Familial Inheritance in Congenital Heart Disease: A Focus ... · 1 Tetralogy of Fallot 1.1 Overview...
Transcript of Familial Inheritance in Congenital Heart Disease: A Focus ... · 1 Tetralogy of Fallot 1.1 Overview...

Familial Inheritance in Congenital Heart Disease:
A Focus on Tetralogy of Fallot
by
Jodi-Ann Maria Swaby
A thesis submitted in conformity with the requirements for the degree of Masters of Science
Institute of Medical Sciences University of Toronto
© Copyright by Jodi-Ann Maria Swaby 2011

ii
Familial Inheritance in Congenital Heart Disease:
A Focus on Tetralogy of Fallot
Jodi-Ann Swaby
Master�’s of Science
Institute of Medical Sciences University of Toronto
2011
Abstract
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease (CHD). The
understanding of the genetics and inheritance of TOF is limited. Although about 15% of cases
are associated with a 22q11.2 deletion, the majority have no known genetic association. Even in
the setting of 22q11.2 Deletion Syndrome (22q11DS), factors that increase the likelihood of
CHD expression are poorly understood. We aimed to determine the prevalence and phenotypes
of CHD in relatives of adults with TOF. We also investigated the prevalence of CHD in relatives
of individuals with 22q11DS who do not themselves have a 22q11.2 deletion. Offspring of
patients with TOF had the greatest prevalence of CHD of all relatives. Diverse cardiac
phenotypes, including left heart obstructive lesions, were found in families. We also found that
unaffected relatives of individuals with 22q11DS had a greater prevalence of complex CHD over
population expectations, suggesting that modifier genetic factors may be involved in expression
of CHD in 22q11DS.

iii
Acknowledgments Thank you to my outstanding program advisory committee, Dr. Candice Silversides, Dr. Anne
Bassett and Dr. Peter Liu, for encouraging my research interest and for their invaluable input and
support.
Thanks to the entire team at the Clinical Genetics Research Program for technical assistance and
personal support. Special thanks to Stefanie Oechslin and Sean Bekeschus for their help with the
Progeny® software and data input.
To the physicians and staff at the Toronto Congenital Cardiac Centre for Adults, for supporting
this effort and allowing me access to their patients.
To Laura, Rhadika and Akasha, for their friendship, laughter and encouragement.
Most of all, thank you to my wonderful family without whom this truly would not have been
possible.

iv
Table of Contents Acknowledgments .......................................................................................................................... iii
Table of Contents ........................................................................................................................... iv
List of Tables ................................................................................................................................ vii
List of Figures .............................................................................................................................. viii
List of Abbreviations ..................................................................................................................... ix
Introduction ..................................................................................................................................... 1
1 Tetralogy of Fallot .................................................................................................................... 1
1.1 Overview ............................................................................................................................ 1
1.1.1 Historical Descriptions of TOF ................................................................................... 1
1.1.2 Anatomy and Variants of TOF .................................................................................... 2
1.1.3 Associated Lesions ...................................................................................................... 4
1.1.4 Pulmonary Atresia with Ventricular Septal Defect ..................................................... 6
1.2 Development of the Heart .................................................................................................. 6
1.2.1 Cardiogenesis and Transcription Factors .................................................................... 8
1.3 Classification of CHD ...................................................................................................... 11
1.4 Clinical Features and Management of TOF ..................................................................... 15
1.4.1 Extracardiac Features of TOF ................................................................................... 16
1.4.2 Surgical management of TOF ................................................................................... 16
1.4.3 Natural and Modified History of TOF ...................................................................... 17
1.4.4 Pregnancy and Reproductive Issues in TOF ............................................................. 18
1.5 Aetiology of TOF: Evidence for Genetic Origins ........................................................... 19
1.5.1 Familial Clustering and Twin Studies ....................................................................... 19
1.5.2 Genetic Principles of Disease .................................................................................... 20
1.6 Known Genetic Causes of TOF: Variable Expressivity and Phenotypic Heterogeneity . 26
1.6.1 Molecular techniques for detection of genetic factors in TOF .................................. 26
1.6.2 Copy Number Variants .............................................................................................. 26
1.6.3 22q11.2 Deletion Syndrome ...................................................................................... 27
1.6.4 1q21.2 Deletion/Duplication ..................................................................................... 33

v
v
1.6.5 Single Gene Mutations in TOF ................................................................................. 35
1.7 TOF Family Studies and Recurrence Risk Estimates ...................................................... 40
1.7.1 Family Studies: Purpose and Definitions .................................................................. 40
1.7.2 TOF Family Studies .................................................................................................. 43
2 Study Rationale, Aims and Hypotheses ................................................................................. 52
3 Study 1 .................................................................................................................................... 55
3.1 Objectives ........................................................................................................................ 56
3.2 Methods ........................................................................................................................... 57
3.2.1 Analyses .................................................................................................................... 62
3.3 Results .............................................................................................................................. 63
3.3.1 Demographic and Clinical Features in Probands with TOF ...................................... 63
3.3.2 Family History of CHD ............................................................................................. 64
3.3.3 Demographic and Phenotypic Features in Probands from Multiplex and Simplex
Families ................................................................................................................................. 64
3.3.4 Relatives with CHD................................................................................................... 65
3.3.5 Recurrence Risk for CHD ......................................................................................... 69
3.4 Discussion ........................................................................................................................ 70
3.4.1 Recurrence Risk for CHD ......................................................................................... 70
3.4.2 Variable Cardiac Phenotypes in Families ................................................................. 71
3.4.3 Study Advantages and Limitations............................................................................ 77
3.4.4 Clinical Implications ................................................................................................. 79
3.5 Conclusion ....................................................................................................................... 80
4 Study 2 .................................................................................................................................... 89
4.1 Objectives ........................................................................................................................ 90
4.2 Methods ........................................................................................................................... 91
4.3 Results .............................................................................................................................. 93
4.3.1 Family History of CHD ............................................................................................. 94
4.4 Discussion ........................................................................................................................ 95
4.4.1 Study Advantages and Limitations............................................................................ 99
4.5 Conclusion ..................................................................................................................... 100
5 Summary of Thesis and Future Directions ........................................................................... 106

v
vi
5.1 Future Directions ........................................................................................................... 110
Glossary ...................................................................................................................................... 111
References ................................................................................................................................... 113

v
vii
List of Tables Table 1-1. Additional structural and vascular cardiac lesions associated with TOF ...................... 5
Table 1-2. Mechanistic and Anatomical Classification Systems for Congenital Heart Disease .. 13
Table 1-3. Copy number variants in Tetralogy of Fallot, syndromic associations and associations
with other congenital heart defects ............................................................................................... 34
Table 1-4. Single gene mutations in tetralogy of Fallot, syndromic associations and associations
with other congenital heart defects ............................................................................................... 39
Table 1-5. Advantages and Disadvantages of Family Studies with Adult and Child Probands ... 42
Table 1-6. Tetralogy of Fallot family studies and recurrence risk estimates ................................ 50
Table 3-1. Auxiliary cardiac lesions in 498 probands with tetralogy of Fallot ............................ 81
Table 3-2. Extracardiac birth defects in 498 probands with tetralogy of Fallot ........................... 82
Table 3-3. Demographic and phenotypic features in probands with TOF from Simplex and
Multiplex families ......................................................................................................................... 83
Table 3-4. Cardiac anomalies in first to third degree relatives of probands with TOF ................ 84
Table 3-5. Concordance rates for TOF in first to third degree relatives with CHD ..................... 85
Table 3-6. Cardiac anomalies in first degree relatives of 40 probands with TOF ........................ 86
Table 3-7. Recurrence risk for CHD in first to third degree relatives of probands with TOF in the
current and comparison studies ..................................................................................................... 87
Table 4-1. Details of CHD in relatives of 14 adult probands with confirmed or probable de novo
22q11.2 deletions ........................................................................................................................ 102
Table 4-2. Recurrence risk figures for CHD in relatives of adult probands with 22q11DS ....... 104

v
viii
List of Figures Figure 1-1. Anatomy of the Normal Heart and Features of Tetralogy of Fallot ............................. 3
Figure 1-2. Stages in cardiogenesis and contributions from extrinsic cell populations .................. 9
Figure 1-3. Developmental origin of cardiac structures ............................................................... 10
Figure 1-4. Chromosomes with Normal Structure and Copy Number Variants ........................... 23
Figure 1-5. The 22q11.2 Deletion Region .................................................................................... 32
Figure 3-1. Selection and Genetic Workup of TOF Cohort .......................................................... 59
Figure 3-2. Sample pedigree showing degree of relationship of relatives to proband with TOF . 61
Figure 3-3. Simplified pedigrees of all seven multiplex families with probands with TOF and a
first degree relative with a left heart cardiac defect�…�…�…�…�…�…�…�…�…�…�…�…�…�…�…�…�…..68

ix
List of Abbreviations
22q11DS 22q11.2 Deletion Syndrome
AGS Alagille Syndrome
ASD Atrial Septal Defect
AVSD Atrioventricular Septal Defect
BAV Bicuspid Aortic Valve
CHD Congenital Heart Disease
CNV Copy Number Variant
CoA Coarctation of the Aorta
DORV Double Outlet Right Ventricle
FISH Fluorescence in-situ Hybridization
IAA Interrupted Aortic Arch
LA Left Atrium
LV Left Ventricle
LVOT Left Ventricular Outflow Tract
LVOTO Left Ventricular Outflow Tract Obstruction
MAPCAS Multiple Aortopulmonary Collateral Arteries
MV Mitral Valve
PA/VSD Pulmonary Atresia with Ventricular Septal Defect

x
x
PDA Patent Ductus Arteriosus
PS Pulmonary Stenosis
RA Right Atrium
RR Recurrence Risk
RV Right Ventricle
RVOT Right Ventricular Outflow Tract
RVOTO Right Ventricular Outflow Tract Obstruction
SNP Single Nucleotide Polymorphism
TGA Transposition of the Great Arteries
TOF Tetralogy of Fallot
VSD Ventricular Septal Defect

1
Introduction
1 Tetralogy of Fallot
1.1 Overview
Occurring with a prevalence of 1% of live births, congenital heart diseases (CHD) are the most
common of all congenital malformations (1, 2). Tetralogy of fallot (TOF) accounts for approximately
3.5-4% of all heart malformations and is the most common of the cyanotic defects (1, 3). The
prevalence of TOF is approximately 4 in 10,000 live births (1). Although of obvious importance in
childhood, dramatic survival into adulthood has resulted in new issues and unanswered questions
about TOF, not only of late clinical sequalae but also of aetiological factors. As the number of adults
with TOF rises, the complexity of this condition, both in cardiac and extracardiac features, is
increasingly being recognized. However the genetic factors that underlie this variable expression are
poorly understood. In this work familial inheritance in Tetralogy of Fallot is explored with a view to
identification of possible phenotypic patterns that may help to identify the genetic underpinnings of
TOF and cardiac development as a whole.
1.1.1 Historical Descriptions of TOF
As the name suggests, TOF consists of four major abnormalities occurring together; subpulmonary
infundibular stenosis, ventricular septal defect, aortic override and right ventricular hypertrophy
(Figure 1-1). The first description of this condition may have been by Danish anatomist Nils Steno
who in 1673 reported these abnormal cardiac findings in a stillborn infant (4). Sandifort in 1777

2
described a �“blue boy�” with the anatomic features of TOF and William Hunter in 1784 described the
cyanotic spells and poor growth in a boy with TOF (4). However it was Louis-Etienne Fallot in 1888
who was the first to correlate the clinical and pathological features of this condition and recognize
them as a �“tetralogie�” after studying a series of patients (4). Maude Abbott in 1924 coined the term
�“tetralogy of Fallot�” and in 1936 produced the first illustrations of the pathologic and circulatory
features, and described x-ray and electrocardiographic features of TOF (3, 4).
1.1.2 Anatomy and Variants of TOF
Although TOF consists of four constant abnormalities, the condition actually represents a
morphologic spectrum from cases with minimal pulmonary stenosis to cases with severe pulmonary
obstruction as is represented in the most extreme form of TOF, pulmonary atresia with ventricular
septal defect (VSD) (5, 6). The unifying morphologic feature however, is anterocephalad deviation of
the outlet septum in relationship to the rest of the ventricular septum, which along with hypertrophy
of the subpulmonary infundibulum give rise to the right ventricular outflow tract obstruction
(RVOTO) that is the hallmark of this condition (6).
The VSD in TOF is usually single, large, and nonrestrictive and in the majority of cases it is
perimembranous in location (3, 6). Infundibular stenosis is present in almost all TOF cases although
other sites of obstruction including valvular, supravalvular and involving the branch pulmonary
arteries can also be present (7). The pulmonary valve rarely causes obstruction but is abnormal in the
majority of cases. Abnormalities of the pulmonary arteries themselves can also occur with stenosis
and hypoplasia being common. There can also be anomalous origins of one or both pulmonary

3
arteries, usually from part of the aorta (7). The degree to which the aortic valve is connected with the
right ventricle, aortic override, varies between 5-95% in TOF (6).
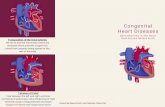
Figure 1-1. Anatomy of the Normal Heart and Features of Tetralogy of Fallot
a. Normal heart structure promotes unidirectional flow of deoxygenated blood (blue) into the lungs and
oxygenated blood (red) into the aorta.
b. In TOF, right ventricular outflow tract obstruction impedes blood flow to the lungs and the VSD and
overriding aorta (*) promote flow of deoxygenated blood in the systemic circulation.
RA- right atrium, LA- left atrium, RV- right ventricle, LV-left ventricle, VSD- ventricular septal defect,
RVOT- right ventricular outflow tract
From the Multimedia Library of Congenital Heart Disease, Children�’s Hospital, Boston, MA, editor Robert
Geggel, MD, www.childrenshospital.org/mml/cvp with permission.

4
1.1.3 Associated Lesions
Several cardiac and vascular lesions can co-exist with TOF. Table 1-1 displays some of the more
commonly reported lesions. An atrial septal defect (ASD) is frequently associated with TOF in up to
20% of cases (5, 7, 8). Other potential cardiac lesions include a patent foramen ovale, a second
muscular inlet VSD and an atrioventricular septal defect, which most often co-exists with TOF in the
setting of Down syndrome (6, 7).
Vascular lesions associated with TOF are many. These include a right aortic arch in 25% of patients
that sometimes is present with an aberrant left subclavian artery in 3 % (7). Many patients also have
well-developed aorto-pulmonary collaterals, even without pulmonary atresia (9).

5
Table 1-1. Additional structural and vascular cardiac lesions associated with TOF
Lesion Frequency in TOF References
Structural
Pulmonary atresia 12% (8)
Atrial septal defect 20% (8)
Additional VSD 5% (8, 10)
Atrioventricular septal defect 1-3% (6-8)
Patent ductus arteriosus 4-6% (8, 10)
Dextrocardia 2% (8)
Vascular
Right aortic arch 15-25% (7, 8, 10)
Coronary artery anomaly 3% (11)
Aberrant subclavian artery 3-8% (7, 12)
MAPCAS 2% (10)
MAPCAS- multiple aortopulmonary collaterals, VSD- ventricular septal defect

6
1.1.4 Pulmonary Atresia with Ventricular Septal Defect
Pulmonary atresia is the absence of a communication between the right ventricle and the main
pulmonary artery. In an extreme variant of TOF, pulmonary atresia occurs with a VSD (6, 7). The
entity of pulmonary atresia with ventricular septal defect (PA/VSD) can actually represent a clinical
spectrum from simple atresia of the pulmonary valve to severe atresia of the main pulmonary artery
or its major branches (6). In this condition, collateral arteries that usually arise from the aorta or its
branches supply some or all of the pulmonary blood flow. These major aortopulmonary collateral
arteries, MAPCAs, are essential for gas exchange and lung parenchymal development (6, 9).
PA/VSD is also often associated with auxiliary cardiac and vascular lesions including a right aortic
arch in 25% of cases, aberrant subclavian artery, dextrocardia, ASD and atrioventricular septal
defects (7).
1.2 Development of the Heart
Beginning at 3 weeks of embryonic life, the heart is the first organ to develop in the human embryo
(13). This complicated process of differentiation is usually complete by week 8 of gestation and is
regulated at every stage by many genetic and epigenetic factors.
Cardiac progenitor cells develop in the embryonic mesoderm. These progenitors condense to form
two lateral heart primordia that contain myocardial and endocardial cell lineages (13, 14). The fusion

7
of these precardiogenic plates forms a beating heart tube (Figures 1-2 and 1-3). Early markers
expressed in this precardiogenic tissue include NKX2.5 and GATA4 (14, 15). Specification of these
pluripotent cells into cardiac cells that will contribute to the conduction system, atria, ventricles and
outflow tract also begins at this stage and is guided by transcription factor expression (13, 14). The
next step in the process is genetically determined rightward looping of the heart which begins right-
left determination in the embryo (14). After the initial looping stage, cells from the pharyngeal
mesoderm, the secondary heart field, migrate into the developing heart (15) (Figure 1-2). The
secondary heart field contributes to formation of the outflow tract, much of the right ventricle and to
a lesser extent the left ventricle (13, 15) (Figure 1-3). Subsequently, septation of the heart into right
and left atria and ventricles and morphologic development of their associated valves begin.
Coincident with this process of septation and valvulogenesis, cells from the dorsal rim of the neural
crest migrate into the embryo where they have various destinations and fates, including craniofacial
structures (14-16). In cardiac tissue, these cells contribute to the septation of the outflow tract into
distinct vessels of the aorta and pulmonary artery and also contribute to the formation of the arteries
of the aortic arch and the ductus arteriosus. Ablation of the neural crest in animal models results in
varying cardiac outflow tract malformations including TOF, and are similar to those found in
humans, for example in 22q11.2 deletion syndrome (17, 18). Secondary heart field ablation also
results in conotruncal anomalies such as TOF and double outlet right ventricle (15, 19). A
perturbation in the development or migration of these extrinsic cell populations might partly explain
the co-existence of extracardiac defects with congenital cardiac anomalies (16, 17, 20). Another
extrinsic cell population, proepicardial cells from the lateral mesoderm or septum transversum
migrate over the surface of the heart to form the epicardium and eventually differentiate into the
coronary vessels (14). A subpopulation of these cells may also infiltrate the atrioventricular canal
and participate in valve and septum formation (14).

