FOLIO -1-interested in receiving FOLIO by e-mail, please let us know. FOLIO is prepared for the...
Transcript of FOLIO -1-interested in receiving FOLIO by e-mail, please let us know. FOLIO is prepared for the...

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-1-FOLIO
©2004 – Flahive, Ogden & LatsonFebruary 2004 Volume 9, No. 1
A Privileged Attorney-Client Communication by Flahive, Ogden & Latson
FOLFOLFOLFOLFOLFOLFOLIO
In This Issue . . .Proposed Amendments to Old RulesReport of Injury and IllnessChanges at TWCC
p. 3p. 4p. 5
As reported in the last issue ofFOLIO, a Dallas television newsstation aired a 3-night segmentdealing with difficulties that workerswere having in obtaining medicaltreatment for workers’compensation injuries. That storyhas been picked up by at least onenewspaper, The Dallas MorningNews.
In a story entitled “A Crisis forWorkers: Injuries Get Red Tape Rather than Bandages,”the Morning News referred to the WFAA – TV newsseries but expanded it somewhat. The paper did notethat one of the problems that workers are having is that“employers aren’t staying in the system.” Accordingto the Morning News, the “most damning allegation”is that TWCC is “too close” to the insurance industryand looks the other way.
That is not the experience of carriers writingbusiness in the state.
The article concluded by making the point that thesystem needs to be balanced. Patients should be ableto find medical care, doctors should not be forced toleave for economic reasons, and employers should nothave to face increased costs. This statement by thenewspaper is reminiscent of the managed care debatefrom several years ago. Insureds want more medicalcare, but at no increased costs.
TEXAS WORKERS’ COMPREMAINS IN THE NEWS
This statement by thenewspaper isreminiscent of themanaged care debatefrom several yearsago. Insureds wantmore medical care, butat no increased costs.
The Morning News closed its article bynoting “workers are paying hefty psychological,physical and economic prices for a system thatis brutally unresponsive.” n
The Texas Workers’ Compensation Act will cease toexist in 2005 unless it is re-enacted by the Legislature.This is the process of Sunset Review that all Texasadministrative agencies must face. The Texas process wasaccelerated by two years in order to earlier evaluate thereforms adopted by House Bill 2600.
Because of the public interest having to do with therefusal of some medical specialists to participate in theworkers’ compensation system, several news outlets havecharacterized workers’ compensation “in crisis.” TheLieutenant Governor’s office echoed that sentiment in anews release in December. As reported in the last issue ofFOLIO, a Senate Subcommittee was appointed.
The House has appointed its subcommittee to bechaired by Helen Giddings, a Democrat from Dallas andJoe Nixon, a Republican (and author of House Bill 4) fromHouston. The House Committee will examine whetherclaims of legitimately injured workers and their doctors are
continued page 15
Groups Preparingfor 2005 Sunset
Review

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-2- FOLIO
Flahive, Ogden & Latson, a 26 lawyerfirm, defends contested workers’compensation cases statewide every day.The firm has represented insurancecompanies and employers before the TexasWorkers’ Compensation agency for morethan 50 years.
For general questions concerning thenewsletter call (512) 435-2234.
Flahive, Ogden & LatsonP.O. Box 13367
Austin Texas 78711
An electronic copy of FOLIO, our monthly clientnewsletter, is now available for clients. If you areinterested in receiving FOLIO by e-mail, please let usknow. FOLIO is prepared for the exclusive use ofFlahive, Ogden & Latson clients only. It containsprivileged communications and further sharing of thisnewsletter (in either hard copy or electronic format)outside your company without the express written consentof Flahive, Ogden & Latson is not permitted.
Our regular office hours are 8:15 a.m. to4:45 p.m.. If you need to call after 4:45,please call Patsy Shelton at (512) 435-2234.She will be on duty until 6:00 p.m. daily.DON’T W AIT UNTIL THE LAST HOUROF THE DAY FOR DEADLINE FILING.ANY FAXES WITH INFORMATION DUEMUST BE RECEIVED BY 3:30 p.m. for anydeadline handling for same day delivery tothe Commission, and faxed according to thefax directory listed on the last page ofFOLIO. Furthermore, if you have a lastminute deadline, call our office by 3:00 p.m.and speak with Tillie Aguirre or PatsyShelton to advise that a last minute filing isnecessary to meet a deadline. We will bewatching and waiting for the fax. Otherwise,last minute faxes could delay receipt. Ourlast daily run to the Commission will be at4:00 p.m., in order to get across town to meettheir 5:00 closing time.
FO&L OFFICE HOURS
The Hospital Fee Guideline case involves approximately 20,000claims for reimbursement by hospitals for the difference in theamounts paid by carriers from 1992 through 1997 under an appellatecourt voided Hospital Fee Guideline (HFG).
The HFG case is pending before SOAH as well as the TravisCounty District Court. The Austin trial court and the Austin Courtof Appeals concluded that about 85% of the claims are barred becauseof the Hospitals’ failure to comply with the one-year rule. After theCourt of Appeal opinion favoring the Insurers, the Hospitals petitionedthe Supreme Court to hear the case. That petition has now beendenied.
Barring a very unlikely granting of a motion for rehearing by theSupreme Court, the Hospitals have forfeited 85% of all outstandingclaims. It should reduce the pending litigation from a $160 millioncase to a $24 million case.
While the remaining amount in dispute is still substantial, theoldest and most difficult to document cases are now barred and thatsubstantially reduces the litigation burden with respect to the remainingcases. It will basically result in the dismissal of all cases prior to 1996,and should mean only the cases in the latter part of 1996 through 1997are eligible for further litigation.
Those cases are subject to a ruling in a Declaratory JudgmentAction that is now pending and in which the Insurers have largelyprevailed in the points asserted. Basically, the remaining cases shouldbe tried under the statutory standards in place and should not bereimbursed according to the informal methodology utilized by insurersprior to 1992. The statutory standards case remains on appeal. n
Supreme CourtDenies Petition in
Hospital Fee GuidelineCase
Conference on FraudHosted By TDI
On January 29th and 30th, TDI posted a statewide insurance fraudconference highlighting its antifraud efforts.
TDI described two basic types of insurance fraud: Opportunistic,(when an individual decides to exaggerate losses on a legitimateclaim); and Organized Fraud Operations (which can include a stagedaccidents, exaggerated injuries, and disability fraud). n

