Functional and Aesthetic Endpoints in Orthognathic Surgery
-
Upload
maxisurgeon -
Category
Documents
-
view
718 -
download
3
Transcript of Functional and Aesthetic Endpoints in Orthognathic Surgery

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
Functional and Aesthetic Endpointsin Orthognathic Surgery
M. E. Elsalanty, MD, PhD,* David G. Genecov, MD, FACS, FAAP,1 J. S. Genecov, JS, DDS, MSD*
Dallas, Texas, USA
Although facial deformity can accurately bedescribed and classified, the treatment goal canbe more difficult to define. Functional and estheticendpoints calibrated to a set of normal facial pro-portionsmay achieve a ‘‘normal’’ face but one that isnot necessarily beautiful. Results of orthognathicsurgery can dramatically be improved by addingan aesthetic concept to the surgical plan. We canachieve a face with both stable occlusion and abeautiful look each time. Additional soft tissueprocedures may be required to perfect the finalbalance and harmony of the face.
Key Words: Functional, aesthetic, endpoints, orthog-nathic, surgery
EVOLUTION OF ORTHOGNATHIC SURGERY
Orthognathic surgery is defined as surgical manip-ulation of the facial skeletal elements to restore
proper anatomic and functional relationships. Overthe last 150 years, several prominent general sur-geons, dentists, oral and maxillofacial surgeons, plasticsurgeons, otolaryngologists, and orthodontists havedeveloped this specialty into what it has become today.
The first reported orthognathic procedure wasperformed by Hullihen in 1849.1 It involved a wedgeostectomy to correct mandibular alveolar protrusion.During the late 19th and early 20th centuries, severaltechniques were introduced, mainly for treatment ofmandibular prognathism. Surgical procedures weretechnically and conceptually simple, but the resultswere less than satisfactory and carried a highincidence of complications and relapse. However, it
was this early that the need for cooperation betweensurgeons and orthodontists was emphasized,2 whenthe orthodontist E. H. Angle and the Surgeon V. P.Blair described the mandibular body ostectomy forthe treatment of mandibular protrusion. Blair2
classified jaw deformities into mandibular progna-thism, mandibular retrognathism, alveolar protrusion,and open bite, whereas it was Angle3 who intro-duced the standard classification of jaw relations intonormal occlusion and class I, II, and III malocclusion.
During the 1950s and 1960s, orthognathicsurgery evolved rapidly with the introduction ofmandibular sagittal split and LeFort I osteotomiesand other techniques that dramatically improved thetreatment results, both in the short and long term.Orthognathic surgery became a real specialty, withits beacon at the Obwegeser’s unit in Switzerland.At about the same time period, craniofacial surgerywas born in France at the hands of Paul Tessier.4Y6
In the late 1960s, the concept of rigid internalfixation of the craniofacial bones was introduced bythe AO group in Switzerland. This provided aneasier and more efficient stabilization method forexisting osteotomies and paved the way for theinnovation of new ones. The use of rigid internalfixation also eliminated the postoperative need forlengthy, inconvenient, and often hazardous inter-maxillary wire fixation.
Another important development that shaped thefuture of orthognathic surgery specifically and bonereconstruction in general was the introduction ofefficient bone substitutes and bone augmentingfactors. Bone inducing factors have been extensivelyinvestigated in promoting dental implant osseo-integration,7Y12 bone regeneration in segmentaldefects,13Y18 and recently in augmenting bone regen-eration produced by distraction osteogenesis.19Y24 Ofthese factors, the bone morphogenic protein family(BMP) appears to have the most promising clinicalapplications.25Y27
DECISION-MAKING IN ORTHOGNATHIC SURGERY
S ince their inception, the focus of orthognathicprocedures has been to achieve ideal dental
725
From the *Baylor College of Dentistry, Texas A&M UniversitySystem Health Science Center; and 1International CraniofacialInstitute, Cleft Lip and Palate Treatment Center, Medical City,Dallas, Texas.