8
1.2.1 Cardiogenesis and Transcription Factors
The functions of transcription factors, involved in every phase of normal cardiac development, and
their implications in CHD are being elucidated by studies in genetically targeted mouse models.
Transcription factors Nkx2.5 and Gata4 are involved in early specification of pluripotent cells and are
among the earliest markers of cardiomyocytes (14). Tbx5 is also an early cardiac marker, present
primarily in the atria and left ventricle at the primitive heart tube stage. Homozygous null mutations
of Nkx2.5, Gata4 and Tbx5 are associated with disruption of atrial and ventricular septation, looping
and chamber differentiation. These mutations are lethal by embryonic day 10.5 (14). Nkx2.5 and
Tbx5 are both expressed throughout the conduction system of the heart (14, 21).
Tbx1 is a transcriptional regulator of the secondary heart field and appears to control cardiac neural
crest migration (13, 22). Tbx1 null mice have embryonic lethality and have a number of defects
affecting outflow tract growth and septation, interventricular septation and conal alignment (14).
Fog2 is expressed in the embryonic mouse heart and septum transversum. Homozygous null Fog2
mutations in mice result in cardiac defects resembling TOF. Epicardial ablation studies in chickens
also have a �“TOF-like�” phenotype (14).

9
Figure 1-2. Stages in cardiogenesis and contributions from extrinsic cell populations
Multiple cell types extrinsic to the original embryonic cardiac tissue contribute to the formation of the
mature heart. From Epstein et al NEJM 2010; 368:1638-1647 (15). Reprinted with permission.

10
Figure 1-3. Developmental origin of cardiac structures
Cardiogenic precursor fields are specified to form regions of the heart tube; b The secondary heart field (SHF, yellow) contributes to
formation of the outflow tract and right ventricle; c Cardiac chamber formation and septation of the heart. Neural crest cells populate the
aortic arch arches (III-IV) d Mature heart showing contributions from various cell populations. A-artery, V-ventricle, RV-right ventricle,
LV-left ventricle, RA-right atrium, LA-left atrium, PA-pulmonary artery, Ao-aorta, Da-ductus arteriosus, RSCA, right subclavian artery,
RCC-right common carotid, LCC-left common carotid, LSCA-left subclavian, AVV-atrioventricular valve.
From Srivastava, D Annu. Rev. Pathol. Mech. Dis. 2006. 1:199-213 (13). Reprinted with permission.

1.3 Classification of CHD
CHD can be classified by various methods. One system often used groups lesions based
on the anatomical location of the defect (Table 1-2). Under this system, TOF is classified
with lesions of the right ventricular outflow tract (RVOT), also known as conotruncal
lesions (23). Other CHD included in this category are pulmonary stenosis at various
levels and double outlet right ventricle (23). Other conotruncal lesions include D-
Transposition of the great arteries and truncus arteriosus. Lesions of the left ventricular
outflow tract (LVOT) include aortic stenosis at various levels, bicuspid aortic valve
(BAV) and coarctation of the aorta (23). Various shunt lesions also occur at different
levels. Intracardiac shunts include atrial and ventricular septal defects and extracardiac
shunts include patent ductus arteriosus.
However, another school of thought suggests CHD could be classified by developmental
biology (24). This so-called �“mechanistic�” approach sees CHD grouped into five
categories based on shared developmental processes (24, 25) (Table 1-2). Category I
lesions are thought to result from disordered cell migration into the developing heart from
the mesenchymal tissue of the neural crest and branchial arteries (24). All conotruncal
abnormalities including TOF are included in this group (24, 25). Category II includes
defects associated with abnormal embryonic blood flow and includes hypoplastic left
heart, pulmonary valve stenosis and coarctation of the aorta. Class III defects result from
abnormal cell death and includes Ebstein�’s anomaly. Class IV and V are associated with

extracellular matrix abnormalities and targeted growth defects (25). Left and right heart
congenital lesions can therefore be grouped together in this mechanistic approach.

13
Table 1-2. Mechanistic and Anatomical Classification Systems for Congenital Heart Disease
Mechanistic Classification Anatomical Classification
Category Mechanism Cardiac Defect Category Cardiac Defect
I Disordered cell migration Tetralogy of fallot
Truncus arteriosus
Transposition of the great arteries
DORV
Interrupted aortic arch-B
Aorto-pulmonary window
VSD (type1, supracristal)
Right Ventricular Outflow Tract Tetralogy of fallot
Truncus arteriosus
Double outlet right ventricle
D-TGA
Pulmonary stenosis
Valvular
Subvalvular
Supravalvular
Bicuspid or unicuspid pulmonary valve
Pulmonary atresia
II Disordered Haemodynamic Flow
Hypoplastic left heart
Coarctation of aorta
Aortic valve stenosis
Bicuspid aortic valve
Pulmonary valve stenosis
Pulmonary atresia
VSD (type II)
Patent ductus arteriosus
Left Ventricular Outflow Tract Aortic stenosis
Valuvular
Supravalvlar
Subvalvular
Bicuspid aortic valve
Coarctation of aorta
Hypoplastic left heart

14
Mechanistic Classification Anatomical Classification
III Cell death Ebstein anomaly
VSD (muscular)
Shunts Intarcardiac
ASD
VSD
AVSD± Cleft mitral
valve
Extracardiac
Patent ductus arteriosus
IV Extracellular matrix anomalies
Endocardial cushion defect
VSD (type III)
V Targeted growth defects Total anomalous pulmonary venous return
Single atrium
VSD- ventricular septal defect, AVSD- atrioventricular septal defect, DORV- double outlet right ventricle, D-TGA- dextro- transposition of the great arteries (References 23-25).

15
1.4 Clinical Features and Management of TOF
TOF is slightly more common in males than in females (5). Patients with TOF most often present
in infancy with cyanosis due to right to left shunting of blood at the level of the VSD (6). The
degree of right ventricular outflow tract obstruction (RVOTO) often correlates with the timing of
presentation. Consequently, patients with mild pulmonary obstruction can present in adulthood
with minimal cyanosis, the so-called �“pink TOF�”, while patients with severe obstruction may
present soon after birth on closure of the ductus arteriosus (6, 7). Dynamic pulmonary
obstruction also occurs in TOF and is believed to be the origin of the hypercyanotic or �“Tet
spells�” which often occur in infants between 2 to 4 months of age (6, 7). Physical examination
findings may vary with the degree of RVOTO but commonly include a single second heart sound
and the systolic ejection murmur of pulmonary stenosis (7).
The diagnosis of TOF is often established on echocardiographic assessment of the four major
features (6, 7). Cardiac catheterization or cardiac magnetic resonance imaging is not usually
necessary for diagnosis but may be required to define vascular and RVOT anatomy. TOF can
also be diagnosed with considerable accuracy on prenatal echocardiogram (3, 26, 27). Referrals
for foetal echocardiogram are often made after an abnormal obstetric ultrasound, worrisome
amniocentesis or because of the history of CHD in a close relative (26). Termination of
pregnancy upon foetal detection of TOF is an issue and in one series was performed in 54%
cases (28).

16
1.4.1 Extracardiac Features of TOF
The clinical phenotype in TOF is broadly heterogeneous. In some patients, the cardiac defect
appears to be isolated while in others TOF appears to be part of a multisystem disorder (3, 29-
31). The latter presentation is often referred to as �“syndromic�”. Some syndromic patients have
clinical features that fit into a recognized genetic pattern such as 22q11 Deletion Syndrome
(22q11DS) (32), but there is a subgroup with syndromic features but no known genetic aetiology
(29). Approximately 17-25% of TOF patients have extra-cardiac congenital anomalies (29, 31,
33, 34). The most common such congenital defects include urogenital, musculoskeletal and
gastrointestinal anomalies (29, 31). However, a number of TOF patients also have late onset
conditions such as neuropsychiatric disease. These may be generally more prevalent in those
with a syndromic presentation (29).
1.4.2 Surgical management of TOF
The evolution of cardiac surgery has revolutionized the management of TOF. In 1944 the first
Blalock-Taussig anastamosis was performed, connecting the pulmonary artery and subclavian
artery and thus improving oxygenation of blood via the lungs (4, 6). Various other palliative
shunt procedures that augment pulmonary blood flow were also developed. Previously these
palliative shunts were performed prior to intracardiac repair but contemporary practice is for
early primary repair at presentation or when patients become symptomatic (7, 35).

17
In 1954 Lillehei and colleagues performed the first successful intracardiac TOF repair (4). The
goals of intracardiac repair are to close the VSD and relieve the RVOTO. Thus repair
traditionally includes a right ventriculotomy with patch augmentation of the infundibulum and
pulmonary annulus along with VSD closure (7).
1.4.3 Natural and Modified History of TOF
The prognosis for children with unrepaired TOF is bleak with a reported survival of just 24% at
10 years of age (36, 37). Cases of unusual longevity in patients with unrepaired TOF have
however been reported (38). The evolution of surgical management of this condition has
dramatically improved the outlook for patients with TOF and survival into the sixth decade is
now expected for patients with repaired TOF (39, 40).
With the increasing experience with adults with TOF, it has become clear that the initial
intracardiac surgery is a reparative and not a curative procedure. Rather, secondary sequalae such
as arrhythmias and heart failure are experienced by many patients (3, 6, 40). Re-operation,
especially for pulmonary valve replacement due to post-operative insufficiency, is necessary in
the long-term for the majority of patients. (41, 42).

18
1.4.4 Pregnancy and Reproductive Issues in TOF
With survival into adulthood expected for patients with corrected TOF, pregnancy, reproductive
fitness and concerns about CHD recurrence are important issues for the patient and managing
cardiologist. Physiological changes of pregnancy include an increase in blood volume, heart rate
and cardiac output. These changes can be challenging for the patient with TOF who may already
have significant pulmonary regurgitation and/or right ventricular dysfunction post surgery (43,
44). However, pregnancy is generally well tolerated in women with TOF (45, 46). Spontaneous
abortion rates are between 15-19%, the majority being first trimester losses (45, 47). This rate is
similar to the miscarriage rate in women without TOF (48). One study did however report a
considerably higher miscarriage rate of 27% (49). In terms of neonatal outcome, there appears to
be an increased risk for adverse events including premature births, low birth weight and
respiratory distress syndrome (44, 47, 50). Recurrence risk for CHD and other congenital
anomalies are increased in offspring of mothers with TOF over population expected rates (44,
45, 49). The recurrence for CHD in offspring will be discussed further in section 1.7.
Although there appears to be no impaired fertility in women with TOF, a considerable number
may elect not to have children (45, 47, 51). In one study, of 83 women with TOF of reproductive
age, 57 (69%) were childless, 41 (72%) by choice (47). In another study of 118 women with
varying CHD including TOF, 18 (23%) of 80 women in whom pregnancy was not
contraindicated reported being advised against pregnancy by a health-care provider (52).
Reproductive fitness in men with TOF has not been specifically studied.

19
1.5 Aetiology of TOF: Evidence for Genetic Origins
1.5.1 Familial Clustering and Twin Studies
The vast improvements in medical and surgical management of TOF have led to renewed interest
in aetiological factors. While management of TOF is largely streamlined, the search for
causative factors has proven to be complex and heterogeneous. Historically, both environmental
and genetic factors were thought to be strongly associated with TOF (33, 53-55), although
environmental factors received more attention. Indeed, maternal factors such as rubella and other
viral infection, diabetes mellitus and exposures to teratogenic agents such as thalidomide during
pregnancy have been shown to be associated with CHD including TOF in various
epidemiological studies (56-58). The overriding theory is that these environmental exposures
occurred during a critical period in cardiac development, which then resulted in formation of
TOF (33, 57). The clear relationship between certain exposures and TOF and the limitations with
proving genetic studies in previous decades led some investigators to postulate that
environmental factors were probably more important than genetic factors in TOF causation (33).
However there is growing evidence of a profound genetic basis to TOF. Several reports of strong
familial clustering of TOF and related lesions can be found in literature dating back to the 1950s
(33, 59-62). One of the most striking examples was a family described by Pitt in 1962 in which
11 members had TOF or one of its component cardiac lesions (59)). There are also cases
described in which multiple offspring with TOF were born to consanguineous parents (63).
Reports of TOF in animal homologies have shown similar familial clustering of lesions as has

20
been seen in human families. Studies in pigs, dogs and mice have all supported this tendency
(54, 64).
Very little data on twin studies in CHD and no adoption studies in CHD can be found in the
literature. There are no specific studies in large cohorts of twins with TOF, although case reports
of twins with TOF can be found (65-67). Findings from studies of any CHD in twins have
supported a strong genetic aetiology. In the 1967 study by Nora et al., CHD was found in both
members of 46% monozygotic twins and only 4.2% nonidentical twins (54, 68). Findings of a
more recent population CHD study also supported the greater occurrence of CHD in
monozygotic than dizygotic twins (2). Interestingly, a recent study reported that dizygotic twins
more often had both members affected with CHD than normal siblings (69). The authors
suggested that this was evidence of an environmental influence during pregnancy in CHD
causation (69).
1.5.2 Genetic Principles of Disease
Although there is growing evidence for a strong genetic aetiology for TOF, the understanding of
underlying genetic mechanisms and inheritance is limited. In order to appreciate basic principles
governing genetic disease, it is necessary to define some key terms. The genotype is the set of
alleles that are found at a particular chromosomal locus while the phenotype is the clinical,
cellular and biochemical expression of a genetic trait. Phenotypic expression of a genetic trait
can be modified by other genetic or environmental factors. When the frequency of phenotypic

21
expression of a trait is less than 100%, it is said to have reduced penetrance. Variable
expressivity exists when the phenotypic severity differs between two individuals with the same
genotype. Variable expressivity and reduced penetrance of genetic traits can be due to modifier
genetic influences, which are genetic or environmental factors that affect expression of genes
(70).
A genetic disorder with a number of phenotypes determined by different genes at different loci is
said to have genetic heterogeneity (70). Alternatively, clinical or phenotypic heterogeneity exists
when variants of the same gene result in distinct phenotypes (70).
Diseases that are wholly or partly genetic in origin can be classified into three main categories,
namely chromosomal diseases, single gene diseases and multifactorial diseases (70). Evidence of
all three forms of inheritance can be found in TOF and specific examples of these are discussed
below.
1.5.2.1 Chromosomal Diseases
Chromosomal diseases result from an excess or deficiency of genes in an entire chromosome
(gross chromosomal change) or chromosomal segment, for example in Trisomy 21 or Down�’s
Syndrome (70). Smaller changes involving deletions or duplications of segments of
chromosomes, copy number variants (CNVs), such as deletion 22q11.2, can also cause disease

22
(Figure 1-4) (2, 71, 72). These deletions and duplications occur by a variety of mechanisms and
can result in haploinsufficiency or over expression of a number of contiguous genes, often with a
negative effect on phenotype (71, 72). Approximately 12% of the human genome is estimated to
be subject to this variation, which may partly account for phenotypic differences between
individuals (73, 74) and can contribute to reduced penetrance and variable expression of genetic
traits (73). These changes can be inherited polymorphisms or can arise spontaneously, so called
de novo CNVs. A growing number of diseases have been linked with CNVs including congenital
and acquired heart disease, psychiatric and developmental disorders and cancer (71, 72, 75, 76).

23
Figure 1-4. Chromosomes with Normal Structure and Copy Number Variants
From Bassett et al. American Journal of Psychiatry 2010 (72). Reprinted with permission from the
American Journal of Psychiatry, (Copyright © 2010). American Psychiatric Association.

24
1.5.2.2 Single Gene Diseases
Single gene defects are caused by mutations in individual genes (70). In dominant inheritance,
one copy of a gene is sufficient to produce a phenotype and a parent carrying such a trait has a
50% chance of having an affected child with each successive pregnancy. Alternatively if two
copies of a gene are required for expression, it is a �“recessive�” trait. In recessive inheritance, two
parents carrying the allele of interest can expect a 25% probability with each pregnancy, of
having an affected child. When a variant allele is found in more than 1% of the population it is
known as a genetic polymorphism whilst rare variants occur in less than 1% of the population
(70). Many rare variants are mutations associated with genetic diseases but some polymorphisms
may also increase disease susceptibility. Polymorphisms may involve a single base pair (single
nucleotide polymorphism) or may involve larger segments of DNA (e.g. in copy number
polymorphism) (70).
1.5.2.3 Multifactorial Inheritance
Some common diseases show the tendency for familial aggregation but do not occur in families
in the proportions expected in single gene disorders. These diseases are subject to multifactorial
(or complex) inheritance, wherein many genetic loci interact, with a variable environmental
contribution, to increase susceptibility to a disease (54, 70). Certain mechanisms thought to
operate in complex diseases include genetic heterogeneity, genetic modification and epigenetic
effects such as genomic imprinting (differences in expression of genes depending on inheritance
from the mother or father) (70, 77).