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-3-FOLIO
TV News ClaimsRe: Peer Reviewers
Within the last ten years, carriers abandoned the prior business practiceof unilateral decisions unsupported by medical evidence. Since that time,virtually all carriers have relied on some report of a physician, includingpeer reviews. The use of peer review physicians now appears to be underattack.
In yet another story from WFAA – TV, court records obtained by thenews station established that “one Dallas-area doctor has grossed nearly $7million in the past four years doing peer reviews for insurance companies.”
The news station quoted an unnamed North Texas doctor who hadperformed “honest and objective peer reviews” and she got less and lessbusiness simply because she was trying to be “honest and correct in medicaldiagnosis.” n
The Texas Workers’Compensation Commission hasproposed amendments to Rule 42.105(Medical Fee Guideline), and the repealof Rule 42.115 (Pharmaceutical FeeGuideline).
The amendments to Rule 42.105are proposed to make all fee guidelinesand pharmaceutical benefit provisionsunder Chapter 134 of theCommission’s rules applicable to thereimbursement of medical treatmentsand services provided to employeeswho sustained compensable injuriesbefore January 1, 1991 (“old law”claims).
Currently, only Rule 134.201 ofthat chapter provides for thereimbursement of professional medicaltreatments and services that relate to“old law” claims. In addition, there iscurrently no facility fee guidelineapplicable to the reimbursement offacility services that relate to “oldlaw” claims. The proposedamendments to Rule 42.105 providethat Rule 134.201 will continue toapply to “old law” claim forprofessional medical treatments andservices rendered before May 1, 2004;
Commission Proposes Changes ToOld Law Medical Rules
and that all the fee guidelines andpharmaceutical benefit provisionswithin Chapter 134 will apply to“old law” claims for professionalmedical treatments and servicesrendered on or after May 1, 2004.
The proposed amendments toRule 42.105 will also make anyfacility fee guidelines currently ineffect, and any facility or otherhealth care fee guidelines adoptedby the commission in the future,applicable to “old law” claims.The proposed amendments to Rule42.105 do not make all of Chapter134 applicable to “old law” claims.Only the fee guideline provisionscurrently found in Subchapters Cand D, and the pharmaceuticalbenefit provisions currently foundin Subchapter F, and any feeguideline provisions orpharmaceutical benefit provisionsadopted by the commission underChapter 134 in the future, wouldapply. The only exception wouldbe Rule 134.501, relating to InitialPharmaceutical Coverage. Rule134.501, which addresses thereimbursement of pharmaceutical
services provided within the first sevendays following the date of injury for newlaw cases.
The applicable Rules of Chapter 134currently in effect would be as follows:• 134.201 Medical Fee Guideline for
Medical Treatments and ServicesProvided under the Texas Workers’Compensation Act
• 134.202 Medical Fee Guideline• 134.203 Dental Fee Guideline• 134.401 Acute Care Inpatient
Hospital Fee Guideline• 134.500 Definitions• 134.502 Pharmaceutical Services• 134.503 Reimbursement
Methodology• 134.504 Pharmaceutical Expenses
Incurred by the Injured Employee• 134.506 Outpatient Drug Formulary
The proposed rules are in AdobePortable Document Format (PDF). Toview the PDF document, you will needAcrobat Reader. If you do not have AcrobatReader, please go to www.adobe.com andfollow the instructions to download thefree software.
Should you wish to comment on theproposed rule, comments must be receivedby 5:00 p.m. CT on by February 16, 2004as follows:• Via the Internet by using the Comment
Form <commentform1.html>, or• By e-mailing your comments to
[email protected] or• By mailing or delivering your
comments to:Linda VelasquezOffice of the General Counsel, MS #4-DTexas Workers’ CompensationCommission7551 Metro Center Drive, Suite 100Austin, Texas 78744-1609 n

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-4- FOLIO
TWCC has issued Advisory 2003-21, having to do with the usual andcustomary charges that pharmaciesmust bill. The rules require healthcareproviders to bill the same fees toworkers’ compensation carriers evenif they are higher than the FeeGuidelines. However, pharmacies andother HCPs should never bill workers’compensation carriers more than theybill other payers. Thus, the discussionabout usual and customary addressesthe already existing rule requirement.There is nothing new about it.
Carriers should reimburse theusual and customary chargesaccording to the Pharmacy FeeGuidelines. This will result in areduction in accordance with thereimbursement methodologyprescribed in Rule 134.503.
When the amount of thereimbursement is disputed, TWCCMRD should order reimbursement inthe amount of the fee guideline if it isless than the pharmacy’s usual andcustomary charge. If thereimbursement is based upon anegotiated contract, during disputeresolution, the carrier should providea copy of a contract between the carrier,or its pharmacy manager, and thepharmacy establishing the pharmacy’sagreement to discount it charges withrespect to the particular prescriptionin dispute. n
Doctor DownloadFile Layout Changes
TWCC announced a new formatfor the doctor download. AlthoughTWCC is still performing Datacleanup related to the previouslydeleted participants, the new file shouldbe online as of February 1, 2004. n
Pharmacy FeeDisputes
For the thirteenth year in a row,the nonfatal workplace injury andillnesses incidence rate in Texas wasmarkedly lower than that of the nation.In 2002, the Texas incidence rate was4.3 injuries and illnesses per 100 full-time workers, while the nationalincidence rate was 5.3. Thisinformation was obtained from asurvey conducted by the TexasWorkers’ Compensation Commission(TWCC) in cooperation with theBureau of Labor Statistics. The ratesare based on survey findings fromapproximately 11,000 private industryemployers.
In 2002, the manufacturingStandard Industrial Classification(SIC) industry group recorded thehighest incident rate at 5.9 (Table 1).The transportation and public utilitiesindustry experienced the secondhighest incidence rate at 5.1 while thefinance, insurance, and real estate SICgroup recorded the lowest rate of 2.0.
Overall, establishments thatemployed between 50 and 249 workersreported the highest incidence rate at5.5 followed by establishments with250 to 999 employees that recorded anincidence rate of 5.3 per 100 full-timeemployees.
The incidence rate of nonfatalworkplace injuries and illnessesrequiring days away from work was1.3 per 100 full-time workers. Therestricted-duty cases (those that involveshortened hours, a temporary jobchange, or restricted job functions)incidence rate was 1.1.
Illness-only incidence rates werecalculated separately from the totalinjury/illness rate. Because of theirrelatively smaller numbers, illnesses
Texas Workplace Injuryand Illness Rate Lower
Than Nationalare reported per 10,000 full-timeworkers. Whereas injuries are usuallythe result of a single event, illnessesdevelop over a period of time as aresult of exposure to physical orchemical hazards, or repetitive trauma.In general the private sector recordeda work-related illness incidence rateof 26.4 per 10,000 full-time workers.As in the case of occupational injuries,the manufacturing SIC sector recordedthe highest illness incidence rates at57.1 per 10,000 full-time workersfollowed by transportation and publicutilities at 33.7.
Due to changes effective January1st, 2002 to the Occupational Safetyand Health Administration (OSHA)recordkeeping system that employersuse to track and record work-relatedinjuries and illnesses, BLS advisesthat 2002 rates cannot be comparedwith previous years’ rates. This newlyrevised OSHA recordkeeping systemis designed to produce betterinformation about occupationalinjuries and illnesses while simplifyingthe overall recordkeeping process foremployers.
Additional Texas fatal andnonfatal occupational injuries andillnesses data are available on-linethrough standard or customized tablesat http://www.twcc.state.tx.us/servicesandresources.html or bycontacting the TWCC SafetyInformation Systems section at 512-804-4663 or [email protected]. n

