features in fourteen dogs
Transcript of features in fourteen dogs

Myelofibrosis: Review of clinical and pathologicalfeatures in fourteen dogs
Brent Hoff, John H. Lumsden, Victor E.O. Valli, Stephen A. Kruth
AbstractA cinicopathological study was performed on 14 dogswith myelofibrosis (MF), in order to correlate clinical,laboratory, and histomorphological parameters andinvestigate factors of prognostic significance. Theclinical signs included fatigue, weight loss, anorexia,and diarrhea. Physical findings included pale mucousmembranes and wasting/emaciation. The major lab-oratory observations were moderate to severe, poorly-responsive anemia with various degrees of marrowcellularity and fibrosis. All dogs with severe, non-responsive anemia should have a bone marrow corebiopsy, stained for connective tissue, in order to detectmyelofibrosis. Myelofibrosis regressed in six dogs.
R6sum6My6lofibrose: caract6rlstiques cliniques etpathologiques chez 14 chiensUne etude clinico-pathologique a ete effectuee sur14 chiens presentant de la myelofibrose afin de deter-miner une correlation entre les signes ciniques, les don-nees de laboratoire et les ele'ments histomorpholo-giques ainsi que pour identifier les facteurs influenVantle pronostic. Les signes cliniques comprenaient de lafatigue, une perte de poids, de l'anorexie et de ladiarrhee. L'examen physique a demontre une paleurdes muqueuses et un amaigrissement/emaciation. Lesdonnees de laboratoire ont indique une anemie, legere-ment regeneratrice, de moderee a severe avec des quan-tites variables de cellules myeloides et de fibrose. Tousles chiens presentant une anemie severe non regenera-trice devraient subir une biopsie de la moelle osseuseavec coloration des tissus conjonctifs afin de detecterla myelofibrose. La myelofibrose a regresse danssix cas.
(Traduit par Dr ThUr6se Lanthier)
Can Vet J 1991; 32: 357-361
IntroductionlA yelofibrosis (MF) is characterized by fibroblasticlproliferation and various degrees of collagen
deposition in the marrow cavity. It was first describedby Hueck in 1879, and has been recognized to occurin association with many diseases (1). Much confusionhas occurred in the human literature, with some 25 dif-ferent names having been proposed for disorders witha prominent myelofibrotic component, includingVeterinary Laboratory Services Branch, Ontario Ministry ofAgriculture and Food, P.O. Box 3612, Guelph, OntarioNIH 6R8 (Hoff); Department of Pathology (Lumsden) andDepartment of Clinical Studies (Kruth), Ontario VeterinaryCollege, University of Guelph, Guelph, Ontario NIG 2W1;Dean's Office, University of Illinois, College of VeterinaryMedicine, Urbana, Illinois, USA 61801 (Valli).
Can Vet J Volume 32, June 1991
agnogenic myeloid metaplasia, leukoerythroblasticanemia, and myelosclerosis (1,2).
Myelofibrosis has been documented infrequently indogs, and these reports only include a small numberof cases (3-7). In dogs, myelofibrosis has beenreported in association with necrosis of bone marrow(3), hemopoietic neoplasia (5), and severe, congenitalhemolytic anemia (6,7).The purpose of our study was to correlate clinical,
laboratory, and histomorphological parameters andinvestigate prognostic indicators in 14 dogs withmyelofibrosis.
EtiologyThe cause of MF is unknown. Some of the theoriesused to explain its development are exposure to toxins,ionizing radiation, chemotherapy, viruses, or as areaction to neoplastic invasion of bone marrow (1).The detection of karyotypic abnormalities has resultedin the suggestion of a genetic basis for some humans (8).Exposure to toxins has been implicated in people
exposed to solvents, benzene, and paint thinners (9,10).Myelofibrosis has been reported in human patientsreceiving therapy for Hodgkin's disease, chronicmyeloid leukemia, and membranous nephritis (11). Itremains unknown whether "chemotherapy-induced"MF in man occurs secondarily to treatment or is anunusual consequence of the basic disease.