Address correspondence and reprint requests to Dr. David G.Genecov, International Craniofacial Institute, Cleft Lip and PalateTreatment Center, 7777 Forest Lane, Suite C717, Dallas, TX 75230;E-mail: [email protected]

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
occlusion through correction of underlying skeletaldisharmony.2 Dentofacial deformities have beendefined and understood in terms of deviations in thedental or skeletal relationships from a ‘‘normal’’ setupthat was largely arbitrarily defined.28 Orthognathicsurgery has primarily been indicated whenever thedeviation in skeletal relations became severe enough tobe functionally or esthetically handicapping28,29 andcould not be resolved by dental procedures. It waswidely believed that whenever the underlying skeletaland dental deformities were corrected, this woulduproot the etiology of any soft tissue disharmony, andfacial esthetics would be achieved in consequence.
In any case of dentofacial deformity, correctingthe underlying skeletal problem has been theprimary goal of the treatment plan. The prevailingdogma, the Angle paradigm, stated that achievingperfect dental alignment and temporomandibularjoint function would bring about facial harmony.3,30
Therefore, soft tissue procedures were rarely incor-porated into the treatment planning, which wasdirected primarily by cephalometric measurementsand dental cast maneuvering.
However, perfect intermaxillary relation did notnecessarily translate into facial harmony,31,32 andseveral studies in the 1980s have shed doubts on thevalidity of using cephalometric analysis of thecraniofacial skeleton as a basis for treatment.33Y35 Ithas been shown that correcting the skeletal deformityuntil a certain ‘‘ideal’’ cephalometric relation wasachieved did not achieve consistent soft tissueresults.33 Moreover, if the soft tissue parameters areignored, skeletal correction may even have detri-mental effects on the facial appearance. For example,maxillary impaction may improve incisor display butcontribute to early aging of the face, especially whenthe upper lip increases in length with age. A maxillaryadvancement and widening in cases of maxillarydeficiency may produce an excellent occlusion butwith a flat or a denture-looking smile.
Surprisingly enough, this revelation was firstarticulated by Blair2 himself when he declared thattargeting the ideal occlusion rarely produced the bestfacial results. A century later, it became evident thatthe facial soft tissue cannot be considered simply as a‘‘latex glove’’ that takes the shape of the hand thatwears it. Indeed, the soft tissue is the envelope of theskeleton; however, it has its own variables that areindependent enough to confound the results of anytreatment that is solely based on skeletal parameters.Therefore, because it is the facial outlook that definessuccess or failure, at least from the patient’s perspec-tive, it should be the starting point for treatment plan-ning as well (Fig 1).
Advances in imaging technology and the intro-duction of computerized cephalometric analysis andfacial soft tissue analysis software have made itpossible to predict the outcome of certain orthog-nathic procedures from a soft tissue perspective. Ithas also become possible to specify the desirable softtissue results and design the skeletal and dentalprocedures to achieve them.36 It appears it will be the‘‘facial’’ component in a ‘‘dentofacial’’ deformity thatdictates the treatment plan in the 21st century.36Y38
The treatment goal of this new ‘‘soft tissueparadigm’’ is to achieve normal soft tissue proportionwhile maintaining optimal functional, even if lessthan ideal, occlusion.39 Treatment planning is basedprimarily on clinical evaluation of the facial soft tissueproportions, keeping in mind the limitations of softtissue adaptation to skeletal changes. Soft tissuelimitations involve the proportions of facial features,the amount of pressure that the lips and cheeks exerton the teeth, the thickness and integrity of facial softtissues, the stresses created by the attached muscles,and the patterns of soft tissue kinetics during jawmovements and facial expression.
Classically, several factors help indicate the needfor a specific orthognathic procedure. These includeunaesthetic facial proportions or interdental relations,temporomandibular joint dysfunction, impaired mas-tication, compromised airway, and difficulty inmaintaining oral hygiene because of deformity.40 Itis also essential to identify the patient’s needs andexpectations regarding the treatment outcome. Dis-cussing the treatment plan with the patient and familyis emphasized now more than ever. This shouldinvolve understanding and addressing the reason thatprompted the patient to seek treatment, which maynot necessarily be what the physician believes is themain problem. Also, the treatment plan should beexplained in detail to the patient, emphasizing therational for alternative approaches, possible compli-cations and limitations to each technique, and ways tomanage these. The most important piece of informa-tion that the patient should receive as accurately aspossible is what to expect in terms of facial outlook atthe end of treatment. Defining the endpoint from thestart is key to patient satisfaction with the outcome,which is a major determinant of success in this game.