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-5-FOLIO
Governor Rick Perry hasappointed Commissioner MikeHachtman to serve as Chairman ofthe Texas Workers’ CompensationCommission (TWCC). Mr.Hachtman will complete theChairmanship term of CommissionerRichard Smith, who has served asChairman since February 2003.Hachtman’s term as Chairman willexpire February 1, 2005. The Actrequires the Governor to appoint asitting Commissioner for two-yearterms as Chairman. That positionalternates every February of odd yearsbetween employer- and employee-commissioners. Mr. Hachtman’s termas a Commissioner began in February2003 and expires February 2009.
Mike Hachtman is Vice Presidentof Business Development for IFCOSystems North America, Inc., thelargest pallet company in the NorthAmerica. Before joining the privatesector, Mr. Hachtman served as Chiefof Staff at the Texas RailroadCommission. In 1989, while servingas a staff member in the Texas House,he worked primarily on the drafting
Commissioner and ManagementChanges at TWCC
and passage of House Bill 1, the TexasWorkers’ Compensation Reform Act.Mr. Hachtman is a graduate of TexasA&M University.
***********************There has also been a major change
of management at the Medical ReviewDivision of the TWCC. Robert L.“Bob” Shipe has accepted the positionof Director of Medical Review. He willassume his new duties January 16,2004.
Mr. Shipe has been with the TWCCsince 1991. His most recent positionwas that of the TWCC’s Director ofGovernmental Relations. Prior to that,Mr. Shipe held various positions withinthe TWCC, including Director ofWorkers’ Compensation TrainingEducation and Development, andAssociate Director of Field Operations.In those capacities and others, Mr.Shipe has been a fixture at TWCCpublic meetings and providing input tothe Medical Advisory Committee andthe Legislature.
Lastly, and importantly, SteveQuick, the former Director ofCompliance & Practices, has retired.
Remember that the 4th Quarter2003 must be submitted on theTWCC-approved matrix. This isrequired to be filed. Failure to timelyfile this matrix may result in a referralto the Division of Compliance &Practices.
Also recall that each carrier mustconsolidate the carrier’s response. Ifall or part of the carrier’s business inTexas is unbundled to TPAs, theTPAs must provide their individualpreauthorization matrix data to thecarrier and the carrier mustconsolidate it prior to submitting it toTWCC. n
The Texas Workers’ Compensation Commission has determined, pursuantto the authority and direction given under the Texas Workers’ CompensationAct (Texas Labor Code, Section 401.023), that any interest or discountprovided for in the Act shall be at the rate of 4.76 percent. This rate is computedby using the treasury constant maturity rate for one-year treasury bills issuedby the United States Government, as published by the Federal Reserve Boardon December 17, 2003 (1.26 percent) plus 3.5 percent as required by Section401.023. The rate shall be effective January 1, 2004 through March 31, 2004.For more information, please call Matt Jung at 512-804-4568. n
Discount Rate and InterestRate Determined
Pre-Auth MatrixDue
He is no longer employed by theagency.
In his place, Teresa Carney hasbeen appointed. Ms. Carney is alongtime employee of TWCC and hasbeen quite prominent within theCompliance & Practices Division. Shewas the manager over the Audit &Compliance Enforcement section afterthe departure of Adam Leonard. Mostrecently, Ms. Carney has supervisedthe division responsible for fraudinvestigation and prosecution. Thus,she has been in a supervisory positionwith respect to both departments withinCompliance & Practices. Becauseshe is so familiar with the division,this change should not significantlyaffect Compliance & Practices policy.
Both Mr. Shipe and Ms. Carneyare very well regarded within theagency and should significantly assistthe Commissioners in dealing with theadditional media focus about medicalbill payment and carrier compliancewith the TWCC Act. n

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-6- FOLIO
Q
A
Q
A
Q
Q
A
Here are several of the most significant generalquestions ( and answers) asked of FO&L attorneysthis month.
CornerQG
A
Q
A
I have a claim with a date of injury of 08/21/03,I denied the claim 09/03/2003. We have receiveda pharmacy bill for date of service 08/27/03. As
the claim is denied, do we owe payment for the pharmacybill pursuant to Rule 134.501. My understanding is thatregardless of compensability we owe pharmacy bills forthe first seven days and may seek recovery from the SIFshould the injury be determined not to be compensable.
According to Rule 134.502, effective 1-1-03, if apharmacy verifies insurance coverage and verifiesa claim has been reported to the carrier the
pharmacy is entitled to reimbursement for the first 7 daysof the prescription, even if there is a dispute overcompensability or extent of injury, provided it wasreasonable and necessary. It does not matter that the billwas not submitted to the carrier prior to the 7 days.
Also, medical benefits accrue when rendered, not when thebill is submitted. Therefore, if the carrier disputes after theseventh day, but before the 60th day, then the carrier isliable for the payment of any medical that was R&N priorto the dispute regardless of whether the bill was submittedafter dispute was filed. There are arguments to thecontrary on this point, but in light of the clarificationissued by the Commission in the proposed amendments toRule 124.3, we are not encouraging reliance on thosecontrary arguments.
We received a TWCC-69 for an exam performedby “a doctor selected by the treating doctor.”The treating doctor did not review the TWCC-69.
Should we begin paying IIBs based on this TWCC-69 ordo we have to wait until we receive a TWCC-69 reviewedby the treating doctor?
Section 408.121 of the 1989 Act requires a carrierto initiate payment of IIBs no later than the fifthday after receiving the report certifying MMI.
Rule 130.1 delineates the types of doctors that are authorizedto certify MMI. Under the circumstances, the treating
doctor (as he made a referral for MMI/IR) is not anauthorized doctor. Although Rule 130.3 requires thereferral doctor to forward a copy to the treating doctor, thisequally applies to a designated doctor, and nothing in therule allows the treating doctor to overrule the doctor heselected. Therefore, you neither have to nor should wait forthe treating doctor to review the certification.
Is the Carrier liable for payment to the treatingdoctor if he chooses to go to the Required MedicalExam?
Yes. Texas Labor Code, Section 408.004(d)indicates that the treating doctor is entitled to bepaid a fee for attending. The reimbursement
amount limits and procedural requirements are set out inRule 134.5.
I have a treating doctor who has released claimantto return to work full duty. The referral ortho hastaken claimant completely off work due to “too
much pain to work.” The claimant continues to work butgoes to physical therapy three times a week.
1) Which doctor has precedent on work status? 2) The claimant is receiving his full salary fromthe employer, so is it correct that the carrier does not owepartial temporary income benefits?
Disability may be shown by any credible evidence,including the claimant’s testimony alone. Somepeople argue that the treating doctor determines
work status, not the referral. This, however, is wrong. Itis up to you to make an evaluation of the credibility of thevarious opinions based upon the totality of the medicalevidence. You should then pay or not based upon thisdetermination. As long as the claimant continues to receive100% of her pre-injury average weekly wage from theemployer she is not entitled to TIBs.
Employee slipped and fell in parking lot on herlunch break. The parking lot is owned andmaintained by our insured. The slip/fall was due
to soft ground from recent rains. Would claimant’sinjuries be compensable?
Your facts bring the “access doctrine” into play.Under the access doctrine, the employer’s premisesare effectively extended to create a “zone of