25
Many congenital as well as adult onset diseases are thought to be subject to multifactorial
inheritance e.g. cleft palate, autism and schizophrenia (70, 77, 78). The theory of multifactorial
inheritance is that close relatives are more likely to have the same gene-gene and gene-
environment interactions that lead to disease (70). Hence in this type of inheritance, the greater
number of alleles a relative has in common with the affected individual, the greater is the
susceptibility of that relative to the particular disease. Therefore first degree relatives would be
more likely than second degree relatives to have disease and monozygotic twins more often have
both members affected than dizygotic twins. The risk to relatives also increases with the number
of affected relatives in a family.
The recurrence risk is the prevalence of disease among relatives of a proband while the
recurrence risk ratio compares this prevalence to that of affected individuals in the population.
The recurrence risk for first degree relatives of an individual with a multifactorial disease is
estimated to be between 1-5% (54). Family, twin and adoption studies are often used to assess
multifactorial inheritance of a disease and to generate empiric risk estimates.
Nora in 1968 ascribed TOF and all CHD not associated with a known genetic syndrome, to
multifactorial inheritance (54). Using results from their family and twin studies and other studies
available in the literature at the time they found that the data conformed to the principles of
multifactorial inheritance. They however acknowledged that in some pedigrees, there appeared
to be single gene inheritance in a dominant or recessive pattern (54). Specific family studies in
TOF are discussed in Section 1.7.

26
1.6 Known Genetic Causes of TOF: Variable Expressivity and Phenotypic Heterogeneity
1.6.1 Molecular techniques for detection of genetic factors in TOF
Since light microscopy for karyotype assessment has been in use since the 1950s, the association
of TOF with Down�’s syndrome and other trisomies has long been known (79). These trisomies
together account for up to 7% of TOF cases (80). Historically, the remaining TOF cases were
ascribed to multifactorial inheritance. However, with the advent of molecular techniques that
improve the resolution of karyotype (~4-5 MB) and allow detection of submicroscopic genetic
alterations, more positive genetic associations have been made. Fluorescent in-situ hybridization
(FISH) is one such technique that allows for targeted detection of smaller chromosomal
aberrations such as 22q11.2 deletions (81). More recently, high resolution technology to perform
genome wide screening for genetic rearrangements such as CNVs has been developed and
detection of chromosomal changes as small as 20kb is now possible (82-84).
Some important known molecular causes of TOF are described below.
1.6.2 Copy Number Variants
Copy number variants (CNVs) have been associated with both syndromic as well as non-
syndromic presentations of TOF (Table 1-3). The most common CNV linked with TOF is

27
22q11.2 deletion in the setting of 22q11.2 Deletion Syndrome (85). This deletion is associated
with about 7-15% TOF cases and is the most common known genetic cause of TOF (30, 80, 85,
86). More recently, other copy number variants, apart from 22q11.2 deletions have been
associated with TOF (Table 1-3). A recent study of copy number variation in 512 children with
non-syndromic TOF estimated that CNVs are causative in a minimum of 10% cases (84). In that
series, two cases with 22q11.2 deletions were included in the estimate (84). The two most
significant CNVs so far identified in TOF, 22q11.2 deletions and 1q21.1 deletions/duplications
are discussed in more detail below.
1.6.3 22q11.2 Deletion Syndrome
1.6.3.1 Prevalence and Transmission of Deletion 22q11.2
With a prevalence of 1 in 4000 live births 22q11.2 Deletion Syndrome is the most common
microdeletion syndrome in humans (87). This is a multisystem disorder comprising various
previously described clinical syndromes including Velocardiofacial Syndrome, DiGeorge
syndrome and Conotruncal anomaly face syndrome (81, 88). The 22q11.2 deletion occurs as a de
novo mutation in over 90% of newly diagnosed cases (89, 90). When inherited, these deletions
are transmitted in an autosomal dominant fashion (88). Typical deletion sizes are between 1.5 or
3 Mb, with about 90% of cases having the 3 Mb deletion (90-92). The 22q11 region is prone to
structural rearrangements due to the many low copy repeats in this part of the genome (93). An
excess of deletions of maternal origin has been reported (90, 94) and may be due to a relative
paucity of deletions of paternal origin in males (90). Clinical laboratory testing for 22q11DS has

28
been available since 1993-1994 and consists of standard fluorescence in-situ hybridization
(FISH) techniques (81).
1.6.3.2 Clinical Spectrum of 22q11DS
22q11DS is a developmental disorder that affects third and fourth pharyngeal pouch structures,
namely the heart and great vessels, thymus, parathyroid glands and craniofacial structures (95).
Ablation of the cardiac neural crest cells has been shown to result in cardiac phenotypes similar
to those seen in 22q11DS and it has been postulated that this syndrome may be linked to
improper neural crest cell migration into the pharyngeal arch structures (96, 97). Therefore,
features of the syndrome that may recognized in infancy include cardiac and other birth defects,
hypocalcaemia, variable immunodeficiency and some facial dysmorphism (98-100). However,
the presence of later onset manifestations, particularly neuropsychiatric features, is increasingly
being recognized (98, 101, 102). Schizophrenia for example, is present in approximately 25%
22q11DS cases and Parkinsonism has also been reported (98, 103, 104). Thyroid disease is also a
feature in about 20% cases (98). A wide-ranging clinical spectrum from severe to extremely mild
phenotypes occurs in 22q11DS and the condition is one of the most under-recognized syndromes
in humans (98, 99, 105, 106). Despite the fairly consistent deletion size, there is variable
expression and severity of all 22q11DS features, including CHD, within families and even
among monozygotic twins (88, 90, 107). Although virtually any system may be affected the
classic extracardiac features of dysmorphic facial features, intellectual disability and
velopharyngeal insuffiency associated with hypernasal speech occurring together have great
predictive value for 22q11DS (32, 98).

29
1.6.3.3 CHD in 22q11DS
CHD occurs in roughly 40% 22q11DS cases when ascertainment bias is accounted for (98, 106).
The most common associated category of cardiac lesions is conotruncal, with interrupted aortic
arch being most strongly associated (30, 108-110). Approximately 50% of cases of interrupted
aortic arch type B are associated with a 22q11.2 deletion (110). Milder congenital cardiac lesions
such as isolated pulmonary stenosis and VSD also occur in 22q11DS (30, 111). There is
evidence that auxiliary cardiac lesions such as right aortic arch, aberrant subclavian artery and
pulmonary atresia/MAPCAS are more common in CHD in the setting of 22q11DS than in
nonsyndromic CHD though they are not predictive of this condition (29). Unique late cardiac
sequalae such as aortic root dilatation have also been reported and premature death, though not
necessarily of cardiac origin, is also a concern in this population (112, 113).
Figure 1-5 shows the genes that are present in the 22q11.2 region. One of the most extensively
studied is TBX1, a transcription factor known to have an essential role in normal pharyngeal and
cardiac development (22, 95, 114). Haploinsuffiency of Tbx1 in mouse models produces
conotruncal malformations similar to those seen in humans with 22q11DS (115) while Tbx1 null
mice have a more severe phenotype and embryonic lethality (116). A possible explanation for
the variable expressivity in 22q11DS, Tbx1 gene dosage variation in mouse models produces the
full spectrum of CHD associated with human 22q11DS (117, 118). Mutations in TBX1 have
been identified in patients with typical 22q11DS phenotype, including cardiac defects, but
without 22q11.2 deletions (119-122). TBX1 mutations that result in loss as well as gain of

30
function have been described and both are associated with a 22q11DS like phenotype, including
cardiac defects. This suggests that there is a threshold of TBX1 activity above which and below
which the risk for malformations increases (123). These mutations are associated with significant
variable expression, within the same family (120, 122, 123). More recently, three rare variants of
TBX1 have been reported in nonsyndromic TOF patients, inherited from a phenotypically
normal parent (normal heart) in all reported cases (123). One of the identified variants in a
patient with TOF and right aortic arch was associated with a 40% reduction in TBX1
transcriptional activity. Mouse models show that the incidence of cardiac outflow tract defects
increased at Tbx1 transcriptional activity below 20% (117). These investigators therefore
postulated that hypomorphic alleles that reduce, but do not ablate, Tbx1 activity may increase
susceptibility for nonsyndromic CHD (123).
However, the variable expressivity of CHD and other birth defects in 22q11DS has also been
postulated to also involve genetic variants outside of the 22q11.2 region (105, 115). One genetic
variant that has been investigated as a potential modifier of CHD in 22q11DS is vascular
endothelial growth factor (VEGF), a protein that plays a critical in angiogenesis (124, 125) and
that has been shown to play a role in pharyngeal arch artery patterning (126). Mice with certain
vegf variants associated with lower gene transcriptional activity have been reported to have
cardiovascular defects resembling those in 22q11DS (126). In addition, vegf was suggested to
interact with tbx1, as reduced tbx1 activity has been noted in mice with these vegf variants. One
study of 90 individuals with 22q11DS reported a greater frequency of VEGF promoter
polymorphisms associated with reduced gene transcription in the 58 individuals with 22q11DS
and cardiac defects than in normal controls (126). Further, VEGF variants also have been

31
implicated in nonsyndromic TOF and other CHD (127). In one study of 148 probands with
nonsyndromic TOF and their parents, overtransmission of these low expression VEGF variants
to children with TOF was reported (127). However, the largest study to date, which included 595
individuals with TOF with no 22q11.2 deletion, failed to identify an association between genetic
variation in VEGF and CHD (128).
Intrafamilial variability in cardiac phenotypes is well described in 22q11DS and could
potentially be due to interaction of the effects of the deletion with genetic variants within the 22q
region or variants elsewhere in the genome. Case reports of isolated CHD in six first-degree
relatives with CHD but no 22q11.2 deletions (129, 130) suggest the possible existence of such
inherited variants affecting CHD expression in 22q11DS.

32
Figure 1-5. The 22q11.2 Deletion Region

33
1.6.4 1q21.2 Deletion/Duplication
One study based on 512 subjects with TOF suggested that CNVs at chromosome 1q21.2 are
associated with 1% nonsyndromic sporadic TOF cases (84). Other studies have shown 1q21.1
deletions and duplications to be present in cases truncus arteriosus, BAV and aortic arch
abnormalities, including coarctation of the aorta and interrupted aortic arch (131, 132). Although
a nonsyndromic phenotype of TOF associated with CNVs at 1q21.1 has so far been described
(84), syndromic presentations of other CHD such as truncus arteriosus and patent ductus
arteriosus have been reported (131). Cardiac conduction abnormalities may also be associated
with polymorphisms at 1q21.1 (132).
The phenotype of CNVs at chromosome 1q21.1 is extremely variable and reduced penetrance
has also been reported (131, 132). Similar to 22q11.2 deletions, duplications and deletions at
chromosome 1q21.1 (usually 1.35MB) are also strongly associated with neuropsychiatric and
developmental disorders such as autism spectrum disorder and schizophrenia (72, 131, 133).
Mild dysmorphic features as well as other congenital abnormalities are also described (74, 131,
134, 135).

34
Table 1-3. Copy number variants in TOF, syndromic associations and associations with other congenital heart defects
Copy number variant
Reports in patients with TOF
Frequency in TOF
Syndromic Features/association
Genes associated with CHD
Other CHD References
22q11.2 del Multiple 7-15% 22q11.2 Deletion Syndrome
TBX1 VSD, IAA, TA (30, 100, 108)
1q21.1 del/dup 5/512 patients with nonsyndromic TOF in one study
~1% No TA, BAV, CoA, IAA
(84, 131, 132)
3p25.1 dup 2/114 patients in one study
<1% No RAF1 (84)
7p21.3 dup/del 2/114 patients in one study
<1% No (84)
9q34.3 del 1/114 patients in one study
<1% No NOTCH1 (84)
20p12.2 del 1/114 patients in one study
<1% No JAG1 (84)
13q13.1-q13.2 del
4 patients from various studies
<1% MR/DD, dysmorphic facies, extracardiac congenital anomalies
Subaortic stenosis, AVSD, single ventricle, absent MV, PDA
(137)
5q35.1-q35.3 del
2 patients in one study
<1% MR, dysmorphic features, microcephaly
NKX2.5 Ebstein anomaly, ASD
(138, 139)
del- deletion, dup-duplication, MR- mental retardation, AVSD- Atrioventricular septal defect, VSD-Ventricular septal defect, IAA- Interrupted aortic arch, BAV-Bicuspid aortic arch, CoA- Coarctation of aorta, MV- Mitral valve, PDA- Patent ductus arteriosus, ASD-Atrial septal defect, TA- truncus arteriosus

35
1.6.5 Single Gene Mutations in TOF
Linkage analysis and candidate gene approaches have been used to identify various single gene
mutations that are associated with TOF (14). The known mutations to date collectively are
estimated to cause about 1-5% of TOF cases (80, 140) and can be associated with syndromic
(e.g. Alagille syndrome) as well as nonsyndromic presentations (Table 1-4). An autosomal
dominant pattern of inheritance, often with reduced penetrance and variable expressivity, is
described for most of these mutations. The majority of the mutations identified in TOF occur in
genes encoding transcription factors and signaling proteins, important in cardiac development
(14, 141). Many of these transcription factors are expressed very early in cardiogenesis, affecting
the specification of different cell types (13, 14). The importance of these factors in development
and their early expression is indicated by the diverse cardiac phenotypes associated with
mutations (14).
1.6.5.1 NKX2.5 Mutations
Mutations in the homeobox transcription factor NKX2.5 have been associated with
nonsyndromic CHD including TOF (140, 142). A dominant locus associated with cardiovascular
malformations and conduction abnormalities has been mapped to chromosome 5q35 (142).
Mutations within the homeodomain, the critical part of the protein that interacts with DNA, are
typically associated with conduction abnormalities (143). Over 30 different mutations in NKX2.5
have been identified (14).

36
NKX2.5 mutations have been described in association with nonsyndromic TOF and are
suggested to cause roughly 4% TOF cases overall (140, 142, 143). Golmuntz et al prospectively
screened 150 patients with TOF and found 6 with NKX2.5 mutations (140). Although the
numbers were small they found a greater prevalence of pulmonary atresia and right aortic arch in
the mutation carriers than would be expected in the normal TOF population. There was also
evidence of reduced penetrance in that first degree relatives of probands in this study were
mutation carriers but had structurally normal hearts (140). These mutations have also been found
to cause various other cardiac structural abnormalities. The most common such abnormality is
ASD (142, 144), often in association with AV conduction abnormalities (142, 145), although
various other conotruncal defects such as truncus arteriosus, double outlet right ventricle and
interrupted aortic arch have also been described (143) . Though much lower in frequency,
associations with left heart lesions such as coarctation of the aorta, bicuspid aortic valve and
hypoplastic left heart have also been reported (143, 146). There have also been reports of an
association with ebstein�’s anomaly of the tricuspid valve (145, 147). The majority of these
reports have been in isolated (i.e. in an individual with no family history of CHD) cases of TOF,
although a few cases of NKX2.5 mutations segregating in families with TOF and ASD/VSD
have been reported (140, 145). The heterogeneity of phenotypes associated with NKX2.5
mutations indicates its fundamental role in diverse cardiac developmental pathways (145).
1.6.5.2 JAG1 Mutations
Mutations in signaling proteins have also been linked with TOF. JAG1 encodes a ligand for the
Notch transmembrane receptor and has been shown to be involved in cell fate determination

37
(148-150). This gene is mapped to the chromosome 20p12 locus (151) and is mutated in Alagille
syndrome (AGS), a multisystem disorder with liver, skeleton, eye and cardiac involvement (149,
152). Cardiac anomalies in AGS commonly include pulmonary stenosis and TOF including
variants with pulmonary atresia and absent pulmonary valve (80, 149, 153). Mutations in JAG1
have also been shown to occur in individuals with much more subtle AGS phenotypes (150).
JAG1 mutations have also been implicated in syndromic TOF presentations that do not have
typical AGS phenotypes (153) and in 3 (3.2%) of 94 patients with nonsyndromic TOF (154).
1.6.5.3 ZFPM2/FOG2 Mutations
ZFPM2/FOG2 is a zinc finger protein expressed in early heart development that regulates
expression of transcription factor GATA4 (155). This gene is mapped to chromosome 8q22
(155). Mutations in the gene encoding this protein in mouse models have been shown to cause
TOF and tricuspid atresia (155-157). In one report, 2 of 47 patients with sporadic nonsyndromic
TOF carried a ZFPM2/FOG2 mutation (155). One of these patients had classic TOF while the
other had the pulmonary atresia/MAPCAS type (155) . In another report, 1 of 178 (0.6%)
patients with TOF had a ZFPM2/FOG2 mutation (158).
1.6.5.4 GATA Mutations
The GATA family of transcription factors has also been linked to CHD. GATA4 mutations have
been identified in patients with TOF and atrial and ventricular septal defects (159-161). GATA4

38
is thought to be responsible for complex CHD including TOF in the setting of 8p23 deletion
syndrome, consisting of facial dysmorphisms, microcephaly, mental retardation and other
congenital anomalies (162). Duplication at this locus has also been identified in association with
a syndromic TOF presentation with incomplete penetrance (163). Overlapping in function with
GATA4, mutations in GATA6 have also been implicated in TOF as well as truncus arteriosus
and septal defects (164-166). In one report a parent carrier of a GATA6 mutation was found to
have a bicuspid aortic valve (165).

