GASTROESOPHAGEAL REFLUX DISEASE
-
Upload
ora-copeland -
Category
Documents
-
view
65 -
download
0
description
Transcript of GASTROESOPHAGEAL REFLUX DISEASE
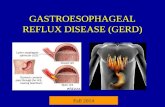
GASTROESOPHAGEAL REFLUX DISEASE
Tiberiu Hershcovici, MDDirector, Gastrointestinal Motility Lab
Hadassah University Hospital
DEFINITION • According to the Montreal International
Consensus Group1: GERD is defined as a condition that develops when the reflux of stomach contents causes troublesome reflux-associated symptoms.
• While GERD is commonly diagnosed in clinical practice based on symptoms alone, it has been demonstrated that esophageal symptoms are not stimulus specific and thus heartburn could result from non-reflux related stimuli.
Vakil N, et al. The American Journal of Gastroenterology 2006;101(8):1900-20
CLASSIFICATION
• Patients with GERD are further classified based on upper endoscopy results, into:• erosive esophagitis, if visible mucosal breaks in the distal
esophagus are present- 20-30% • nonerosive reflux disease (NERD), if the mucosal breaks
are absent- 60-70%• Esophageal complications of erosive esophagitis are:
• ulceration • stricture • Barrett’s esophagus • adenocarcinoma of the esophagus.
EPIDEMIOLOGY
• Population-based studies suggest that GERD is a common condition with a prevalence of 10–30% in Western Europe and North America.
• GERD is less commonly seen in the Asia-Pacific region.
• The prevalence of GERD and GERD-related disorders has been steadily increasing in the US, Western Europe, Australia and Asia.
• An opposing trend time was observed between 1970 and 1995 in the prevalence of peptic ulcer disease and GERD.
• The rates of peptic ulcer and gastric cancer fell while at the same time the rates of GERD and esophageal adenocarcinoma rose significantly.
EPIDEMIOLOGY
CAUSES AND RISKS FACTORS
• Age: prevalence of GERD increases with age, older patients are more likely to develop less symptomatic but more severe disease
• Cigarette smoking • Alcohol • Coffee • High fat diet• Food products such as chocolate, peppermint, citrus
juices but not carbonated beverages• Medications: narcotics, calcium channel blockers etc.
GERD -OBESITY
• Obesity is associated with:– 1.5- 2-fold increase risk for GERD symptoms and erosive
esophagitis– 2- 2.5-fold increase risk for esophageal adenocarcinoma
• Mechanisms proposed to explain the close relationship between increased BMI and GERD include:– increased gastroesophageal pressure gradient– increased prevalence of hiatal hernia– increased prevalence of transient lower esophageal
sphincter relaxations (TLESR)
RELATIONSHIP BETWEEN HELICOBACTER PYLORI AND GERD
• Some studies suggested that H. pylori infection conferred protection from GERD and its eradication was associated with an increased risk of developing GERD.
• A more recent meta analysis of twelve trials revealed no association between H. pylori eradication in patients with duodenal ulcer and: – development of erosive esophagitis, – appearance of new symptomatic GERD, – worsening of symptoms in patients with pre-existing GERD.
Laine L, et al. The American Journal of Gastroenterology 2002;97(12):2992-7.
DYSFUNCTION OF THE LES
• GER occurs predominantly during transient lower esophageal sphincter relaxation (TLESR),
• TLESR is a spontaneous (not preceded by a swallow), prolonged relaxation of the LES (>10 sec). It is triggered primarily by gastric fundic relaxation and mediated by a vago-vagal reflex.
• Although recent trials found no increased rate of TLESR’s in patients with GERD, TLESR was more likely to be associated with an acid reflux event in patients with GERD as compared to healthy controls.
• This may be caused by increased compliance of the esophago-gastric junction in GERD patients.
HIATAL HERNIA• The presence of a hiatal hernia, particularly if it is large (≥5
cm) is associated with increased severity of GERD . • The prevalence of hiatal hernia increases with the severity of
esophageal mucosal involvement. – 20-30% in NERD patients– 95% in patients with long segment Barrett’s esophagus
• Displacement of LES from the crural diaphragm into the chest:– reduces LES basal pressure– loss of the intra-abdominal LES segment– reduced threshold for TLESR in response to gastric distension
PATHOGENESIS –OTHER FACTORS
• Esophageal mucosal defense mechanisms• Esophageal clearance – peristaltic dysfunction• Gastric acid secretion • Duodenogastroesophageal (bile) reflux• Acid pocket –related to hiatal hernia• Gastric dysmotility
CLINICAL PRESENTATION-TYPICAL SYMPTOMS
• Heartburn: a sensation of discomfort or burning behind the sternum rising up to the neck, made worse after meals and eased by antacids.