The decision to use a specific treatment methoddepends on many factors. Purely dental problemswith no underlying skeletal problem can be con-trolled by orthodontics alone. However, if thedeformity is so severe that it cannot be corrected byorthodontic treatment or camouflage, then growthmodification, if the patient still has significant growthto come, or surgery, if not enough growth is expected,
THE JOURNAL OF CRANIOFACIAL SURGERY / VOLUME 18, NUMBER 4 July 2007
726

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
will be needed. The underlying skeletal deformityand its pathogenesis, stage of patient growth anddevelopment, condition of the soft tissues, and thepatient’s needs and expectations will help decide howthe treatment plan will be set. Again, the treatmentgoal will be facial soft tissue harmony, healthyperiodontium and TMJ, and functional occlusion.
Generally, for a young patient before or duringthe adolescent growth spurt, growth modificationtechniques are tried first. The idea is to change thepattern of growth to slow down, stop, or reverse theprogress of deformity. Although the amount of gaincan only be within a few millimeters, this can be asufficient correction in some patients. Even if thecondition requires larger skeletal movements,growth modification can assist in improving thecondition so that only an orthodontic or surgicalcamouflage procedure are required when growthstops, rather than orthognathic surgery.
Some deformities, such as mandibular progna-thism, do not respond well to growth modification
techniques.39 Furthermore, in severe deformities,treatment should be continued until no furthergrowth is anticipated; otherwise, relapse is likely tooccur. In maxillary deficiency, treatment should bestarted before the age of 8 to be effective.41,42
If the patient does not have enough remaininggrowth to allow for an effective growth modification,orthognathic surgery is still not the only answer.Another valid option is to correct the obvious featuresof the deformity without interfering with the under-lying deformity itself. The decision to ‘‘camouflage’’ adeformity rather than address its skeletal aspect maybe taken because the patient prefers this over moreaggressive surgical procedures. In any case, the simu-lated outcome should be visualized for the patientthrough computer simulation, with thorough empha-sis put on the limitations of such treatment.
Orthodontic camouflage can have satisfactoryresults by itself in mild anteroposterior jaw discre-pancy with dental crowding of less than 6 mm.However, it is not adequate in patients with increased
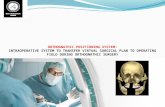
Fig 1 Seventeen-year-old female with maxillary deficiency. (A to E) Before treatment. (F to K) After treatment. Satisfactoryresults involved correction of occlusion and soft tissue projection.
FUNCTIONAL AND AESTHETIC ENDPOINTS / Elsalanty et al
727

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
facial height or when the deformity involves atransverse skeletal component.43
An example of combined orthodontic andsurgical camouflage is the retraction of protrusivemaxillary incisors with or without anterior move-ment of mandibular incisors in the treatment of aclass II deformity. This can be accompanied orfollowed by chin augmentation or rhinoplasty toachieve facial harmony. If satisfactory results cannotbe achieved by surgical and orthodontic camouflage,orthognathic surgery is the only remaining option.
Orthognathic surgery directly addresses theunderlying skeletal deformity. Treatment is stagedso that the dental arches are orthodontically pre-pared before surgery; then, surgery is performedto correct the skeletal deformity, followed by post-surgical orthodontic finish. Treatment planningshould be based on integrated soft tissue andcephalometric prediction. After presurgical ortho-dontic preparation, both the soft tissue and cephalo-metric parameters should be reevaluated. Thedesired skeletal changes are outlined on the cepha-lometry, and the soft tissue effects are predictedusing image analysis software. Then, the surgery issimulated on the patient’s updated models to verifythe feasibility and accuracy of the cephalometricplanning and to create the occlusal splints accord-ingly. Occlusal splints will be used to guide theinterdental position at each stage of the surgery.
CURRENT INDICATIONS FOR
ORTHOGNATHIC SURGERY
Dentofacial deformities can be classified accord-ing to the plane(s) through which correction is
needed:
1. Mandibular:
a. Anteroposterior deficiency, producing a class IImalocclusion
b. Anteroposterior excess, producing a class IIImalocclusion
c. Vertical ramus excess or shorteningd. Anterior vertical excess or shorteninge. Transverse narrowing or widening of the
mandibular archf. Asymmetric vertical height of the mandibular
ramus, condyle, or body.
2. Maxillary:
a. Anteroposterior deficiency, producing a class IIImalocclusion
b. Anteroposterior excess, producing a class IImalocclusion
c. Vertical maxillary excessd. Vertical maxillary shorteninge. Horizontal narrowing or widening of the max-
illary archf. Asymmetric vertical height of the maxilla.