In man, MF is a frequent observation in patientswith a variety of neoplastic disorders, especiallymyeloproliferative disorders known as myeloid meta-plasia with myelofibrosis (MMMF), agnogenic myeloidmetaplasia, or idiopathic myelofibrosis (12,13).Myeloid metaplasia with myelofibrosis was consideredto be a neoplastic proliferation of fibroblasts derivedfrom a primitive mesenchymal cell that was thoughtto be the progenitor of hematopoietic cells (14). Ithas now been shown that the marrow fibroblasts aremesenchymal cells derived neither from hematopoieticstem cells nor as a clone of neoplastic cells (15).Fibroblast cultures from fibrotic marrow have all theproperties of, and are indistinguishable from, thoseof nonfibrotic marrows (16).The pathogenesis of MF has been extensively inves-
tigated in patients with myeloproliferative disease (17).The most widely accepted hypothesis is that growthfactors derived from megakaryocytes or platelets stim-ulate the increase in the number of fibroblasts and theproduction of collagen (17). Megakaryoblasts are oftenincreased in the bone marrow of patients with MF. Ithas been suggested that the syndrome of acute MF inpeople may be an acute megakaryocytic leukemia (9).A positive correlation has been found between the con-centration of platelets in blood and the degree of
357

in vitro fibroblast stimulation (18). Ineffectivemegakaryopoiesis may result in increased concentra-tions of platelet factor 4 and platelet-derived growthfactor (PDGF) (17). Fibroblast growth and prolifera-tion are stimulated by a PDGF (19).The connective tissue framework of normal bone
marrow is synthesized by fibroblasts and consists ofreticulin fibers that are continuous with the reticulinof blood vessel walls, sinusoids, and endosteum (1).It was believed that bone marrow fibrosis developedwith two distinct patterns: reticulin fibrosis, in whichthe normal pattern is exaggerated; and collagen fibrosis,in which the bone marrow architecture is obliterated.The latter was thought to be more serious (20). It hasnow been shown that both patterns consist of types I,
III, IV and V collagen with predominance of type IIIand its precursor, procollagen III (21). Fibronectinproduced by fibroblasts and endothelial cells is alsodeposited in fibrotic marrows (22). The normal inhib-itory action of prostaglandin El (PGE1) on fibronectinproduction seems to be decreased in MF; this may berelevant in the uncontrolled proliferation of someclones (23).Immune-mediated disorders have been demon-
strated in patients with MF (24). Several reports havedescribed elevated antinuclear antibodies, rheumatoidfactor, and positive direct Coombs' tests (25,26). Itis not known whether these abnormal immunologicalmarkers are of significance in the pathogenesis of MF,but there is some evidence that the presence of intra-cellular immune complexes is predictive of responseto immunosuppressive therapy in man (27).
Case selection and methodsTwenty-six dogs with histological evidence of MF wereinitially included in this study but 12 cases wereexcluded later because of missing data. The cases wereobserved from 1983 to 1989 at the Ontario VeterinaryCollege and the Veterinary Laboratory Services BranchLaboratory, Ontario Ministry of Agriculture andFood. Blood was collected for hematology and serumchemistry determinations. A bone marrow aspirate anda core biopsy were attempted from the wing of theilium of each animal retained in the study (n = 14).Age, sex, breed, clinical signs of disease, and addi-tional laboratory test results and treatment wereobtained from the medical records.
