First seizure emergency investigation
-
Upload
scgh-ed-cme -
Category
Health & Medicine
-
view
729 -
download
4
Transcript of First seizure emergency investigation

FIRST –EVER SEIZUREDr Nicholas LawnDr Jacqui Saw

4 pillars of first seizure management in ED
• Diagnosis• Investigations• Neuroimaging
• CT vs MRI vs None• Advice to patient
• Treatment • Acute• Long-term• Can we make a diagnosis of epilepsy?
• Driving/ Safety issues

Diagnosis – was it a seizure?• History from Patient
• no test is a substitute for an inadequate history• Collateral history – critical
• sometimes ED is the best place as the witness may be available when they are not there later in the clinic
• “Historical drift” issue – the initial history may differ form that taken at the clinic for many reasons including
• Initial phase of seizure – ictal cry, head/eye deviation• Convulsive phase - tonic• Post-ictal phase – stertorous breathing highly specific for a GTCS (Sisodyia et al JNNP)• Confusion/agitation,
• Video of event from bystanders• Examination - limited value but look for post-ictal behaviour, post-ictal hemiparesis/aphasia
(may be the only opportunity to identify this if short-lived, is highly specific for focal onset seizure)
• Fever, focal neurology
• No single sign, symptom or test is 100% specific for seizure except recording an event during EEG

Other points to consider• Post ictal confusion
• Unusual with syncope except elderly• Myoclonic or jerk-like movements?
• Up to 90% of syncopal events can result in this (video)• Tongue biting
• Thought to be more specific – lateral• Incontinence
• Non-specific
• Collateral history is the key• Was the first the first?


Diagnosis – was it a provoked event?
• What is provoked?• Acute CNS process vs acute systemic process
• Importance – risk of recurrence• Can cluster if cause not addressed eg hyponatraemia

Diagnosis – what was was the cause?
• Blood tests• FBC, U+Es, LFTS• Glucose• Lactate ?prolactin ?ammonia (mod increase following
majority GTCS)• ECG (long QT, short PR etc)
• CSF if febrile, headache, persistent confusion, +/-focal neurology with normal CT
• Imaging

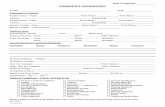
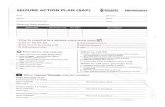
Seizure Protocol (FSH) – this says it all actually

Imaging CT vs MRI vs nothing
• Why?• Identify cause – missed lesion with CT 1-2%• Pick up - our series 20-30% but many expected (eg known prior
stroke). • Type of seizure – lesion provides evidence the seizure was focal in
onset

The minimum needed in ED…• History, History, History• Examination
• Focal neurology• Meningism• Intercurrent illness
• Bloods• Lactate, not prolactin anymore• Electrolytes
• CT head• 1% of lesions will still be missed

Ho et al, Neurol Clin Practice 2014, 3.398-403The cumulative likelihood of seizure recurrence (figure 1) at 1 year was 59% (95% CI54%–65%) for those with an epileptogenic lesion on any imaging, and 44% (95% CI 41%–48%) for those without a lesion (log-rank p , 0.001).

56% (51-62) 63% (58-68)

EEG• Who to get it on in the ED?• Ongoing twitching ?continued seizure• Persistent confusion following GTCS ? NCSE• Atypical features (usual things
• out-of phase limb movents, pelvic thrusting, side to side head movemnets, convulsive events with normal breathing, no lactate rise
• But rarely practical/possible – ask your friendly neurology registrar for help during hours

Advice to patient• Admit vs home?
• Admit – lesion on CT, cluster (more than one seizure with recovery within 24 hrs)
• Acute CNS process• Acute systemic process that is not clearly self-limited
• Treat – rarely needed – occasionally short-term benzos eg CZP 0.5mg daily for 2-3 days for cluster
• Driving• Private vehicle - 6 months for first-ever seizure, provoked or
unprovoked. • Commercial - 5 years for first-ever unprovoked seizure, one year if
provoked


Prognosis – risk of epilepsy
• What do we tell our patients?• Whilst generally agreed that seizure recurrence is most likely within
the first 6 months, estimates of the overall risk of recurrence vary widely, from 29 to 71% at 2 to 3 years3-9
• Working number 40-50% at 2-3 yrs, 60-70% if epileptogenic lesion/remote symptomatic
• Why is the range so wide?• Flawed follow up, most trials based on 1st seizure clinic data
• Too long – waitlist 6 months in Perth• Time to ascertainment bias
Patients who have a second seizure may go somewhere
else
Patients who don’t have a second event may just not turn
up


• Flawed definition


Aim of the first-ever seizure project
• Aims: To assess risk of recurrence after a first-ever seizure in adults.
• • Hypothesis: The risk of seizure recurrence at 2 years is
50% (i.e., the mid-point of prior studies’ upper and lower risk estimates.)

Method• Study type: Prospective cohort study of adults with first-
ever seizure. • • Participants: Adults (aged 18 years or over) with first-
ever seizure. Patients with prior seizures or non-epileptic events that mimic seizures (eg convulsive syncope) will be excluded.

Patient presents with ?first seizure episode
Clinical Assessment by ED physician
Not a first seizure episode Patient is not given handout, no EDIS code allocated, not referred to clinic
Likely first seizure episode
Referred to First seizure Clinic
Given first seizure handout
Discharged home EDIS CODE ALLOCATED
24 hrs
later
PI accesses EDIS coding
PI phones patient, confirms consent verballyQuestionnaire completed
PCIF mailed outPatient enrolled
Yes, eligible for enrolment
No, not eligible for enrolment
Follow-up as planned in 1st seizure clinic
No further contact with PI/AI
Patient Enters study

Questions?

Good Reference