A patient with a dentofacial deformity will mostoften present with a combination of some of theabove-mentioned skeletal deviations, producingclass II or III malocclusion, anterior open bite, crossbite, occlusal cant, inappropriate incisor display,unaesthetic smile, disproportionate middle or lowerfacial height, or gross facial disharmony. The focus ofthe clinical assessment should be the impact of theskeletal deviations on the facial soft tissue featuresand not the actual skeletal measurements.
ORTHODONTIC PREPARATION FOR
ORTHOGNATHIC SURGERY
Preorthodontic Treatment
Orthognathic surgery is an elective procedure andshould not expose the patient to any unneces-
sary risk. Therefore, the patient’s general conditionshould be assessed to exclude any cardiac, pulmon-ary, hepatic, renal, or psychological contraindicationfor surgery. Moreover, pathologic conditions andmedications that affect bone healing and oral healthhave to be addressed. The patient’s nutritional statusshould be appropriate for surgery, and he/sheshould be advised to stop smoking for at least 2months before surgery.
Dental caries should be controlled before startingorthodontic and surgical treatment. If possible, it ispreferable to retain the natural crown and delay itsrestoration until after the deformity correction. How-ever, if dental extraction or restoration is absolutelyneeded, temporary restorations should be used, withdelay of the application of permanent restorationsuntil after the end of postsurgical orthodontics.
A healthy periodontium should be establishedbefore treatment. It may be necessary to perform agingival graft before orthodontics to cover an areaexposed by gingival recession. However, if boneresorption is evident or if pockets exist, every effortshould be made to restore the teeth and supportingperiodontium to optimum health. After deformitytreatment, the periodontium should be reassessed,and guided bone regeneration techniques can beused to address any remaining pockets. Oral hygieneshould be thoroughly maintained throughout thetreatment period.39,44
THE JOURNAL OF CRANIOFACIAL SURGERY / VOLUME 18, NUMBER 4 July 2007
728

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
PRESURGICAL ORTHODONTIC TREATMENT
The goal of presurgical orthodontic procedures isto prepare the teeth for the skeletal changes that
will occur during surgery, with no regard for thepresurgical dental occlusion. In fact, presurgicalorthodontic typically reverses any camouflage ordental compensation that may exist to optimize theskeletal movement that can be achieved duringsurgery. This would cause the deformity to looktemporarily worse during the presurgical treatmentperiod. The extent and duration of preparatoryorthodontic treatment is case-dependant, varyingfrom a few days up to 18 months.
One aim of presurgical orthodontic treatment isto restore the proper curvature of the occlusal plane(curve of Spee). Patients with facial deformitiescommonly have accentuated or reversed curve,necessitating vertical height adjustment. In general,surgery is the best way to induce vertical facialchanges; however, the relative vertical and horizon-tal position of the incisors should be establishedbefore surgery. To establish the desired verticalposition of the incisors within an acceptable curveof Spee, some presurgical leveling may be requiredby selective extrusion and intrusion of teeth.
Intuitively, we can see that extrusion would bemore appropriate in cases where facial height needsto be increased and vice versa. If segmental surgery isplanned for a severe deformity, the teeth should beleveled within each segment so that arch alignment isachieved after surgical segmentation.44 In any case,finalizing the alignment should be delayed to thepostsurgical phase. Although intrusion must beperformed before or during surgery, extrusion isbetter achieved after surgery.44
Another aim of preparatory orthodontics isadjusting the horizontal incisor position that willguide the anteroposterior positioning of the jawsduring surgery. Dental extraction can be necessary tocreate spaces that can be partially used for adjustingthe incisor position while leaving enough room forthe planned interdental osteotomies.
Arch alignment, incisor position, and verticalleveling of the teeth should be compatible with theplanned surgical positioning of the jaw bones.Extrusion or intrusion of teeth to restore verticalleveling should be decided on the basis of thepatient’s facial height. It should be noted thatorthodontic treatment will have to be continuedafter surgery; therefore, it is a waste of both time andenergy to try to achieve perfect dental relationsbefore surgery. Furthermore, it is inefficient toattempt to orthodontically achieve changes that can
be more easily achieved by the planned surgicalprocedure. However, it is advisable to perform asmuch presurgical orthodontic finishing as possible tolessen the amount needed after surgery and thusenhance postsurgical stability.