Routine methods were used for hematology andserum chemistry. Bone marrow aspirate granulesmears were air-dried and stained using Wright's stain.Bone marrow core biopsies were obtained using aJamshidi needle (Kormed Inc., St. Paul, Minnesota,USA). The core biopsies were fixed in 1007 neutralbuffered formalin. Bone marrow specimens wereembedded in paraffin by routine methods. Most of thesamples were demineralized for two to three hours butthis was unnecessary when only a few spicules of bonewere present (7). Sections were stained with hema-toxylin and eosin (H&E), Gomori's method for retic-ulin, Masson's trichrome stain, and the Prussian blue
reaction for hemosiderin.The degree of reticulin fibrosis was graded in histo-
logical sections stained with Gomori's method. Sec-tions without, or with rare, fine argyrophilic fibers in358
hematopoietic cords were graded as 0. A diffuse net-work of focal areas of fine, or coarse, fibers wasgraded as 1 or 2, respectively. A bone marrow withmarkedly increased reticulin with linear coarse fiberswas graded as 3. The degree of collagen fibrosis wassimilarly graded as 0 to 3 on the Masson's trichrome-stained sections. Hemosiderin concentration wasgraded as decreased, normal, or increased. Mega-karyocytes, per high power field, were counted in sec-tions stained with H&E and graded as normal, increased,or decreased.
TreatmentTreatment was attempted in 13 of the 14 dogs. Cortico-steroids were administered to 13, anabolic steroids tonine, kaolin/pectin to seven, whole blood transfusionsto six, antibiotics to five, B-vitamins to five, andfolate/B12 to one dog.
ResultsThe mean age of the 14 dogs with myelofibrosis at thetime of diagnosis was 6.5 years (range, 3-12 years),with gender distribution of eight males and six females.Fourteen different breeds were represented. Seven dogswere alive after one year. Six dogs lived more than2.5 years and were considered to have recovered com-pletely from the original clinical condition. Three dogswere euthanized during the first week of therapy because
Can Vet J Volume 32, June 1991
Table 1. Historical andphysical findings in 14 dogswith myelofibrosisHistory
Fatigue 11Weight loss 11Anorexia 9Diarrhea/vomiting 7Fever 3Seizure/syncope 3
Physical examinationPale mucous membranes 13Wasting/emaciation 6Splenomegaly 4Hepatomegaly 3Abdominal pain 1
Table 2. Hematological findings in 14 dogsat time of MF diagnosis
ReferenceMean Minimum Maximum range
RBC count(x 10'2/L) 2.60 1.20 5.68 5.6-8.5
Packed cellvolume (L/L) 0.18 0.08 0.38 0.38-0.57
Hemoglobin(g/L) 44 30 135 132-193
Platelet count(x109/L) 333 60 1000 145-440
Reticulocytes(x 109/L) 18 0 36 20-80
aHematology reference intervals used for adult dogs at Veter-inary Laboratory Services, Ministry of Agriculture and Food,and Ontario Veterinary College

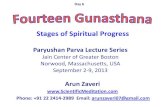
Figure la Figure lc
Figure lb Figure ld
Figure 1. Histopathology of the bone marrow in MF.a. Mildly hypercellular bone marrow without fibrosis. H&E.b. Early hyperplastic stage with mild fibrosis. H&E.
of lack of clinical response (n = 1) or transfusion reac-tion (n = 2).The clinical signs reported by owners of affected
dogs were nonspecific, and included fatigue, weightloss, anorexia, diarrhea, fever and seizures/syncope(Table 1).
Physical examination revealed pale mucous mem-branes, wasting/emaciation, splenomegaly, hepato-megaly, and abdominal pain (Table 1).
Hematological findings at the time of diagnosis aresummarized in Table 2. A moderate to marked, poorly-responsive anemia was present in 13 dogs. One doghad marginal anemia (packed cell volume 0.38 L/L)and a poor erythroid response. The leukocyte and
c. Moderate degree of reticulin (argyrophilic) fibers. Gomori'ssilver impregnation.d. Coarse bundles of collagen fibers encompassing a fewhematopoietic elements in terminal stages of MF. Masson's.
platelet counts were generally normal or slightlyincreased. One dog had severe leukopenia on initialexamination, and three dogs developed mild throm-bocytopenia as the disease progressed.
Biochemical profiles were within reference limits inseven dogs. Alanine aminotransferase (ALT) activitywas mildly increased in four and glutamic dehydroge-nase (GDH) activity was mildly increased in two dogs.One of the dogs with mildly increased ALT and GGTactivity also had a moderate increase in alkalinephosphatase activity (1040 U/L). One dog had mildazotemia (urea 14.7 mmol/L and creatinine 187 pmol/L);another dog had a moderate increase in cholesterolconcentration (22.2 mmol/L).