• Acid Regurgitation: the perception of flow of refluxed gastric content into the mouth or hypopharynx.
CLINICAL PRESENTATION-ATYPICAL SYMPTOMS
• Angina-like chest pain-non cardiac chest pain• Globus sensation• Chronic cough• Hoarseness • Asthma
CLINICAL PRESENTATION
• GERD symptom frequency or severity does not correlate with the extent of esophageal mucosal involvement in patients with erosive esophagitis.
• Heartburn severity and intensity are similar in patients with erosive esophagitis and NERD.
• In the elderly patient with GERD, heartburn and acid regurgitation are less frequent than in younger subjects.
• In contrast, atypical symptoms such as vomiting, anorexia, dysphagia, respiratory symptoms, belching, dyspepsia, hoarseness, and postprandial fullness are more common presentations in elderly.
DIAGNOSTIC METHODS
• Clinical evaluation• The proton pump inhibitor (PPI) test• Upper endoscopy • Ambulatory 24-hour esophageal pH monitoring
DIAGNOSTIC METHODS
• Clinical evaluation• The proton pump inhibitor (PPI) test:
– a short course (1–4 weeks) of high-dose PPI given twice daily for the diagnosis of GERD in patients with typical, atypical or extraesophageal manifestations of GERD.
– If symptoms disappear with therapy and then return when medication is stopped, GERD can be assumed and no further testing is required.
– Sensitivity: from 66% to 89%, – Specificity: from 35% to 73%.
UPPER ENDOSCOPY
• The gold standard procedure for diagnosing erosive esophagitis, GERD complications, and Barrett’s esophagus.
• Allows an assessment of the degree of esophageal mucosal injury, and tissue sampling can be performed if necessary.
• Sensitivity: 30–50% in patients with typical symptoms of GERD, as most patients with GERD have NERD.
• Specificity: 9095%.
• Allows assessment of :– 24-hour esophageal acid exposure – the temporal relationship between patient symptoms
and acid reflux events
AMBULATORY 24-HOUR ESOPHAGEAL pH MONITORING
TREATMENT-GOALS
• Adequate relief of GERD symptoms• Healing of erosive esophagitis if present• Maintenance of mucosal healing• Improvement of quality of life
LIFESTYLE MODIFICATIONS
• Adequate for patients with mild and infrequent reflux symptoms
• Weight loss• Cessation of smoking • Elevation of head of the bed • Avoidance of aggravating foods
PROTON PUMP INHIBITORS
• For patients with erosive esophagitis :effective control of reflux symptoms (77%) and a high rate of healing of esophagitis (84%).
• The proportion of NERD patients responding to a standard dose of PPI is approximately 2030% lower than in patients with erosive esophagitis.
• A once-daily morning dosing of PPI, half an hour before a meal, is generally the most appropriate initial therapy, but may fail in up to 30% of patients.
HISTAMINE TYPE 2 RECEPTOR ANTAGONISTS
• Standard doses have been proven to be effective in controlling symptoms and in healing mild to moderate erosive esophagitis.
• Tachyphylaxis develops quickly with H2RAs, limiting their regular use in clinical practice.
• The main appeal of H2RAs is their rapid effect on GERD symptoms, unsurpassed by any of the currently available PPIs.
• Nighttime use for refractory symptoms-currently unproven
TLESR REDUCERS
• Gamma-aminobutyric acid B (GABAB ) receptor agonists:– Baclofen– Arbaclofen placarbil– Lesogaberan
• Metabotropic glutamate receptor 5 (mGluR5) antagonists– ADX10059
PROMOTILITY AND PROKINETIC DRUGS
• May improve gastroesophageal reflux by:– increasing LES basal pressure– restoring esophageal peristalsis– facilitating gastric emptying
• The benefit of these compounds in controlling heartburn and in healing erosive esophagitis has been very modest, primarily because of lack of effect on TLESR.
ANTIREFLUX SURGERY
• Laparoscopic Nissen fundoplication remains the most commonly performed operation and consists of a 360° wrap of the gastric fundus around the distal esophagus
• Results in augmentation of LES basal pressure and a decrease in the rate of TLESR.
• Relieves reflux symptoms and heals erosive esophagitis.
• However: Barrett’s esophagus does not regress.
CLINICAL STRATEGIES• The step-up approach initiates patients on the least
effective antireflux modality and upgrades treatment if satisfactory control of symptoms is not achieved.
• The step-down approach initiates patients on the most potent antireflux modality and downgrades patients to a therapeutic modality that still controls their symptoms effectively.