FUNCTIONAL SURGICAL ENDPOINTS
Skeletal modification carried out during surgery aimsat influencing the facial soft tissue outline to achieve
attractive facial features while maintaining a stablefunctional occlusion. The degree of skeletal correctionis limited by the ability of the soft tissues to adapt toskeletal changes. When satisfactory bone stability isensured, postsurgical orthodontics can be started.
Postsurgical orthodontic treatment aims atreaching the best possible dental occlusion withoutcompromising the stability of skeletal changesachieved during surgery. The goal is to ensurecoordination of the centric relation, in which thecondyles are anatomically seated in their anatomicpositions, and centric occlusion, in which the teeth fitor bite best together, which is also called maximumintercuspation.
Functional treatment guidelines include establish-ing stable normal occlusion with consistent centricrelation of the TMJ and centric occlusion. Normalocclusion is defined by proper dental intercuspation,proper incisor overlap, with elimination of overjet,reverse overjet, open bite, or overbite. Discrepancybetween centric relation and centric occlusion is a ‘‘redalert’’ that should be monitored throughout thetreatment period, especially during the postsurgicalorthodontic treatment. Starting the orthodontic toothmovements before full stability of bone segments is amajor cause of such a complication.
Another functional marker of treatment successis the restoration of appropriate longitudinal andhorizontal curvature of the occlusal plane (curve ofSpee and curve of Wilson), proper dental align-ment, and elimination of dental crowding andinterdental spaces. Additional postsurgical dentalalignment and leveling may be necessary to achievethe final result.
AESTHETIC ENDPOINTS
The ultimate measure of success lies in achievingthe predicted facial appearance that the patient
anticipated and agreed to. Although normative softtissue and skeletal values are helpful as guidelines,they should not be regarded as concrete targets. Infact, if we applied the ‘‘ideal’’ soft tissue proportionsto a large number of individuals who are considered
FUNCTIONAL AND AESTHETIC ENDPOINTS / Elsalanty et al
729

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
to have beautiful or attractive facial profiles, wewould find that most of them have significantlydifferent proportions. This makes deviation from the‘‘ideal’’ the rule rather than the exception, whichmeans that the endpoint of treatment should beindividually defined for each patient. The patientshould fully understand and be comfortable with thisconcept before treatment starts.
People have been trying to define beauty for aslong as art and sculpture have existed. Renaissanceartists identified several anthropometric rules thatdefine the ideal facial relationships as based uponclassical Greek canons.45 Later, the classical artisticdefinition of beauty was transferred from art tomedical practice. However, testing these parametershas proven that they cannot consistently be appliedto define aesthetic endpoints for a specific race.45 Itmakes no sense, therefore, to try to achieve the samecriteria across racial lines.46
Some guiding criteria for facial harmony havebeen proposed, including the rule of thirds, the ruleof fifths, and smile parameters. These and othercriteria were adopted over the years in the attempt toquantify the elements of facial beautyVfacial sym-metry, balance between hard and soft tissues, andharmony in facial featuresVso that these ‘‘abstract’’elements could be measured, analyzed, and com-pared. Although the patient’s situation can bedefined using such guidelines, the goal of treatmentshould not be to bring each individual measurementback to its ‘‘normal’’ value. Instead, the treatmentendpoint for a specific patient is reached whenoptimal facial projection that is balanced, symmet-rical, harmonious, and stable has been achieved.
The rule of thirds (Fig 2) states that the verticalfacial height is divided into equal thirds by fourhorizontal lines at the hairline, the glabella, the baseof the nose, and the menton. In adults, the philtrumheight should constitute one third of the lower facialheight. The commissure height is typically 2 to 3 mmlonger than the philtrum in adults but is shorter inadolescents. During growth, the upper lip may lagbehind the lower lip in vertical height but catches uparound adolescence. When the head is in neutralposition, the nostrils should be barely visible. Thecolumella should be parallel to the alae of the nose,regardless of the direction of view.
The rule of fifths states that the anterior profile ofthe face can be divided vertically into five regionsthat are almost equal. The lines of division are acrossthe lateral and medial canthus on both sides (Fig 3).Vertical lines from the inner canthus, the pupil, andthe outer canthus should consequently coincide withthe ala of the nose, the oral commissure, and themandibular gonial angle. Therefore, the nasal widthshould be equal or slightly larger than the inter-canthal width, whereas the oral width should beequal to the interpupillary distance.