Ca Ve Voum 32 Jun 199 359
Table 3. Marrow cellularity, fibrosis, megakaryocytes, andhemosiderin
Reticulin Collagen HemosiderinCellularity grade grade' Megakaryocytes grade
(07.) (No. of dogs) (No. of dogs) (No. of dogs) (No. of dogs)Mean 49 1 (5) 1 (7) Normal (8) 1 (3)Min. 30 2 (8) 2 (3) Decreased (1) 2 (5)Max. 75 3 (1) 3 (4) Increased (5) 3 (6)
aGrading of reticulin and collagen is described in case selection and methods section of text
Can Vet J Volume 32, June 1991 359

Aspiration biopsies were successful in six dogs. Onlysinusoidal blood was obtained from three dogs, andfor five dogs there was a "dry tap". Core biopsies weresuccessful for each of the 14 dogs.The bone marrow core biopsy results are sum-
marized in Table 3. The cellularity of these biopsieswas estimated and ranged from 30-75% (mean 49%).The marrow granulocyte reserve (MGR) was slightlydecreased in 10 and normal in four of the dogs. A com-parison of a mildly hypercellular bone marrow withoutfibrosis to early hyperplastic stage with mild fibrosisis shown (Figures la and lb). The megakaryocyteswere moderately increased in five, and normal in ninedogs (Figure lb). Coarse hemosiderin was markedlyincreased in 11 and moderately increased in three ofour dogs. Erythrophagocytosis was evident in theaspiration or core biopsy of three dogs. Only one ofthese dogs was Coombs' positive. The bone marrowin nine dogs had moderate to severe reticulin fibrosis(score 2 or 3) and, in five dogs, mild reticulin fibrosis(score 1) at the time of diagnosis (Figure lc). In sevendogs the H&E and Masson's stains indicated a moderateto marked increase in collagen (score 2 or 3) (Figure Id),and in the other seven dogs a mild increase in collagen(score 1).
DiscussionIn each of the 14 dogs reported in this study, the nor-mal trilineage marrow was replaced by fibroblasts withvarious amounts of reticulin and collagen deposition.The reticulin and collagen patterns appeared to besimilar to that reported in human MF (1). As inhumans, there were no characteristic clinical criteriawhich defined the disease syndrome (28).
In our study, myelofibrosis was most common inmiddle-aged dogs, with all but one being over fouryears old (mean age 6.5 years). The most commonobservations reported by owners of affected dogs werefatigue, anorexia, weight loss, diarrhea, fever, andseizures/syncope. With the exception of the diarrheaand gastrointestinal problems, these symptoms werepredictable, nonspecific, and not helpful in estab-lishing a diagnosis of MF. The severe bouts of diar-rhea in over 50% of the dogs are unexplained and dif-ficult to relate to MF. It is possible that an infectiousagent, such as canine parvovirus, caused concurrentdisease of the intestinal mucosal epithelium and themarrow stromal cells, but in the latter organ incompleterepair or prolonged injury resulted in subsequentfibrosis. Fibrosis is a common sequel to a variety ofagents in tissues as diverse as lung, liver, and kidney.Parvoviral infection has been associated with chronicmarrow failure in an immunocompromised humanhost (29).The laboratory findings for the dogs in this study
were consistent with previous reports (3,4), the primaryobservation being normocytic, normochromic, non-regenerative anemia. For the dogs in our study, theleukocyte and platelet counts generally were within ref-erence limits or slightly increased, although mildthrombocytopenia developed in three dogs as thedisease progressed. One dog had a moderate to severeleukopenia as has been reported in man (1). Three360
stages in the development of myelofibrosis are reportedin man: 1) the cellular phase with "panmyelosis"(increase pertaining to all the elements); 2) MF withoutmarked osteosclerosis (hypercellularity may persist);and 3) osteosclerosis and hypocellularity with marrowfailure (1). If the disease progression is similar in dogs,alterations in the hemogram will depend upon the stageof myelofibrotic development. Extramedullary hema-topoiesis is commonly reported in the spleen and liverin MF in humans (30), including immature erythro-cytes, granulocytes, and megakaryocytes. Four of thedogs in this study (297o) had hepatomegaly and three(21(!7) had splenomegaly which is slightly higher thanreported in man (27).The exact stimulus for fibroplasia in MF is
