Fluid and Electrolytes
-
Upload
icay-dela-pena-cabrera -
Category
Documents
-
view
524 -
download
3
Transcript of Fluid and Electrolytes


Blood, skin,
muscle
Skeleton
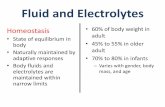
Fluid and Electrolytes- These are the liquid component of the human body that account for approximately
60% of the body weight of a typical adult.
Important functions
1. Maintenance of blood volume.
2. Cellular transport of vital substances such as oxygen and glucose.
3. Transport of cellular waste products to the lungs and kidneys for removal.
4. Lubrication and cushioning
5. Hydrolysis of food in the digestive system.
6. Reactant and medium for the chemical reactions in cells.
7. Maintenance of body temperature.
Factors that influence the amount of body fluid are as follows
Influencing Factor Parameter Amount
AgeOlder
Younger
GenderFemale
Male
Body fatAverage
Overweight
Amount of fluid in organs:
Fluid and electrolytes are found in body’s two different compartments:
> Intracellular – within the cell.
> Extracellular – outside the cell.
Approximately, two thirds of the fluid is in the intracellular
compartment and the remaining one third on the extracellular compartment.
Medical Surgical Nursing|

Newborn One Year Adult0
10
20
30
40
50
60
70
80
Column1 Extracellular Fluid
The Intracellular Compartment
- It is primarily located in the skeletal mass.
- It comprises two thirds of the fluid since 70% of a cell is water.
The Extracellular Compartment
- this compartment is further subdivided into:
Interstitial fluid space
o It contains the fluid that surrounds the cell and totals about 11-12L in an
adult.
o It delivers materials as well as removal of body waste.
o It also plays a role in intercellular communication.
Intravascular fluid space
o This makes up the fluid within blood vessels. Approximately 3L of the
average 6L of blood volume is made up of plasma. The remaining 3L then
comprises the erythrocytes, leukocytes, and thrombocytes.
Transcellular fluid space
o This makes up 1% to 3% of body weight or approximately 1L of fluid. It
includes the following:
● Digestive fluid● Pericardial fluid● Pleural fluid● Synovial fluid● Lymphatic fluid● Intraocular fluid● Cerebrospinal fluid
o Large amount of fluid in this space can become sequestered. This event is
what we call “third spacing” . In this event, the fluid is not available for
Medical Surgical Nursing|

exchange between compartments or spaces not because of fluid loss.
*Body fluid normally shifts between the two major compartments or spaces in an effort to maintain equilibrium between the spaces ultimately leading to homeostasis that is crucial for life.
Electrolyte Normal Range (mEq/L) FunctionsSodium (Na+)
Intravascular
142
Interstitial
146Intracellula
r
15
● Exerts an extracellular osmolality, thereby regulating movement of body fluids.
●Facilitates nerve impulses through active transport and the sodium-potassium pump
Potassium (K+)
5 5 150
●Maintains nervous impulse conduction in the heart
●Promotes skeletal muscle function
●Plays a small role in osmotic regulation
●Assists with acid-base regulation
Chloride (Cl-)
102 114 1
●Maintains electroneutrality by passively following the positively charged ions
● Helps regulate osmotic pressure differences between intracellular and extracellular fluid compartments
●Regulates body water balance with sodium
● Combines with H+ in gastric mucosal cells to make hydrochloric acid.
Calcium (Ca2+) 5 3 2
● Major structural component of bones and teeth
● Plays a role in blood coagulation
● Promotes muscle contraction and nervous impulse transmission
● Decreases neuromuscular irritability
Phosphorous (PO4+) 2 2 100
● A structural component of bones and teeth
● Helps maintain acid-base balance
● Energy production (ATP)
● Delivery of oxygen to tissues as a component of 2.3-DPG
Medical Surgical Nursing|

Magnesium (Mg2+) 2 1 27
● Ensures the cross-membrane transport of sodium and potassium in the sodium-potassium pump
● Promotes neuromuscular excitability
● Plays role in heart contraction
● Facilitates transmission of central nervous system impulses
●Part of many enzymatic reactions for carbohydrate and protein metabolism
Regulation of Fluid Body CompartmentsFluid shifts from through the membrane from region of low solute concentration until
the solutions are of equal concentration. This diffusion of water caused by a fluid
concentration gradient is known as osmosis.
In osmosis, the magnitude of force depends on the number of particles dissolved in
the solutions, not on their weights. The number of dissolved particles contained in a unit of
fluid determines the osmolality of a solution which influences the movement of fluid
between the fluid compartments.
OSMOSIS. Movement of fluid from area of lower solute concentration to an area of higher
solute concentration with eventual equalization of the solute concentrations.
Osmolality expresses the concentration of a solution in terms of how strongly it can
attract water across a membrane. Expressed in osmoles (the amount of molecules/ions in
solution) or milliosmoles per kilogram (mOsm/kg) of the solution, plasma osmolality
averages 290 +/- 5 mOsm/kg.
Tonicity is the ability of all the solutes to cause an osmotic driving force that
promotes water movement from one compartment to another. It determines the normal
state of cellular hydration and cell size. Sodium, glucose, and mannitol do not readily cross
the cell membrane and are therefore effective osmoles affecting water movement.
Medical Surgical Nursing|

osmotic pressurehydrostatic pressure
Three other terms are associated with osmosis:
● Osmotic pressure – is the amount of hydrostatic
pressure needed to stop the flow of water by osmosis. It
is primarily determined by the concentration of solutes.
● Oncotic pressure – is the osmotic pressure exerted by
proteins i.e. albumin.
● Osmotic dieresis – is the increase in urine output
caused by the excretion of substances such as glucose,
mannitol, or contrast agents in the urine.
Diffusion is the natural tendency of a substance to move
from an area of higher concentration to one lower concentration. It occurs through the
random movement of ions and molecules.
Examples of diffusion are the exchange of oxygen and carbon dioxide between the pulmonary capillaries and alveoli and the tendency of sodium to move from the ECF compartment, where the sodium concentration is high, to the ICF where the concentration is low.
Filtration
Hydrostatic pressure in the capillaries tends to filter fluid out of the intravascular
compartment into the interstitial fluid. Water and solute movement occurs from an area of
high concentration area to an area of low hydrostatic pressure. This allows the kidneys to
filter 180L of plasma per day.
Another example of filtration is the passage of water and electrolytes from the
arterial capillary bed to the interstitial fluid. In this instance, the hydrostatic pressure is
furnished by the pumping of the heart.
Sodium-Potassium Pump
Since sodium has a greater concentration in the ECF than that of the ICF, it tends to
enter the cell by diffusion. This tendency is offset by the sodium-potassium pump which is
located in the cell membrane and actively moves sodium from the cell into the ECF.
Conversely, the high intracellular concentration of potassium is maintained by
pumping potassium into the cell.
Medical Surgical Nursing|

Normal Gains and Loses of Fluid and Electrolytes
A healthy normal person body fluids are constantly being lost and replaced. Water
and electrolytes are gained and lost in various ways and different routes.
Kidneys
This organ is responsible in excreting fluids in the form of urine and accounts for
approximately 1 to 2L in a typical adult. A general rule is that the output is approximately
1mL of urine per kilogram of body weight per hour (1mL/kg/h) in all age groups.
Skin
Sensible perspiration refers to visible water and electrolyte loss through the skin
(sweating). The chief solutes in sweat are sodium, chloride, and potassium. Actual sweat
losses can vary from 0 to 1000 mL or more every hour depending on the environmental
temperature. Continuous water loss by evaporation (approximately 600mL/day) occurs
through the skin as insensible perspiration, a non-visible form of water loss. Fever
greatly increases insensible water loss through the lungs and the skin, as does of the natural
skin barrier i.e. major burns.
Lungs
The lungs normally eliminate water vapor (insensible loss) at a rate of approximately
400mL every day. The loss is much greater with increased respiratory rate or depth, or in a
dry climate.
Gastrointestinal Tract
Eight liters of fluid circulates through the GI tract every 24 hours but has the usual
loss of only 100-200mL daily. This happens because the bulk of the fluid is normally
reabsorbed in the small intestine.
Approximate values of average gains and losses
Average Daily Intake and Output in an Adult
Intake (mL) Output (mL)
Medical Surgical Nursing|

Oral Liquids 1200-1300 Urine 1500
Water in Food 1000 Stool 150-200
Metabolism 300 Insensibl
e
Lungs 300-350
Skin 500-600
Total 2500-2600 Total 2500-2600
Laboratory Tests for Evaluating Fluid Status
Osmolality
It is the concentration of fluid that affects the movement of water between fluid
compartments by osmosis. It also measures the solution’s ability to create osmotic pressure
and affect the movement of water. It is expressed as milliosmoles per kilogram of water
(mOsm/kg).
Osmolarity is another term that describes the concentration of solutions but osmolality is
more commonly used in clinical practice. It is expressed as milliosmoles per liter of solution
(mOsm/L)
Serum osmolality primarily reflects the concentration of sodium, although blood
urea nitrogen (BUN) and glucose play a major role in determining serum osmolality.
Plasma osmolality- it is useful to measure
this because plasma osmolality is the main
regulator of the release of antidiuretic
hormone (ADH), which plays a major role in
water regulation. Since sodium predominates
in the ECF, plasma osmolality can be estimated by bedside by doubling the serum sodium
level or by using the formula:
Na+ x 2 = Glucose + BUN 18 3 *approximate value of serum osmolality
Urine osmolality- determined by urea, creatinine, and uric acid. When measured with
osmolality, urine osmolality is the most reliable indicator of urine concentration.
Urine specific gravity- measures the kidneys’ ability to excrete or conserve water. The
specific gravity of urine of compared to the weight of distilled water, which has the specific
gravity of 1.000. Normal range for specific gravity is 1.010 to 1.025. Urine specific gravity
can be measured in two ways:
By placing a calibrated hydrometer or urinometer in a cylinder of approximately
20mL of urine.
Medical Surgical Nursing|
Osmolality Normal Range
Serum/Plasma 275-300 mOsm/kg
Urine 250-900 mOsm/kg