The most relevant dental landmark for the patientmay be incisor position and inclination. Changes inthis landmark will greatly influence the amount ofincisor display during rest, which should be within 3 to4 mm. During social smiling, the upper incisors shouldbe completely displayed with a rim of gingival toproduce an attractive, youthful smile. Even if moregingival show occurs during smiling, this does notrequire correction as long as the display at rest iswithin 3 to 4 mm.39 With age, the labial thickness
Fig 2 Rule of thirds: vertical facial height is divided into equal thirds by four horizontal lines at hairline, glabella, base ofnose, and menton. In adults, philtrum height should constitute one third of lower facial height.
THE JOURNAL OF CRANIOFACIAL SURGERY / VOLUME 18, NUMBER 4 July 2007
730

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
decreases, increasing the length of the upper lip, andthe gingival show will typically decrease.
One of the most prominent factors that deter-mines the attractiveness of the face is the smile. It isalso one of the most variable factors and is difficult tocontrol. The achievement of an aesthetic smile is veryimportant for patient satisfaction with the treatment
outcome; therefore, it should be foremost in thetreatment plan. Parameters such as Cupid’s bowoutline, philtrum height, lip thickness, buccal corri-dors, smile arc, and symmetry of the dental displayand nasolabial folds during smile have gained well-deserved attention in recent years. In addition to theclassical incisor display and gingival show, theseparameters have dramatic influence on the personalityof the face. Criteria for an esthetic smile have beenpreviously identified.39,47Y51
Intuitively, we can see it is the facial features thatwill ultimately define the beauty and attractivenessof the face and not its outline or dimensional ratios. Itis interesting how very fine changes in nasal profile,symmetry of the nasolabial folds, commissure height,depth of the labiomental sulcus, lip-chin-throatangle, chin projection, and chin-neck angle candramatically change the facial outlook. Adequateprominence of specific points of the face, more sothan others, defines its overall projection, and theseinclude the chin, the temples, tip of the nose, andsupraorbital ridges (Fig 4). Therefore, treatmentresults can be greatly enhanced if some ‘‘fine-tuning’’of these features is considered. This may includegenioplasty, which can be performed as a part of thejaw surgery, malar augmentation, lip augmentation,submental liposuction, fat injection, or rhinoplasty.The result is a visually pleasing, attractive face, not amatrix of calculated lines and angles.
CONCLUSION
Functional endpoints aligned with societal normstypically provide a ‘‘normal’’ face that is not
Fig 3 Rule of fifths: face can be divided vertically into fiveequal regions. Lines of division are across lateral andmedial canthus on each side. Vertical lines from innercanthus, pupil, and outer canthus should consequentlycoincide with ala of nose, oral commissure, and mandib-ular gonial angle.
Fig 4 Not all areas of the face are of equal importance in determining facial projection. Most important points are chin,temples, tip of nose, and supraorbital ridges.
FUNCTIONAL AND AESTHETIC ENDPOINTS / Elsalanty et al
731

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
necessarily beautiful. Orthognathic surgery candramatically change the look and proportions ofthe face even without changing functional occlusion.By adding an aesthetic concept to the surgical plan,we can achieve a face with stable occlusion and abeautiful look each time. Additional soft tissueprocedures may be required to give final balanceand harmony to the face.