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-7-FOLIO
Q
A
Q
A
A
Q
A
employment” for employees between the hazards of travelon the streets (hazards to which all workers are exposed),and the risk in the actual workplace to which the employeesare exposed. Within this zone of employment, the injury istreated as if it occurred on the employer’s premises, and iscompensable without any further analysis of whether theemployee was engaged in or in the furtherance of the affairsof the employer at the time of the accident (i.e., the personalcomfort and convenience doctrine). Because you statedthat this occurred in an employer-owned parking lot, the“access doctrine” applies. Different results may occur ifthe parking lot was neither owned nor maintained by theemployer.
I received an enormous stack of chiropractorbills on a claimant with an open leg wound. Thechiropractor was treating him for the neck, lower
back, hips, and finally the leg wound. We disputed allcharges (TWCC-21 for extent of injury was already filedto accept the leg only, not to include all other body parts)since the other body parts were not compensable. Iadvised the provider to pull out the services for the legwound only and we could reconsider the bill for payment.They sent back the entire stack of bills once more and tookoff all the diagnosis codes for the neck and back, leavingonly a diagnosis code for the leg and re-billed the exactsame charges all over again. So I am seeing things likemyofacial releases (for a leg wound?) and manipulationsthat we knew were for the back. Other than reviewing itvery carefully, code by code, is there anything else we cando? Plus we know they are continuing to treat him for thedisputed body parts .
Pursuant to Rule 133.304(l), you have 21 days torespond to the resubmission. You must take oneof the final actions permitted by section (b). You
have to pay what you owe for the compensable injury anddispute the rest. The provider can then take the issue tomedical review, or wait on the outcome of the extent ofinjury dispute. In this case, you probably will have to goline by line.
I have a case where we will argue that the cervicalsurgery performed was not reasonable andnecessary. However, the surgery went so badly
that the claimant needed two other surgeries to correctthe mess. What are your thoughts as to whether we areliable for the consequences of the surgery, even though itwas caused by inappropriate treatment?
If your URA preauthorized the original surgery,then you have lost the right to now take the positionthat it was not reasonable and necessary. Under
those circumstances, the carrier is responsible for theresults of the treatment, even if medical malpractice. Youcan sue the doctor or intervene in the claimant’s suitagainst the doctor for the carrier’s losses associated withthe maltreatment. However, if the original surgery was notpreauthorized, then you can certainly take the position itwas not reasonable and necessary. You are only liable forbad results from
I have a claimant who has returned to work for 20hours a week making $16.02 an hour. She is aregular 40-hour work employee and her pre-
injury AWW is $1,112.00 per wage statement. Her post-injury AWW is $320.40. This gives $792.46 loss wages x70% = maximum comp rate of $537.00. Even with claimantworking 20 hours, her comp rate has not changed. Shestill gets the maximum of $537.00. The employer does notthink that is right with them paying her 20 hours and shestill gets the maximum comp rate. Did I figure thiscorrectly?
Your calculations are CORRECT. This is acommon issue with high wage earners.
Claimant is currently completely off work pertreating doctor. Once the claimant is released toreturn to work, he will not be allowed to return
with the insured due to an invalid Social Security number.If the claimant is released to return to work on restrictions,and the insured would normally be able to accommodatehim if it was not for the invalid Social Security number, dowe have to continue benefits?
This is similar to the illegal alien situations. Yourposition is that the claimant would have a lightduty job paying pre-injury wage if he had not been
terminated for using a fraudulent social security card. It isa fact question for the Hearing Officer and there are casesin which carriers have won. Recently, however, theAppeals Panel has held that the carrier has to show that thefact that the claimant was an illegal alien was the sole causeof disability. This is a red herring, however, as that hasalways been the carrier’s position in such a case. There areseveral arguments we can make, but the Appeals Panel hasbeen very pro-claimant of late, and you would need to beprepared to take the case into the court house where youmight have a much stronger case depending upon venue.
Q

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-8- FOLIO
Q I have a claimant who was recently off worktaking sick leave for non-work related back pain/problems, then returned to work. While bending
at the knees at work, he claims he heard a “pop” andbegan to have sharp pains in his back. He is now claiminga workers’ compensation injury and has been taken offwork. Medical dated just before the reported injuryindicates a herniated disk. Is there anything we can do,or do we have to accept the claim as compensable?
You have a decent case for no injury in course andscope. The claimant’s condition may simply be amanifestation or flare-up of the pre-injury
condition. You would deny that any work-related activitycaused any damage or harm to the physical structure of thebody or in any way aggravated the pre-existing andunderlying conditions. Whether there is a new injury is aquestion of fact, however.
If a doctor is on the ADL (but is expired), but latergets renewed, can they re-bill for the dates ofservice while they were in an expired status? If the
doctor treats a patient and then gets approved on theADL, do we owe for the treatment before the doctor wasapproved ?
A carrier is not liable for reimbursing a medicalcare provider who is not on the ADL at the timetreatment is rendered. So, in answer to your first
question, you would not be liable for the costs of anytreatment that was provided while the doctor was in“expired” status.In answer to your second question, you would not be liablefor the costs of treatment provided prior to the doctor’sapproval/listing on the ADL.
Claimant was released to return to work lightduty. A bona fide job offer sent and signed byclaimant. Please note that once the claimant
returned to work he was terminated due to companypolicy regarding the work incident/accident. Please adviseif I should pay full comp or partial based on the light dutyjob offer.
A bona fide offer of employment has to be “bonafide.” That is, it cannot be a ruse for precluding theclaimant from getting benefits. If the employer
knows that it intends to terminate an employee at the timethe offer is made, it can hardly be said to be bona fide.Under those circumstances you would have to show that
light duty was reasonably available but for the terminationfor cause.
However, once the claimant returns to work at the pre-injury AWW, the issue of a bona fide offer of employmentbecomes moot as disability has ended. A claimant can thenonly reestablish disability based upon a change in conditionor a showing that he is unable to obtain employment at thepreinjury AWW due to the injury. This generally requiresan affirmative and unsuccessful job search on the part ofthe claimant. On the other hand, if the claimant was offeredless than the preinjury AWW, you should have alreadybeen paying partial TIBs. Those would continue as theclaimant has, by definition, disability.
In that latter situation, the question becomes whether youare required to increase the TIBs to the full amount. Thatwould depend on whether the activity causing the terminationoccurred before or after the claimant returned to work. Ifthe offense occurred prior to the offer, then the claimantwould probably be due full TIBs as the claimant hasdisability, and the employer is effectively withdrawing theoffer. If it occurred after the offer, then you can argue thatthe claimant’s actions effectively were a rejection of theoffer.
I have been told that we can offer a bona fide joboffer on restrictions provided by an RME doctor.Is that correct?
The statute provides no limitation on the status ofthe doctor who has released the claimant. Anylimitation is imposed solely by rule. That rule,
Rule 129.6, is somewhat inconsistent. Under subsection(b) an offer may be made on the basis of a report from anydoctor who has actually examined the claimant, as long asthe treating doctor does not specifically disagree with thoserestrictions Subsection (f) then provides an order ofpreference. Since a TWCC RME trumps a treating doctorunder that section, we know that subsection (b) cannot beread to limit offers as such an interpretation would createan irreconcilable conflict. Further, Section 408.0041(e),added after the effective date of Rule 129.6, also allows anemployer to make a bona fide offer on the basis of adesignated doctor’s release. Therefore, it is our positionthat an employer may make a bona fide offer of employmentbased upon the report of an RME and that it is a fact issuefor the hearing officer as to whether the doctor’s restrictionsare credible. Please see the editor’s comments to this rulein the FOL Manual for much greater discussion of thispoint.
A
Q
A
Q
Q
A
A