By using refractometer or dipstick with a reagent for this purpose.
Specific gravity varies inversely with urine volume: normally, the larger the volume of the
urine, the lower the specific gravity. Specific gravity is a less reliable indicator of urine
concentration than that of the urine osmolality since increased glucose or protein can falsely
elevate specific gravity.
Factors Affecting Serum and Urine Osmolality
Fluid Increasing Osmolality Decreasing Osmolality
Serum
(275-300 mOsm/kg water)
● Severe dehydration
● Free water loss
● Diabetes insipidus
● Hypernatremia
● Hyperglycemia
● Stroke or head injury
● Renal tubular necrosis
● Consumption of methanol
● Fluid volume excess
● SIADH
● Renal failure
● Diuretic use
● Adrenal insufficiency
● Hyponatremia
● Overhydration
●Paraneoplastic syndrome
Urine
(250-900 mOsm/L water)
● Fluid volume deficit
● SIADH
● Congestive heart failure
● Acidosis
● Fluid volume excess
● Diabetes insipidus
● Hyponatremia
● Aldosteronism
● Pyelonephritis
Blood Urea Nitrogen (BUN)
It is the end product of the metabolism of protein (from both muscle and dietary
intake) by the liver.
The normal BUN is 10 to 20 mg/dL (3.6 to 7.2 mmol/L). The BUN level varies with
urine output.
Factors that increase BUN includes: Factors that decrease BUN
includes:
● Decreased renal function ● End-stage liver disease
● Gastrointestinal bleeding ● Low protein diet
● Dehydration ● Starvation
● Increased protein intake ● Conditions that expand fluid
volume
● Fever
● Sepsis
Creatinine
It is the end product of muscle metabolism. It is a better indicator of renal function
than BUN since it does not vary with protein intake and metabolic state. The concentration
however depends on lean body mass and therefore varies from person to person. The
normal serum creatinine is approximately 0.7 to 1.4 mg/dL (62 to 124 mmol/L) Creatinine
levels increase when renal function decreases.
Medical Surgical Nursing|
Amino acid
Ammonia molecule
sUrea
Excretion through
urine

Hematocrit
It measures the volume percentage of red blood cells (erythrocytes) in whole blood
and normally ranges from 42% to 52% for males and 35% to 47% for females.
Urine Sodium Values
It changes with sodium intake and the status of fluid volume: as sodium intake
increases, excretion increases and as the circulating fluid volume decreases, sodium is
conserved.
Normal urine sodium levels range from 75 to 200 mEq/24 h (75 to 200 mmol/24 h).
A random specimen usually contains more than 40 mEq/L of sodium. Urine sodium levels
are used to assess volume status and are useful in the diagnosis of hyponatremia and acute
renal failure.
Homeostatic Mechanisms
Kidney Functions
The kidneys normally filter 170 L of plasma every day in adult while excreting only
1.5 L of urine. Major functions of the kidneys in maintaining normal fluid balance include
the following:
Regulation of the ECF volume and osmolality by selective retention and excretion
of body fluids.
Regulation of electrolyte levels in the ECF by selective retention of needed
substances and excretion of unneeded substances.
Regulation of pH of the ECF by retention of hydrogen ions.
Excretion of metabolic wastes and toxic substances.
*For geriatric patients, there may substantially reduced renal function therefore there may
be high-normal or minimally elevated creatinine levels.
Heart and Blood Vessel Functions
The pumping action of the heart circulates blood through the kidneys under sufficient
pressure to allow for urine formation. Failure of this pumping action interferes with renal
perfusion and thus with water and electrolyte regulation.
Lung Function
Through exhalation, the lungs remove approximately 300 mL of water daily in the
normal adult. Abnormal conditions, such as hyperpnea (abnormally deep respiration) or
Medical Surgical Nursing|
Increase in hematocrit DehydrationPolycythemia
Decrease in hematocrit OverhydrationAnemia

continuous coughing increases fluid loss; mechanical ventilation with excessive moisture
decreases the loss.
Also, the lungs play a major role in maintaining acid-base balance.
Pituitary Functions
The hypothalamus manufactures ADH, which is stored in the posterior pituitary
gland and released as needed. ADH is sometimes called the water conserving hormone
because it causes the body to retain water.
Adrenal Functions
Aldosterone, a mineralocorticoid secreted by the zona glomerulosa of the adrenal
cortex, has a profound effect on fluid balance. Increased secretion of aldosterone causes
sodium retention and thus, water retention and potassium loss; conversely, decreased
secretion of aldosterone causes sodium and water loss and potassium retention.
Parathyroid Functions
This organ embedded in the thyroid gland, regulates calcium and phosphate balance
by means of the parathyroid gland (PTH). The PTH influences bone resorption, calcium
absorption from intestine, and calcium reabsorption from renal tubules.
Baroreceptors
These are small nerve cell receptors that detect changes in pressure within blood
vessels and transmit this information to the central nervous system.
Renin-Angiotensin-Aldosterone System
Aldosterone is a volume regulator and is also released as serum potassium increases, serum
sodium decreases, or adrenocorticotropic (ACTH) hormone increases.
Antidiuretic Hormone (ADH) and Thirst
ADH and thirst mechanism have important roles in maintaining sodium concentration
and oral intake of fluids. Oral intake is controlled by the thirst center located in the
hypothalamus. As serum concentration or osmolality increases or blood volume decreases,
neurons in the hypothalamus are stimulated by intracellular dehydration; thirst then occurs,
and the person increases her intake of oral fluids.
The absence or presence of ADH is the most significant factor in determining whether
the urine that is excreted is concentrated or dilute.
Medical Surgical Nursing|
Decreased renal perfusion
Release of renin by the juxtaglomerular cell in the kidneys.
Converts angiotensinogen found in
the liver into ANGIOTENSIN I
ANGIOTENSIN II in the lungs
VASOCONSTRICTION
Activates SNS thereby releasing ALDOSTERONE

SNS stimulatio
n
Angiotensin II
stimulation
Increased
arterial pressur
e
Atrial Natriuretic Peptide (ANP) also called atrial natriuretic factor
It is a 28-amino-acid peptide that is synthesized, stored, and released by muscle cells
of the atria of the heart in response to several factors.
Osmoreceptors
Located on the surface of the
hypothalamus, it changes sodium
concentration. As osmotic pressure
increases, the neurons become
dehydrated and quickly release impulses
to the posterior pituitary which increases
the release of ADH. The ADH then travels
in the blood to the kidneys, where it alters
permeability to water causing increased
reabsorption of water and decreased urine
output. The retained water dilutes the ECF
and returns its concentration to normal.
Restoration of normal osmotic pressure
provides feedback to the osmoreceptors
to inhibit further ADH release.
Fluid Volume Disturbances
HYPOVOLEMIA
Also known as fluid volume deficit it occurs when loss of ECF volume exceeds the
intake of fluid. It occurs when water and electrolytes are lost in the same proportion as they
exist in normal body fluids, so that the ratio of serum electrolytes to water remains the
same.
Medical Surgical Nursing|

It should not be confused with the term dehydration which refers to loss of water
alone, with increased serum sodium levels.
Third space fluid shifts or the movement of fluid from vascular system to other body
spaces also cause fluid volume deficit as in edema formation in burns or ascites with liver
dysfunction.
Clinical manifestations:
Acute weight loss Decreased skin turgor
Oliguria Cool, clammy skin related to peripheral
vasoconstriction
Postural hypertension Weak, rapid heart rate
Flattened neck veins Increased temperature
Thirst, anorexia, nausea, latitude Muscle weakness and cramps
Decreased central venous pressure Concentrated urine
Assessment and Diagnostic Findings:
Elevated BUN out of proportion to the serum creatinine (ratio greater than 20:1)
The cause can be identified through the patient’s health history and physical
examination
Increased hematocrit level since red blood cells become suspended in a
decreased plasma volume.
Electrolyte changes: sodium and potassium
● Hypokalemia occurs with GI and renal losses
● Hyperkalemia occurs with adrenal insufficiency
● Hyponatremia occurs with increased thirst and ADH release.
● Hypernatremia results from increased insensible losses and diabetes insipudus.
Urine specific gravity is increased in relation to the kidneys’ attempt to conserve
water and decreased with diabetes insipidus
Urine osmolality is greater than 450 mOsm/kg because the kidneys try to
compensate by conserving water.
Medical management
Medical Surgical Nursing|
Hypovolemia
vomiting, diarrhea,
suctioning, sweating
decreased intake or inability to gain access to
water
diabetes insipidus, adrenal
insufficiency, osmotic diuresis, hemorrhage, and
coma

The ultimate goal is to replace the lost fluid and electrolyte and the health care
provider plans for the maintenance requirements of the patient. If the deficit is not very
severe, the oral route is preferred, provided that the patient can drink.
However, if the fluid losses are acute or severe, the intravenous route is required.
Isotonic Intravenous Fluids
Solution Common Use
0.9% NaCl (308 mOsm/L)
[Na+ 154 mEq/L] [Cl- 154mEq/L]
● Expands ECF; beneficial in providing fluid
replacement when sodium and chloride loss has
occurred.
● Not used for maintenance
D5W (252 mOsm/L)
[5% dextrose in water]
● Used when replacing water in hypernatremic
patients.
● Provides 170 calories
● Can lead to water intoxication and dilutional
hyponatremia
Lactated Ringer’s Solution (274
mOsm/L)
[Na 130 mEq/L, Cl 109 mEq/L, K 4
mEq/L,
Ca 3 mEq/L, lactate 28 mEq/L]
● Used for replacement of fluid because of multiple
electrolytes and isotonic expansion of blood
volume.
● Used commonly for GI losses
● Not given for more than 48 hours due to the
riosk of calcium depletion.
Dextran 70 [6% solution of
polysaccharide combined with saline
or dextrose or water]
● Expands blood volume
● Decreases blood viscosity
Hetastarch (310 mOsm/L) ● Used for rapid volume expansion
● May prolong bleeding time
Hypotonic Solutions
Solution Common use
0.45% NaCl (1/2 strength) (154
mOsm/L)
[1/2 normal saline, ½ water]
0.33% NaCl (1/3 strength) (103
mOsm/L)
[1/3 normal saline, 2/3 water]
● These are fluids that hydrate the cell and do not
provide calories.
● Useful in treating hypernatremia when it is
desired to replace water and sodium.
Hypertonic Solutions
Solutions Common Use
5% dextrose in 0.45% NaCl (406
mOsm/L)
● Promotes hydration and good for maintenance
50% dextrose in water (2525
mOsm/L)
● Used to treat hypoglycemia and nutritional
replacement
● Can cause osmotic dieresis
3% or 5% NaCl (grossly hypertonic) ● Used to treat SIADH
Medical Surgical Nursing|