REFERENCES
1. Steinhauser EW. Historical development of orthognathicsurgery. J Craniomaxillofac Surg 1996;24:195Y204
2. Blair VP. Operations on the jaw-bone and face. Surg GynecolObstet 1907;4:67Y78
3. Angle EH. Malocclusion of the Teeth. ed 7. Philadelphia: S. S.White Dental Mfg. Co., 1907
4. Tessier P. Total facial osteotomy. Crouzon’s syndrome, Apert’ssyndrome: oxycephaly, scaphocephaly, turricephaly. Ann ChirPlast 1967;12:273Y286
5. Tessier P, Guiot G, Rougerie J, et al. Cranio-naso-orbito-facialosteotomies. Hypertelorism. Ann Chir Plast 1967;12:103Y118
6. Tessier P. The definitive plastic surgical treatment of the severefacial deformities of craniofacial dysostosis: Crouzon’s andApert’s diseases. Plast Reconstr Surg 1971;48:419
7. De Ranieri A, Virdi AS, Kuroda S, et al. Local application ofrhTGF-beta2 modulates dynamic gene expression in a ratimplant model. Bone 2005;36:931Y940
8. De Ranieri A, Virdi AS, Kuroda S, et al. Local application ofrhTGF-beta2 enhances peri-implant bone volume and bone-implant contact in a rat model. Bone 2005;37:55Y62
9. Sykaras N, Triplett RG, Nunn ME, et al. Effect of recombinanthuman bone morphogenetic protein-2 on bone regenerationand osseointegration of dental implants. Clin Oral ImplantsRes 2001;12:339Y349
10. Boyne PJ, Lilly LC, Marx RE, et al. De novo bone induction byrecombinant human bone morphogenetic protein-2 (rhBMP-2)in maxillary sinus floor augmentation. J Oral Maxillofac Surg2005;63:1693Y1707
11. Barboza EP, Duarte ME, Geolas L, et al. Ridge augmentationfollowing implantation of recombinant human bone morpho-genetic protein-2 in the dog. J Periodontol 2000;71:488Y496
12. Wikesjo UM, Sorensen RG, Wozney JM. Augmentation ofalveolar bone and dental implant osseointegration: clinicalimplications of studies with rhBMP-2. J Bone Joint Surg Am2001;83A(Suppl 1):S136YS145
13. Seto I, Marukawa E, Asahina I. Mandibular reconstructionusing a combination graft of rhBMP-2 with bone marrowcells expanded in vitro. Plast Reconstr Surg 2006;117:902Y908
14. Seto I, Asahina I, Oda M, et al. Reconstruction of the primatemandible with a combination graft of recombinant humanbone morphogenetic protein-2 and bone marrow. J OralMaxillofac Surg 2001;59:53Y62
15. Boyne PJ. Animal studies of application of rhbmp-2 inmaxillofacial reconstruction. Bone 1996;19(Suppl 1):83SY92S
16. Cook SD, Wolfe MW, Salkeld SL, et al. Effect of recombinanthuman osteogenic protein-1 on healing of segmentaldefects in non-human primates. J Bone Joint Surg Am1995;77:734Y750
17. Marukawa E, Asahina I, Oda M, et al. Bone regeneration usingrecombinant human bone morphogenetic protein-2 (rhBMP-2)in alveolar defects of primate mandibles. Br J Oral MaxillofacSurg 2001;39:452Y459
18. Marukawa E, Asahina I, Oda M, et al. Functional reconstruc-tion of the non-human primate mandible using recombinant
human bone morphogenetic protein-2. Int J Oral MaxillofacSurg 2002;31:287Y295
19. Rachmiel A, Aizenbud D, Peled M. Enhancement of boneformation by bone morphogenetic protein-2 during alveolardistraction: an experimental study in sheep. J Periodontol2004;75:1524Y1531
20. Cheung LK, Zheng LW. Effect of recombinant human bonemorphogenetic protein-2 on mandibular distraction at differ-ent rates in an experimental model. J Craniofac Surg 2006;17:100Y110
21. Ozec Y, Ozturk M, Kylyc E, et al. Effect of recombinant humanbone morphogenetic protein-2 on mandibular distractionosteogenesis. J Craniofac Surg 2006;17:80Y83
22. Zakhary K, Motakis D, Hamdy RH, et al. Effect of recombinanthuman bone morphogenetic protein 7 on bone density duringdistraction osteogenesis of the rabbit mandible. J Otolaryngol2005;34:407Y414
23. Ashinoff RL, Cetrulo CL Jr, Galiano RD, et al. Bone morpho-genic protein-2 gene therapy for mandibular distractionosteogenesis. Ann Plast Surg 2004;52:585Y591
24. Terheyden H, Wang H, Warnke PH, et al. Acceleration ofcallus maturation using rhOP-1 in mandibular distractionosteogenesis in a rat model. Int J Oral Maxillofac Surg 2003;32:528Y533