39
Table 1-4. Single gene mutations in tetralogy of Fallot, syndromic associations and associations with other congenital heart defects
Gene Reports in patients with TOF
Syndromic association Other CHD association References
NKX2.5 5/150 (4%) patients with TOF in one study, 2/230 (0.9%) in another series
No ASD, VSD, IAA, CoA (80, 140)
TBX1 4 syndromic patients with no 22q11.2 deletion from 3 studies, 3/93 (3%) nonsyndromic patients in one study
22q11.2 Deletion Syndrome
IAA, VSD, PS (80, 120, 122, 123)
JAG1 9 patients from a family with syndromic but non AGS phenotype, multiple with AGS, 3/94 (3%) patients with nonsyndromic TOF in one study
Alagille Syndrome PS, pulmonary atresia (80, 149, 150, 153, 154, 167)
ZFPM2/FOG2 2/47(4%) patients with nonsyndromic TOF in one study, 1/178 (0.6%) patients with TOF in one study
No Pulmonary atresia, DORV
(155, 158)
GATA4 1/201 (0.5%) with TOF in one report, 1/12 (8%) with TOF in one study
8p23 Deletion Syndrome ASD, VSD (159, 161)
GATA6 1 of 270 patients with various CHD 1/33 (3%) patients with TOF
No ASD, BAV, Truncus arteriosus
(164-166)
ASD-Atrial septal defect, VSD-Ventricular septal defect, IAA-Interrupted aortic arch, CoA-Coarctation of aorta, PS-Pulmonary stenosis, AGS-Alagille Syndrome, DORV-Double Outlet Right Ventricle

40
1.7 TOF Family Studies and Recurrence Risk Estimates
1.7.1 Family Studies: Purpose and Definitions
Studying familial patterns of disease is invaluable to the understanding of the inheritance
patterns that govern expression. Important information about natural history and variable
expression of a condition can be gleaned from studying its familial aggregation (70). Information
gained from family studies is also invaluable for genetic counselling purposes and forms an
important foundation for molecular testing. Knowledge of specific genetic aetiologies of a
disease also allows for phenotype correlation and risk assessment. Briefly, genetic counseling
involves empowering families with information about prognosis and treatment options of a
disease, genetic implications and recurrence risk and often dispelling notions of guilt
surrounding responsibility for a condition (168). As more information about specific genetic
aetiologies becomes available, re-visiting and updating family studies is important to determine
whether accepted recurrence risks and thus genetic counselling need be modified (169). For TOF
specifically, clinical and molecular evidence demonstrate the inhomogeneous nature of the
disease. Thus, although empiric risks are necessary for genetic counselling purposes, they may
misrepresent the true risk to individual families. Therefore studying phenotypic patterns of TOF
in families to identify at-risk pedigrees and as a prelude to identification of specific genetic
factors is useful to augment information given in empiric recurrence risks.
The conception of a family study usually begins with identifying the first member of a family
with the condition of interest (the proband or index case) and then investigating the presence or

41
absence of disease in other relatives (70). Families in which only the proband has the disease of
interest are often called simplex families. In these families, where no inherited component can be
identified, the disease in the proband is referred to as an isolated case. If the disease is
determined to be due to a de novo (new) mutation in the proband, it is referred to as a �“sporadic�”
case (70). Alternatively, there are multiplex families in which one or more relatives, in addition
to the proband, are affected. In multiplex families, the degree of concordance (same condition in
relative as proband) or discordance (relative having a different form of disease from that in
proband) of the disease in the relative with the disease in the proband is assessed. For congenital
cardiac defects, concordance traditionally refers to anatomical agreement with the defect in the
proband. For example in TOF, a relative who also has TOF has a fully concordant defect while
one with a cardiac defect that is a component of TOF e.g. VSD, is sometimes referred to as
�“partially concordant�”. A lesion such as coarctation of the aorta for example would be discordant
with TOF.
There are advantages and disadvantages to studying families ascertained with adult probands
over child probands (Table 1-5). Studying adult probands allows for more complete assessment
of clinical features, as many features may not be present or may not be easily recognizable in
children. In addition, adult probands naturally have more relatives available for study and allow
for more complete family history than studies with child probands. However, survival issues for
complex diseases, such as congenital cardiac defects, mean that adult studies may under-
represent severe phenotypes. An overview of the previous family studies of TOF, recurrence
risks and familial phenotypes is given below.

42
Table 1-5. Advantages and Disadvantages of Family Studies with Adult and Child
Probands
Adult Probands Child Probands
Advantages Disadvantages Advantages Disadvantages
More complete
recognition of
clinical features,
including late onset
features in probands
and relatives
Severe phenotypes
in probands and
relatives may be
under-represented
Severe phenotypes
more likely to be
ascertained
Later onset clinical
features (e.g.
syndromic features)
may be missed
More relatives
available for study,
including offspring,
nieces and nephews
Parents of probands
are more likely to be
available for study
Some relatives may
not be available e.g.
offspring
Genotype-
phenotype
correlation with
later onset sequalae
Relatives may be
more motivated to
participate when a
child is affected

43
1.7.2 TOF Family Studies
Relatively few systematic family studies of TOF can be found in the literature dating back to the
1960s with reported recurrence risks of 1-16% for CHD in first degree relatives (33, 54, 170-
175). A summary of these studies is shown in Table 1-6. One of the most frequently quoted
studies on which the multifactorial hypothesis for CHD was based is that by Nora et al. in 1966
(54, 176). These investigators examined at a cohort of 517 randomly selected paediatric
probands with various CHD and found unequivocal evidence a family history of CHD in 34%
cases, significantly greater than in a matched control group of 100 individuals with no CHD
(176). Probands with CHD and known genetic syndromes, such as Down�’s syndrome, were
excluded. CHD in relatives was initially ascertained by family history and an attempt was made
to perform physical examination of all affected relatives. An attempt was also made to examine
accompanying first degree relatives of child probands with CHD, regardless of their cardiac
status on initial history (176). Specifically for the 118 paediatric probands with TOF, 6 of 273
siblings had CHD, a recurrence risk of 2.2% and 1 of 236 parents had CHD for a rate of 0.4%
(54). The observed prevalence rates for siblings closely matched predicted recurrence based on
mathematical principles of multifactorial inheritance (54). The lower rate in parents was
proposed to be due to reduced survival into reproductive age among older individuals with
significant CHD (54). Recurrent CHD in all affected relatives was reported to be completely
concordant or a closely related lesion (partially concordant lesion) of TOF in the proband,
although related lesions were not delineated (176, 177). The investigators however
acknowledged that unavailable cardiac diagnoses in some relatives prevented them from

44
reporting on concordance in some cases (176). The same authors also reported a recurrence rate
of 4.2% among offspring of probands with TOF (177). From a meta-analysis of the available
data on parent to child transmission of various types of CHD, they proposed that offspring of
affected females with CHD were more likely to also have CHD than offspring of affected males
(178). This excess of maternally transmitted CHD was not statistically significant for TOF
however, although the investigators proposed that small numbers might explain the lack of this
trend in the TOF group (178).
Lamy et al. 1957 reported CHD in 4 of 404 siblings of 238 pediatric probands with TOF, a
recurrence rate of approximately 1% (33). They found no affected parents in this cohort. The
authors also reported that 15.13% of the probands had extra-cardiac defects including
�“mongolism�”, suggesting that probands with known genetic syndromes were likely included
(33). Cardiac defects in relatives of TOF probands were reported to be TOF in all but 2 cases, in
which the specific heart defect could not be determined (33).
Boon et al. 1972 also reported a family study of 100 child probands with TOF from two
institutions, mean age 7 and 13 years (171). Of the 100 included probands, 8 had another relative
with TOF and 16 had a relative with another CHD. For 189 siblings, recurrence rates of 1% (2
siblings affected) for TOF and 2.2% (4 siblings in total) for any CHD were reported. The authors
also reported recurrence rates of 0.17% (2/1165) and 0.16% (4/2541) for second and third degree
relatives respectively (171). Risks for specific relatives in these categories were not reported.
CHD in close relatives was generally concordant or partially concordant (e.g. VSD) with TOF.

45
Two distant relatives (5th degree) had completely discordant cardiac defects, namely coarctation
of the aorta and truncus arteriosus (171). An elevated prevalence (16%) of non-cardiac
malformations was noted in the probands that was not observed in their siblings. These included
cleft lip and/or cleft palate, urogenital and skeletal abnormalities most frequently. Two probands
were noted to have severe mental retardation (171).
Recurrence of CHD in offspring of probands with TOF was examined in the 1990 study by
Zellers et al. (172). Using a mailed questionnaire, they aimed to obtain information about family
history of CHD in relatives of 395 probands with TOF. A response rate of 58% (228 probands)
was reported and the mean age of the included sample was 38 ± 10 years (172). No description
of possible syndromic features within the cohort, or exclusion criteria based on known
syndromes was given. With respect to first degree relatives, they reported that of 253 offspring, 3
(~1.2%) had CHD, namely TOF, truncus arteriosus and VSD. Prevalence rates for CHD among
siblings and parents were similar to previous reports at 2.3% (13/567 siblings) and 0.43% (2/456
parents) respectively (172).
In contrast to the above studies, Whittemore et al 1982 reported a much higher rate of CHD
recurrence among offspring of probands with CHD (173). They prospectively studied 233
women with various CHD and reported a recurrence rate of 16.1% in their live born children.
Although the number of women with TOF was not reported specifically, they did report a high
rate among children of the small cohort (n=35) of women with cyanotic heart disease, 6 of 41
(~15%) live born infants (173). CHD in offspring was reported to be the same or similar to the

46
defect in the mother in the majority of cases. Importantly, the authors followed the affected
children for 3 years after birth and septal defects that subsequently closed were included in the
reporting (173). In addition, women with known genetic syndromes such as Noonan syndrome
were included in the study cohort (173).
The CHD family study of Burn et al. 1998 included 395 individuals with TOF, the largest TOF
cohort studied to date (175). Individuals with severe learning difficulties or any known genetic
syndromes were excluded but there was no clinical or molecular evaluation for 22q11DS. One
individual with known Cat-eye syndrome with a marker on chromosome 22 was included in
some analyses. With respect to first degree relatives, they found 7 (3.1%) of 223 offspring and
12 (2.2%) of 539 siblings with CHD among probands with TOF (175). There were no cases of
TOF among the 7 offspring with CHD but partial concordance was described. Four children had
VSDs, two were isolated lesions and one each also had RVOTO obstruction and patent ductus
arteriosus. Two offspring had discordant lesions, mitral stenosis in one child and coarctation of
the aorta in a child with Turner�’s syndrome (monosomy of the X chromosome in a female).
Although finding an excess of children with CHD born to mothers than to fathers for CHD
overall, this trend was not significant for probands with TOF (175).
Recurrence risks for second and third degree relatives in the Burn et al. study were reported to be
0.32% and 0.29% respectively but no specific categories of relatives or defects in these relatives
was given (175). Computer modeling of recurrence data for all CHD did not support a polygenic
model as would be found in multifactorial disease. Specifically for TOF, they proposed that the

47
best fitting model was one in which three genetic loci act by multiplication, i.e. the combined
effect of the three loci was greater than the sum of their individual effects (175).
The study by Digilio et al. 1997 investigated CHD recurrence in relatives of 97 children with
non-syndromic TOF (174). This was the only study to evaluate all participants for 22q11DS by
means of FISH testing for the 22q11.2 deletion. Any patients positive on FISH or otherwise
clearly syndromic were excluded. Of the 97 included probands, 10 (10.3%) had a total of 12
relatives with CHD (174). Three (3.1%) of 96 siblings of probands had CHD, concordant in all
cases with TOF. Four of the remaining nine relatives with CHD had discordant lesions, valvular
pulmonary stenosis in two relatives, and ASD in one and coarctation of the aorta in another
relative (174). The reported recurrence risks generally agreed with those predicted for
multifactorial inheritance. The authors therefore suggested that after exclusion of TOF cases with
22q11DS and known syndromes such as Trisomy 21, the remaining cases were probably
multifactorial in origin (174).
Most recently, the large Danish population study by Oyen et al. examined recurrence ratios of
CHD in relatives of probands with various classes of CHD (2). Strong familial clustering of
phenotypically similar lesions overall was described (2). No recurrence ratios specific to TOF
were delineated and it is unclear in which category these lesions were included since reports for
conotruncal as well as RVOTO lesions were given. As the study relied on Danish population and
health registry data, there was necessarily no clinical assessment of probands (2).

48
In summary therefore, many previous TOF family studies were conducted prior to the
widespread use of echocardiography and other CHD detection methods and before the
improvements in survival to reproductive age in TOF (33, 54, 171, 177). The most contemporary
family study of adults with TOF did not assess probands for 22q11DS, the most common known
genetic cause (175). The one study that did screen for 22q11.2 deletions used paediatric probands
(174), which precluded assessment of CHD in offspring, nieces and nephews and may have
limited clinical assessment of syndromic features (Table 1-5). Considering all these factors,
recurrence risks reported by these earlier studies may have limitations in accuracy and
completeness and may not reflect contemporary trends in survival and improved detection
methods for CHD. Updating recurrence risks for relatives of individuals with TOF would have
direct implications to genetic counselling and screening for these families but would also aid in
appreciation of inheritance patterns that govern this complex disorder.
Further, advancements in knowledge of cardiogenesis suggest that extrinsic cell populations
such as the secondary heart field or neural crest may contribute cardiomyocytes that eventually
become part of the right heart or left heart (14, 15, 141). Perturbations in these processes in
animal models lead to varying types of CHD (15). The few known putative mutations in TOF,
many expressed very early in cardiogenesis (before development of the right or left heart), have
diverse other cardiac phenotypes, including CHD anatomically unrelated to TOF (14, 179).
These findings suggest that a spectrum of CHD should be present in families of probands with
TOF but this phenotypic diversity has not been systematically studied in previous reports.
Defining the complete spectrum of CHD related to TOF in families is an important step towards

49
understanding the embryologic and genetic underpinnings of TOF and other CHD, and would
also advance knowledge of cardiogenesis in general.

50
Table 1-6. Tetralogy of Fallot family studies and recurrence risk estimates
Study Cohort
mean age
No. of
probands
Exclusions Recurrence Risks for Relatives Notes
Parents Siblings Offspring Second
degree
Third
degree
Lamy et
al. 1956
Paediatric 238 ? 0 1% - - - Known genetic
syndromes included
Nora at
el. 1968
Paediatric 118 Gross
chromosomal
aberrations
0.4% 2.2% - - -
Boon et
al. 1972
Paediatric 100 Down�’s
Syndrome
(n=2); Other
recognized
syndromes
(n=3)
- 2.2% - 0.17% 0.16% Extracardiac
anomalies in 16%
probands, including
severe MR
Nora et
al. 1976
Adult ? Known
syndromes
- - 4.2%

51
Study Cohort
mean age
No. of
probands
Exclusions Recurrence Risks for Relatives Notes
Parents Siblings Offspring Second
degree
Third
degree
Zellers et
al. 1990
38 ± 10
years
228 ? 0.43% 2.3% 1.2% - -
Digilio et
al 1997
6.5 years 97 Known
syndromes
including
22q11DS
0.5% 3% - 0.2% 0.6% Probands all
negative on FISH
for 22q11.2
deletions
Burn et
al 1998
Adult 395 Significant
learning
disability,
known
genetic
syndromes
- 2.2% 3.1% 0.32% 0.29% No evaluation for
22q11.2 deletions
RR- recurrence risk, MR- mental retardation (References 33, 54, 170-172, 174-176)

52
2 Study Rationale, Aims and Hypotheses
Success in medical and surgical management has created a large and increasing adult
cohort of patients with TOF, a rich but largely untapped resource for studying familial
patterns of heart disease in this common, complex condition. Despite the impressive
success in management of this condition, surprisingly little is known about genetic
aetiologies. Only in the minority of TOF cases have specific genetic causes been
determined and most are singleton cases with extracardiac or syndromic features.
Evidence for the genetic factors that may increase CHD susceptibility in families is
limited. Even in the face of a significant risk for CHD such as a 22q11.2 deletion, there is
considerable variable expressivity and reduced penetrance of cardiac lesions (30, 98,
105). One study has suggested that relatives of individuals with a 22q11.2 deletion may
still be at increased risk of CHD, even though they do not carry a 22q11.2 deletion
themselves (129). However, further evidence is needed to support the possibility that
additional inherited factors may be involved in expression of CHD in 22q11DS.
Previous family studies of TOF have largely focused on TOF and anatomically related
lesions (54, 170-172). However, molecular evidence from the few mutations identified
suggests that genetic factors that cause TOF may also cause a variety of other CHD,
including discordant lesions (132, 143, 179, 180), a potential indication of a
developmental relationship between different cardiac defects. Few data are available on
whether these diverse phenotypes are also seen in families. Determining the broader
phenotypic patterns of CHD in families is one way to explore such a relationship and

53
may have implications to current understanding of cardiogenesis and CHD classification.
In addition, delineation of familial phenotypes might help point to specific genetic factors
in TOF.
In the absence of specific mutations for the majority of patients, an updated family study
of TOF can have immediate practical implications. For example, standard genetic
counselling recommendations may need to be modified and would benefit from
contemporary data from an adult cohort given the increasing number of patients with
TOF of child-bearing age. Up to 15% of TOF cases are associated with a 22q11.2
deletion, which may be transmitted in an autosomal dominant fashion (30, 80). FISH
testing for this deletion became widely available in 1994 (81, 86). Thus, inclusion of
these and other cases of known genetic syndromes in a cohort may lead to misleading
recurrence figures. In addition, paediatric ascertainment may limit recurrence data for key
groups of relatives such as offspring, nieces and nephews and assessment of later onset
syndromic features. Auxiliary cardiac and extracardiac characteristics may provide
further clues to genetic predisposition (29, 32, 99).
In STUDY 1, we investigated the familial occurrence of CHD in relatives of adult
probands with TOF but no known genetic syndrome in order to obtain recurrence data for
first to third degree relatives and define cardiac phenotypes that occur with TOF in
families. We also investigated potential associations between familial CHD and auxiliary
cardiac and extracardiac features. We hypothesized that close relatives of probands with
TOF would have an elevated prevalence of CHD but that cardiac phenotypes would

54
include anatomically unrelated defects. We further hypothesized that probands with
nonsyndromic TOF would be more likely than probands with syndromic TOF to have
relatives with CHD.
In STUDY 2, a well characterized cohort of adults with 22q11DS was examined for the
occurrence of CHD in relatives without 22q11.2 deletions. We tested the hypothesis that
a positive family history of CHD would be more common in probands with CHD than in
those without CHD. We also predicted that CHD would segregate with the intact
chromosome 22 in families, consistent with the importance of variants in the 22q11.2
deletion region to CHD expression.