● Can cause increased intracranial pressure
Albumin (25%) [1500 mOsm/L]
given in 50 or 100 ml units
● Expands plasma volume and increases oncotic
pressure
● Use with caution in cardiac or renal patients
HYPERVOLEMIA
This refers to an isotonic expansion of the ECF caused by the abnormal retention of
water and sodium in approximately the same proportions in which they normally exist in the
ECF. It is always secondary to an increase in the total body sodium content, which, in turn,
leads to an increase in total body water. Since there is isotonic retention of body substances,
the serum sodium concentration remains essentially normal.
Clinical manifestations
These stem from expansion of the ECF and include:
Edema
Distended neck veins
Crackles over the lung field
Tachycardia, increased blood pressure
Shortness of breath and wheezing
Increased weight
Assessment and Diagnostic Findings
Decreased BUN and hematocrit levels because of plasma dilution
If with renal problems:
o decreased serum osmolality and sodium level
o increased sodium level
Chest x-rays may reveal pulmonary congestion
Medical Management
Management will always be directed at the causes i.e. removing the offending
substance or drug as in excessive administration of sodium-containing fluids.
Symptomatic treatment consists of administering diuretics and restricting fluid and
sodium.
● Pharmacologic treatment
Diuretics- the choice of drug will be based on the following:
Severity of the hypervolemic state
Degree of impairment of renal function
Medical Surgical Nursing|
Simple fluid overload
Diminished homeostatic functions
Excessive administration of table salts
Excessive administration of sodium-containing fluids

Potency of the diuretic
● Thiazide diuretics – block sodium reabsorption in the distal tube, where 5% to
10% of filtered sodium is reabsorbed. Eg. hydrochlorothiazide or metolazone.
● Loop diuretics – block sodium in the ascending limb of the loop of Henle, where
20%-30% of sodium is reabsorbed. Eg. furosemide, bumetanide, or torsemide
Usage of diuretics can also cause hypokalemia since potassium will also be
removed. Diuretics that act on the last distal tubule of the nephrons (eg.
Spirinolactone) will prevent hypokalemia. However, these kinds of diuretics can
cause hyperkalemia especially in patients with decreased renal function.
Hyponatremia occurs with diuresis due to increased release of ADH secondary to
reduction in circulating volume.
Hypomagnesemia occurs due to decreased reabsorption and increased excretion of
magnesium by the kidney.
● Hemodialysis
This modality will reinforce removal of excess sodium and fluid from the body.
● Nutritional Therapy
Dietary restriction of sodium
● A normal diet without sodium restriction commonly contains 6 to 15 g of
salt whereas a sodium-restricted diet can range from mild restriction to as
little as 250 mg of sodium.
● Half of ingested sodium is in the form of seasoning therefore, seasoning
substitute can
play a major role in decreasing sodium intake.
Water restriction
● Depending on water source, it may contain as little as 1 mg or more than
1500 mg per quart. Distilled water may be needed to use or if bottled water
will be used, the label must be carefully read because some of them have 0 to
1200 mg/L.
Protein intake may be increased in patients who:
● Are malnourished
● Have low serum protein levels in an effort to increase capillary oncotic
pressure and pull fluid out of the tissues into vessels for excretion by the
kidneys.
Nursing Management
Accurate measurement of intake and output
This should be done on a daily basis, taken at the same time and with the
same clothes the patient wears. A weight gain of 2.2 lb (1kg) is equivalent to a
gain of 1 L of fluid
Assessment of breath sounds
This should be done at regular intervals in an at risk patients, particularly if
parenteral fluid is being administered.
Assessment of edema
Medical Surgical Nursing|

The nurse should assess to monitor for the degree of edema in the most
dependent parts of the body such as the feet and ankles in ambulatory patients
and the sacral region in patients confined to bed.
The degree of pitting edema is assessed and the extent of peripheral edema
is monitored by measuring the circumference of the extremity with a tape marked in
millimeters.
Preventing Fluid Volume Excess
● Adherence to sodium-restricted diet
● Avoiding over-the-counter drugs for they may contain sodium
Detecting and Controlling Fluid Volume Excess
● Regular rest periods may be beneficial because bed rest favors diuresis
of edema fluid. This should promote blood circulation and increase renal
perfusion since this will diminish venous pooling.
● Rate of parenteral fluid and patient’s response must be closely
monitored. If dyspnea or orthopnea is present, the patient is placed then to
semi-fowler’s position to promote lung expansion. The patient cold also be
turned at different positions at regular intervals.
Teaching Patients About Edema
Edema is a common manifestation of FVE and patients need to recognize its
symptoms and understand its importance.
Medical Surgical Nursing|
INCREASED CAPILLARY PERMEABILITY (burns, allergic inflammation reaction)
Loss of plasma proteins
DECREASED CAPILLARY ONCOTIC PRESSURE INCREASED TISSUE ONCOTIC PRESSURE
EDEMA
Decreased transport of capillary filtered protein
LYMPH OBSTRUCTION
Decreased absorption of interstitial fluid
Decreased absorption of interstitial fluid
Fluid movement to tissues
Increased Na + H20 renal retention

Edema can be localized (in the ankle as in rheumatoid arthritis) or generalized (as
in cardiac and renal failure). A severe generalized edema is called anasarca. Pitting
Edema is so named because a pit forms after a finger is pressed in to the edematous area.
In pulmonary edema, the amount of fluid in the pulmonary interstitium and the alveoli
increases. The patient with pulmonary edema commonly complains of shortness of breath,
diaphoresis, increased respiratory rate, diaphoresis, and crackles and wheezing upon lung
auscultation.
Ascites is a form of edema in which fluid accumulates in the peritoneal cavity; it
results from nephritic syndrome, cirrhosis, and some malignant tumors. The patient
commonly reports shortness of breath, and a sense of pressure because of the
pressure on the diaphragm.
The goal of treatment is to preserve or restore the circulating intravascular fluid volume.
Signs and symptoms of hypervolemia and hypovolemia
Parameters Hypovolemia HypervolemiaSkin and
subcutaneous tissues
Dry, less elastic Warm, moist, pitting edema over bony prominences,
wrinkled skin from pressure of clothing
Face Sunken eyes (late symptom) Periorbital edema
Tongue Dry, coated (early symptom)Fissured (late symptom)
Moist
Saliva Thick, scanty Excessive, frothy
Thirst Present May not be significant
Temperature May be elevated May not be significant
Pulse Rapid, weak, thread Rapid
Respirations Rapid, shallow Rapid dyspnea, moist rales, cough
Blood pressure Low, orthostatic hypotension, small pulse pressure
Normal to high
Weight Loss Gain
Factors affecting water balance
Water Excess Water DeficiencyIntake Thirst Decreased thirst threshold
Increased osmolalityPotassium depletionHypercalcemiaFeverDry mucous membranes, poor oral hygiene, unmisted O2 administrationHypotension
Increased thirst thresholdDecreased osmolalityLack of accessPsychiatric disorders
Medical Surgical Nursing|

Parenteral fluids Psychiatric disordersExcessive D5W
Deficient replacementOsmotic loadsHyperalimentationHyperglycemiaMannitolRadiographic contrast agents
Output Sweating High ambient temperatureHigh altitudeFever
Renal excretion Inappropriate ADH releaseAppropriate ADH releaseCongestive heart failureDecompensated cirrhosisVolume depletionAdrenal insufficiencyRenal salt wastingHemorrhageDiuretics, NSAIDs BurnsHypothyroidismRenal diseases
Excess excretionPotassium depletionHypercalcemiaLithium administrationDemeclocycline Methoxyflorane
source: 8th ed. Critical Care Nursing Morton et. al. pp. 656
Electrolyte Imbalances
SODIUM IMBALANCESSodium is regulated by ADH, thirst, and the renin-angiotensin-aldosterone system. It
is the primary regulator of ECF volume. A loss or gain of sodium is usually accompanied by a loss or gain of water.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPONATREMIASodium deficit
● Muscle twitching
● Lethargy, confusion, seizures, and coma
● Hypotension and tachycardia
● Nausea and vomiting
● Oliguria or anuria
● Serum sodium <135 mEq/L
● Decreased urine specific gravity
● Decreased serum osmolality
● Urine sodium
● Increased RBC count
Contributing Factors
Loss of sodium, as in use of diuretics, loss of GI fluids, renal disease, and adrenal insufficiency.
Gain of water as in excessive administration of D5W and water supplements. Disease states associated with SIADH such as head trauma and oat-cell lung tumor Medications associated with water retention (oxytocin and certain tranquilizers) Hyperglycemia and heart failure
Medical Management
Sodium replacement
Medical Surgical Nursing|

Careful administration of sodium by mouth, nasogastric tube, or parenteral
route. Serum sodium must not be increased by more than 12 mEq/L in 24
hours to avoid neurologic damage due to osmotic demyelination.
Water restriction
Hyponatremia is treated by restricting fluid to a total of 800 mL in 24 hours.
This is far safer than sodium administration and is usually effective but if
neurologic symptoms are present, administration of hypertonic solutions is
needed.
Nursing Management
The nurse monitors for the patient’s intake and output daily and measures the
patient’s weight on a daily basis as well.
The nurse should also watch out for central nervous system changes such as:
o Lethargy
o Confusion
o Muscle twitching
o Seizures
Watch out for GI symptoms such as
o Anorexia
o Nausea
o Vomiting
o Abdominal cramping
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPERNATREMIA
Sodium excess
● Agitation, restlessness, fever, and decreased level of consciousness
● Hypertension, tachycardia, pitting edema, and excessive weight gain
● Thirst, increased viscosity of saliva, rough tongue
● Dyspnea, respiratory arrest, and death
● Serum sodium >145mEq/L
● Urine sodium <40 mEq/24h
● High serum osmolality
Contributing factors
Water deprivation
Diabetes insipidus
Heat stroke
Hyperventilation
Watery diarrhea
Burns, diaphoresis
Excess corticosteriod, sodium bicarbonate, and sodium chloride administration
Salt water near drowning
Medical Management
Medical Surgical Nursing|

Gradual lowering of the serum sodium level by infusing hypotonic (0.3% NaCl)
electrolyte solution or an isotonic nonsaline (D5W) solution.
To decrease the risk for cerebral edema, hypotonic solution is used rather than
using D5W because a hypotonic solution allows a gradual reduction in the serum
sodium level.
Diuretics may also be prescribed to treat sodium excess.
As a general rule, the serum sodium level is reduced at a rate not faster than 0.5 to
1 mEq/L per hour to allow sufficient time for readjustment through diffusion across
fluid compartments.
Nursing Management
Alert the patient about using over-the-counter medications that have a high salt
content.
The nurse must also obtain medication history.
Note the patient’s thirst or elevated body temperature.
Monitor for behavioral changes such as restlessness, disorientation, and lethargy.
Monitor for the patient’s response if he is on parenteral fluids to manage the
condition.
POTASSIUM IMBALANCES
It is the major intracellular electrolyte and 98% of the body’s potassium is inside the
cell and the remaining 2% is in the ECF, this 2% is important in neuromuscular function.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPOKALEMIAPotassium deficit
● Dizziness, hypotension, dysrhythmias, ECG changes, and cardiac arrest
● Nausea, vomiting, anorexia, diarrhea, decreased peristalsis, and abdominal distension
● Muscle weakness, fatigue, and leg cramps
● Serum potassium <3.5mEq/L
● Coexisting low serum calcium and magnesium levels not responsive to treatment for hypokalemia usually suggest hypomagnesemia
● Metabolic alkalosis
● ECG changes, including flattened T waves, elevated U waves, depressed ST segment
Contributing factors
Diarrhea
Medical Surgical Nursing|