unknown. There is evidence that growth factors pro-duced by megakaryocytes cause fibroblast prolifera-tion in vitro and that these factors may be releasedduring ineffective megakaryopoiesis (17,31,32). Fiveof our dogs had a moderate to marked increase inmegakaryocytes with early asynchrony (lack of matura-tion). Although each of these five dogs was moderatelyanemic, none was thrombocytopenic, and there wasa variable degree of bone marrow fibrosis. Studies inother species implicate leukemic lymphocytic andgranulocytic cells as possible causes of myelofibrosis.Leukemic monocytes from chickens with experimen-tally induced viral leukemia release a factor thatstimulates fibroblast colony formation (13). In studiesof human patients with acute myelogenous leukemiaand MF, serial sampling before and after chemo-therapy demonstrated that fibrosis decreased duringremission (33). Nine of our 14 dogs had increased num-bers of blast cells which appeared to be granulocyticprecursors. This increase in blast cells may correspondwith the cellular phase of MF development that hasbeen described in humans (1,34).An association between hemosiderin concentration
and myelofibrosis has been reported in dogs and catswith hemolytic anemia (7,35,36). In dogs with pyruvatekinase deficiency, treatment of the hemolytic anemiaby bone marrow transplantation corrects the iron over-load and prevents development of myelofibrosis (37).Hemosiderin was abundant in the marrow of each dogin our study. Hemosiderin accumulation, as estimatedmorphologically, does not appear to be correlated withthe degree of fibrosis as dogs with only a mild increasein hemosiderin had marked fibrosis. Marrow iron isdependent upon diet and age and is increased in manytypes of anemia (10). Increased iron absorption mayoccur during the myelodysplasia which often precedesclinical disease in these dogs (2).
Conventional treatment ofMF in dogs has been sup-portive, with red cell and platelet transfusions givenwhen required (3-5). Six of our dogs that appearedto recover clinically were treated with corticosteroids,anabolic steroids, and vitamins, but therapy did notappear to be different for the dogs that did not recover.The clinical situations were sufficiently confusing thatattempts to obtain reliable numerical data aboutresponses were futile.
Indicators of poor prognosis in human patients withmyelofibrosis are hemoglobin concentrations < 100 g/Land bone marrow hypocellularity (1). In previous
Can Vet J Volume 32, June 1991

studies, anemia has been a highly negative predictorin humans (28,37,38). Reports are conflicting on thevalue of marrow cellularity or severity of fibrosis(16,28,37). The degree of bone marrow fibrosis doesnot appear to be a good indicator of prognosis in thedogs in our study, though it has been reported inhumans (16). Bone marrow fibrosis does not appearto be correlated with liver and spleen weight in humans(39). In our study, all six dogs that recovered hadmoderate reticulin fibrosis and a moderate increase incollagen at the time of initial diagnosis. This compareswell with observations in human patients where thedegree of fibrosis does not correlate with duration ofsymptoms or outcome (39).
All dogs that recovered had normal or increasedcellularity (45%-75Vo) at the time of diagnosis. Althoughthe number of dogs was low, our data indicate thatincreased cellularity may be a positive prognosticindicator and that only very severe anemias withouterythroid responsive marrows and with low cellularitywarrant a poor prognosis.