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-9-FOLIOI have a claimant who prevailed at the CCH. Weowe him benefits. He owes attorney’s fees and 2separate child support orders. The attorney’s
fees total owed exceed 25% of the amount owed. I knowthat I only send the claimant’s attorney 25%. What I wantto know is how do we calculate the amount owed on thechild support orders. One order states that a deductionshould be taken weekly (due to arrears) and another orderalso states an amount owed weekly (again due to arrears).What I really need to know is what do I pay for childsupport and is there some rule on how to determine whogets what amount.
1). First, pay usual attorneys fee lien. They takeprecedence.
2). Then pay child support lien out of any income benefits,including TIBs.
3). Pay up to 50% of weekly benefits to fund current childsupport obligation until further order.
4). Pay up to 100% of benefits if the order is for the purposeof reimbursing accrued child support arrearage until theamount has been fully reimbursed. After accrued arrearageis fully paid, contact the Child Support Division at thenumber indicated on the notice to determine if a furtherbalance has accrued. If not, resume payments to worker.Otherwise, continue payments per notice of lien.
5). Order of withholding should direct whether lien is forcurrent or arrearage and if does not, we should assume thatwe pay no more than 50% of weekly benefit per week.
6). If we have a D&O from TWCC, and if we are orderedto pay a lien, and if it does not specify whether it isarrearage or current, then we should assume current, andshould withhold 50% of weekly benefits times the numberof weeks that we have had order of withholding to the dateof payment. n
Q
A
TDI Announces 2004Workers’ Compensation
RelativitiesAccording to the Texas Department of Insurance
(TDI,) the Workers Compensation Relativities for calendaryear 2003 must continue to be used. Their website states“Relativities will not be amended 1/1/2004. 1/1/2003Relativities will apply.” For further information, pleasereview relativity-related information at TDI’s websiteusing this link: http://www.tdi.state.tx.us/company/wcrate03.html
Additionally, a TDI representative has posted anelectronic advisory about the relativities information. Hisbulletin can be found at http://www.tdi.state.tx.us/commish/bulletins/b-0040-3.html. It states that “Notice is herebygiven that the January 1, 2003 workers’ compensationclassification relativities and other rating values in theTexas Basic Manual of Rules, Classifications andExperience Rating Plan for Workers’ Compensation andEmployers’ Liability Insurance will not be amendedeffective January 1, 2004.”
All insurance companies must either use the January1, 2003 classification relativities adopted byCommissioner’s Order No. 02-1122 or company-specificclassification relativities that have been filed with theTexas Department of Insurance (Department).
If your organization is affected by this information, weencourage you to contact TDI for further clarification.Questions regarding this matter should be referred toTDI’s Property and Casualty Actuarial Division at (512)475-3017 or by e-mail at [email protected]. nn
TDI Completes QuarterlyMandatory Data Call
Survey
TDI recently completed its mandatory data call forworkers compensation deductible plans. The data call wasrelated to 2003, third quarter experience information. TDIpublished information about this data call on its website athttp://www.tdi.state.tx.us/general/pdf/b-0036-3.pdf. Thedata call was to be completed by 11/15/03. If yourcompany was required to complete this data call and hasnot done so, please contact TDI for further clarification.Further information about this data call is available at theabove link. n
FOL Annual Seminar
Set for: Dallas and Houston
Need more information? Contact [email protected]

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-10- FOLIO
FLAHIVE, OGDEN & LATSON DIRECTORY
KEY TASK DIRECTORY
Allain Collins 435-2170 867-1715 APC Sharon Youso 435-2233
Bobby Stokes 435-2150 867-1705 RDS Anita Drake 435-2249
Carlos Acosta 435-2177 867-1712 CA1 Sally Stephens 435-2242
Chuck Finch 435-2158 867-1713 CCF Ryan Wimble 435-2264
Dana Gannon 435-2151 867-1710 DMG Margo Davis 435-2263
Greg Solcher 435-2175 867-1718 GDS Sally Stephens 435-2242
Jack Latson 435-2156 867-1724 JWL Patsy Shelton 435-2234
James Sheffield 435-2169 867-1703 JRS Sharissa Karol 435-2224
Katie Flahive 435-2168 867-1702 KMF Gina Mitschke 435-2229
Kevin MacEwan 435-2166 867-1706 KEM Cynthia Sherman 435-2274
Lynette Phillips 435-2165 867-1708 LLP Karen VanLoo 435-2240
Nancy Ippolito 435-2181 867-1735 NHI Anita Drake 435-2249
Pamela Peavy 435-2163 867-1736 PEP Rita Paul 435-2250
Paul Stone 435-2157 867-1716 PBS Bronna Sanders 435-2269
Paul Warren 435-2159 867-1719 PDW Kiran Hashmi 435-2225
Rebecca Strandwitz 435-2160 867-1720 RMS Bronna Sanders 435-2269
Rhett Robinson 435-2154 867-1709 SRR Marilyn Mueller 435-2236
Rob Dollars 435-2164 867-1707 RAD Karen VanLoo 435-2240
Ron Johnson 435-2178 867-1722 RMJ Ryan Wimble 435-2264
Roy Leatherberry 435-2179 867-1714 RJL Andrea Tuttle 435-2238
Scott Bouton 435-2153 867-1737 SDB Marilyn Mueller 435-2236
Steve Tipton 435-2162 867-1704 SMT1 Mary Casebier 435-2275
Susan Veltman 435-2152 867-1717 SRV Sharon Durr 435-2230
Tom Wilkins 435-2183 867-1727 TRW Gina Mitschke 435-2229
Tricia Blackshear 435-2180 867-1723 PHB Lisa Black 435-2260
Attorneys Direct Dial(512)
Direct Fax*(512)
E-Mail **[email protected]
Paralegal Paralegal(512)
*Attorney's direct dial fax no. is directed to his/her paralegal.** Alternative e-mail address: first initial+last [email protected] (Example: [email protected])
Admin. Violations Dianne Townsend 435-2289 867-1724 DLT
BRC Settings (FO&L - Req. For Evid.) Cindi Friedel 435-2244 477-4987 CAF
Disputed Claims (TWCC-21) Tillie Aguirre 435-2235 477-4996* TAA
General Questions Receptionist 477-4405 867-1700 GQS
Insurance Coverage (TWCC-20) Phyllis Devine 435-2267 867-1748 PAD
Med Review Disputes Annette Moffett 435-2266 867-1733 AMM
Records Request/Photostats Phyllis Devine 435-2267 867-1748 PAD
Request for BRC (TWCC-45) Tillie Aguirre 435-2235 477-4996 TAA
Designated Doctor Filings Brandi Senters 435-2251 479-5319 BES
TWCC Manual Sales Joel Ogden 435-2256 472-9160 JMO
*#2 TWCC-21 fax # Tillie Aguirre 435-2235 472-4935* TAA
Task Direct Dial(512)
Direct Fax(512)
ContactPerson