55
3 Study 1 Spectrum of Congenital Heart Disease in Family Members of Adults with
Tetralogy of Fallot

56
3.1 Objectives
TOF is a complex condition with considerable heterogeneity both in cardiac and
extracardiac features (3, 29). The understanding of genetic aetiology and inheritance
patterns in TOF is limited. Although up to 15% of cases are associated with a 22q11.2
deletion (30, 80, 86), in the majority of cases the genetic cause of TOF is unknown.
Previous family studies in TOF used paediatric cohorts (33, 171, 174), were executed
prior to the use of technologies such as FISH to detect 22q11.2 deletions (33, 54, 170-
173) and some prior to the era of improved detection and survival in CHD (33, 54, 170,
171). These factors may have limited completeness and accuracy of recurrence data from
previous studies, which has direct implications to clinical practice and genetic screening.
Although the clinical spectrum of TOF is broad, potential relationships between auxiliary
cardiac and extracardiac features in probands and a family history of CHD have not been
explored. Identifying clinical features in probands that may indicate a tendency towards
risk for CHD in relatives would improve on the use of empiric recurrence risks for
genetic counselling and help identify specific genetic factors in TOF.
Of the few known genetic factors associated with TOF to date, many also show
expression as other cardiac anomalies (80, 132, 140, 142, 165), suggesting a potential
embryologic relationship between different cardiac defects (14, 15, 145, 179). Evidence
of such a developmental relationship in families with TOF would have potential
implications to current understanding of cardiogenesis and conventional CHD
classification.

57
This study aimed to examine the recurrence risks for CHD in relatives of an adult cohort
of patients with TOF with no known genetic diagnosis and to investigate clinical factors
in probands that may be associated with familial CHD. We hypothesized that CHD in
relatives would show variable expressivity. We also hypothesized that probands with
nonsyndromic TOF would be more likely than probands with syndromic TOF to have a
family history of CHD.
3.2 Methods
The study population comprised adults (>17 years) with TOF followed at the Toronto
Congenital Cardiac Centre for Adults (TCCCA). The diagnosis of TOF was confirmed by
both diagnostic procedures such as echocardiogram and cardiac catheterization and
subsequent anatomy at the time of surgery. Auxiliary cardiac lesions were noted and
defined as congenital structural and vascular lesions other than TOF. Individuals with
known genetic syndromes other than 22q11DS, such as Down�’s syndrome, were
excluded a priori from this cohort. In total, 557 individuals with TOF consecutively
recruited from 1998 to 2010 were available for study after initial exclusions. Of these, 14
adopted individuals were excluded. Figure 3-1 shows the selection and genetic screening
(with FISH for 22q11.2 deletions and karyotype) of the study cohort. Written consent
was obtained from all research participants and the study was approved by the
institutional ethics boards of the University Health Network and the Centre for Addiction
and Mental Health.

58
All participants underwent a structured clinical assessment for features of a genetic
syndrome with an evaluation of dysmorphic facial features, abnormalities of voice and
cognitive ability (32, 98). Patients were defined as syndromic if they met two of three
criteria, previously validated to detect 22q11DS, including dysmorphic facial features,
hypernasal voice and learning difficulties (32). A history of extra cardiac birth defects
and learning difficulties was also obtained. Major birth defects included those requiring
surgery or affecting function of the patient (181), e.g. scoliosis requiring surgery,
horseshoe kidney and cleft palate. Clinical history was confirmed by retrospective chart
review. Standard karyotype analysis and fluorescence in situ hybridization (FISH) for
22q11.2 deletions using a TUPLE 1 (Vysis) or N25 (ONCOR) probe (81) were obtained
for 51 (78%) of 65 syndromic and 44 (10%) of 433 nonsyndromic patients, all confirmed
negative results (Figure 3-1). A further 45 of the 110 syndromic individuals who were
positive on FISH for deletion 22q11.2 were excluded from the study.

59
Figure 3-1. Selection and Genetic Screening1 of TOF Cohort
Included in Study 1
1 Genetic screening with FISH and standard karyotype

60
A total of 498 unrelated individuals with TOF comprised the final study cohort. All study
participants had a prospective interview for a family history of CHD in their relatives.
Pedigrees were constructed for each family using Progeny® software to reflect first to
third degree relatives as this information was available. The individual with TOF
followed at the TCCCA was designated as the proband and is identified with an arrow on
the pedigree (Figure 3-2). In the four cases where two members of the same family were
followed at our centre, only one (the first person seen at the centre) was designated the
proband. First degree relatives of the proband included parents, siblings and children.
Second degree relatives included grandparents, aunts and uncles and nieces and nephews.
Third degree relatives were predominantly first cousins and all relatives greater than third
degree were considered distant relations. A pedigree that included second degree relatives
was obtained for 369 (74%) probands and third degree relatives for 198 (40%) probands.
Families with only one known member with CHD (i.e. the proband with TOF) were
designated as �“simplex families�” and those with one or more family members with CHD
other than the proband were designated as �“multiplex families�”. In this study families in
which the proband with TOF had a first to third degree relative with CHD were
considered multiplex families.
Each relative with CHD was assigned one primary cardiac diagnosis by history, based on
the major cardiac lesion. For example, D-TGA with VSD would be noted as D-TGA.
Follow up interviews were conducted to verify cardiac diagnoses given at initial
screening. In addition, a clinical history of the presence of cyanosis, failure to thrive,
cardiac follow up or surgery and age of death of relatives with CHD was determined on
subsequent interview. A retrospective chart review for all probands reported having a
relative with CHD was conducted to examine for additional documentation of the

61
positive family history. For 23/43 (53%) first-degree relatives, echocardiographic, cardiac
catheterization, surgical or post mortem reports were obtained and reviewed to confirm
the cardiac diagnosis given on history. CHD in relatives was designated unspecified
when a specific cardiac diagnosis was unavailable, but a satisfactory history obtained that
was consistent with a congenital cardiac defect and/or that intracardiac surgery was
performed. Cases of neonatal death reported to be due to unspecified CHD were
included. To minimize the possibility of a falsely elevated recurrence of cardiac defects,
neither a history of heart murmurs nor late onset cardiac conditions were considered as
CHD.
Figure 3-2. Sample pedigree showing degree of relationship of relatives to proband
with TOF

62
3.2.1 Analyses
All statistical analyses were performed using SPSS Version 11.5 (Chicago, Illinois) and
SAS 9.13 (SAS Institute, Cary, North Carolina, USA). Recurrence risk for specific
relative categories was given by:
Number of relatives with CHD/All relatives x 100%.
Continuous data were expressed as mean ± standard deviation. Chi-square or two-tailed
Fisher exact tests were used to compare categorical variables. Student t tests were used to
compare continuous variables. A two-tailed p value less than 0.05 was considered
statistically significant.
In Table 3-3 the definition of a significant p value was corrected for multiple
comparisons using the Bonferroni method. Based on 13 comparisons we determined a
significant p value to be less than 0.004. Comparisons between the simplex and multiplex
groups based on the presence of auxiliary cardiac lesions, extracardiac abnormalities and
syndromic designation were made. Comparisons with general population prevalence of
any CHD (0.58%) and of severe CHD (0.061%) used figures derived from combined
numbers for adults and children in a large Canadian study (182). Statistical comparisons
and recurrence risk calculations were determined for first to third degree (first cousins)
relatives only.

63
3.3 Results
3.3.1 Demographic and Clinical Features in Probands with TOF
Of the 498 probands with TOF included in the study, 273 (54.8%) were male. The mean
age at assessment was 38.0 ± 13.6 years. Ethnicity of the cohort was Caucasian in 395
(79%) probands, Asian in 57 (11%), Black in 15 (3 %) and Other/Mixed in 31 (6%)
probands. One or more auxiliary cardiac lesions were present in 225 (45.2%) probands,
with 142 (28.5%) having structural lesions and 128 (25.7%) having vascular lesions. TOF
with pulmonary atresia was present in 65 (13.1%) probands (Table 3-1). The most
common other structural abnormalities in the cohort were ASD in 38 (7.6%), patent
foramen ovale in 28 (5.6%) and patent ductus arteriosus in 13 (2.6%) probands (Table 3-
1). Right aortic arch (21.6%, n=108) was the most common vascular lesion.
Sixty-five (13%) probands met criteria for syndromic designation (32). FISH testing for
22q11.2 deletions and standard karyotype analysis were performed in 51 (78%) of these
and were negative by definition in all cases. Among the 433 probands with nonsyndromic
TOF, FISH and karyotype testing were also available for 44 (10%) probands and did not
reveal any abnormality.
Overall, 68 (13.7%) probands had one or more major birth defects. Musculoskeletal
(n=36 probands, 7.2%) and urogenital (n=27 probands, 5.4%) anomalies were the most
frequently noted major defects (Table 3-2). Nine (13.8%) of 65 syndromic probands had
at least one major birth defect, not significantly greater than the prevalence of birth
defects in nonsyndromic probands (59/433 (13.6%), 2=0.002, p=0.96, 1df). Probands

64
with TOF/PA were not more likely to have a major birth defect than probands with TOF
(13/65 (20%) vs. 55/433 (12.7%), 2=2.553, p=0.11, 1df) and were not more likely to
have a syndromic designation (12/65 (18.5%) vs. 53/433 (12.2%), 2=1.928, p=0.16,
1df).
3.3.2 Family History of CHD
Of the 498 probands with TOF, 97 (19.5%) reported having a family history of CHD in at
least one other relative and 17 of these 97 (17.3%) had more than one affected relative.
Considering only those with a first to third degree affected relative (and not those with
only distant relatives), 78 (15.7%) probands of the total cohort reported a family history
of CHD. These 78 families were designated as multiplex families and the remaining 420
were designated as simplex families.
3.3.3 Demographic and Phenotypic Features in Probands from Multiplex and Simplex Families
Table 3-3 presents demographic and phenotypic factors in probands with TOF from
multiplex and simplex families. There were no differences in gender or Caucasian
ethnicity in probands with a family history (multiplex) compared with those with no such
history (simplex).

65
Multiplex probands were not more likely to have an auxiliary cardiac lesion or a
syndromic designation. If only subjects with auxiliary lesions other than pulmonary
atresia were considered, there was also no difference between the groups (simplex
165/420 (39.3%) vs. multiplex 24/78 (30.8%) 2=2.026, p =0.16, 1df). The presence of a
major extracardiac birth defect of any type did not differ between simplex and multiplex
probands (Table 3-3).
Considering only those 124 probands with a major birth defect and/or a syndromic
designation, there were 24 (19.4%) with a positive family history of CHD. This was not
significantly greater than the prevalence of a family history of CHD among the probands
with neither a major birth defect nor a syndromic designation (54/374, 14.4%, 2=1.704,
p =0.19, 1df).
3.3.4 Relatives with CHD
In total, 8384 relatives (first to third degree) were ascertained for this study, an average of
17 relatives per proband. There were 124 relatives with CHD of whom 43 were first
degree, 28 second-degree, 29 third degree and 24 were more distant relatives. The overall
prevalence of CHD in first to third degree relatives in this cohort was greater than the
expected population prevalence of CHD [100/8384 (1.19%) vs. 0.58%, p=0.000, OR
2.10, 95% CI 1.69-2.54].
Table 3-4 shows the frequency of specific heart defects in first to third degree relatives
with CHD. Severe or cyanotic CHD (including cases of neonatal death due to CHD) was

66
present in 25 first degree relatives, 11 second degree and 14 third degree relatives. The
prevalence of severe/cyanotic CHD relatives (50/8384, 0.60%) was also greater than the
population expectations (182) [0.061%, p=0.000, OR 9.76 95% CI 7.39-12.90].
Right ventricular outflow tract lesions as a group were most commonly reported in all
relative categories although the frequency of these lesions decreased as the relative
became more distant from the proband (49% first-degree, 29% second-degree and 17%
third-degree relatives). TOF was the most common lesion in this group for all relative
categories. Other RVOT lesions reported included truncus arteriosus and D-transposition
of the great arteries (Tables 3-4).
In first-degree relatives, left sided lesions (19%, n=8), including left ventricular outflow
tract lesions (LVOT) (n=7) and cleft mitral valve (n=1) were the next most commonly
reported group (Table 3-4, Figure 3-3). Bicuspid aortic valve ± coarctation of the aorta
(BAV CoA) was most common in the LVOT group and reported in 6 (14%) first-degree
relatives. There was one case of hypoplastic left heart in the brother of a proband whose
daughter also had a BAV/CoA (Family II, Figure 3-3) and two cases of cleft mitral valve
in one first and one second degree relative in two other families.
Intracardiac shunts comprising atrial and ventricular septal defects were the third most
common group of lesions reported in first-degree relatives (16%) and second most
common in second and third degree relatives (21% and 24% respectively). Cases in

67
which the level of shunting was unknown and simply described as a �“hole in the heart�”
were also included in this category.
Simple isolated cardiac anomalies such as dextrocardia (2%) and patent ductus arteriosus
(2%) were reported in two fathers of probands with TOF.

68
Figure 3-3. Simplified pedigrees of all seven multiplex families with the probands
with TOF and a first degree relative with a left heart cardiac defect
Table 3-5 shows the disease concordance rates for TOF among categories of relatives
with CHD. The overall TOF concordance among first to third degree relatives in this
study was 30% with the highest concordance among siblings (58%), followed by
offspring (35%). Other categories of relatives had lower concordance rates for TOF with

69
the lowest (14%) for parents of probands. Table 3-6 shows the cardiac anomalies found
in specific categories of first degree relatives.
3.3.5 Recurrence Risk for CHD
Table 3-7 shows the recurrence risks for CHD in first to third degree relatives of the adult
probands with TOF in our study. Recurrence risks in relatives of a paediatric cohort
(mean age 6.5 years) of TOF probands, all negative on FISH for 22q11.2 deletions, are
also shown (174). In the current study, the recurrence risk for CHD was highest for first-
degree relatives (2.04% overall), with the greatest risk to offspring of probands (5.84%).
The offspring risk was significantly greater than the risk to parents (0.70%, 2=32.501,
p=0.00, 1df) and siblings (2.34%, 2=8.345, p=0.004, 1df).
Overall, 163 (33%) probands with TOF had children. Eighty-two female probands with
TOF had 149 children of whom 12 (8.05%) had CHD. This prevalence was not
significantly greater than the prevalence of CHD among children of 81 male probands
(5/142 (3.5%), 2=2.716, p=0.10, 1df), even though the sample is small and there was
more than doubling of the risk with female probands. However, female probands were
more likely to have a female child with CHD (9/74, 12.2%) than a male child with CHD
(1/75 (1.3%), 2 =6.976, p=0.009, 1df). This analysis excluded two cases of pregnancy
termination for CHD in the foetus. Male probands with TOF were equally likely to have a

70
child with CHD of either gender [3/72 female children (4.2%) vs. 2/70 male children
(2.9%), 2 =0.179, p=1.000, 1df].
Among the 22 grandparents, aunts and uncles with CHD, 13 (59%) were paternal
relatives. There were also more paternal first cousins (17/25, 68%) than maternal first
cousins with CHD in this study. Nieces and nephews had the greatest prevalence of CHD
among second and third degree relatives.
3.4 Discussion
3.4.1 Recurrence Risk for CHD
This study aimed to investigate the family history of CHD in relatives of a large cohort of
adult probands with TOF. We found the risk for CHD was greatest to first degree
relatives, with the greatest prevalence among offspring of probands with TOF. The
recurrence risks for parents and siblings were similar to previous studies (54, 171, 175)
although the risk for offspring of 5.8% was slightly higher than in previous reports (1.2-
4.2%) (170, 172, 175). This was possibly due to improved detection of CHD, including
prenatally diagnosed cardiac disease. Indeed our numbers included two cases of
pregnancy termination for CHD diagnosed on foetal echocardiogram.
Contrary to studies reporting a greater risk to children of mothers than of fathers with
CHD (174, 175, 178), we found no increased tendency for maternal transmission of CHD
among offspring of probands with TOF. Our numbers for offspring were small but it is
possible that we had better ascertainment of CHD in children of male probands than the

71
previous studies. However, we did find a tendency for female probands with TOF to have
female children with CHD, although we were unable to include two cases of foetal
termination for CHD in this analysis. Although no definitive conclusions can be made,
the findings could potentially suggest an epigenetic effect in transmission of CHD.
Among second and third degree relatives, nieces and nephews had the greatest prevalence
of CHD followed by first cousins. Parents and grandparents had the lowest recurrence
risks of any relative category. The evolution of surgical management and the improved
survival of individuals with CHD in recent decades likely accounted for the greater
prevalence of CHD in younger relatives.
Our findings did not support a hypothesis of an increased prevalence of a positive family
history of CHD among probands with nonsyndromic TOF. Instead probands with
syndromic disease were equally likely to have relatives with CHD.
3.4.2 Variable Cardiac Phenotypes in Families
For first to third degree relatives overall in this cohort, there was a significantly greater
prevalence of severe or cyanotic CHD than would be expected from population
predictions (182). However, we found a spectrum of abnormalities in relatives both in
severity and phenotype, with TOF making up only a third of the CHD in relatives overall.
Consistent with previous reports of a �“horizontal transmission�” of TOF, we found the

72
highest concordance for TOF among siblings (54, 174). This could suggest that genetic
variants inherited from both parents were important in TOF expression.
Lesions other than TOF in relatives ranged from those that were partially concordant e.g.
VSD to those that were completely discordant. As a group, RVOT lesions were the
greatest in frequency among relatives and included truncus arteriosus and D-TGA. These
lesions might be expected to cluster in a family because they affect the same anatomical
site of the heart, though with a different ultimate phenotype. However, left heart lesions,
including LVOT defects and cleft mitral valve, were second highest in frequency among
first-degree relatives. The most common left heart lesion observed in relatives was BAV
with or without aortic coarctation, a finding that is counterintuitive to the accepted
embryological development of these anatomically unrelated lesions. However, BAV and
aortic stenosis occurred at very low frequency (0.2% and 0.6% respectively) in our
proband cohort with TOF (Table 3-1). A recent large review of over 2200 cases for
unusual cardiac associations in the setting of TOF also found 0.2% with BAV (8). A few
other case reports of the uncommon association of TOF ± pulmonary atresia with LVOT
lesions can be found in the literature (183, 184). There is also evidence of intrinsic
aortopathy in TOF patients, especially in the setting of 22q11DS (112, 185). As these
anatomically distinct lesions can infrequently occur in the patient with TOF, it is not
implausible that they may occur with TOF in families.
Among more distant relatives, there was only one case of a left heart lesion in a second
degree relative. This may due to under-ascertainment of simple lesions such as BAV in
these relatives. In addition, the higher proportion of unspecified CHD in these groups

73
meant that more severe left heart lesions such as hypoplastic left heart could also have
been included in this category.
This trend for left heart lesions to occur in families with TOF has not been systemically
studied in previous TOF family cohorts (54, 171, 172). More often, highlighting the
concordance or partial concordance of CHD in relatives with TOF in the proband was the
focus of these reports (54, 171). Cases of discordant CHD were often not specified
further. However, three cases of left sided cardiac lesions in relatives can be found in the
previous TOF family reports (174, 175). The study by Burn et al. reported coarctation of
the aorta and mitral stenosis in two children of offspring with TOF, although Turner�’s
syndrome was diagnosed in the former case (175). The Digilio et al. TOF study reported
on a cousin with coarctation of the aorta of a proband with TOF (174).
Familial CHD studies of LVOT lesions have not highlighted aggregation with TOF or
other right heart lesions in families. Instead, very strong familial clustering of these
anatomically related LVOT lesions has been reported (25, 186-190). Recurrence risks of
up to 13% for left heart obstructive lesions among first-degree relatives have been
reported (188). One study assessing by echocardiography asymptomatic CHD in relatives
of infants with left heart obstructive lesions found a markedly elevated prevalence of
aortic valve disease, predominantly BAV (186). In this study, only two group discordant
lesions were described, pulmonary valve stenosis and VSD (186).