• The step-in approach initiates and maintains patients on the most potent antireflux modality. It is the most popular therapeutic strategy in clinical practice.
• On-demand or intermittent PPI therapy: in patients with NERD and potentially in those with mild erosive esophagitis.
REFRACTORY GERD
• Patients who failed to obtain satisfactory symptomatic response after a course of standard-dose PPI.
• Any attempt to narrow the definition of refractory GERD might exclude many true sufferers
The PPI Failure DilemmasWhat Constitutes PPI Failure?
• Failure of PPI once a day
– No GERD indications for PPI twice daily– Drug development– Third-party payers and institutions
• Failure of PPI twice daily– Clinically relevant
• Symptoms cutoff Complete Partial
The Reported Rate of Symptomatic Failure in Therapeutic Trials of GERD Patients
PPI Failure
Nonerosive reflux disease
40%–50%
Erosive esophagitis
25%–30%
Barrett’s esophagus
20%
• Psychological comorbidity • Compliance
• Improper dosing time
• Weakly acidic reflux• Duodenogastroesophageal reflux• Residual acid reflux
• Delayed gastric emptying
• Concomitant functional bowel disorder
• Reduced PPI bioavailability• Rapid PPI metabolism• PPI resistance• Others
• Functional heartburn (esophageal hypersensitivity)
• Eosinophilic esophagitis (?)
Fass & Sifrim. Gut 2009;58:295-309
Putative Underlying Mechanisms for PPI Failure
• Psychological comorbidity • Compliance
• Improper dosing time
• Weakly acidic reflux• Duodenogastroesophageal reflux• Residual acid reflux
• Delayed gastric emptying
• Concomitant functional bowel disorder
• Reduced PPI bioavailability• Rapid PPI metabolism• PPI resistance• Others
• Functional heartburn (esophageal hypersensitivity)
• Eosinophilic esophagitis (?)
Fass & Sifrim. Gut 2009;58:295-309
Putative Underlying Mechanisms for PPI Failure
Distribution of Adherence to Proton Pump Inhibitor Treatment Over Time
Van Soest et al. Aliment Pharmacol Ther 2006;24:377-385)
Suboptimal Proton Pump Inhibitor Dosingin PPI Failure Patients
38.9
29.6 27.8
3.7
0
10
20
30
40
50
% o
f pat
ient
s <60 minutes before meals
After meals
At bedtime
As needed
N = 100
Gunaratnam et al. Aliment Pharmacol Ther 2006;23(10):1473-1477
• Psychological comorbidity • Compliance
• Improper dosing time
• Weakly acidic reflux• Duodenogastroesophageal reflux• Residual acid reflux
• Delayed gastric emptying
• Concomitant functional bowel disorder
• Reduced PPI bioavailability• Rapid PPI metabolism• PPI resistance• Others
• Functional heartburn (esophageal hypersensitivity)
• Eosinophilic esophagitis (?)
Fass & Sifrim. Gut 2009;58:295-309
The Persistent Reflux Hypothesis
Terms You Need to Know
Acidic Reflux – Reflux pH <4
Nonacidic reflux – Reflux pH 4 Weakly acidic reflux – 4 reflux pH <7 Neutral reflux – Reflux pH = 7 Alkaline reflux – Reflux pH > 7
How Common is Residual Acid Reflux in Patients Who
Failed PPI Once or Twice Daily?
31 30
7
1
0
5
10
15
20
25
30
35
Typical Extraesophageal
% A
bn
orm
al
QD
BID
Charbel et al. Am J Gastroenterol 2005;100(2):283-289.
N = 79 56 N = 40 75
Results of Combined pH and Bilitec Monitoring in Symptomatic GERD Patients While on PPI
Therapy
Karamanolis et al. Dig Dis Sci 2008;53:2387-2393
Acid refluxBile refluxMixed refluxNo pathological reflux
N=184
33% 40%
5%
22%
PPI once daily (2 months)
Failure
Switch to another PPI (2 months)
PPI twice daily (am &pm) for 2 months
Review proper PPI dosingtime and compliance
Failure
Failure
Failure
Pain modulatorsTricyclics
SSRIsTrazodone
Review againPPI dosing timeand compliance
TLESR Reducers Pain modulators
Antireflux surgery
Esophageal impedance + pH
Negative Positive for acid reflux
Positive forweakly acidic reflux
Failure
Hershcovici and Fass. Best Prac Res Clin Gastroenterol (in press)
H2RA qhsTLESR reducersPain modulators
Upper endoscopy
Treat mucosal findings
Alarm symptoms