Vomiting
Gastric suction
Corticosteriod administration, diuretic administration
Bulimia, starvation
Alkalosis
Digoxin toxicity
Medical Management
Oral or intravenous replacement therapy.
Administration of 40 to 80 mEq/L of potassium is adequate in an adult without
abnormal losses.
Foods high in potassium such as fruits and vegetable, legumes, whole grains, milk,
and meat should be recommended.
IV route for replacement is mandatory if the deficit is severe (2 mEq/L)
Nursing Management
Watch out for fatigue, anorexia, muscle weakness, decreased bowel motility,
paresthesias, and dysrhythmias.
Closely monitor patients who are taking digitalis for they are prone for digitalis
toxicity.
NEVER ADMINISTER POTASSIUM BY IV PUSH.
Potassium should be administered only after adequate urine flow has been
established.
Look closely for ECG changes (flat T wave or a prominent U wave)
Renal function should be monitored through BUN and creatinine levels and urine
output.
Great care should be taken when administering potassium most especially in older
adults, who have lower lean mass and total body potassium levels and therefore
lower potassium levels.
Remember that loss of renal function declines with advancing years so potassium
may be retained more readily in older adult than in younger people.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPERKALEMIAPotassium excess
● Tachycardia changing to bradycardia, ECG changes, and cardiac arrest
● Nausea, vomiting, and abdominal cramps
● Muscle weakness and flaccid paralysis
● Serum potassium >5mEq/L
● Metabolic acidosis
● ECG changes, including tented and elevated T waves, widened QRS complex, prolonged PR interval, flattened or absent P waves, depressed ST segment
Medical Surgical Nursing|

Contributing Factors
Oliguric renal failure Use of potassium sparing diuretics Metabolic acidosis Crush injury Burns Rapid IV administration of potassium
Medical Management
An immediate ECG should be obtained. Shortened repolarization and peaked T
waves are seen initially.
Do a repeat serum potassium level from a vein without an IV infusing potassium.
In non-acute situations, potassium restricted diet is advised and removal of
potassium-containing medications.
Prevention of hyperkalemia can be achieved by administration either orally or
through retention enema of cation exchange resins (i.e. Kayexalate) however this
medication is contraindicated for patients with paralytic ileus because
intestinal perforation can occur.
If K levels are dangerously elevated, it may be necessary to administer IV calcium
gluconate. This drug will not reduce the serum potassium but will antagonize
adverse cardiac conduction abnormalities. Be aware that calcium gluconate is not
interchangeable with calcium chloride because calcium gluconate has 4.5 mEq
of calcium and calcium chloride has 13.6 mEq/L of calcium.
IV administration of sodium bicarbonate may be necessary to alkalinize the
plasma and cause a temporary shift of potassium into the cells.
The use of beta-2 antagonists such as albuterol shows an evidence of highly
effective decreasing of potassium but remains controversial because they can cause
tachycardia and chest discomforts.
If hyperkalemic condition is transient, actual removal of potassium is necessary. This
could be done by using cation exchange resins, peritoneal dialysis, hemodialysis, or
other forms of renal replacement therapy.
IV administration of insulin and a hypertonic dextrose solution causes a
temporary shift of potassium into the cells. Diuretics can also be used to excrete
potassium.
Nursing management
Early identification of hyperkalemia in patients at risk should be done i.e. those with
renal failure.
The nurse then observes for signs of muscle weakness and dysrhythmias. Also,
observe for signs of paresthesias and GI disturbances such as nausea and
intestinal colic are noted.
To avoid erroneous reports of high serum potassium levels, observe the following
when withdrawing the blood:
Medical Surgical Nursing|

Avoid prolonged use of a tourniquet
Warn the patient not to exercise the extremity before the blood is
drawn.
Do not take the blood sample at the extremity where potassium is
administered.
Deliver the blood sample as soon as possible to prevent hemolysis.
Reinforce potassium-restricted diet. The following foods should be avoided:
Fruits and vegetables
Legumes
Whole-grain breads
Meat
Milk and eggs
Coffee, tea, and cocoa
Conversely, the following foods can be prescribed for they have minimal potassium
content:
Butter and margarine
Cranberry juice or sauce
Ginger ale
Gumdrops or jellybeans
Hard candy
Root beer
Sugar and honey
Great care should be taken when administering potassium, paying close attention to
the solution’s concentration and rate of administration.
Remember that potassium is always incorporated to the IV solution and then
mixed with the fluid by inverting the bottle several times.
Remember not to add the potassium in a hanging bottle because potassium might
be administered as a bolus.
CALCIUM IMBALANCES
More than 99% of the body’s calcium is located in the skeletal system; calcium is a
major component of bones and teeth. About 1% of skeletal calcium is rapidly exchangeable
with blood calcium, and the rest is more stable and only slowly exchanged. Calcium plays a
Medical Surgical Nursing|

major role in transmitting nerve impulses and helps regulate muscle contraction and
relaxation, including cardiac muscle.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPOCALCEMIACalcium deficit
● Anxiety, irritability, twitching around the mouth, laryngospasm, seizure, positive Chvostek’s sign and Trousseau’s sign
● Hypotension and dysrhythmias due to decreased calcium influx
● Tetany
● Serum calcium <8.5mg/dL
● Low platelet count
● ECG changes: lengthened QT interval, prolonged ST segment, arrhythmias
● Possible changes in serum protein levels
Contributing Factors
Hypoparathyroidism that may follow thyroid surgery or radical neck dissection.
Malabsorption, Vitamin D deficiency, alkalosis
Pancreatitis
Massive subcutaneous infection
Generalized peritonitis
Massive transfusion of citrated blood
Chronic diarrhea
Decreased parathyroid hormone
Diuretic phase of renal failure
Burns
Medical Management
Acute symptomatic hypocalcemia is life-threatening and requires prompt treatment
with IV administration of calcium. Parenteral administration of calcium salts
include the following:
o Calcium gluconate, calcium chloride, calcium gluceptate
Although calcium chloride has significantly more ionized calcium level,
I is not commonly used because it is more irritating and can cause
sloughing of tissue if it infiltrates.
Administer calcium diluted in D5W solution and given as slow IV bolus of slow IV
infusion. It should not be given with 0.9% sodium chloride because it increases renal
calcium loss.
Vitamin D therapy may be instituted to increase calcium absorption.
Aluminum hydroxide, calcium acetate, or calcium carbonate antacids may be
prescribed to decrease elevated phosphorous levels before treating hypocalcemia in
patients with chronic renal failure.
Medical Surgical Nursing|

Nursing Management
Calcium can cause postural hypotension therefore; the patient must be kept in
bed.
Observe the patient for signs of digitalis toxicity because calcium ions exert a
similar effect to that of the digitalis.
Also, the nurse must closely observe the rate of administration because too rapid IV
administration can cause cardiac arrest.
The nurse must also clarify with the physician about which calcium salt should be
administered since calcium gluconate yields 4.5 mEq/L of calcium while
calcium chloride yields 13.6 mEq/L.
Seizure precautions must be initiated and status of the airway is given paid
more attention. Safety precaution is also observed because patient may experience
confusion.
Recommend taking foods that are high in calcium to at least 1000-1500 md/day:
o Milk products
o Green, leafy vegetables
o Canned salmons or sardines
o Fresh oysters
The nurse must also advise the patient in taking in calcium supplements if calcium
cannot be well supplied by the patient’s diet. These supplements must be taken in
divided doses with meals.
Warn the patient about alcohol and caffeine intake because these can decrease
calcium absorption, and smoking increases urinary calcium excretion.
The patient is also cautioned about the overuse of laxatives and antacids that
contain phosphorus because their use decreases calcium absorption.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPERCALCEMIACalcium excess
● Drowsiness, lethargy, headaches, irritability, confusion, depression, or apathy
● Weakness and muscle flaccidity
● Bone pain and pathological fractures
● Heart block
● Anorexia, nausea, vomiting, constipation, and dehydration● Flank pain
● Serum calcium >10.5mg/dL
● ECG changes: sign of heart block and shortened QT interval
● Azotemia
● Decreased parathyroid hormone level
Contributing Factors
Hyperparathyroidism, malignant neoplastic disease
Prolonged immobilization
Overuse of calcium supplements or Vitamin D excess
Medical Surgical Nursing|

Oliguric phase of renal failure
Thiazide diuretic use
Increased parathyroid hormone, digoxin toxicity
Medical Management
Therapeutic aims in hypercalcemia include decreasing the calcium serum level
Reversing the process causing hypercalcemia
Treating the underlying cause includes:
o Chemotherapy for a malignancy
o Parathyroidectomy for hyperparathyroidism
IV administration of 0.9% sodium chloride solution to temporarily dilute the serum
calcium level and increases urinary calcium excretion by inhibiting tubular
reabsorption of calcium.
Administration of IV phosphate can cause a reciprocal drop in serum calcium
Furosemide is often used in conjunction with administration of saline solution to
cause diuresis increasing calcium excretion.
Calcitonin is often used to lower calcium levels for patients with heart disease or
renal failure who cannot tolerate large amounts of sodium. It reduces bone
resorption, increasing depositing of calcium and phosphorous in the bones and
increases urinary excretion of calcium and phosphorous.
Nursing Management
Remember to do skin allergy testing before administration of calcitonin and must be
administered intramuscularly rather than subcutaneously because patients with
hypercalcemia have poor perfusion in the SQ.
Encourage mobilization and increasing fluid intake. Fluids with sodium are
encouraged unless contraindicated because sodium favors calcium excretion. The
patient is advised to take 3 to 4 quarts of fluids.
Adequate fiber should be provided in the diet to offset a tendency of constipation.
The patient and the family are informed that there may be some mental changes
and can be reversed with the treatment.
Medical Surgical Nursing|