74
Emerging molecular aetiologies in CHD offer a possible explanation for the variable
expressivity of CHD in families. Transcription factors, constitutively expressed in
cardiogenesis, are known to work cooperatively with other transcription factors and
regulatory proteins to promote normal cardiac development (14, 141). Since transcription
factors and signaling proteins are involved at multiple stages in cardiogenesis (14), it is
likely that the same gene affecting different embryological processes might result in
discordant cardiac phenotypes, depending on the status of other transcription factors and
environmental influences. Although known single gene mutations account for only up to
5% of TOF cases to date (80, 140), diverse cardiac phenotypes have been reported.
NKX2.5 mutations for example, which are expressed at the pluripotent cell stage in
cardiogenesis (14), most commonly cause septal defects but also cause TOF and other
right heart lesions (142-144). Though much less commonly reported, these mutations
have also been associated with left heart lesions such as bicuspid aortic valve, aortic
coarctation and hypoplastic left heart (143, 146). Intrafamilial variability in cardiac
phenotype is a feature of NKX2.5 mutations.
Studies of copy number variation in CHD have also reported variable cardiac phenotypes
(84, 131, 134, and 138). CNVs at chromosome 1q21.1 have so far been reported in
association with nonsyndromic TOF (84) but also with left heart obstructive lesions,
including BAV and coarctation of the aorta (131, 132). Although a study of CNVs in
familial CHD has not so far been reported, it is possible that these variants may underlie
some of the observed cases of CHD recurrence in the present study.

75
Reduced penetrance of CNVs and point mutations causing CHD is a fairly consistent
finding in cases that have been described (120, 123, 132, 140). Therefore, although the
cardiac defect in the proband may seem to arise sporadically, it may actually be a
function of variable expression of a mutation shared by other family members.
Studies in animal models and human subjects have shown that cardiac development is
extremely sensitive to changes in gene dosage (84, 117, 118, 123). Varying tbx1 dosage
in mouse models for example, produces a spectrum of cardiac abnormalities from simple
to complex defects (117, 118). Human CHD appears to be even more sensitive to
alterations in gene dosage, occurring at more modest reductions in transcriptional activity
than in mouse models (123). Modifier genes and variants impacting expression of the
gene of interest might therefore contribute to intrafamilial variation. JAG1 for example is
a ligand for transcription factor NOTCH1 (149). Potentially, a mutation in NOTCH1,
strongly associated with BAV (191) could affect JAG1 binding and expression, leading
to CHD. Although JAG1 mutations have usually been found in patients with syndromic
CHD, hypomorphic alleles, as have been found in TBX1 (123), could potentially be
associated with nonsyndromic disease. The recent study of CNVs in nonsyndromic TOF
identified CNVs that altered NOTCH1 and JAG1 gene dosage and provided evidence that
NOTCH1 mutations could cause TOF (84).
Although the anatomical classification of CHD is important from a treatment perspective,
it may not be as useful in explaining the pathogenesis of CHD (179). Instead, the
mechanistic approach suggests that a number of aetiologic factors may affect a similar

76
mechanism or developmental anomaly, producing a spectrum of anatomically separate
but mechanistically related defects (15, 24). The mechanistic classification of CHD as
described by Clark et al. for example, links TOF and other RVOT lesions by abnormal
cell migration in cardiogenesis, specifically from the neural crest (24). The relationship of
TOF with left heart obstructive lesions is not completely explained by this scheme.
However, category II lesions, due to abnormal embryonic haemodynamic flow, sees left
heart obstructive lesions such as hypoplastic left heart and BAV classified with
components of TOF such as pulmonary stenosis and perimembranous VSD (25). These
component lesions have been found in first-degree relatives of patients w/ left heart
obstructive lesions (186).
Alternatively, it has been proposed that BAV/CoA may actually fall in the spectrum of
diseases caused by abnormal neural crest migration, including TOF, since the neural crest
plays a significant role in formation of the aortic arch as well as the outflow tract (184,
192). Proper neural crest migration and function is also important for normal
development of craniofacial structures. One study of patients with coarctation of the aorta
showed that extracardiac abnormalities in neural crest derived head and neck structures
occurred more commonly in patients with BAV than in patients with coarctation but
normal aortic valves (192). Although the prevalence of extracardiac birth defects in
relatives was not examined in this study, two children of a male proband with TOF, one
with a cleft mitral valve, had cleft palates (Figure 3-3, Family I). These findings may
imply that genetic factors affecting neural crest cell function could play a role in
development of both cardiac and extracardiac congenital defects. The details of the two

77
approaches are different but both suggest that anatomically distinct cardiac and
extracardiac lesions may actually be linked by common embryological origins.
3.4.3 Study Advantages and Limitations
This study is the largest to date to examine family history in a cohort of adults with TOF,
all systematically assessed for features of genetic syndromes. Examining family history
in adults rather than children allowed us to report on CHD recurrence in offspring and
nieces and nephews, relatives unavailable for probands ascertained as children. In the
Digilio et al. family study with child probands for example, a family history of CHD was
reported in 10% participants (174). Using adults, we found that ~20% of probands
reported a family history of CHD. We had a slightly higher offspring recurrence risk than
previous reports, a possible reflection of improved CHD detection methods. The
tendency for female probands with TOF to have female offspring with CHD has not been
previously reported. We were able to report on recurrence risks for specific categories of
second and third degree relatives. Finally, this is the first study to fully characterize the
spectrum of CHD occurring in families of probands with TOF. The significant proportion
of left heart lesions in relatives is a novel finding which may be a helpful prelude to more
hypothesis driven molecular studies and help to advance the overall understanding of
cardiogenesis.
This study spanned many generations and therefore not all relatives with reported CHD
had echocardiograms or cardiac catheterization to confirm their cardiac disease. Family
history was the main ascertainment tool for CHD and relatives were not directly

78
examined. Previous studies assessing the reliability of family history for ascertainment
have shown that it is a very useful tool but with limitations (193-195). It tends to
underestimate the true prevalence of disease, with greater sensitivity for detection of
severe than milder phenotypes (193-195). We did however validate information gleaned
from family history by review of clinical records in more than 50% first-degree relatives
for whom this data was available, suggesting reasonable accuracy in our study. The
reliability of family history would decrease with increasing distance of relations from the
proband. Although we found a diversity of cardiac anomalies in relatives, we had a
significant number of unspecified CHD among second and third-degree relatives.
It is likely that the true prevalence of CHD in this cohort is underestimated. Survival
disadvantage of older relatives in our sample means that cases of early and suspicious
deaths which could not be included here may well have been due to CHD. In the 1960s,
the death rate from CHD was 40% with many deaths before school age (196). Indeed,
probands with a family history of CHD tended to be younger than those who did not
report such a history, a possible function of improved survival and better detection
methods. Foetal detection of CHD and subsequent termination of pregnancy are
contemporary issues. Recent estimates are that up to 58% of pregnancies are terminated
after identification of CHD and that termination might account for a significant reduction
(~21%) in the birth prevalence of CHD (28, 40). It is impossible to know with accuracy
the termination rate in our sample but two cases of pregnancy termination for CHD in the
foetus were reported. In addition, only a third of probands had children while data from
Statistics Canada show that in the general population, almost two-thirds of families have
children (197). The average age of women who had children in Canada in 2005 was 29.2

79
years (198). The lower rate in our sample could potentially be due to the relatively young
cohort, with 33% being less than 30 years old at the time of interview. Alternatively, it is
possible that some probands may have elected not to have children, for varying reasons
(45, 47, 51, 52).
3.4.4 Clinical Implications
In this study, using a detailed interview technique 20% of individuals with TOF were
found to have a family history of CHD. Clinicians need to be aware of the strong
potential for familial susceptibility to CHD and prioritize obtaining a detailed family
history in the clinical patient encounter (199). Using a simple enquiry about family
history of CHD may miss a significant portion of positive family history (200) and a
more in-depth interview about suspicious deaths and murmurs in relatives for example
may be required to identify at-risk pedigrees.
The suggestion that males may be as likely as females to have affected children with
CHD, means that pre-conception counseling, foetal echocardiograms and screening of
children is equally important in males as well as females with TOF. The possibility for
subclinical CHD in relatives, that can have serious clinical sequalae, for example aortic
dissection in BAV (201), must also be recognized.
Families of patients with TOF need to be educated about the potential for recurrence of
CHD not only for first degree relatives, but that the risk for second and third degree

80
relatives may not be negligible. While quoting an overall recurrence risk is important
from a genetic counseling perspective however, it is important to recognize that risks may
be greater in individual families. The selection of families for mutation screening and
more lesion specific genetic counselling can be guided by known familial CHD patterns.
3.5 Conclusion
Adults with TOF commonly have family members with CHD. The phenotypic spectrum
of TOF in families is broad and includes anatomically unrelated cardiac defects. This
study is an important prelude to genome-wide research in cases of familial CHD that
should shed light on variants that produce these phenotypes.

81
Table 3-1. Auxiliary cardiac lesions in 498 probands with tetralogy of Fallot
Auxiliary Cardiac Lesion No. of subjects % of Total
Structural abnormalities 142 28.5
Pulmonary atresia 65 13.1
Atrial septal defect 38 7.6
Patent foramen ovale 28 5.6
Patent ductus arteriosus 13 2.6
Dextrocardia 4 0.8
Aortic stenosis 3 0.6
Hemitruncus arteriosus 2 0.4
Atrioventricular septal defect with cleft mitral valve 1 0.2
Bicuspid aortic valve 1 0.2
Vascular abnormalities 128 25.7
Right aortic arch 108 21.7
Aorto-pulmonary collateral arteries 16 3.2
Aberrant subclavian artery 8 1.6
Coronary artery anomaly 8 1.6
Double aortic arch 1 0.2
Any auxiliary cardiac lesion 225 45.2

82
Table 3-2. Extracardiac birth defects in 498 probands with tetralogy of Fallot
Defect N=498 %
Musculoskeletal1 36 7.2
Urogenital2 27 5.4
Craniofacial3 12 2.4
Gastrointestinal4 11 2.2
Any defect 68 13.7
1 Includes scoliosis requiring surgery, club foot, vertebral abnormality, absent radius, absent digits, polydactyly, scapular abnormality 2 Includes duplicate ureter, ectopic kidney, absent kidney, horseshoe kidney, bicornuate uterus, hypospadias 3 Includes cleft palate, cleft lip, microtia, hemifacial microsomia, skull malformation 4 Includes anal atresia, oesophageal atresia, duplicate small bowel, tracheo-oesophageal fistula

83
Table 3-3. Demographic and phenotypic features in probands with TOF from
Simplex and Multiplex families
Factor Simplex
n = 420
Multiplex
n = 78
Statistic p*
Mean age 38.8 ± 13.6 34.5 ± 13.0 t = 2.48 0.01
Male gender 233 (56%) 40 (51%) 2 =�0.47 0.54
Caucasian 336 (80%) 59 (76%) 2 = 0.76 0.38
Auxiliary cardiac lesion 198 (47.1%) 27 (34.6%) 2 = 4.17 0.04
Pulmonary atresia 56 (13.3%) 9 (11.5%) 2 = 0.19 0.67
Structural lesion 124 (29.5%) 18 (23.1%) 2 = 1.34 0.25
Vascular lesion 112 (26.7%) 16 (20.5%) 2 = 1.31 0.25
Extracardiac birth defect 53 (12.6%) 15 (19.2%) 2 = 1.31 0.12
Musculoskeletal 28 (6.7%) 8 (10.3%) 2 = 1.26 0.26
Urogenital 20 (4.8%) 7 (9.0%) 2 = 2.28 0.13
Craniofacial 8 (1.9%) 4 (5.1%) 2 = 2.91 0.10
Gastrointestinal 10 (2.4%) 1 (1.3%) 2 = 0.37 1.00
Syndromic 55 (13.1%) 10 (12.8%) 2 = 0.004 0.94
* The definition of a significant p value was corrected for multiple comparisons using the
Bonferroni method (p <0.004).

84
Table 3-4. Cardiac anomalies in first to third degree relatives of probands with TOF
Cardiac Anomaly First degree
relatives n=43
(40 probands)
Second degree
relatives n=28
(25 probands)
Third degree
relatives n=29
(26 probands)
RVOT Lesions 49% 29% 17%
Tetralogy of Fallot 16 7 4
PA/VSD 2 - -
VSD + RVOTO 1 - -
Truncus arteriosus 1 - -
TGA 1 1 1
Left Heart Lesions 19% 7% -
BAV ± coarctation 6 1 -
Hypoplastic left heart 1 - -
Cleft mitral valve 1 1 -
Intracardiac shunts 16% 21% 24%
ASD 2 1 1
VSD 2 1 3
�“ Hole in heart�” 3 4 3
PDA 1 - -
Dextrocardia 1 - -
Neonatal Deaths with CHD 4 3 9
Unspecified CHD 1 9 8
RVOT- right ventricular outflow tract, PA/VSD- pulmonary atresia with ventricular septal defect,
RVOTO- right ventricular outflow tract obstruction, TGA- transposition of the great arteries,
BAV- bicuspid aortic valve, ASD- atrial septal defect, PDA- patent ductus arteriosus, CHD-
congenital heart disease

85
Table 3-5. Concordance rates for TOF in first to third degree relatives with CHD
Relative w/ CHD n No. with TOF Concordance for
TOF
First-degree 43 18 42%
Parent 7 1 14%
Offspring 17 6 35%
Sibling 19 11 58%
Second-degree 28 7 25%
Grandparent 8 2 25%
Aunt/Uncle 14 4 29%
Niece/Nephew 6 1 17%
Third-degree* 25 4 16%
All relatives 96 29 30%
* First cousins only

86
Table 3-6. Cardiac anomalies in first degree relatives of 40 probands with TOF
a with pulmonary atresia in one sibling and one child (foetal termination at 20 weeks)
b foetal termination at 20 weeks

87
Table 3-7. Recurrence risk for CHD in first to thirda degree relatives of probands with TOF in the current and comparison
studies
Current Study Digilio et al 1997 b
Average age of probands (yrs)
38 13.6 6.5
Relative Number of probands
Number with CHD/ Total number of relatives
Recurrence Risk
Number of probands
Number with CHD/Total number of relatives
Recurrence Risk
First degree 498 43/2100 2.04 % 97 4/290 1.38 %
Parents 498 7/996 0.70 % 97 1/194 0.52 %
Siblings 387 19/813 2.34 % 3/96 3.13 %
Offspring 163 17/291c 5.84 % - -
Of females 82 12/149 8.05 %
Of males 81 5/142 3.52 %
Second degree 369 28/4275 0.65 % 2/960 0.21 %
Grandparents 498d 8/1992 0.40 % 97 1/388 0.26 %
Half siblings 45 0/95 - - -
Aunts/Uncles 250 14/1815 0.77 % 1/572 0.17 %

88
Current Study Digilio et al 1997 b
Relative Number of probands
Number with CHD/Total number of relatives
Recurrence Risk
Number of probands
Number with CHD/Total number of relatives
Recurrence Risk
Nieces/Nephews 95 6/373 1.61 % - -
First cousins 198 25/2009 1.24 % 6/936 0.64 %
a Recurrence risk calculations for first cousins only for third degree relatives
b Digilio et al. 1997 paediatric family study of TOF (174)
c Two cases of foetal termination for CHD included
d Four grandparents per proband assumed