There are many similarities in the development ofmyelofibrosis in dogs and humans. The frequency ofmyelofibrosis in dogs appears to be inadequatelyappreciated as is the potential for successful treatment.It is our view that investigation of suspect cases ofmyelofibrosis should include a bone marrow core aswell as aspiration biopsy. Sequential biopsies arenecessary for correlating histological lesions withclinical and hematological factors which may prove tobe useful predictors for survival. cvi
References1. Smith RE, Chelmowski MK, Szabo EJ. Myelofibrosis: A concise
review of clinical and pathologic features and treatment. Am JHematol 1988; 29: 174-180.
2. McCarthy DM. Fibrosis of the bone marrow: content andcauses. Br J Haematol 1985; 59: 1-7.
3. Weiss JW, Armstrong PJ. Secondary myelofibrosis in threedogs. J Am Vet Med Assoc 1985; 187: 423-425.
4. Dunn JK, Doige CE, Searcy GP, Tamke P. Myelofibrosis-osteosclerosis syndrome associated with erythroid hypoplasiain a dog. J Small Anim Pract 1986; 27: 799-806.
5. Thompson JC, Johnstone AC. Myelofibrosis in the dog: threecase reports. J Small Anim Pract 1983; 24: 589-601.
6. Prasse KW, Crouser D, Beutler E, Walker M, Schall WD.Pyruvate kinase deficiency anemia with terminal myelofibrosisand osteosclerosis in a beagle. J Am Vet Med Assoc 1975; 166:1170-1175.
7. Randolph JF, Center SA, Kallfelz FA, et al. Familial non-spherocytic hemolytic anemia in Poodles. Am J Vet Res 1986;47: 687-695.
8. Soule HD, Albert S, Wolfe PL, Bond B. Spontaneous and viral-induced myeloproliferative disorders in mice. U.S. AtomicEnergy Symposium Series 1970; 19: 171-176.
9. Throng LD, Saleem A, Schwartz MR. Acute myelofibrosis:A report of four cases and review of the literature. Medicine1984; 63: 182-188.
10. Hunstein W. Das myelofibrose-syndrom. In: Handbook ofInternal Medicine. Vol 2. New York: Springer, 1983: 191-250.
11. Carroll WL, Berbeich FR, Glader BE. Pancytopenia with myelo-fibrosis: An unusual presentation of childhood Hodgkin'sdisease. Clin Pediatr 1986; 25: 106-110.
12. Ellis JT, Peterson P. Myelofibrosis in the myeloproliferativedisorders. In: Berk PD, Castro-Malaspina H, Wasserman LR,eds. Myelofibrosis and the Biology of Connective Tissue.New York: Alan R. Liss Inc., 1984: 19-42.
13. Dodge WH. Avian monocytic leukemia cells release fibroblastgrowth factor: implications to associated myelofibrosis. LeukRes 1985; 9: 1559-1564.
14. Nalbandian RM, Wilner FM, Blackall CJ. Myeloid megakary-ocytic hepatosplenomegaly. Case study with a proposed systemof matrix classification of the myeloproliferative disorders. AmJ Clin Pathol 1968; 49: 535-555.
15. Gold DW, Hocking WG, Quan SG, Sparkes RS, Gale RP.Origin of human fibroblasts. Br J Haematol 1980; 44: 183-187.
16. Castro-Malaspina H, Jhanwar SC. Properties of myelofibrosis-derived fibroblasts. In: Berk PD, Castro-Malaspina H, WassermanLR, eds. Myelofibrosis and the Biology of Connective Tissue.New York: Alan R. Liss, Inc., 1984: 307-322.
17. Groopman JE. The pathogenesis of myelofibrosis in myelo-proliferative disorders. Ann Intern Med 1980; 92: 857-858.
18. Castro-Malaspina H, Moore MAS. Pathophysiological mech-anisms operating in the development of myelofibrosis: Role ofmegakaryocytes. Nouv Rev Fr Hematol 1982; 24: 221-228.
19. Burnstein SA, Malpass TW, Yee E, et al. Plantelet factor-4excretion in myeloproliferative disease: Implications for theaetiology of myelofibrosis. Br J Haematol 1984; 57: 383-388.
