) along with Nick Sireau (AKU Society), Christine Collins (Huntington’s Disease Association of Northern Ireland) and Susie Gear. RDAG will make recommendations to NHS England and the devolved administrations of NHS Scotland, NHS Wales and NHS Northern Ireland (to be confirmed) on developing and implementing the strategy for rare diseases and highly specialised services. We look forward to being involved in and
helping to shape this work.
I’d like to thank everyone who attended our annual conference and AGM this year. If you have any suggestions as to what you’d like to see at the next conference or about any topics you’d like to hear about,
please let me know.
Julian Walker, Marketing and Communications
Officer, [email protected]
We had a great turn out of member representatives who got
to ask questions of our speakers
Nick Meade and Sarah Dennis pose before presenting our
work on Preimplantation Genetic Diagnosis

Genetic Alliance UK Newsletter Autumn 2013
8
Alström Syndrome UK (ASUK) became aware of the
possibility of getting an Alström service commissioned
by the NHS following a talk by Alastair Kent at our
Family Conference in 2005.
Alström Syndrome is a life – limiting disease which in my
two children’s case caused childhood blindness, hearing
loss, heart failure, diabetes type two, kidney failure,
bladder dysfunction and many associated problems.
Matthew died aged 25 following heart transplant
surgery in 2003 and Charlotte following heart and
kidney transplantation in 2010 aged 29.
I founded Alström Syndrome UK charity in 1998
following the late diagnosis of my two children,
Matthew was 18 and Charlotte was 15. They had years
of mis-diagnosis at my local hospital, before finally
being asked to attend Great Ormond Street Hospital as
a doctor was looking into their latest diagnosis. I had
studied Law at Exeter University as a mature student,
primarily because I was having to fight so many issues
for my children and fortunately also specialised in
Charity Law.
I informed the Consultant who made the diagnosis that I
wanted to start a charity for the condition and she
contacted 12 other families she knew with the condition
and invited them to our first family conference in 1998.
Seven families attended and it soon became clear that
even those with a diagnosis were not having all aspects
of the disease identified. The following year we invited
physicians who were
working with my own two
children from Torbay
Hospital to attend.
This was the beginning of
our multi-disciplinary
clinics. In a hotel in
Brixham, Devon,
audiology tests took
place in the bedrooms,
families gathered round
a cardiologist, an
endocrinologist and
dietician and ad hoc consultations took place wherever
they could find a spare room in the hotel. The unmet
needs of these families were clear as were the needs of
the physicians to see more patients, gain more
experience and learn more about the disease.
The family conference/clinic progressed on these lines
for a number of years. As our numbers grew it became
increasingly difficult for families to travel to Torbay and
back in a weekend. I was already in touch with
Birmingham Children’s Hospital and it was agreed that
we could use their facilities at the weekend of our
family conference. All was still on an ad hoc voluntary
basis with doctors giving freely of their time at the
weekends to examine our Alström patients and Alström
Syndrome UK charity organising and funding the family
conference and the clinic lists.
Following Alastair Kent’s talk, Torbay Hospital,
Birmingham Children’s Hospital and AS UK decided that
we would apply for NHS Commissioning to fund the
clinical service on a more professional basis. In 2006 the
NHS Commissioning Team for Highly Specialised
Services agreed to fund 4 clinics for children at the
Birmingham Children’s Hospital yearly and 4 adult
clinics at Torbay Hospital. Two outreach clinics in Leeds
were also arranged. However, the NHS said at that
time that they did not fund charities.
Fortunately my legal training equipped me with the
skills to challenge this decision and I set about tracking
the legal basis to do this. The COMPACT document,
signed by Tony Blair when Prime Minister, laid out the
principles of how the public sector should work with the
voluntary sector. On reading the document it became
clear that there were a number of breaches in our
dealings with the NHS. The NCVO had COMPACT
officers funded by the Big Lottery who took up our case.
When the breaches were pointed out to the NHS
Commissioners, AS UK was invited to meet with them.