89
4 Study 2 Complex Congenital Heart Disease in Unaffected Relatives of Adults with
22q11.2 Deletion Syndrome
Contents of this chapter have been published in the American Journal of Cardiology:
Swaby et al. Complex Congenital Heart Disease in Family Members of Adults with
Tetralogy of Fallot. American Journal of Cardiology 2011;107:466�–471

90
4.1 Objectives
A deletion on chromosome 22q11.2 is the most common known genetic cause of TOF
(30, 85) but can be associated with virtually any other CHD (30). Multiple factors are
thought to affect the expression of CHD in 22q11DS. These include hemizygosity of the
45 genes in the 22q11.2 deletion region and interaction of the effects of hemizygosity
with genetic variants both in the intact chromosome 22 and elsewhere in the genome
(105, 115, 126). In families of probands with 22q11.2 deletions, an elevated prevalence
of CHD in relatives who do not have 22q11.2 deletions would support a hypothesis of
genetic interaction with the effects of the 22q11.2 deletion. Two previous paediatric
studies have suggested that the prevalence of isolated CHD without deletion 22q11.2 may
be elevated in relatives of patients with 22q11DS (129, 130). However these reports
involve in total just six first degree relatives with CHD and did not report on parental
origin of the 22q11.2 deletion in probands with affected relatives.
In this study, a well characterized group of adults with 22q11DS was examined for a
family history of CHD in their relatives without 22q11.2 deletions. We tested the
hypothesis that a positive family history of CHD would be more common in probands
with CHD than in those without CHD. We compared the observed prevalence of CHD in
this sample with that predicted for familial recurrence of nonsyndromic CHD (174) and
for the general population (182). We also predicted that CHD would segregate with the

91
intact chromosome 22 in families, consistent with the importance of variants in the
22q11.2 deletion region to CHD expression.
4.2 Methods
Patients followed at our clinic for adults (>17 years) with 22q11DS (n=131) were
available for study. Individuals with 22q11.2 deletions who were adopted (n=4), had
inadequate family history (n=12) or were family members of probands (n=11) were
excluded. Most subjects were ascertained because of the presence of CHD or a
psychiatric disorder (90). Informed consent was obtained in writing from probands and
their parents. The study was approved by the Research Ethics Boards of the University of
Toronto, Centre for Addiction and Mental Health and University Health Network.
We evaluated 104 probands with the 22q11.2 deletion, all of whom met clinical criteria
for 22q11DS (102) and had lifetime clinical data available, including cardiac assessments
(98). All probands with 22q11DS had echocardiograms and/or cardiac catheterisation to
evaluate their cardiac status. CHD was classified by structural complexity as previously
described (113, 202). Among probands with 22q11DS in this series, major CHD included
TOF, pulmonary atresia or absent pulmonary valve. Simple CHD included ventricular
septal defects (VSDs) or atrial septal defects (ASDs) (113, 202). Ethnicity of the sample
was 90% caucasian (n=94), 4% asian (n=4), 2% black (n=2) and 4% other (n=4).

92
A comprehensive family history was obtained in multiple interviews from all families
and pedigrees constructed to include first to third degree relatives. A history of CHD in
the relatives was confirmed by medical records review where possible. To avoid a falsely
elevated recurrence rate of CHD, a history of heart murmurs or cardiac conditions that
were detected later in life were not considered as CHD. All available parents of probands
underwent assessment for clinical features suggestive of 22q11DS (90). Relatives with
CHD who were confirmed (n=8; 6 children, 1 mother and 1 sibling) to have
microdeletion 22q11.2 or suspected (n=6; 5 siblings and 1 uncle) to have microdeletion
22q11.2, based on a history given of syndromal features or when 22q11.2 deletion status
of one or both parents was unavailable, were excluded. Genetic testing for syndromes
other than 22q11DS and karyotypic anomalies was not performed.
The 22q11.2 microdeletion was confirmed in all probands by standard fluorescence in
situ hybridisation (FISH) techniques using a TUPLE 1 (Vysis) or N25 (ONCOR) probe
(81). Once the 22q11.2 deletion was confirmed in the proband, testing was offered to all
available parents. For a study of copy number variation in 22q11DS, DNA samples from
99 subjects (probands) with 22q11DS and 122 unaffected parents were genotyped for
approximately 250,000 SNPs with the Affymetrix Gene CHIP® Human mapping 250K
Nspl Array as previously described (90). These data were used to determine the mode of
22q11.2 deletion and parental origin of de novo deletions as well as copy number variant
(CNV) content. The mode of the 22q11.2 deletion within the cohort was confirmed to be

93
de novo in 70 probands and transmitted in five probands. In cases where parental DNA
was unavailable for genotypic study we assigned a �“probable de novo�” (n=14) or
�“probable transmitted�” (n=2) deletion status based on clinical features (90). There were
13 probands for whom the origin of the 22q11.2 deletion could not be determined (90).
Among the probands with confirmed or probable de novo 22q11.2 deletions, parental
origin of the 22q11.2 deletion was determined for 74 probands, of whom 42 were of
maternal origin. In the confirmed or probable transmitted group (n=7), parental origin
was maternal in 4 cases (90).
All statistical analyses were performed using SPSS Version 11.5 (Chicago, Illinois) and
SAS 9.13 (SAS Institute, Cary, North Carolina, USA). Chi square or two-tailed Fisher
exact tests were used to compare categorical variables. Comparisons with general
population prevalence of any CHD (0.58%) or severe CHD (0.061%) used figures
derived from combined numbers for adults and children in a large Canadian study (182).
4.3 Results
Of the 104 probands with 22q11DS in the study (48 males, 56 females, mean age 33.3 ±
10.3 years), 66 (63.5%) had CHD (n=23 simple CHD, n=43 major CHD). The presence
of CHD in the proband was not significantly associated with parental origin of the
22q11.2 deletion for either the de novo (maternal n=29/42 (69%) vs. paternal n=17/32

94
(53%), p=0.16) or transmitted (maternal n=2/4 (50%) vs. paternal n=3/3 (100%), p=0.43)
groups. In addition, probands with CHD did not exhibit de novo CNVs or any excess of
novel inherited CNVs outside the 22q11.2 region (data not shown) (90).
4.3.1 Family History of CHD
A total of 2639 relatives were included in this study, on average 25 relatives per proband.
Fourteen probands (13.5%), 9 with confirmed and 5 with probable de novo 22q11.2
deletions, had a positive family history of CHD of various types in a total of 17 (0.64%)
relatives (see Table 4-1). Of these, three were first degree, 11 second degree and three
were third degree relatives.
The overall prevalence of CHD in relatives of 22q11DS probands (0.64%) was similar to
that of the general population for any CHD (0.58%, p=0.8) (182). However, probands
with 22q11DS who themselves had CHD were more likely to have relatives with any
CHD than probands with no CHD [15/1663 (0.9%) vs. 2/976 (0.2%), p=0.041, OR 4.43,
95% CI= 1.03-40.00]. In addition, six (40%) of the 15 relatives of 22q11DS probands
with CHD had severe and/or cyanotic CHD, significantly greater than the general
population prevalence (182) [(6/1663) 0.36% vs. 0.061%, p=0.007, OR 5.88, 95% CI
2.16-12.85]. Eight of 11 (73%) second and third degree relatives with CHD were
maternal relatives (Table 4-1). Contrary to our prediction, there was no apparent

95
relationship between the familial side (maternal or paternal) of the affected relative and
that of the intact chromosome 22 (Table 4-1).
Table 4-2 shows the recurrence risk for CHD in first to third degree relatives of 104
22q11DS probands in our cohort and comparable data from another study of 108
probands with 22q11DS that reported nonsyndromic CHD in first degree relatives (129).
Recurrence risks for first degree relatives using the combined data for 22q11DS (n=212
probands) and for relatives of a paediatric sample of 97 nonsyndromic TOF patients with
no 22q11.2 deletions (174) are also shown for comparison purposes (Table 4-2). Our data
suggest a greater prevalence of CHD in aunts and uncles of 66 probands with 22q11DS
and CHD than in comparable relatives of probands with nonsyndromic forms of TOF
(8/439 (1.82%) vs. 1/572 (0.17%), p=0.013, OR 10.60, 95% CI 1.41-471.01). Comparing
only probands with TOF, there was still a greater prevalence of CHD among aunts and
uncles of the 43 probands in our sample than in comparable relatives of the
nonsyndromic TOF sample (6/258 (2.33%) vs. 1/572 (0.17%) p=0.004, OR 13.60, 95%
CI 1.63-626.30).
4.4 Discussion
This study investigated the presence of CHD in families of adult probands with 22q11DS.
We found that in relatives of individuals with 22q11DS, who did not themselves have

96
microdeletion 22q11.2, there appeared to be an increased risk of CHD if the proband with
22q11DS also had CHD. Like CHD in 22q11DS (30, 85, 129) and consistent with a
previous family study (129), recurrent CHD in relatives tended to involve severe or
complex defects. The prevalence of these major CHD lesions in relatives was
significantly elevated over population estimates for severe CHD (182). Collectively,
these results support a heritable susceptibility to CHD in these families, in addition to the
susceptibility imparted by the microdeletion 22q11.2.
The specific origins of this increased susceptibility remain unclear but the results suggest
they may be related to the factors that contribute to the expression of CHD in the proband
with the 22q11.2 deletion. Genes on the intact chromosome 22q11.2 such as TBX1, have
been shown to play a role in expression of CHD in animal models and humans (115, 117,
118, 120). Cardiac development appears to be profoundly sensitive to gene dosage.
Indeed, variation of Tbx1 gene dosage in mice produced the entire spectrum of cardiac
abnormalities seen in humans with 22q11DS. Although TBX1 mutations have previously
been found in humans with syndromic CHD but no 22q11.2 deletion (120), variants that
reduced but did not completely ablate TBX1 gene function were recently shown to be
associated with nonsyndromic CHD (123). The existence of these hypomorphic alleles
could potentially explain the presence of CHD without 22q11.2 deletions in family
members of probands with 22q11DS.

97
Our findings however suggest that factors outside of the 22q11.2 region may also be
involved in risk for CHD. Four of the relatives with CHD were not from the known side
(paternal or maternal) of the intact chromosome 22 in the probands and the other four had
at most a 50% chance of sharing the same chromosome 22 (Table 4-1). Using the results
from our previous study of genome-wide CNVs in this cohort of patients with 22q11DS
(90), in which CNVs of about 30 kb could be detected, we did not identify any novel
CNVs in the probands that could explain the observed familial CHD susceptibility.
However, the possibility exists that newer technologies with improved resolution could
identify such CNVs. Results from adequately powered genome-wide studies of 22q11DS
may shed light on specific structural and/or sequence-based genetic variants that increase
the likelihood of CHD in the presence of a 22q11.2 deletion.
The higher prevalence of CHD in second than in first degree relatives in our CHD
subgroup is an interesting finding. When compared to recurrence figures for
nonsyndromic TOF, which is thought to have a multifactorial aetiology (54), the level of
elevated risk for CHD in our cohort was considerably higher than has previously been
reported for second degree relatives (174, 175). This may in part be explained by the
ability to ascertain additional relatives (nieces and nephews), conferred by examining an
adult sample. However, results for comparable numbers of aunts and uncles showed
significantly higher risk for the 22q11DS group. Consistent with literature implicating a
somewhat greater role for maternal than paternal inheritance of susceptibility to CHD
(174, 175, 178), we found that the majority of affected second and third degree relatives

98
in our series were maternal. These findings may be related to better knowledge of
maternal than paternal relatives but could also suggest a potential role for genes on the X
chromosome. While finding no parents with CHD could be explained by a survival
disadvantage of older parents in our sample, the relatively low recurrence in siblings of
individuals with 22q11DS is more difficult to account for. It is possible that exclusion of
five siblings with CHD but with unknown 22q11.2 deletion status was overly
conservative. Alternatively, this pattern of results may suggest that additive genetic
effects are more likely than dominant mendelian inheritance with reduced penetrance in
expression of CHD in these families. Also, there were relatively low numbers of siblings
in the comparison studies (129, 174).
Results combining our sample with that of Digilio et al. (175) indicate that overall the
risk of familial recurrence of CHD among unaffected relatives of individuals with
22q11DS appears similar to recurrence amongst relatives of subjects with TOF but
without a 22q11.2 deletion (174) (Table 4-2). This finding has important implications for
genetic counselling of individuals with 22q11DS. Beyond the 50% risk of transmitting
the 22q11.2 deletion and the elevated risk of CHD associated with the deletion, relatives
who do not have deletion 22q11.2 may still be at increased risk for CHD over general
population expectations, especially for severe disease. The tendency towards more
complex CHD lesions which invariably require surgery likely creates economic and
social burdens on these families. The potential for elevated risk for complex cardiac
disease in relatives without deletion 22q11.2 warrants further investigation.

99
4.4.1 Study Advantages and Limitations
This study is the first to investigate nonsyndromic CHD in second and third degree
relatives of 22q11DS probands and the first to report a significant finding of elevated
recurrence risk of severe CHD. Data available on parental origin of the 22q11.2 deletion
(90) allowed us to consider whether the intact chromosome 22q11.2 appeared to be a
factor with respect to CHD in relatives. Our sample size was sufficient to show
significant results for severe CHD when compared to a large population study (182).
Consistency with results of other studies supports the overall findings.
Information on family history of CHD was obtained in multiple personal interviews with
the families and substantiated where possible by review of clinical data. Nonetheless, we
were unable to determine a definitive CHD diagnosis in every reported case of
recurrence. Subclinical CHD is unlikely to be detected by family history. Ideally,
neonatal echocardiogram data would have been available for all relatives. Recall bias in
family history is more likely to result in under-reporting than over-reporting.
Collectively, these factors suggest the true prevalence of CHD in relatives is likely higher
than we have reported. Effects of these limitations would be minimized however for
severe CHD. On the other hand, for children of probands with 22q11DS, small numbers
and possible effects of assortative mating between the proband and co-parent may have
magnified the recurrence risk for CHD. Cohort effects must also be considered. The
contemporary general population prevalence study used for comparison (182) included

100
only living individuals and would reflect improved survival over previous generations.
Our study reported on living and deceased relatives. Arguably, four of the five deceased
relatives with severe CHD in our study (three children and one adult born in the 1940s to
1950s) may have survived if born in more recent decades. Also, genetic testing for
22q11.2 deletion was not available for all relatives with CHD and the presence or
absence of syndromal features indicative of 22q11DS was determined by history. This
could have contributed to a lower recurrence risk because we excluded affected relatives
with CHD who had syndromal features but unknown deletion status. A difference from
other family studies that warrants consideration is that probands with CHD and 22q11DS
represent a sample with enhanced genetic homogeneity. Samples of other probands with
CHD are aetiologically heterogeneous with discoveries of major causal factors emerging
(14, 84, 141).
4.5 Conclusion
We found that relatives of individuals with 22q11.2 deletions, who do not themselves
have deletion 22q11.2, may still be at increased risk for major CHD. There is the
potential for this risk to be further elevated if the proband with 22q11DS also has CHD,
suggesting that factors involved in the expression of CHD in the proband with 22q11DS
may be involved in familial CHD susceptibility. The aetiology of this increased
susceptibility is undoubtedly complex but is likely genetic and not necessarily confined to
genes in the 22q11.2 region. These findings have potential implications for genetic

101
counselling of individuals with 22q11DS and their families. The results predict that
forthcoming genome-wide association studies of 22q11DS may shed light on specific
genetic variants that interact to promote expression of CHD in the presence of a
hemizygous 22q11.2 deletion and thus on genes important in cardiac development.

102
Table 4-1. Details of CHD in relatives of 14 adult probands with confirmed or probable de novo 22q11.2 deletions
Proband Relative(s) Case 22q11.2 deletion CHD in
proband Relative Degree
of relation
CHD in relative
Severe Syndromal features
Absence of 22q11.2 deletiona
Relative on the same side of the family as that of the intact chromosome 22 in the proband
Length (Mb)
Confirmed or probable de novo
Parental origin
1 3 Probable Unknown - Child 1st CHD unspecified - Dev. delay Confirmed - 2 3 Confirmed Maternal - Sibling 1st PDA - 0 Presumed - 3 3 Confirmed Unknown TA Sibling 1st VSD - 0 Confirmed - 4 3 Probable Unknown VSD Nephew 2nd CHD unspecified - 0 Confirmed - 5 3 Probable Unknown TOF Niece 2nd VSD not
requiring surgery - 0 Presumed -
6 3 Confirmed Paternal TOF Nephew 2nd D-TGA + 0 Confirmed - 6 Maternal
aunt 2nd CHD unspecified
�“blue baby�”, died at age 1 year
+ 0 Presumed +b
7 3 Confirmed Maternal PA/VSD Maternal aunt
2nd PDA, repaired at age 8 years
- 0 Presumed 0
8 3 Confirmed Maternal TOF Maternal aunt
2nd TOF, died at age 18 months without repair
+ 0 Presumed 0
9 1.5 Confirmed Maternal TOF Maternal aunt
2nd �“Hole in heart�”, detected in pregnancy
- 0 Presumed 0
10 3 Confirmed Paternal VSD, ASD
Maternal uncle
2nd 2 �“holes in heart�”, repaired at age 12 years
- 0 Presumed +b
11 3 Confirmed Maternal TOF Paternal uncle
2nd �“Hole in heart�” not requiring surgery
- 0 Presumed +b
12 3 Probable Unknown TOF Maternal aunt
2nd CHD unspecified, blue baby, died in infancy
+ 0 Presumed -

103
Proband Relative(s) Case 22q11.2 deletion CHD in
proband Relative Degree
of relation
CHD in relative Severe Syndromal features
Absence of 22q11.2 deletion
Relative on the same side of the family as that of the intact chromosome 22
Length (Mb)
Confirmed or probable de novo
Parental origin
12
Maternal
uncle
2nd
CHD unspecified cyanotic, died at
38 years
+
0
Presumed
-
13 3 Confirmed Paternal VSD Paternal first cousin
3rd CHD unspecified, died at 9 years
+ 0 Presumed 0
13
Maternal first cousin
3rd �“Hole in heart�” - 0 Presumed +b
14 Unknown Probable Unknown TOF Paternal first cousin
3rd �“Hole in heart�”, surgically repaired in early childhood
- 0 Presumed -
TA = Truncus arteriosus, VSD = Ventricular septal defect, TOF = Tetralogy of Fallot, PA = Pulmonary atresia, ASD = Atrial septal defect
a Confirmed = Direct testing using standard FISH and 22q11.2 probe; Presumed = Both parents of proband negative for 22q11.2 deletion
b Even where the affected relative was on the same side as the origin of the intact chromosome 22 in the proband, there would be at most a 50% chance (in
the case of an aunt/uncle) of sharing that intact chromosome 22.