MAGNESIUM IMBALANCESMagnesium is the second most abundant electrolyte in the intracellular compartment
after potassium. It acts as an activator for many intracellular enzyme systems and plays a
role in both carbohydrate and protein metabolism. Magnesium produces its sedative effect
at the neuromuscular junction, probably by inhibiting the release of the neurotransmitter
acetylcholine.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPOMAGNESEMIAMagnesium deficit
● Nearly always co-exists with hypokalemia and hypocalcemia
● Hyperirritability, tetany, leg and foot cramps, positive Chvostek’s sign and Trousseau’s sign, confusion, delusions, and seizures
● Dysrhythmias, vasodilation, and hypotension
● Serum magnesium <1.5mEq/L
● Coexisting low serum potassium and calcium levels
Contributing factors
Hyperparathyroidism, hyperaldosteronism
Chronic alcoholism
Diuretic phase of renal failure
Malabsorption
Diabetic ketoacidosis
Refeeding after starvation, parenteral nutrition
Chronic use of laxative, diarrhea
Acute myocardial infarction, heart failure
Decreased serum potassium and calcium
Pharmacologic agents (gentamicin, cisplatin, cyclosporine)
Medical Management
Mild magnesium deficiency can be corrected by diet alone. The following foods are
principal dietary sources of magnesium:
o Green leafy vegetables
o Nuts, seeds, legumes, whole grains, and seafood
o Peanut butter and cocoa
Magnesium salts can be administered orally in an oxide or gluconate form to replace
continuous excessive losses. Magnesium sulfate is the most commonly used
magnesium salt.
Nursing Management
Medical Surgical Nursing|

Patients receiving IV magnesium should be monitored not to exceed 150 mg/min or
67 mEq/L over 8 hours.
Vital signs must be monitored accurately to identify changes in cardiac rhythm,
hypotension, and respiratory distress.
Monitoring of the patient’s urine output before and after magnesium administration;
physician is notified if the urine output is less than 100 mL over 4 hours
Calcium gluconate must be readily available to treat possible hypocalcemic tetany or
hypomagnesmia
Seizure precaution is instituted
The ability to swallow should be assessed with water before administering oral
medications or food to the patient.
The nurse also assesses neuromuscular irritability by grading deep tendon reflexes.
For patients experiencing hypomagnesemia from abuse of alcohol, the nurse
provides teaching, counseling, support, and possible referral to alcohol abstinence
programs.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPERMAGNESEMIAMagnesium excess
● Uncommon, caused by decreased renal excretion (renal failure) or increased intake of magnesium
● Diminished reflexes, muscle weakness to flaccid paralysis
● Respiratory distress
● Heart block, bradycardia
● Hypotension
● Serum magnesium >2.5mEg/L
● Coexisting elevated potassium and calcium levels
Contributing Factors
Oliguric phase of renal failure
Adrenal insufficiency
Excessive IV magnesium administration
Diabetic ketoacidosis
Hypothyroidism
Medical Management
This can be prevented by avoiding the administration of magnesium to patients with
renal failure.
In emergency situations such as respiratory distress or defective cardiac
conduction, ventilator support and IV calcium gluconate are indicated. IV calcium
gluconate will antagonize the effect of magnesium in the cardiovascular and
neuromuscular systems.
Medical Surgical Nursing|

Hemodialysis with magnesium-free dialysate can reduce the serum magnesium to a
safe level within hours.
Administration of loop diuretics and sodium chloride or Lactated Ringer’s solution
enhances magnesium excretion in patients with adequate renal function.
Nursing Management
The nurse monitors for hypotension and shallow respirations as well as decreased
patellar reflexes and diminished level of consciousness.
Caution is essential when taking over-the-counter drugs that may contain
magnesium.
PHOSPHOROUS IMBALANCESIt is essential to the function of muscle and red blood cells, the formation of
adenosine triphosphate (ATP) and of 2,3-diphosphoglycerate which facilitates release of
oxygen from hemoglobin, and the maintenance of acid-base balance, as well as to the
nervous system and the intermediary metabolism of carbohydrate, protein, and fat.
Electrolyte Imbalance Clinical manifestations Diagnostic test results
HYPOPHOSPHATEMIAPhosphorous deficit
● Muscle weakness, tremor, and paresthesia
● Peripheral hypoxia
● Serum phosphate <2.5mg/dL
● Urine phosphate >1.3g/24h
Contributing Factors
Refeeding after starvation
Alcohol withdrawal
Diabetic ketoacidosis, respiratory alkalosis
Decreased magnesium and potassium, vitamin D deficiency
Vomiting, diarrhea
Hyperparathyroidism
Burns, acid-base disorders
Diuretic and antacid use
Medical Management
Adequate amounts of phosphate should be added to parenteral solutions, and
attention should be paid to the phosphorous levels in enteral feeding solutions.
Aggressive IV phosphorous correction is usually limited to patients whose serum
phosphorous levels decrease to less than 1 mg/dL and whose GI tract is not
functioning.
The rate of phosphorous administration should not exceed 10 mEq/h.
Medical Surgical Nursing|

Nursing Management
IV site where phosphorous is being administered should be monitored for sloughing
off and necrosis that can possibly occur alongside infiltration.
Be aware of the dangers of IV phosphorous that include tetany from hypocalcemia
and calcifications in tissues (blood vessels, heart, lung, kidneys, eyes) from
hyperphosphatemia.
Give attention to preventing infection because hypophosphatemia may alter
granulocytes.
For mild hypophosphatemia, dietary replacement should be enough:
o Milk and milk products
o Organ meats
o Nuts and whole grains
o Fish and poultry
With moderate hypophosphatemia, supplements such as:
o Neutra-Phos capsules (240 mg phosphorous/capsule)
o Fleet’s phosphorous soda (815 mg phosphorous/5 mL)
Electrolyte Imbalance Clinical manifestations Diagnostic test results
HYPERPHOSPHATEMIAPhosphorous excess
● Usually asymptomatic unless leading to hypocalcemia then evidenced by tetany and seizures
● Serum phosphate >4.5mg/dL
● Serum calcium <9mg/dL
● Urine phosphorous <0.9g/24h
Contributing Factors
Acute and chronic renal failure
Excessive intake of phosphorous
Vitamin D excess
Respiratory Acidosis
Hypoparathyroidism
Volume depletion
Leukemia/lymphoma treated with cytotoxic agents
Increased tissue breakdown
Rhabdomyolysis
Medical Management
Treatment is directed at the underlying disease.
Vitamin D preparations such as calcitrol which is available in both oral (Rocatrol) and
parenteral (Calcijex)
IV administration of calcitrol does not increase serum calcium unless its dose is
excessive, thus permitting more aggressive treatment of hyperphosphatemia with
calcium-binding antacids, phosphate-binding gels or antacids.
Medical Surgical Nursing|

Forced diuresis with a loop diuretic, volume depletion with saline, and dialysis.
Surgery may be indicated for removal of large calcium-phosphorous deposits.
Nursing Management
Advise the patient to avoid phosphorous-rich foods such as:
o hard cheese
o nuts, whole grain cereals
o dried fruits and dried vegetables
o meat and kidneys
o sardines
o sweetbreads and foods made with milk
When appropriate, advise the patient to avoid phosphate containing substances such
as
o Laxatives
o Enemas
The nurse also monitors for signs of impending hypocalcemia and to monitor
changes in urine output.
CHLORIDE IMBALANCESIt is contained in gastric and pancreatic juices, sweat, bile, and saliva. Sodium and
chloride in water make up the composition of the ECF and assist in determining osmotic
pressure. The serum level of chloride reflects a change in dilution and concentration of the
ECF and does so in direct proportion to the sodium concentration.
Electrolyte Imbalance
Clinical manifestations Diagnostic test results
HYPOCHLOREMIAChlorine deficit
● Muscle hypertonicity and tetany
● Shallow, depressed breathing
● Usually associated with hyponatremia and its characteristic symptoms, such as muscle weakness, and twitching
● Serum chloride <98mEq/L
● Serum pH >7.45 (supportive value)
● Serum CO2 >32 mEq/L (supportive value)
Contributing Factors
Addison’s disease
Reduced chloride intake or malabsorption
Untreated diabetic ketoacidosis, metabolic alkalosis, overuse of bicarbonate
Excessive sweating, diarrhea
Vomiting, gastric suctioning
Sodium and potassium deficiency
Medical Surgical Nursing|

Loop, osmotic, thiazide diuretic
Rapid removal of ascitic fluid with high sodium content
Intravenous fluids that lack chloride (dextrose and water)
Draining fistulas and ileostomies
Heart failure, cystic fibrosis
Medical Management
Treatment involves correcting the cause of hypochloremia and the contributing
electrolyte and acid-base imbalances.
Normal saline (0.9%) and half strength (0.45%) solution is administered to replace
chloride.
Reevaluate whether the patient receiving diuretic should be discontinued or
changed.
Ammonium chloride may be prescribed to treat metabolic alkalosis depending on
patient’s weight and serum chloride level. Use in caution with patients with impaired
liver or renal fxn.
Nursing Management
Foods high in chloride should be given:
o Tomato juice
o Eggs, cheese, and milk
o Salty broth, canned vegetables, and processed meats
Water without electrolytes should be avoided because it excretes large amount of
chloride.
Monitor for the patient’s intake and output; ABGs as well as consciousness and
muscle strength.
Monitor patient’s vital signs and respiratory assessment is frequently carried out.
Electrolyte Imbalance Clinical manifestations Diagnostic test results
HYPERCHLOREMIAChlorine excess
● Deep, rapid breathing
● Weakness
● Diminished cognitive ability, possibly leading to coma
● Serum chloride >108mEq/L
● Serum pH <7.35,
● Serum CO2 < 22 mEq/L(supportive values)
Contributing Factors
Excessive sodium chloride infusions with water loss; hypernatremia
Head injury
Renal failure
Corticosteroid use
Dehydration; severe diarrhea (loss of bicarbonate)
Respiratory alkalosis
Administration of diuretics, overdose of salicylates
Medical Surgical Nursing|