The outcome was that we were to be funded as equal
partners with the two hospitals we worked with in
Alstrom Syndrome UK’s experience By Kay Parkinson, Founder
Editor’s note:
Thank you Kay for sharing
your story! We hope that, by
sharing the story, other
members can learn from
Alström Syndrome UK’s
experiences

Genetic Alliance UK Newsletter Autumn 2013
9
delivering the Alström clinical service that we had
developed.
The NHS Commissioned clinics have gone from strength to
strength since we started and our numbers have doubled
since we incorporated an Asian Mentoring Scheme after
the Alström gene was found to be present in a number of
families in the Leeds and Bradford area. In 2012 we
successfully moved the adult clinic from Torbay Hospital
to the brand new state of art Queen Elizabeth Hospital in
Birmingham. It had become clear that the needs of our
adults could not be met at a district hospital, and
although thankful to Torbay for their initial help with
setting up the clinics it was time to move on.
On the back of the success of the clinics AS UK applied
for and were successful in gaining a Big Lottery Fund
Medical and Scientific grant to develop research into the
condition through taking skin samples from consenting
patients and starting a research database. Cambridge
University partnered with AS UK and were commissioned
to generate pluripotent stem cells that will be
differentiated into cell types. Birmingham and Torbay
Hospitals were commissioned to take the skin samples
and develop a research database.
Six months prior to the completion of the grant when AS
UK were expecting to be able to review the database,
Torbay Hospital announced that AS UK could not have
access to it for ethical reasons. As we were not NHS
“employees” it was unethical for us to have access and
as our patient numbers were so small we would still be
able to recognise anonymised data. The fact that we
see un-anonymised patient information, as part of our
role as a partner in the NHS England, National
Specialised Commissioned Alström Clinical Service was
ignored. The fact that we owned the database was
ignored. This information announced at such a late
date in the project that it put the grant and AS UK into
jeopardy. If the Big Lottery Fund were to call back in
the grant AS UK would be ruined. Our members had
believed that when they consented to the database
that AS UK would, as owners of the database, have
access to it.
ASUK kept the Lottery closely informed of discussions
and an emergency meeting was held between
partners. The outcome was that the Database will
move to the Queen Elizabeth Hospital, Birmingham and
all patients will be re-consented to the database
explicitly stating that they allow AS UK access. AS UK,
will now add further consents to the form; allowing the
data to be shared, with EU and International
databases.
Alström Syndrome is an ultra-rare condition, the vast
majority of patients have been found through the
infrastructure and services that I have developed over
the years. I instigated, pioneered and fought for the
first Alström Syndrome multi-disciplinary clinics in the
UK and started the first research through the Big
Lottery Fund grant.
I hope the above information helps other groups be
more prepared for issues which can arise when
working with the NHS and the other groups avoid the
problems we encountered. Patient groups have patient
interests at heart - the solutions for rare diseases will
only come by all parties to their care bringing down
the barriers that prevent collaborative working.
With such a complex condition as Alström it is only the
patient groups, families and patients who have lived
with all the multiple manifestations of the disease and
managed them on a daily basis. We cannot “lock out”
their valuable experience and expertise. Patient
groups deserve and need better recognition.
Kay Parkinson, Founder, Alström Syndrome UK Mathew Parkinson (9-2-1978-11-5-2003) and Charlotte
Parkinson (11-4-1981- 29-4-2010). The picture was taken in
1998 shortly after diagnosis by Great Ormond Street
Hospital. We are flying to the USA- the only country at that
time with any knowledge of the disease. Local press took the
photo as we were about to depart.

Genetic Alliance UK Newsletter Autumn 2013
10
“Champions Of Hope” Lead World Pioneering Research A patient-led charity has won an international award for their ground-breaking research into the world’s first
genetic disease.
More than 110 years since the discovery of alkaptonuria (AKU), 13 European organisations have been recognised for their global research collaboration into the world’s first treatment for alkaptonuria (AKU)
by a 2013 RARE Champions of Hope award.
Working with 12 other organisations from across Europe, the AKU Society managed to secure funding from the European Commission for their clinical trials on the drug nitisinone. The research collaboration, named DevelopAKUre, brought together the patient organisations, the EU Commission and the company that owns the treatment, and is considered to be a “first”. They have now been recognised by a European award from the Global Genes Project, a worldwide non-profit
patient organisation.