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-11-FOLIO
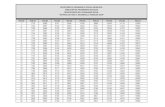
Interest CalculatorFirst Quarter
4.76%
12
3
4
5
"X" Value Weeks "X" Value Weeks "Y" Value Weeks "Y" Value0.0014 27 0.3456 1 0.0009 27 0.02470.0032 28 0.3711 2 0.0018 28 0.02560.0060 29 0.3976 3 0.0027 29 0.02650.0096 30 0.4250 4 0.0037 30 0.02750.0142 31 0.4533 5 0.0046 31 0.02840.0197 32 0.4825 6 0.0055 32 0.02930.0261 33 0.5126 7 0.0064 33 0.03020.0334 34 0.5437 8 0.0073 34 0.03110.0416 35 0.5756 9 0.0082 35 0.03200.0507 36 0.6085 10 0.0092 36 0.03300.0607 37 0.6423 11 0.0101 37 0.03390.0717 38 0.6769 12 0.0110 38 0.03480.0836 39 0.7125 13 0.0119 39 0.03570.0964 40 0.7491 14 0.0128 40 0.03660.1100 41 0.7865 15 0.0137 41 0.03750.1247 42 0.8248 16 0.0146 42 0.03840.1402 43 0.8641 17 0.0156 43 0.03940.1566 44 0.9042 18 0.0165 44 0.04030.1739 45 0.9453 19 0.0174 45 0.04120.1922 46 0.9873 20 0.0183 46 0.04210.2114 47 1.0302 21 0.0192 47 0.04300.2315 48 1.0740 22 0.0201 48 0.04390.2525 49 1.1188 23 0.0211 49 0.04490.2744 50 1.1644 24 0.0220 50 0.04580.2972 51 1.2110 25 0.0229 51 0.04670.3209 52 1.2584 26 0.0238 52 0.0476
NOTE: For partial weeks, round up to next week (8 2/7ths weeks = 9 weeks).
Determine number of weeks of continuous payment owed. Find corresponding “X” value on chart.
TIBs: Calculate interest from the 7th day after first day benefits began, or the 7th day after the first notice, whichever is LATER.
Calculate interest from the 5th day after notice of the certification of MMI and impairment, or the date of a CARRIER dispute of MMI or impairment, whichever is EARLIER.
IIBs:
Interest Rate Effective from 1/1/2004 through 3/31/2004:
Determine total benefits plus interest owed by adding interest from steps 2 and 4, and adding total benefits to be paid.
Multiply “Y” by the total benefits owed (not including interest determined in steps 1 and 2 above). This is the approximate amount of interest owed from benefit ending date to payment date.
Determine number of weeks between ending date of payments and date benefits are to be paid. Find corresponding “Y” value on chart.
Multiply “X” by weekly compensation rate. This is the approximate amount of interest owed on the ending date of benefits.
2526
6789
10111213
21222324
1920
5
14151617
4
23
18
Weeks1
Accumulated Interest from Beginning to End of Continuous Payment
Accumulated Interest from End of Payment Period to Date Paid

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-12- FOLIO
APPEALS PANEL DECISIONS
Texas Workers' Compensation Commission Appeal No. 032769With regard to hearings conducted after July 27, 2003, involving impairment ratings for spinal surgery which wouldbe affected by TWCC Advisory 2003-10, it is an error not to consider and apply that advisory.
Facts: Following the occurrence of a back injury, the claimant was ultimately seen by a designated doctor,Dr. P. Dr. P initially determined that the claimant had not reached maximum medical improvement. After a subsequentexamination, Dr. P determined that the claimant reached maximum medical improvement August 19, 2002 with animpairment rating of zero percent. The claimant then underwent a two-level lumbar fusion in January of 2003. TheTWCC provided additional information concerning this surgery to the designated doctor with a request for comment.Dr. P responded by indicating that her opinion remained unchanged. Subsequently the TWCC issued Advisory 2003-10, effective July 22, 2003 which provided in part the following: “Multilevel fusion meets the criteria for [Diagnosis-Related Estimate (DRE)] Category IV, Structural Inclusions, as this multilevel fusion is equivalent to ‘multilevel spinesegment structural compromise’ per DRE IV.”
The Hearing Officer determined that the claimant reached MMI on August 19, 2002 with an impairment ratingof zero percent as determined by the designated doctor. The claimant appealed.
Holding: Reversed and remanded. “We have previously held that with regard to hearings conductedafter July 22, 2003, involving impairment ratings for spinal surgery which would be affected by TWCC Advisory 2003-10, it is error not to consider and apply that advisory.” The Appeals Panel remands with instructions to seek aclarification from the designated doctor with specific instructions to “consider and apply Advisory 2003-10.”
Texas Workers' Compensation Commission Appeal No. 032689A claimant’s satisfactory participation with TRC or work at a job relatively equal to his/her abilities during anyportion of the qualifying period satisfies the requirements of Rule 130.102 establishing a good faith effort to findemployment commensurate with the employee’s ability.
Facts: At issue was the claimant’s entitlement to supplemental income benefits for the second, third and fourthcompensable quarters. The evidence established that during the qualifying period for the second quarter the claimantmade no job search efforts. During the qualifying period for the third quarter the evidence established contact with theTexas Rehabilitation Commission. That involvement with TRC included the creation of an individualized plan foremployment identifying an employment goal, steps to achieve the goal, a description of the services to be provided orarranged and the start and end dates for the described services. The records from TRC further established that the TRChad provided payment for “job placement services” from a service provider. A letter from an employee of the serviceprovider indicated that the claimant was active with the provider, remained in contact with a counselor employed by theprovider “at least three times a week for possible employment,” provided a list of possible employers to the claimantand performed follow up with the employers after the claimant contact. The evidence further indicated that the claimantfound a job through one of these contacts.
The evidence further established that during the qualifying period for the fourth quarter, the claimant workedsome but not all of the weeks. She was initially working 39 hours per week. Her hours were later reduced to 15 hoursper week. According to the claimant the reduction resulted from the fact that her knees were worsening.
The Hearing Officer determined that the claimant did not establish a good faith effort to find employment duringthe qualifying period for any of the three quarters. The claimant appealed.
Holding: Affirmed in part, reversed and remanded in part. The Appeals Panel affirms the HearingOfficer’s determination with respect to the second quarter. The Hearing Officer’s decision regarding the third and fourthquarters was reversed. The Appeals Panel notes that there was evidence of participation with TRC during at least aportion of the qualifying period for the third quarter. The Panel “would note that if claimant was satisfactorilyparticipating in such a TRC program during any portion of the qualifying period, then she has satisfied (Rule130.102(d)(2)).” They remand with instructions that, “If the Hearing Officer finds that claimant was not acting in goodfaith regarding TRC participation, she should explain her reasoning.”