Kayexalate, acetazolamide, phenylbutazone
Ammonium chloride use
Hyperparathyroidism, metabolic acidosis
Medical Management
Directed at correcting the underlying cause and restoring electrolyte, fluid, and acid-
base balance are essential.
Hypotonic IV solutions may be given to restore balance.
o Lactated Ringer’s solution may be prescribed to convert lactate to
bicarbonate in the liver ultimately increasing bicarbonate and corrects the
acidosis.
IV sodium bicarbonate may be administered to increase bicarbonate levels. This will
lead to the renal excretion of chloride ions as bicarbonate and chloride compete for
combination with sodium.
Diuretics may be prescribed as well.
Sodium, chloride, and fluids are restricted.
Nursing Management
Monitoring of vital signs and arterial blood gas values.
Measuring patient’s intake and output.
Assessment findings related to respiratory, neurologic, and cardiac systems are
documented and observed for any changes that should be communicated with the
physician.
The nurse teaches the patient about the diet that should be followed to manage
hyperchloremia and maintain adequate hydration.
ACID-BASE IMBALANCESAlterations in acid-base balance can affect cellular metabolism and enzymatic
processes.
Acids and Bases
Acids are substances that give up a hydrogen ion. Hydrochloric acid, as a common
acid, can separate into hydrogen and chloride. Bases are substances that accept a
hydrogen ion. Bicarbonate (HCO3) as a common base then can accept a hydrogen ion to
form carbonic acid (H2CO3), a weak acid.
In acid-base balance and regulation, the weak acid carbonic acid and the base
bicarbonate plays are the most important. While carbonic acid plays a major role in acid-
Medical Surgical Nursing|

base balance, it is hardly measured because it dissolves in the plasma to form carbon
dioxide (CO2) and water (H2O).
Since carbon dioxide is in balance with carbonic acid and is easier to measure, it is
then expressed as a component in the acid-base balance. Carbon dioxide is referred to as
PCO2 when discussing acid-base balance because the ‘P’ represents partial pressure of
carbon dioxide. PaCO2 is used to refer to carbon dioxide in the arterial blood.
Carbon dioxide is a volatile acid because it is eliminated by the lungs and is
generated by the metabolism of food.
The base bicarbonate is added to the body in small amounts from dietary intake. The
gain of bicarbonate is offset by the normal loss of it through the stool. It plays a major role in
acid-base balance since it accepts hydrogen ion to neutralize acids.
The acid-base ratio is 1:20 where there is one part acid for every 20 parts base.
If this ratio is altered, derangement occurs in the acid-base environment.
pH
Acidity or alkalinity of body fluids is expressed in terms of the concentration of
hydrogen ions. The normal concentration of hydrogen ions has a very narrow range and is
small that makes it difficult to work with clinical setting so the concentration of hydrogen
ions is expressed as pH.
The pH has an inverse relationship to hydrogen ion concentration therefore;
The more hydrogen ions present, the lower the pH (acidic)
The fewer hydrogen ions present, the higher the pH (alkaline)
Medical Surgical Nursing|

Physiology
The normal acid-base environment is achieved by and maintained by three primary
mechanisms:
Chemical buffering (neutralizing) by intracellular and extracellular buffers.
Respiratory control of carbon dioxide via changes in rate and depth of respirations.
Renal regulation of bicarbonate concentration and secretion of hydrogen.
Mechanism of Regulating Acid-Base Balance
Action Time Effect
Chemical buffers in cells and extracellular fluidInstantaneous
Combine with the acids and bases added to
system to prevent marked changes in pH.
Respiratory SystemMinutes to hours
Controls carbon dioxide concentration in ECF
by changes in rate and depth of respiration.
KidneysHours to days
Increases or decreases quantity of sodium
bicarbonate in ECF.
Combines bicarbonate or hydrogen with
other substances and excretes them in urine.
Chemical Buffers
The presence of chemical buffers in body fluids and tissue allows the pH to remain in
narrow range so that the pH is not greatly altered. This does not change the absolute
number of hydrogen ions liberated by a strong acid or removed by a strong base but lessens
the effect of acid and base. The primary chemical buffers include:
Bicarbonate buffers
o This is the most important buffer in the plasma and interstitial fluid and is
responsible for 80% of buffering in extracellular fluid. It buffers by accepting a
hydrogen ion and forming the weak acid carbonic acid.
Bicarbonate can be depleted quickly when buffering large acid loads but in the short
term it is effective in maintaining a life-sustaining pH.
Intracellular buffers
o It plays an important role in maintaining acid-base balance since it accounts for
approximately 75% of all chemical buffering that takes place inside the cells.
Hemoglobin is the most plentiful and powerful protein buffer, since red blood cells
provide almost 70% of all buffering in the blood.
Medical Surgical Nursing|
Bicarbonate
Hydrogen ion
Carbonic acid

Phosphate buffers
o It is present in tubular fluid in the kidney aside from its role in intracellular
buffering. Phosphate buffers enable the kidney to increase excretion of hydrogen
ions in the urine. Without the phosphate buffers, the urine would quickly become
very acidic.
Bone buffers
o Bone carbonate contributes to maintaining the acid-base balance by buffering up
to 40% of an acute acid load. In the presence of a chronic acidic load as in chronic
renal failure, the bone buffers play an even greater role.
Respiratory Regulation
The role of the lungs in acid-base balance involves the regulation of carbon dioxide.
The rate and depth of alveolar ventilation determines how much carbon dioxide is
eliminated or retained. Normally, the amount of carbon dioxide eliminated equals the
amount produced by metabolic processes. When this balance is not maintained there will be
two conditions may occur:
Respiratory acidosis
o Retention of the volatile acid carbon dioxide or too little carbon dioxide eliminated
for amount produced.
Respiratory alkalosis
o Loss of the volatile acid carbon dioxide or too much carbon dioxide eliminated for
amount produced.
Respiratory compensation does occur with metabolic disturbances but since the
lungs are only able to eliminate volatile acids, compensation is limited when a fixed acid
load occurs. Maximal respiratory compensation can take up to 12 to 24 hours.
Renal Regulation
Renal regulation prevents progressive metabolic acidosis as bicarbonate buffers are
used up. Normally functioning kidneys does this by resorption and regeneration of
bicarbonate and excretion of hydrogen ions.
Regeneration of bicarbonate is done when hydrogen is secreted in the tubular fluid
and then combines with bicarbonate and forms carbonic acid which separates into carbon
dioxide and water. The water part is excreted and the carbon dioxide is resorbed converted
back to bicarbonate thus replacing the bicarbonate lost to buffering. In the presence of
alkalosis, less bicarbonate is generated because fewer hydrogen ions are secreted.
Conversely in acidosis, increased amount of bicarbonate is generated because of the
increased hydrogen ion secretion.
The kidneys help maintain a 1:20 ratio of acids to bases by excreting excess
hydrogen ions depending on pH. Renal compensation for respiratory acidosis or alkalosis
returns the pH to near normal. It is much more effective for respiratory disturbances than
respiratory compensation is for metabolic disorders. However, the initial renal compensation
response takes up to 24 hours with a maximal response taking 3 to 4 days.
Medical Surgical Nursing|

Arterial Blood Gases
Arterial blood provides valuable information about the acid-base status because
venous blood is not suitable for assessment of oxygen tension and pH. The nurse draws
arterial blood without exposure to air in a heparinized syringe using the appropriate artery
(radial, brachial, or femoral).
ABG analysis is the measurement of the following parameters:
pH
o The direct reflection of hydrogen ions and thus the acid/base ratio. This signals
the severity of the disorder. The perfect pH is 7.40 with the range of 7.35-7.45.
A normal pH may exist in the following conditions:
mixed acid-base disturbance
when the compensation has returned the pH to normal or near normal
PaCO2
o This reflects the alveolar function.
Hypercapnia (PaCO2 greater than 45 mmHg) signals alveolar
hypoventilation and respiratory acidosis or compensation for metabolic
alkalosis.
Hypocapnia (PaCO2 less than 35 mmHg) results from alveolar
hyperventilation causing respiratory alkalosis or compensation for
metabolic acidosis.
Bicarbonate
o As a major component of bases, bicarbonate is calculated from the pH and
PaCO2. Its normal values are 22 to 26 mEq/L.
Serum Electrolytes
Electrolytes are affected by the acid-base status. Acute changes in pH are
accompanied by changes in serum potassium concentration:
In acidemia, potassium shifts out of the cells and excess hydrogen moves into the
cell to be buffered.
In alkalemia, potassium goes into the cells and hydrogen moves out of the cells to
be buffered.
Electrolyte values are necessary to calculate anion gap which is the difference
between measured cations (sodium and potassium) and measured anions (chloride and
bicarbonate). Because potassium has a low value (3.5-5.0 mEq/L), it is not used in
calculating anion gap:
Anion gap= Na – (Cl + HCO3)
The normal anion gap is 12 +- 2. A gap greater than 14 usually indicates the
presence of unmeasured anions such as the organic acids lactate or ketoacids.
Albumin is a measurable anion and important buffer that can affect anion gap when
decreased.
Medical Surgical Nursing|

ACID-BASE DISTURBANCESDisturbances of acid-base balance can be metabolic or respiratory in origin and
can cause either an acidosis or alkalosis. These imbalances are also classified as acute
or chronic. It is important to note that more than one condition can occur at the same time.
The only two disorders that cannot occur simultaneously are respiratory acidosis and
respiratory alkalosis.
Respiratory Acidosis
Whether acute or chronic, it is the result of alveolar hypoventilation and results in
hypercapnia. This condition has partial pressure of carbon dioxide (PaCO2) greater than 45
mmHg. The degree to which the increased PaCO2 alters the pH depends on how rapidly the
increase occurs and the body’s ability to compensate with the blood buffer system and renal
regulation. Because of the limitations of blood buffer system and the delay in renal
regulation, a rapid decrease in pH is usually seen in acute increases in PaCO2.
Clinical manifestations:
● Dyspnea ● Tachypnea
● Restlessness ● Confusion
● Diaphoresis
In severe cases:
● Lethargy ● Ventricular dysrhythmias
● Cyanosis ● Coma
● Dilated conjunctival and facial blood vessels
Common causes:
o Depression of the respiratory center by drugs, cerebral injury or disease,
sudden cardiac arrest.
o Structural abnormalities as in flail chest
o Neuromuscular abnormalities as in hypokalemia
o Systemic Problems as in acute respiratory distress syndrome
o High carbohydrate diet
o Airway obstruction and lung disorders
o With acute lung disorders, hypoxemia occurs before hypercapnia
Medical Management:
o Patients may require suctioning to ensure open airway and chest
physiotherapy may be ordered.
o If PaCO2 is greater than 50 to 60 mmHg, the patient may require intubation
and mechanical ventilation.
o In patients with chronic respiratory acidosis, treatment with supplemental
oxygen must be approached cautiously. It is usually administered at 1 to 3
L/min, with careful ongoing monitoring.
o Antibiotics are prescribed if infection is causing or contributing to respiratory
acidosis.
Medical Surgical Nursing|