For the first time in the UK, patients are able to play a leading role in clinical research for their disease, providing important patient insights in an area of work typically led by pharmaceutical companies. And the fruits will go far beyond the rare disease community, because the clinical trials will also improve understanding of osteoarthritis, which affects
approximately 8 million people in the UK.
The DevelopAKUre collaboration was chosen from over 200 nominations, winning one of only five awards available: the RARE Champions of Hope Award for Collaborations in Science. The awards are organised by the Global Genes Project, which recognises individuals and collaborations for their contributions to patient advocacy, scientific research and medical care. DevelopAKUre will receive the 2013 RARE Champions of Hope award at a gala event in Newport Beach,
California, USA on 21 September 2013.
Professor Jim Gallagher, from the University of Liverpool, will accept the award on behalf of DevelopAKUre. He said: “Our consortium is delighted with this RARE Champions of Hope award from Global Genes. International co-operation is vital in fighting rare diseases. In my view, it is an outstanding example of how fundamental research can be translated into
patient benefit.”
The award coincides with the end of the first of three clinical trials on nitisinone. If these trials are successful, the AKU Society will work with the other participating organisations with the objective of getting nitisinone
authorised as the world’s first treatment for AKU.
Yogesh Rathod, an AKU patient who is taking part in the clinical trials, said: "These trials have given us great hope. This treatment could completely change the lives of myself and many others affected by AKU. With the
first trial complete, we’re that one step closer to a cure.”
Jenni Thorburn, Online Communities Officer, AKU
Society
Genetic Alliance UK has been working closely with the panel set up by the Welsh Government to review the appraisal process for orphan and ultra orphan medicines in Wales. I presented at the panel’s first meeting to outline the difficulties that patients with rare conditions have been experiencing in Wales
gaining timely and equitable access to medicines.
Genetic Alliance UK also made a written submission to the panel outlining our position regarding the current medicines appraisal process which can be viewed here: www.geneticalliance.org.uk/
policycampaigns.htm.
The review group invited patients and patient organisation representatives to attend a patient engagement event in August. Genetic Alliance UK attended the workshop and was pleased to see many of our member organisations in attendance including We now await the recommendations that will be sent from the review group to the Health Minister, Mark
Drakeford in October.
In addition to the work around access to medicines in Wales, I have been working to establish a network of patients and families affected by rare conditions. Four events will be held across Wales during October
Access to working for specialised services in
Wales - would you like to get involved?

Genetic Alliance UK Newsletter Autumn 2013
11
It has been a lovely summer in Scotland and a very busy one too! Our work on access to new medicines continues and we were invited to contribute to the Scottish Government’s recent consultation on the issue. A written submission outlining our suggestions for improvements to the current process for accessing new medicines for rare diseases in Scotland was made, and I attended the Scottish Government’s stakeholder meeting alongside representatives of a number of patient organisations, health boards and pharmaceutical companies. We are eagerly awaiting the Scottish Government’s announcement on the outcome of this consultation, which is expected
in October.
The Cross Party Group on Rare Diseases has received formal approval by the Scottish Parliament’s Standards, Procedures and Public Appointments Committee and the first formal meeting took place on October 1st 2013. The topic for this meeting was the UK Strategy for Rare Disease and Alastair Kent joined us to talk about Rare Disease UK’s work. We were also joined by representatives from
the Scottish Government who gave
an overview of the work to implement a plan for rare diseases in Scotland. Meetings are open to all, and patient organisations that represent families affected by a rare disease and operate in Scotland are welcome to join as
members of the Cross Party Group.
I have been attending lots of interesting events over the summer too. I was very pleased to be asked to give a presentation on the work of Genetic Alliance UK in Scotland at the Tuberous Sclerosis Scottish Patient Day. It was a fabulous event and it was wonderful to hear of the work of the TSA and meet a number of the families that were there. I also exhibited at the Scottish Government’s Carers Strategy Learning and Sharing Event, to promote our partnership working
with The Carers Trust in Scotland.
In other exciting news, two new projects have begun in Scotland this summer. Our Supporting Patient Groups project, which has been running for almost two years, has received additional funding from the Scottish Government. The
project, which originally aimed to
help patients with rare conditions
start up patient groups where none existed, has now been extended. The Project can now assist UK patient organisations that may not have the resources to reach patients based in Scotland. For example, the project can help arrange patient information meetings or assist in promoting a particular patient
organisation in Scotland.