20. Editorial: Myelofibrosis. Lancet 1980; 1: 127.21. Gay S, Gay RS, Puchal JT. Immunological studies of bone mar-
row collagen. In: Berk PD, Castro-Malaspina H, WassermanLR, eds. Myelofibrosis and the Biology of the ConnectiveTissue. New York: Alan R. Liss, Inc., 1984: 292-322.
22. Jaffe EA, Mosher DF. Synthesis of fibronectin by culturedhuman endothelial cells. J Exp Med 1978; 147: 1779-1786.
23. Aglietta M, Piacibello W, Gavosto F. Myelofibrosis and prosta-glandins: Effect of prostiglandin El in colony-forming cells(CFU-GM). Br J Haematol 1981; 48: 167-170.
24. Rondeau E, Solal-Celigny P, Vrodans M, Brousse N, BernardJF, Boiven P. Immune disorders in agnogenic myeloid meta-plasia: Relation to myelofibrosis. Br J Haematol 1983; 53:467-474.
25. Caligari CF, Vigliani R, Novarino A, Camussi G, Gavosto F.Idiopathic myelofibrosis: A possible role for immune complexesin the pathogenesis of bone marrow fibrosis. Br J Haematol1981; 49: 17-25.
26. Bernhardt B, Valletta M. Lupus anticoagulant in myelofibrosis.Am J Med 1976; 272: 229-231.
27. Pitcock JA, Reinhard EH, Justus BW, Mendelshohn RS. Aclinical and pathological study of seventy cases of myelofibrosis.Ann Intern Med 1962; 57: 73-80.
28. Varki A, Lottenberg R, Griffith R, Reinhard E. The syndromeof idiopathic myelofibrosis; A clinicopathologic review withemphasis on the prognostic variables predicting survival. In:Medicine. Baltimore: The Williams & Wilkins Co., 1983:353-371.
29. Kurtzman GJ, Ozawa K, Cohen B, Hanson G, Oseas R, YoungNS. Chronic bone marrow failure due to persistent B19 parvo-virus infection. N Engl J Med 1987; 37: 287-294.
30. Soderstrom N, Bardman U, Lundh B. Patho-anatomicalfeatures of the spleen and liver. Clin Haematol 1975; 4: 309-314.
31. English RV, Breitschwerdt EB, Grindem CB, Thrall DE,Gainsburg LA. Zollinger-Ellison syndrome and myelofibrosisin a dog. J Am Vet Med Assoc 1988; 192: 1430-1434.
32. Fabich DR, Raich P. Acute myelofibrosis. Am J Clin Pathol1976; 67: 334-339.
33. Islam A, Catovsky D, Goldman JM, Galton DAG. Bone mar-row fibre content in acute myeloid leukemia before and aftertreatment. J Clin Pathol 1984; 37: 1259-1263.
34. Manoharan A, Pitney WR. Chemotherapy resolves symptomsand reverses marrow fibrosis in myelofibrosis. Scand J Haematol1984; 33: 453-459.
35. Blue JT. Myelofibrosis in cats with myelodysplastic syndromeand acute myelogenous leukemia. Vet Pathol 1988; 25: 154-160.
36. Weiden PL, Hackman RC, Deeg HC, Graham TC, ThomasED, Storb R. Long-term survival and reversal of iron overloadafter marrow transplantation in dogs with congenital hemolyticanemia. Blood 1981; 57: 66-69.
37. Barosi G, Berzuni C, Liberato LN, Costa A, Ascari P, Ascari E.A prognostic classification of myelofibrosis with myeloidmetaplasia. Br J Haematol 1988; 70: 397-401.
38. Thiele J, Steinberg T, Zankovich R, Fischer R. Primarymyelofibrosis-osteomyelosclerosis: Correlation of clinical find-ings with bone marrow histopathology and prognosis. Anti-cancer Res 1989; 9: 429-436.
39. Bentley SA, Herman CJ. Bone marrow fibre production inmyelofibrosis: A quantitative study. Br J Haematol 1979; 42:51-56.
Can Vet J Volume 32, June 1991 361