Nursing Management:
o Health history, assess for the following:
Length of time since onset of symptoms
Presence of dyspnea
Complaints of anxiety or restlessness
Changes in level of consciousness-confusion or lethargy
o Physical examination:
Increased heart rate and respiratory rate
Signs of diaphoresis
Asterixis
Dilated conjunctival and facial blood vessels
Ventricular dysrhythmias
Cyanosis (late sign)
o Patient’s airway is maintained by encouraging coughing.
o For patients under mech-vent, the nurse monitors for the settings and checks
for the patency of the tubes.
o Monitoring of the bowel sounds and abdominal distention is necessary to
prevent a decrease in diaphragmatic movement secondary to abdominal
pressure, which may further compromise respiratory status.
o The semi-fowler’s position allows for expansion of the chest wall and is
appropriate for most patients.
o For mechanically ventilated patients with unilateral lung disease, a side lying
position would be best so that it increases perfusion to the dependent (down
side) healthy lung and increases ventilation to the diseased upper lung.
o Prone position often benefits patients with ARDS because it improves
ventilation/perfusion mismatch.
Respiratory Alkalosis
This is the result of hyperventilation leading to hypocapnia (PaCO2 less than 40
mmHg). The acute decrease in PCO2 causes a mild but rapid decrease in serum bicarbonate,
occurring within 10 minutes and reaching a constant state in approximately 10 minutes.
Respiratory alkalosis that persists beyond 6 hours is classified as chronic and renal
compensatory changes can cause further decrease in bicarbonate concentration and an
increase in pH toward normal levels.
Clinical Manifestations:
● Anxiety ● Lightheadedness
● Paresthesias ● Circumoral numbness
Common causes:
o Most commonly associated with hyperventilation related to anxiety.
o Occurs with pain, gram negative sepsis, high altitude sickness, and some
pulmonary disorders with or without coexisting hypoxemia.
Medical Surgical Nursing|

o Salicylate overdose and intracerebral trauma that exert direct stimulation on
the respiratory center leading to hyperventilation.
Medical Management:
o Treatment aims at correcting underlying disorder
o The physician may order tranquilizers to treat anxiety-induced respiratory
alkalosis. If symptoms are severe, rebreathing into a paper bag or an oxygen
mask with a carbon dioxide reservoir may be useful.
o Pulse oximetry may be used to assess oxygenation before and during
treatment.
o Adequate pain management is important if the condition is caused by the
patient’s response to pain.
o If hypoxemia is the cause, oxygen therapy may be necessary
Nursing Management:
o Health history, assess for the following:
Length of time since the onset of symptoms
Complaints of pain or anxiety
Complaints of shortness of breath, dyspnea, lightheadedness
Presence of paresthesias or circumoral numbness
History of asthma, other pulmonary disorders, and central nervous
system trauma and related information.
o Physical examination, assess for the following:
Increased heart rate and depth of respiration
Confusion
Tetany, syncope, and seizures
Cardiac dysrhythmias and ST-T waves
o The nurse should assess for degree of anxiety and offer to stay with the
patient.
o Encourage the patient to have a normal breathing pattern by pacing the
client’s breathing or having the patient mimic the nurse’s breathing pattern.
o It may also help to have the patient rebreathe into a paper bag or oxygen
mask with an attached carbon dioxide reservoir.
o Monitor and check the patient’s pulse oximetry.
Metabolic Acidosis
This condition occurs when there is a primary decrease in serum bicarbonate
concentration (to less than 22 mEq/L)
Clinical Manifestations:
● Hypotension ● Tachypnea
● Fruity breath ● Cold, clammy skin
● Nausea, vomiting ● Diarrhea
● Confusion
In severe cases:
● Kussmaul’s respirations ● Flushed, warm, dry skin
Medical Surgical Nursing|

● Dysrhythmias ● Stupor
● Coma
Common causes:
o Loss of Bicarbonate:
Gastrointestinal: Diarrhea, biliary and pancreatic drainage
Renal: Renal tubular acidosis type 2
Acetazolamide
o Excess Acid Production:
Ketoacidosis, diabetes, alcohol-induced starvation
Lactic acidosis, rhabdomyolysis
o Excess Acid Ingestion:
Salicylates, methamphetamine
Cocaine
3,4-methylenedioxymethamphetamine (Ecstasy)
Medical Management:
o Directed at underlying disease
o In DKA, fluid and insulin are required
o In alcohol-related ketosis, glucose and saline are necessary
o Acute and renal failure would need hemodialysis or peritoneal dialysis to
restore acid-base balance
o Administration of sodium bicarbonate may be given in severe cases but
should be use in caution to patients with congestive heart failure or
pulmonary edema
Nursing Management:
o Health history, assess for the following:
Length of time since the onset of symptoms
History of headache, anorexia, nausea, vomiting, and diarrhea
Polyuria, Polydipsia
o Physical examination, assess for the following:
Hypotension
Tachypnea or Kussmaul’s respirations
Cold, clammy skin progressing to flushed, warm, and dry skin
Fruity breath
Changes in level of consciousness
Ventricular dysrhyhtmias
Metabolic Alkalosis
This condition occurs when there is excess serum bicarbonate from either a gain of
bicarbonate or loss of hydrogen, resulting in increase in pH.
Clinical Manifestations:
● Muscle weakness ● Hyporeflexia
● Polyuria or polydipsia ● Cardiac rhythm disturbance
In severe cases:
Medical Surgical Nursing|

● Neuromuscular irritability ● Apathy
● Confusion ● Stupor
Common causes:
o Gastrointestinal
Vomiting
Nasogastric suctioning
o Renal
Diuretics (especially thiazides)
Mineralcorticoid excess
Post chronic hypercapnia
Hypercalcemia, hypoparathyroidism
o Hydrogen ion shift into cells
Hypokalemia
Carbohydrate refeeding after starvation
o Bicarbonate retention
Administration or ingestion of bicarbonate
Massive blood transfusion
o Contraction alkalosis
Diuretics
Cystic fibrosis
Medical Management:
o Mild to moderate metabolic alkalosis does not usually require specific
therapeutic intervention and treatment is directed at correcting the
underlying disorder.
o Testing urine electrolyte before beginning treatment is necessary to
differentiate the cause of alkalosis.
o Hypokalemia often occurs and is responsible for symptoms of muscle
weakness and cardiac rhythm disturbances.
o Serum potassium may be given either orally or IV K salts to treat hypokalemia
o Isotonic saline infusion may be prescribed to correct volume deficits related
to metabolic alkalosis caused by diuretics or loss of gastric secretions.
o Acetazolamide (Diamox) may be used in patients with congestive heart
failure who cannot tolerate rapid volume expansion. This drug can cause
large losses of potassium and bicarbonate; therefore, potassium
supplementation may be necessary before starting the treatment.
Nursing Management:
o Health history, assess for the following:
Length of time since the onset of symptoms
History of vomiting, nasogastric suctioning, bulimia, diuretic use, or
abuse
Presence of muscle weakness
History of polydipsia and polyuria
o Physical examination, assess for the following:
Medical Surgical Nursing|

Postural hypotension
Neuromuscular excitability associated with tetany
Changes in level of consciousness
o The nurse must monitor the electrocardiogram for the presence of
dysrhythmias.
o The nurse assesses for apical and radial pulses simultaneously to detect pulse
deficit.
Catheters
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or
vessel. Catheters thereby allow:
Drainage
Administration of fluids or gases
Access by surgical instruments.
The process of inserting a catheter is catheterization.
In urinary catheterization, or "cathing" for short, a plastic tube known as a urinary catheter
that is gently slid into a patient's bladder via his or her urethra. Catheterization allows the
patient's urine to drain freely from the bladder for collection, or to inject liquids used for
treatment or diagnosis of bladder conditions. The procedure of catheterization will usually be
done by a clinician, often a nurse, although self-catheterization is possible as well.
Indications for urinary catheterizations:
Intermittent catheterization
Collection of sterile urine sample.
Provide relief of discomfort from bladder distention.
Decompression of the bladder.
Measure residual urine.
Management of patients with spinal cord injury, neuromuscular degeneration, or
incompetent bladders.
Short-term indwelling catheterization
Post surgery and in critically ill patients to monitor urinary output.
Surgical procedures involving pelvic or abdominal surgery repair of the bladder,
urethra, and surrounding structures.
Urinary obstruction (e.g. enlarged prostate), acute urinary retention
Prevention of urethral obstruction from blood clots with continuous or intermittent
bladder irrigations
Instillation of medication into the bladder.
Long-term indwelling catheterization
Refractory bladder outlet obstruction and neurogenic bladder with urinary retention.
Prolonged and chronic urinary retention.
To promote healing of perineal ulcers where urine may cause further skin breakdown.
Contraindications
Medical Surgical Nursing|

Foley catheters are contraindicated in the presence of urethral trauma. Urethral
injuries may occur in patients with multisystem injuries and pelvic factures, as well as
straddle impacts. If this is suspected, one must perform a genital and rectal exam
first. If one finds blood at the meatus of the urethra, a scrotal hematoma, a pelvic
fracture, or a high riding prostate then a high suspicion of urethral tear is present.
One must then perform retrograde urethrography (injecting 20 cc of contrast into the
urethra).
Risks associated with catheterization include:
Urethral trauma and bleeding from inappropriate catheter size or use of
force.
Urinary tract infections related to poor sterile technique or long-term
catheterization.
Bladder spasms and pain
Choosing the appropriate catheter depends on
The size of the patient’s urethral canal
The expected duration of catheterization (e.g. intermittent or indwelling)
Knowledge of any allergies to latex or plastic.
The indications for catheterizing the patient (i.e. clot retention, child, bladder
instillation).
Catheters come in several basic designs
A Foley catheter (indwelling urinary catheter)is retained by means of a balloon at
the tip which is inflated with sterile water. The balloons typically come in two
different sizes: 5 cc and 30 cc. They are commonly made in silicone rubber or natural
rubber.
A Robinson catheter is a flexible catheter used for short term drainage of urine.
Unlike the Foley catheter, it has no balloon on its tip and therefore cannot stay in
place unaided.
A Coudé catheter is designed with a curved tip that makes it easier to pass through
the curvature of the prostatic urethra.
A hematuria (or haematuria) catheter is a type of Foley catheter used for Post-TURP
hemostasis. This is useful following endoscopic surgical procedures or in the case of
gross hematuria. There are both 2-way and 3-way hematuria catheters (double and
triple lumen).[1]
An external Texas or condom catheter is used for incontinent males and carries a
lower risk of infection than an indwelling catheter
Catheter diameters are sized by the French catheter scale (F). The most common
sizes are 10 F (3.3mm) to 28 F (9.3mm). The clinician selects a size large enough to allow
free flow of urine, and large enough to control leakage of urine around the catheter. A larger
size can become necessary when the urine is thick, bloody or contains large amounts of
Medical Surgical Nursing|

sediment. Larger catheters, however, are more likely to cause damage to the urethra. Some
people develop allergies or sensitivities to latex after long-term latex catheter use making it
necessary to use silicone or Teflon types. Silver alloy coated urinary catheters may reduce
infections. Types:
Straight-single use catheters
Have a single lumen with a small 1¼ cm opening.2-way Foley catheters (retention catheters)
Have an inflatable balloon that encircles the tip near the lumen or opening of the catheter.
Curved or Coude
Catheters have a rounded curved tip (elbowed) used in older male patients
with enlarged prostates which partially obstruct the urethra.
3-way Foley catheter
Medical Surgical Nursing|