The second new project is research based and will look at the current service provision for Multiple Sclerosis in Scotland, and in particular, look at whether there is a need for a managed clinical network for the condition in Scotland. In addition to desk based research, I will be visiting a number of Multiple Sclerosis clinics, meeting patients and clinicians and working closely with patient organisations
representing MS patients.
Both our new projects will run for one year and if you would like to find out more about them, or any of the work going on in Scotland,
please contact me.
Natalie Frankish, Development Officer for Scotland
bringing together patients, families and patient organisation representatives to investigate the current service provision for specialised services. If you would
like to find out more about the events, please visit
www.geneticalliance.org.uk/e-updates/august2013.htm#Policy_2. Please contact me if you
would like to attend.
The Human Transplantation Wales Act received Royal Ascent on 10 September. This law will come fully into effect on 1st December 2015. The Act introduces a soft opt-out system for consent to deceased organ and tissue donation in Wales from 2015. Until then, the current opt-in system will remain in place. The aim of the Act is to increase the number of organs and tissues
available for transplant.
For more details on how this may affect you, please
visit the Welsh Government’s website www.wales.gov.uk/topics/health/nhswales/
majorhealth/organ
I have also been busy attending the Rare Disease Stakeholder Forum and Workshop, The Action Duchenne Welsh Parliamentary Lobby Event, the Cross Party Group on Muscular Dystrophy and an event held by the Cystic Fibrosis Trust to raise awareness of transplantation. Our Director, Alastair Kent, and I met with the Deputy Chief Medical Officer, Chris Jones regarding moving forward the Wales rare disease
implementation plan.
I have recently moved offices and you can find my new
address and phone number on our website.
Emma Hughes, Development Officer for Wales
New projects and opportunities to establish
patient support groups in Scotland

Genetic Alliance UK Newsletter Autumn 2013
12
Opinions in this publication are not necessarily
those of Genetic Alliance UK. Articles accurate at time of writing. Genetic Alliance UK is a Charity registered in England and Wales (no. 1114195) and in
Scotland (no. SC039299). Company limited by guarantee (no. 05772999).
It’s been an exciting few months for SWAN UK.
We were delighted to be selected out of 900 entries as one of the 49 finalists for the National Lottery Awards, eventually coming 4th in the Best Health Project category. As part of the voting process each project was required to submit a case study video. The SWAN UK case study was selected as one of three projects to be professionally filmed and broadcast on the National
Lottery Break The Safe programme.
This was a fantastic opportunity to help raise the profile of the SWAN UK project and the issues faced by the families we support. You can watch the film on the National Lottery Good Causes YouTube channel
http://youtu.be/QuBA5fPItxo.
The summer months saw a number of SWAN UK events occurring, including over 50 families attending fundays in Maidenhead, Leeds and Cannock. The fundays are an important part of the SWAN UK calendar providing not only a chance for families to get together and cement the friendships made online, but they also provide an opportunity for an enjoyable day out that all members of the family can enjoy. It’s great to see parents chatting and all the children having
fun and making new
friends. Everyone had a great time
and we are hoping to add more around the UK next year. Over 900 hundred parents have now made contact with SWAN UK and our online community continues to thrive. There are over 700 members of our main Facebook group and we have recently created two new age based groups for parents of children and young people aged 10+ and 16+ to discuss
issues affecting them and share information.
On the 26th of November we will holding our first information event on undiagnosed genetic conditions. Hosted at Great Ormond Street Hospital in partnership with the clinical genetics department the event aims to bring together parent carers of undiagnosed genetic conditions and interested professionals to raise awareness and share information. Planned talks will include ‘why some children are undiagnosed’, ‘genetic testing and why it can take so long’ and ‘raising an undiagnosed child, a parents perspective’. For more information on attending the event please contact
Lauren Roberts, SWAN UK Coordinator,
An exciting summer for SWAN UK
Families and Buzz Lightyear at the Maidenhead family funday
Trying out
the new
bikes &
trikes at
the funday