25. Lieberman JR, Daluiski A, Einhorn TA. The role of growthfactors in the repair of bone. Biology and clinical applications.J Bone Joint Surg Am 2002;84A:1032Y1044
26. Ebara S, Nakayama K. Mechanism for the action of bonemorphogenetic proteins and regulation of their activity. Spine2002;27(Suppl 1):S10YS15
27. Einhorn TA. The cell and molecular biology of fracture healing.Clin Orthop Relat Res 1998;(355 Suppl):S7YS21
28. Morris A. Seriously Handicapping Orthodontic Condition.Washington, DC: National Academy of Sciences, 1976
29. Salzmann JA. Editorial: Seriously handicapping orthodonticconditions. Am J Orthod 1976;70:329Y330
30. Ackerman JL. Orthodontics: art, science, or trans-science?Angle Orthod 1974;44:243Y250
31. Bergman RT. Cephalometric soft tissue facial analysis. Am JOrthod Dentofacial Orthop 1999;116:373Y389
32. Mack MR. Perspective of facial esthetics in dental treatmentplanning. J Prosthet Dent 1996;75:169Y176
33. Park YC, Burstone CJ. Soft-tissue profile: fallacies of hard-tissue standards in treatment planning. Am J Orthod Dento-facial Orthop 1986;90:52Y62
34. Holdaway RA. A soft-tissue cephalometric analysis and its usein orthodontic treatment planning. Part I. Am J Orthod1983;84:1Y28
35. Holdaway RA. A soft-tissue cephalometric analysis and its usein orthodontic treatment planning. Part II. Am J Orthod1984;85:279Y293
36. Sarver DM. Esthetic Orthodontics and Orthognathic Surgery.St. Louis: Mosby, Inc., 1998
37. Ackerman JL, Proffit WR, Sarver DM. The emerging soft tissueparadigm in orthodontic diagnosis and treatment planning.Clin Orthod Res 1999;2:49Y52
38. Proffit WR. The soft tissue paradigm in orthodontic diagnosisand treatment planning: a new view for a new century. J EsthetDent 2000;12:46Y49
39. Proffit WR, White RP Jr, Sarver DM. Contemporary Treatmentof Dentofacial Deformity. St. Louis: Mosby, Inc., 2003
40. Bailey LJ, Proffit WR, White RP Jr, et al. Patient selection fororthognathic surgery. In: Fonseca RJ, Betts NJ, Turvey TA, eds.Oral and Maxillofacial Surgery. Vol. 2. Philadelphia: W. B.Saunders, 2000:3Y23
41. Baccetti T, McGill JS, Franchi L, et al. Skeletal effects of earlytreatment of class III malocclusion with maxillary expansionand face-mask therapy. Am J Orthod Dentofacial Orthop 1998;113:333Y343
THE JOURNAL OF CRANIOFACIAL SURGERY / VOLUME 18, NUMBER 4 July 2007
732

Copyright @ 200 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.7
42. Franchi L, Baccetti T, McNamara JA Jr. Shape-coordinateanalysis of skeletal changes induced by rapid maxillaryexpansion and facial mask therapy. Am J Orthod DentofacialOrthop 1998;114:418Y426
43. Sarver DM. Esthetic Orthodontics and Orthognathic Surgery.St. Louis: Mosby, Inc., 1997
44. Proffit WR, Fields HW. Contemporary orthodontics. 3rd ed. St.Louis: Mosby, Inc., 2000
45. Farkas LG, Hreczko TA, Kolar JC, et al. Vertical and horizontalproportions of the face in young adult North Americancaucasians: revision of neoclassical canons. Plast ReconstrSurg 1985;75:328Y338
46. Farkas LG, Forrest CR, Litsas L. Revision of neoclassical facialcanons in young adult Afro-Americans. Aesthetic Plast Surg2000;24:179Y184
47. Sarver DM, Ackerman MB. Dynamic smile visualizationand quantification. Part II. Smile analysis and treatmentstrategies. Am J Orthod Dentofacial Orthop 2003;124:116Y127
48. Sarver DM, Ackerman MB. Dynamic smile visualization andquantification. Part I. Evolution of the concept and dynamicrecords for smile capture. Am J Orthod Dentofacial Orthop2003;124:4Y12
49. Ackerman MB, Ackerman JL. Smile analysis and design in thedigital era. J Clin Orthod 2002;36:221Y236
50. Ackerman MB, Brensinger C, Landis JR. An evaluation ofdynamic lip-tooth characteristics during speech and smile inadolescents. Angle Orthod 2004;74:43Y50
51. Ackerman MB. Buccal smile corridors. Am J Orthod Dentofa-cial Orthop 2005;127:528Y529. author reply 529
FUNCTIONAL AND AESTHETIC ENDPOINTS / Elsalanty et al
733