Often called retention catheter, they have 2 or 3 lumens that encircle the
body of the catheter. One lumen drains the urine through the catheter into a
collection bag. The second lumen holds the sterile water when the catheter
is inflated and is also used to deflate the balloon. The third lumen maybe
used to instill medications into the bladder or provide a route for continuous
bladder irrigation.
Pediatric catheterization:
Size- 5, 6, 8, 10Fr. or smaller depending on the size of the urethra and age
of child.
Rarely are catheters left indwelling, typically they are intermittent and are
used to obtain sterile urine sample to rule-out infection.
In children <2years of age a 5Fr. feeding tube can be used if a small
diameter catheter is not available.
Using feeding tubes can cause urethra trauma, a second pair of hands for
assistance is recommended for very young children.
Male catheterization:
16Fr. or 18Fr. catheter is typically used for most men, as they are more rigid
and often easier to insert past the prostate.
In males it is helpful to use a Urojet (syringe with lidocaine jelly) to minimize
the discomfort with the catheterizations.
Males who present with gross hematuria require 3-way Foley catheters with
the largest diameter that can be safely inserted. (22Fr., 24Fr.,)
Catheters should be attached to the inner upper thigh with a CathSecure.
This will minimize discomfort and prevent the catheter from being pulled
on/out.
When the foreskin is retracted for the purpose of catheterization remember
to return it back to its original place.
If resistance is met while inserting the catheter due care is used not to
damage the enlarged prostate. Never inflate the balloon until urine has been
visualized and is draining.
Female Catheterization:
12fr., 14Fr.or 16Fr. catheter is typically used.
Positioning is important to properly visualize the urethra in females.
If you are unable to visualize the urethra, raise pelvis with a pillow, blanket or
inverted bedpan.
If you insert catheter into the vagina leave it in place as a landmark and start
again with another sterile catheter.
Never inflated the balloon until you see urine.
If patient presents with gross hematuria a larger 3-way catheter needs to
inserted.
Medical Surgical Nursing|

Combating infection
Everyday care of catheter and drainage bag is important to reduce the risk of infection.[7] Such precautions include:
Cleansing the urethral area (area where catheter exits body) and the catheter itself.
Disconnecting drainage bag from catheter only with clean hands
Disconnecting drainage bag as seldom as possible.
Keeping drainage bag connector as clean as possible and cleansing the drainage bag
periodically.
Use of a thin catheter where possible to reduce risk of harming the urethra during
insertion.
Drinking sufficient liquid to produce at least two liters of urine daily
Sexual activity is very high risk for urinary infections, especially for catheterized
women.
Recent developments in the field of the temporary prostatic stent have been viewed as a possible alternative to indwelling catheterization and the infections associated with their use
Prior to starting, explain to the patient what is going to happen and why they
need to be catheterized. Assess patients understanding and answer any questions
they may have. Collect supplies, it is helpful to bring a second catheter in case of
contamination of the first catheter. Clear off work space/ bedside table and begin to
position the patient. Raise the bed to an appropriate working height and position
yourself on the opposite side of you dominant hand. Keep in mind that it may be
necessary to obtain additional help with the catheterization.
Credits for urinary catheter: This web-based module was developed by Adam Szulewski based on content written by Lucy Rebelo for the Queen's University Faculty of Health Sciences Patient Simulation Lab.The module was created using exe : eLearning XHTML editor with support from Amy Allcock and the Queen's University School of Medicine MedTech Unit.
Nephrostomy tube
A small rubber tube that is placed through a hole in the skin and that extends
into the kidney. The tube allows direct drainage from the kidney. Often called a
percutaneous nephrostomy tube, the device attaches to a collection bag that
collects and measures urine output. The tube allows urine to bypass blocked or
damaged ureters in order to avoid the risk of infection or irreversible damage that
the backflow of urine causes for a patient with a blockage or leak.
Nephrostomy tube has several other functions, including the following:
To remove or dissolve renal calculi
To obtain direct access to the upper urinary tract for various endourologic procedures
To diagnose ureteral obstruction, filling defects, and anomalies via antegrade
radiography
To deliver chemotherapeutic agents to the renal collecting system
Medical Surgical Nursing|

To provide prophylaxis after resection for local chemotherapy in patients with tumors
of the renal pelvis.
Indications
Temporary urinary diversion associated with urinary obstruction secondary to calculi
Diversion of urine from the renal collecting system in an attempt to heal fistulas or
leaks resulting from traumatic or iatrogenic injury, malignant or inflammatory
fistulas, or hemorrhagic cystitis
Treatment of nondilated obstructive uropathy
Treatment of urinary tract obstruction related to pregnancy
Treatment of complications related to renal transplants
Access for interventions such as direct infusion of substances for dissolving stones;
chemotherapy; and antibiotic or antifungal therapy
Access for other procedures (eg, benign stricture dilatation, antegrade ureteral stent
placement, stone retrieval, pyeloureteroscopy, endopyelotomy)
Decompression of nephric or perinephric fluid collections (eg, abscesses, urinomas)
Contraindications
Bleeding diathesis (most commonly, uncontrollable coagulopathy)
Uncooperative patient
Severe hyperkalemia (>7 mEq/L) should be corrected with hemodialysis before the
procedure.
Preprocedural evaluation
Laboratory studies, including determination of prothrombin time (PT), activated partial
thromboplastin time (aPTT), platelet count, BUN and creatinine levels, hematocrit (Hct) and
hemoglobin (Hgb) levels, WBC count, and urinalysis and urine culture, are made.
Pertinent images (eg, sonograms, CT scans, intravenous urograms [IVUs], radionuclide
scintigrams) are reviewed to assess the location of the colon, liver, and spleen in
determining the approach.
Intravenous access is established and the patient is adequately hydrated.
Prophylactic antibiotics are administered 60 minutes before the procedure, especially if
pyonephrosis is suspected or if the obstruction is caused by a renal calculus. The use of
antibiotics is somewhat controversial; however, in patients with a known urinary tract
obstruction, antibiotics should be administered before the procedure (preferably 1 h before
puncture) and should be continued for at least 24 hours after the procedure. Antibiotics
should be chosen on the basis of urine culture results, if available. If the results are not
available, use of a broad-spectrum antibiotic is recommended.
The patient should receive nothing by mouth (NPO) for 4-8 hours before the procedure,
for conscious sedation precautions.
Some have advocated the placement of percutaneous nephrostomy tubes without
performing preprocedural coagulation studies, although the authors disagree with this
approach unless the situation is an absolute emergency. Because the kidney is highly
Medical Surgical Nursing|

vascular, needle puncture and tract dilation in a patient with a coagulopathy could result in
massive hemorrhage.
Postprocedural management and follow-up
Postprocedural management and follow-up may include the following:
o Bedrest for 4 hours
o Return to the preprocedural diet
o Checking of vital signs every 30 minutes for 4 hours and then every shift
o Antibiotic therapy, if infection is identified or suspected
o Catheter flushing with 5 mL of bacteriostatic isotonic sodium chloride solution
and then aspiration every 6-12 hours
o Monitoring of urine output
Major complications with percutaneous nephrostomy tube placement include the following:
o Bleeding
o Sepsis
o Injury to an adjacent organ
Other major complications, though somewhat rare, have been reported to occur in as many
as 5% of patients. Complications of percutaneous nephrostomy may include the following:
o Massive hemorrhage requiring transfusion, surgery, or embolization (1-3%)
o Pneumothorax (<1%)
o Microscopic hematuria (common)
o Pain (common)
o Urine extravasation (<2%)
o Inability to remove the nephrostomy tube because of crystallization around
the tube site
o Death (0.2%)
o Sepsis (1.3%)
o Catheter dislodgement during the first month (<1%)
Suprapubic catheter
When placement of a urethral catheter is contraindicated or unsuccessful, percutaneous suprapubic urinary bladder catheterization is a commonly performed procedure to relieve urinary retention.1
This topic describes the Catheter over needle technique. The Seldinger technique is described in the Clinical Procedures topic Suprapubic Aspiration.
IndicationsSuprapubic catheterization is indicated (when transurethral catheterization is contraindicated or technically not possible) to relieve urinary retention due to the following conditions:
Urethral injuries
Urethral obstruction
Bladder neck masses
Benign prosthetic hypertrophy (BPH)
Medical Surgical Nursing|

Prostate cancer
Contraindications
Suprapubic catheterization is absolutely contraindicated in the absence of an easily
palpable or ultrasonographically localized distended urinary bladder.
Suprapubic catheterization is relatively contraindicated in the following situations:
o Coagulopathy (until the abnormality is corrected)
o Prior lower abdominal or pelvic surgery (potential bowel adherence to the
bladder or anterior abdominal wall; may recommend that a urologist perform
an open cystostomy)
o Pelvic cancer with or without pelvic radiation (increased risk of adhesions)
SP Catheter Care
It is very important to take good care of the suprapubic tube and drainage system.
They should be kept very clean. The bag should not be allowed to drag on the floor.
If the bag should accidentally be cut or begin to leak, it must be changed. An opening
anywhere along the entire system of tubing and bag will allow bacteria to enter. If these
would then reach your child's bladder, a urinary tract infection could result. It is not
acceptable to place the drainage bag in a plastic bag if it leaks.
Cleaning the Catheter
Follow the steps below to clean the area where the catheter enters the patient's body.
1. Wash your hands with soap and water.
2. Once a day, use a warm wet soapy wash cloth to clean the catheter and the skin
around it. Take care that you do not pull excessively on the catheter.
3. If there is any crustiness on the catheter that does not come off with soap and water,
you may use hydrogen peroxide on the catheter. Pour some hydrogen peroxide on a
cotton ball or gauze pad and wipe gently on the catheter.
4. Rinse the skin and catheter with plain water. Pat dry with a towel.
5. You may place a slit gauze dressing over the catheter site if you wish. It is not
required, but some people feel more comfortable doing so.
Bathing
While the patient has the SP catheter, he/she will need to take a sponge bath. Baths,
showers and swimming are not allowed.
Emptying the Bag
The large drainage bag must be emptied at least every 8 hours even if it is not full. If the
bag is small and fills quickly, it should be emptied when the bag is 2/3 full.
When emptying the bag, be careful not to touch the top of the spout to the container into
which it is being drained. Also, do not touch the top of the spout with your hands.
Medical Surgical Nursing|

Changing the Bag
1. Wash your hands with soap and water.
2. Disconnect the tubing from the catheter. Insert the new drainage bag tubing into the
catheter.
3. If you are going to reuse the bag you just switched from, the connection site must be
covered with a sterile cap or gauze. The bag must be kept in a clean place.
Tips
Keep the drainage system below the level of the bladder so the urine does not back
up.
The leg bag will allow you to wear regular clothes and be free to play or work.
Remember that because it is small, it will need to be emptied often.
Be sure there are no kinks or bends in the tubing. Urine will not drain if this happens.
If the patient's drainage bag becomes dirty or foul-smelling, it needs to be changed.
If a hole is punctured in the bag or tubing, it also needs to be changed.
Make sure the patient drinks plenty of fluids. The urine should be light yellow and
clear.
Medical Surgical Nursing|