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-13-FOLIOThe Appeals Panel made similar determinations with respect to the fourth quarter noting that the claimant did
work either full or part-time during several weeks of the qualifying period. “If the Hearing Officer finds that claimantworked relatively equal to her ability to work during the six weeks when claimant testified that she worked 39 hours perweek, then the Hearing Officer can find that claimant has satisfied the Rule.” The Panel further states that, “If claimantreturned to work relatively equal to her ability to work during any portion of the qualifying period, the claimant doesnot then have to establish that she also searched for work during the period of time during the qualifying period whenshe was not working relatively equal to her ability to work.”
CASE DECISIONSTEXAS COURT OF APPEALS
Truck Insurance Exchange v. Smetak, 102 S.W3d 851 (Tex.App.—Dallas 2003, no pet.h.)Facts: Claimant, while employed as a carpenter, was carrying tools at a construction site, and stepped on a piece
of cardboard on stairs. He slid down the stairs and struck his foot on a wall at the bottom of the stairs. He was initiallydiagnosed with an ankle sprain, and then he developed an infection caused by methicillin resistant staphylococcus aureus(MRSA). At the CCH, the Hearing Officer found that claimant had sustained a compensable injury in the course andscope of his employment. The Appeals Panel affirmed, and the carrier appealed to the district court. On behalf of thecarrier, a physician testified that the infection could only enter his body through a break in the claimant’s skin, and therewere no noted cuts or abrasions by the treating doctors. A jury found that the claimant had sustained a compensableinjury, including the staff infection.
To the appellate court, the carrier argued that the trial court should not have admitted the Appeals Panel decisionbecause it was hearsay and did not meet the public records exception to the hearsay rules because the decision was basedon inadmissible conclusions.
Holding: Rejecting this argument, the appellate court held that if properly authenticated, reports from a publicagency, such as an Appeals Panel decision, which set forth the activities of the agency and report observations aboutwhich the agency has a duty to report, are admissible under the public records exception to hearsay. Because the AppealsPanel decision met this criteria, it was found to be admissible.
Exxon Corp. v. Makofski, 116 S.W.3d 176 (Tex. App.—Houston [14th Dist.] 2003)Facts: Plaintiffs alleged that exposure to benzene caused acute lymphocytic leukemia. On behalf on plaintiffs,
a toxicologist testified that exposure to benzene caused the leukemia, based upon a 51% certainty. Current epidemiologystandards require a 95% certainty. A district court jury awarded damages to the plaintiffs. The defendant appealed onthe basis that the plaintiffs’ experts lacked scientific basis for their opinions regarding causation.
Holding: The Court of Appeals held that the expert’s testimony was legally insufficient under the currentepidemiology standards. Additionally, because an expert had reinterpreted an inconclusive study by adding his own data,it was determined that unreliable expert evidence constituted no evidence, which mandated reversal of the decision.
TIG Premier Insurance Company v Pemberton, 2003 WL 23120102, 10th Court of Appeals - WacoFacts: Claimant fell over a railing, injuring his right shoulder and left knee. The carrier did not contest the
compensability of claimant’s injury. Claimant subsequently was diagnosed with deep vein thrombosis (DVT), or bloodclots, in his right leg. He was assessed with a 10% impairment rating, 2% of which was for the DVT. Six months later,the carrier filed a dispute stating that the DVT was not caused by the fall and was not compensable. The TWCC heldthat although the claimant had not shown a causal relationship between the fall and the DVT, the carrier had waivedthis dispute by not raising it within 60 days of learning of the doctor’s findings. The carrier appealed to a district court,and the trial court granted summary judgment for the claimant.

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-14- FOLIOHolding: Carrier appealed the waiver issue; however, the claimant did not appeal the findings regarding the
lack of causal relationship. The appellate court reversed summary judgment, and rendered for the carrier. The court heldthat §409.021(c)—the statute requiring a carrier to contest an injury within 60 days of learning of it—did not applybecause that statute pertains only to whether the carrier disputes the overall injury after initially learning of an employee’sclaim. Disputes that arise later about the extent or specific aspects of the injury are not subject to the 60-day rule. Theappellate court also held that because the claimant had not appealed the findings regarding the lack of causation, theTWCC decision on that matter became final and binding.
Hartford Underwriters Insurance Company v. Hafley, 96 S.W.3d 469 (Tex. App.—Austin, 2002, no pet. h.)Facts: Claimant was a resident of New Braunfels in Guadalupe County. Claimant sustained a compensable
injury and became eligible for Supplemental Income Benefits (SIBs). He brought a claim for the 6th quarter of SIBs.At the time of his injury, the claimant was earning wages. However, during the 6th quarter, he was self-employed. Atthe CCH on the 6th quarter, claimant submitted into evidence both his gross income and his business expenses, in theform of receipts and testimony from accountants. The Hearing Officer calculated his post-injury earnings (PIE) basedupon his “net income—the difference between his total self-employment income and his expenses. This determinationwas affirmed by the Appeals Panel. The carrier appealed in Comal County, based on the claimant’s original filing.Carrier argued that claimant’s PIE should be based upon his gross earnings. The trial court ruled in claimant’s favorand awarded him attorney’s fees.
Holding: The carrier appealed the trial court decision regarding the PIE, and appealed the award of attorney’sfees because the claimant did not prevail on any issue listed in the attorneys fees provisions. The claimant appealedarguing that the district court should have dismissed the carrier’s case for want of jurisdiction because he was a residentof Guadalupe County. The appellate court held that §410.252 addresses venue only and not subject-matter jurisdiction.Therefore, it held that Comal County had jurisdiction to review the TWCC decision. The appellate court, with respectto the wages calculation issue, noted that the legislature did not provide a method for calculating the earnings of a self-employed claimant. The court found that TWCC had discretion to choose a method for calculating earnings under thecircumstances. With respect to the attorneys fees, the appellate court found that the claimant’s attorney was entitled tofees because the TWCC had awarded SIBS benefits to the claimant, and that was a final decision and issue on whichhe prevailed.
LeBlanc v. Everest National Insurance Company, 98 S.W.3d 786 (Tex. App.—Corpus Christi 2003, no pet. h.)Facts: Claimant unsuccessfully sought benefits at a Contested Case Hearing. The Appeals Panel affirmed the
decision. She was not represented, but began seeking an attorney to represent her in an appeal to the district court. Afterbeing rejected by approximately 27 attorneys, claimant found an attorney willing to take her case. That attorney filedsuit on January 31, 2001; however, that was one day late. The trial court granted summary judgment to the carrier onthe basis that the suit was not timely filed.
Holding: Claimant appealed, arguing that the jurisdictional requirements of the Act should be liberallyconstrued in her favor. The Court of Appeals affirmed, holding that a petition for appeal from a TWCC decision thatwas filed one day late would not be treated as timely filed because the statutory 40-day deadline for filing an appeal within§410.252 was mandatory and jurisdictional.
McGatlin v. Hartford Insurance Company of Texas, 94 S.W.3d 311 (Tex. App.—Texarkana 2002, no pet. h.)Facts: Claimant alleged a work injury and pursued her claim through the TWCC. Both parties appealed the
Hearing Officer’s decision, and the Appeals Panal affirmed in 1999. The Appeals Panel stated that the carrier had timelyresponded to the claimant’s appeal; however, the claimant had not timely responded to the carrier’s appeal. To theAppeals Panel, claimant filed a request to reconsider its determination.
Before the Appeals Panel responded to the request to reconsider, claimant filed an appeal in district court.Subsequently, in 2000, the Appeals Panel granted claimant’s request for reconsideration, and issued a new opinion,holding that claimant’s appeal was timely filed; however, the CCH decision was affirmed. Claimant did not appeal the

CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
-15-FOLIOAppeal Panel’s 2000 decision. Subsequently, the carrier argued that the district court did not have jurisdiction to hearthe claimant’s case involving the 1999 decision because the 2000 decision was the final decision of the Appeals Panel.The trial court agreed with carrier, and dismissed claimant’s action.
Holding: Claimant appealed. The issue before the Court of Appeals was whether TWCC had the authority toreconsider its Appeals Panel decisions, and whether the trial court erred in dismissing claimant’s action. The Court ofAppeals reversed and remanded for further proceedings. The court noted that Chapter 410 neither expressly prohibitsnor permits such reconsideration. The court noted that §410.206 authorizes the Appeals Panel to correct clerical errors.The court interpreted the 2000 decision as a correction of a clerical mistake; therefore making the second decisionretroactive to the 1999 decision. On that basis, the appellate court held that the claimant had properly appealed the 1999decision, and that the trial court had erred in dismissing her appeal.
Sunset ReviewContinued from p. 1
being “routinely denied” by many insurance carriers. Oneof the issues that seemed to trouble the committee is whyan insurance carrier can deny a doctor’s bill based upon apeer review report. There was some concern that anincrease in the number of denials was prima facie evidence
We have been receiving a new class of Compliance &Practices Referral Notices not encountered before.
TWCC is beginning to notify an insurance carrier ifTWCC receives a complaint about an individual adjuster.The intake complaint is attached to the notice. An exampleof a complaint described to TWCC is: “The claimant iscomplaining his adjuster is being extremely rude and liedthat she has not received documentation and claimantknows she was reading the documentation word-by-wordbecause he had the same document.”
This type of notice simply forwards the notes taken bythe Compliance & Practices referral person at TWCC. Itdoes not establish that the complaint is valid. There is noinformation as to whether the particular complainant is aperson who has also complained about TWCC. Thatinformation may be available through a request for theDRIS logs about the particular claimant.
TWCC has indicated no intention to take an action asa result of these referrals. They are simply communicatedto the carrier with the following notice:
This allegation has been recorded for future referencein performance evaluation and profiling of XZY Insurancecompany.
TWCC requests that the carrier review thecomplaint and take whatever appropriate action might beappropriate. n
New ComplianceReferrals
Important NewExclusive Remedy CaseIn Etie v. Walsh & Albert Company, the Court of
Appeals concluded that all contractors and subcontractorsinsured under the same policy were entitled to assert anexclusive remedy to the suit of an employee injured whileworking for one of the companies. This is an extremelyimportant new case.
The opinion was handed down by the Court of Appealson January 22, 2004. Sheldon Etie worked for WayEngineering Company. Way Engineering Company was asubcontractor on the job site. The general contractorpurchased a single workers’ compensation insurance policyto cover all subs and all employees working for subs at thatparticular building site.
Etie was injured due to the alleged negligence of anemployee of another contractor. Etie had recovered workers’compensation benefits, and the defendant contractorobtained a summary judgment holding that it was immunefrom Etie’s lawsuit. The court concluded that an agreementto provide coverage made the general contractor “theemployer of the subcontractor and subcontractor’semployees” for purposes of the Workers’ CompensationAct. All subcontractors and all employees of allsubcontractors became “employees.” Therefore, Etie’ssuit was a claim against the fellow employee, and barredunder the exclusive remedy provisions of the Act.
The importance of this case cannot be overstated. Ifaffirmed by the Supreme Court, for Owner ControlledInsurance Programs, it will afford very significant remediesto general contractors and subcontractors on job sites inTexas. n
that the denials are in bad faith. According to one newssource, the House Committee Chairwoman, Helen Giddingsof Dallas, “asked for assurances from Commission officialsthat insurance carriers are being punished.” n

Flahive, Ogden & LatsonP.O. Box 13367Austin, Texas 78711
FO&L Fax DirectoryTo help expedite your faxed information to the correct area within FO&L and get it to the responsible person at the earliest time, usethe following fax directory. Please remember the 3:30 p.m. receipt deadline for material required to be date stamped at theCommission. Material received after 4:00 p.m. does not permit time to deliver it across town prior to the Commission close.
Note: TWCC numbers are bolded.
CLIENT NEWSLETTER BY FLAHIVE, OGDEN & LATSON
FOLFOLFOL
Fax Number Attention To: Subject Matter:
(512) 477-4996 Tillie Aguirre Notice of Refusal (TWCC-21) or BRC Requests (TWCC-45)(512) 472-4935
(512)867-1748 Phyllis Devine Insurance Coverage (TWCC-20)Record ChecksPhotostats
(512) 867-1733 Annette Moffett Medical Review Disputes (TWCC-60)SOAH/Medical Review
(512) 867-1701 Patsy Shelton Advisory InformationExtra Hazardous Employer
(512) 867-1724 Dianne Townsend Compliance & Practices
(512) 479- 5319 Brandi Senters Designated Doctor Filings (TWCC-32)Suspension of TIBs (TWCC-34)
(512) 477-4987 Cindi Friedel BRC & PHC HearingsRFEs, Set Notices, Hearings,Files, Cancellations
(512) 867-1700 Paralegals All CCH-Related Info.
(512) 867-1700 FOL All materials not listed above
(512) 472-9160 Joel Ogden TWC Manual Orders & Information