104
Table 4-2. Recurrence risk figures for CHD in relatives of adult probands with 22q11DS
22q11DS Family Studies Non-22q11DS TOF
Family Study
Current study Digilio et al. 2005a Combined samples Digilio et al. 1997 b
Number of probands 104 (Total cohort) 66 (Subgroup with CHD) 108 212 97
Average age (years) 33 ± 10 32 ± 10 NA NA 6.5
Relationship of
relatives
No. with
CHD/ Total
no. relatives
Risk
(%)
No. with
CHD/ Total
no. of relatives
Risk
(%)
No. with
CHD/ Total
no. relatives
Risk
(%)
No. with CHD/
Total no. of
relatives
Risk
(%)
No. with CHD/
Total no. of
relatives
Risk
(%)
First degree 3/405 0.74 1/257 0.39 5/253 1.98 8/658d 1.22d 4/290 1.38
Parents 0/201 - 0/127 - 1/198c 0.51 1/399 0.25 1/194 0.52
Siblings 2/192 1.04 1/122 0.82 3/54 5.56 5/246 2.03 3/96 3.13
Children 1/12 8.33 0/8 - 1/1d - 2/13d 15.38d - -
Second degree 11/1276 0.86 11/806 1.36 NA NA - 2/960 0.21
Grandparents 0/416 - 0/264 - - - - 1/388 0.26
Aunts/uncles 8/666 1.20 8/439 1.82 - - - 1/572 0.17

105
aDigilio et al. 2005 study of nonsyndromic CHD in 253 first degree relatives of 108 probands with deletion 22q11.2 (88 probands (81.5%) with CHD) (129)
bDigilio et al. 1997 study of recurrence of CHD in relatives of 97 nonsyndromic TOF probands without 22q11.2 deletion (174) c18 parents with deletion 22q11.2 were excluded (174)
dIn the Digilio et al. 2005 sample only one of the 253 first degree relatives studied was a child of a proband (personal communication) NA= Not available
Nieces/nephews 3/145 2.07 3/85 3.53 - - - - -
Half siblings 0/49 - 0/18 - - - - -
First cousins 3/958 0.31 3/600 0.50 NA NA - 6/936 0.64

106
5 Summary of Thesis and Future Directions
In complex developmental disorders multiple genetic mechanisms are believed to play a role in
susceptibility to disease (70). These include gene-gene interactions, gene-environment
interactions and epigenetic effects (70, 77, 203). However compared to other developmental
disorders such as autism for example, relatively little is known about the genetics and inheritance
of TOF. This thesis work has helped to advance our understanding of the complex genetics of
TOF by examining inheritance patterns in families of individuals with TOF and/or with
22q11DS. In STUDY 1, familial inheritance in TOF was examined in a large cohort of adults
with no known genetic diagnosis in order to define the phenotypic expression of TOF within
families. In STUDY 2, familial inheritance was examined in a more genetically homogenous
cohort, a population of patients with 22q11DS, to determine if there was clinical evidence for
additional inherited risk factors for CHD.
In STUDY 1, by examining family history, we have defined a broad spectrum of CHD that
occurs in close relatives of individuals with TOF. Cardiac defects in families included simple and
complex abnormalities, other RVOT lesions and left heart obstructive lesions. This phenotypic
diversity in families is an indication of the genetic heterogeneity of TOF and suggests that
complex genetic mechanisms contribute to its development. The results are also consistent with
the variable expressivity seen in the few described putative genetic factors in TOF.

107
The aggregation of TOF with anatomically unrelated left heart defects was a novel finding and
further suggests that genetic factors active early in development may be responsible for different
cardiac defects. Advancements in understanding of cardiogenesis reveal that early extrinsic cell
populations such as those found in the secondary heart field for example, may contribute
cardiomyocytes to both the left and right heart (13-15). While conventional understanding of
CHD emphasizes pathways of regional cardiac development (179), for example septation or
development of the outflow tract, much earlier perturbations of these embryological processes
might explain the variety of phenotypes seen in families. Although an appreciation of anatomical
differences between cardiac defects is important for understanding cardiac physiology and
management, our findings suggest that anatomically distinct cardiac lesions might have an
embryologic relationship. The potential existence of common genetic variables present early in
development may be helpful for future gene targeting technologies to treat and prevent
congenital cardiac disease.
In STUDY 2, we selected a genetically more homogeneous cohort to investigate further the
possible genetic mechanisms that underlie TOF. Even with a large deletion on chromosome
22q11.2, only about 40% patients with 22q11DS have CHD (98, 106). Variable expression and
reduced penetrance occur (90, 98, 105), suggesting that other factors, genetic or environmental,
may increase CHD susceptibility. Similar to STUDY 1, cardiac lesions in probands and relatives
varied in phenotype and severity. We found that relatives of probands with 22q11DS and CHD
were more likely to have cardiac defects than relatives of probands with normal hearts. This
finding provided clinical evidence of potential genetic modifiers in families of individuals with
22q11DS that could increase CHD risk. We found no clinical evidence of segregation of CHD

108
with the intact chromosome 22q11.2 in families, suggesting that potential genetic modifiers may
be present elsewhere in the genome. The potential for genetic modification of CHD expression in
22q11DS offers a possible explanation for the variable expressivity seen in families of the more
heterogeneous cohort with TOF.
Although only a trend in our study, the prevalence of CHD in offspring of mothers with TOF
was greater than that among fathers with TOF. Perhaps greater numbers would have led to a
more definitive observation of significance. Alternatively, it is possible that under-ascertainment
of CHD among children of males due to less frequent screening of partners during pregnancy and
of children was responsible for the apparent trend towards maternal transmission of CHD.
Mothers with TOF were more likely to have female children with CHD than affected male
children. In 22q11DS, an excess of deletions of maternal origin have been reported (90, 94) and
in the family study of 22q11DS, greater numbers of maternal than paternal relatives with CHD
were found. Although not definitively proven, our findings could imply a potential role for
epigenetic mechanisms in TOF.
The 22q11DS model also offers a possible explanation for the trend towards a greater prevalence
of craniofacial abnormalities in probands with TOF from multiplex families than in those from
simplex families. Perturbed neural crest function is believed to explain the occurrence of cardiac
and extracardiac congenital abnormalities in 22q11DS (16, 96, 97). TBX1, a gene thought to
have an important role in cardiac and some noncardiac phenotypes of 22q11DS, is a
transcriptional regulator of the secondary heart field and also is believed to have a role in neural

109
crest function (13, 22). Although TBX1 mutations have not been reported in patients with
22q11DS, they have been found in patients with syndromic features including CHD, but no
22q11.2 deletion (120-122). In addition, hypomorphic variants of TBX1 have been found in
patients with nonsyndromic TOF (123). The potential for co-segregation of cardiac and
extracardiac disease in families is an acknowledgement of the multisystem nature of TOF and
further suggesrs that genetic factors involved in TOF are active early enough in development to
affect multiple processes. The segregation of TOF with certain noncardiac phenotypes could
potentially point to specific genetic aetiologies and deserves further study.
Our findings have direct implications to current clinical practice. The previous studies promoting
the notion of greater risk of maternal than paternal transmission of CHD (54, 174, 175, 178) may
have influenced the practice of greater referral of females with TOF than males for pre-
pregnancy and genetic counseling and routine pregnancy screening (i.e. foetal echocardiogram
and pediatric referrals). Our results suggest that males with TOF and their partners should also be
offered pre-conception counseling and screening of their children. Clinicians should also be
attentive to the potential existence of subclinical CHD such as BAV in close relatives of persons
with TOF and should enquire about their cardiac status. Although direct examination of all close
relatives may not always be feasible, a history of cardiac symptoms in these relatives should
prompt further investigation. An awareness of the potential for elevated CHD susceptibility in
unaffected relatives of persons with 22q11DS should also prompt a high index of clinical
suspicion for cardiac disease in these relatives. Individuals with 22q11DS should also be made
aware of the possible increased risk of CHD in offspring, apart from susceptibility imparted from
transmitting the 22q11.2 deletion.

110
5.1 Future Directions
The determination of inheritance patterns in TOF and factors that increase familial susceptibility
would benefit from further expansion of the current cohort, possibly in a multicentre design, to
prospectively follow family history of CHD. Screening of family members by echocardiography
and electrocardiograms to detect structural as well as functional cardiac disease would also be
helpful to further define familial cardiac phenotypes and refine recurrence risks. As the clinical
spectrum of TOF includes extracardiac features, studies to examine the familial occurrence of
extracardiac congenital and late onset abnormalities such as psychiatric disease would be useful
in both the TOF and 22q11DS groups. These studies could further add to understanding of the
developmental links between the heart and other organs such as the brain and the genetic factors
unifying organ development.
Further studies employing candidate gene (123, 140, 204), linkage (205), CNVs (84, 90) or
genome wide association approaches (206) should follow clinical studies to detect specific
genetic factors that may underlie the phenotypic variability in TOF and increase the
susceptibility to CHD in 22q11DS. Identification of these factors would advance current
understanding of cardiogenesis and improve on the use of empiric risks for genetic counselling.

111
Glossary ALLELE: A form of a gene
CANDIDATE GENE: Gene suspected to cause a disease of interest
PHENOTYPIC HETEROGENEITY: Variants of the same gene result in different phenotypes
COPY NUMBER VARIANTS: deletions or duplications of segments of chromosomes
CONCORDANCE: Two members of a family with the same condition
DE NOVO MUTATION: Genetic change that arises spontaneously
DOMINANT GENETIC TRAIT: Expressed when only one copy is present
GENETIC HETEROGENEITY: Genes at different loci giving rise to the same
disease/phenotype
GENETIC POLYMORPHISM: Genetic trait found in more than 1% of the population
GENOMIC IMPRINTING: Differential gene expression dependent on inheritance from a mother
or a father
GENOTYPE: The set of alleles that are found at a particular chromosomal locus
HAPLOINSUFFICIENCY: Only one functional copy of a gene
LINKAGE: Tendency for genetic markers to be inherited together because of close proximity in
chromosomal location
LINKAGE ANALYSIS: Study aimed at establishing linkage between genes

112
MODIFIER GENE: Gene that affects expression of another gene
MULTIPLEX FAMILY: More than one family member with the condition of interest
PENETRANCE: The proportion of people with phenotypic expression of a genetic trait
PHENOTYPE: The clinical, cellular and biochemical expression of a genetic trait
PROBAND: The first member of a family to be identified with a condition of interest
RECESSIVE GENETIC TRAIT: Requires two copies of gene to be expressed
RECURRENCE RISK: The prevalence of disease among relatives of a probands
REDUCED PENETRANCE: Frequency of phenotypic expression of a trait less than 100%
SIMPLEX FAMILY: Only one family member (the probands) with the condition of interest
VARIABLE EXPRESSIVITY: Phenotypic severity differs between two individuals with the
same genotype

113
References
1. Hoffman JIE, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39(12):1890-900.
2. Oyen N, Poulsen G, Boyd HA, Wohlfahrt J, Jensen PK, Melbye M. Recurrence of congenital heart defects in families. Circulation. 2009;120(4):295-301.
3. Apitz C, Webb GD, Redington AN. Tetralogy of fallot. Lancet. 2009;374(9699):1462-71.
4. Neill CA, Clark EB. Tetralogy of fallot - the 1st 300 years. Texas Heart Institute Journal. 1994;21(4):272-9.
5. Starr JP. Tetralogy of fallot: Yesterday and today. World J Surg. 2010;34(4):658-68.
6. Gatzoulis MA, Webb GD, Daubeney PEF, editors. Diagnosis and management of adult congenital heart disease. Second ed. London: Churchill Livingstone; 2011.
7. Wyszynski DF, Correa-Villasenor A, Graham TP, editors. Congenital heart defects from origin to treatment. New York, New York 10016: Oxford University Press, Inc.; 2010.
8. Changela V, John C, Maheshwari S. Unusual cardiac associations with tetralogy of fallot-A descriptive study. Pediatr Cardiol. 2010;31(6):785-91.
9. Rabinovitch M, Herreradeleon V, Castaneda AR, Reid L. Growth and development of the pulmonary vascular bed in patients with tetralogy of fallot with or without pulmonary atresia. Circulation. 1981;64(6):1234-49.
10. Saeed S, Hyder SN, Sadiq M. Anatomical variations of pulmonary artery and associated cardiac defects in tetralogy of fallot. J Coll Physicians Surg. 2009;19(4):211-4.
11. Mcmanus BM, Waller BF, Jones M, Epstein SE, Roberts WC. The case for preoperative coronary angiography in patients with tetralogy of fallot and other complex congenital heart-diseases. Am Heart J. 1982;103(3):451-6.
12. Ramaswamy P, Lytrivi ID, Thanjan MT, Nguyen T, Srivastava S, Sharma S, et al. Frequency of aberrant subclavian artery, arch laterality, and associated intracardiac anomalies detected by echocardiography. Am J Cardiol. 2008;101(5):677-82.
13. Srivastava D. Genetic regulation of cardiogenesis and congenital heart disease. Annu Rev Pathol -Mech Dis. 2006;1(1):199-213.
14. Clark K, Yutzey K, Benson D. Transcription factors and congenital heart defects. Annu Rev Physiol. 2006;68(1):97-121.

114
15. Epstein JA. Franklin H. epstein lecture: Cardiac development and implications for heart disease. N Engl J Med. 2010;363(17):1638-47.
16. Minoux M, Rijli FM. Molecular mechanisms of cranial neural crest cell migration and patterning in craniofacial development. Development. 2010;15;137(16):2605-21.
17. Kirby ML, Bockman DE. Neural crest and normal development - a new perspective. Anat Rec. 1984;209(1):1-6.
18. Porras D, Brown CB. Temporal-spatial ablation of neural crest in the mouse results in cardiovascular defects. Dev Dyn. 2008;237(1):153-62.
19. Ward C, Stadt H, Hutson M, Kirby ML. Ablation of the secondary heart field leads to tetralogy of fallot and pulmonary atresia. Dev Biol. 2005;1;284(1):72-83.
20. Hutson MR, Kirby ML. Model systems for the study of heart development and disease - cardiac neural crest and conotruncal malformations. Semin Cell Dev Biol. 2007;18(1):101-10.
21. Moskowitz IP, Patel VV, Jay P, Pizard A, Peterson M, Bruneau BG, et al. The role of Tbx5 and Nkx2.5 in cardiac conduction system development. Faseb Journal. 2004; 23;18(4):A402-.
22. Calmont A, Ivins S, Van Bueren KL, Papangeli I, Kyriakopoulou V, Andrews WD, et al. Tbx1 controls cardiac neural crest cell migration during arch artery development by regulating Gbx2 expression in the pharyngeal ectoderm. Development. 2009;136(18):3173-83.
23. Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease. J Am Coll Cardiol. 2008;52(23):E1-E121.
24. Clark EB. Cardiac embryology - its relevance to congenital heart-disease. Am J Dis Child. 1986;140(1):41-4.
25. Boughman JA, Berg KA, Astemborski JA, Clark EB, Mccarter RJ, Rubin JD, et al. Familial risks of congenital heart defect assessed in a population-based epidemiologic-study. Am J Med Genet. 1987;26(4):839-49.
26. Tometzki AJP, Suda K, Kohl T, Kovalchin JP, Silverman NH. Accuracy of prenatal echocardiographic diagnosis and prognosis of fetuses with conotruncal anomalies. J Am Coll Cardiol. 1999;33(6):1696-701.
27. Pepas LP, Savis A, Jones A, Sharland GK, Tulloh RMR, Simpson JM. An echocardiographic study of tetralogy of fallot in the fetus and infant. Cardiol Young. 2003;13(3):240-7.
28. Poon LCY, Huggon IC, Zidere V, Allan LD. Tetralogy of fallot in the fetus in the current era. Ultrasound in Obstetrics & Gynecology. 2007;29(6):625-7.
29. Piran S, Bassett AS, Grewal J, Swaby J, Morel C, Oechslin EN, et al. Patterns of cardiac and extracardiac anomalies in adults with tetralogy of fallot. Am Heart J. 2011;161(1).

115
30. Momma K. Cardiovascular anomalies associated with chromosome 22q11.2 deletion syndrome. Am J Cardiol. 2010;105(11):1617-24.
31. Song MS, Hu A, Dyhamenahali U, Chitayat D, Winsor EJT, Ryan G, et al. Extracardiac lesions and chromosomal abnormalities associated with major fetal heart defects: Comparison of intrauterine, postnatal and postmortem diagnoses. Ultrasound Obstet Gynecol. 2009;33(5):552-9.
32. Fung WLA, Chow EWC, Webb GD, Gatzoulis MA, Bassett AS. Extracardiac features predicting 22q11.2 deletion syndrome in adult congenital heart disease. Int J Cardiol. 2008;131(1):51-8.
33. Lamy M, Degrouchy J, Schweisguth O. Genetic and non-genetic factors in the etiology of congenital heart disease - study of 1188 cases. Am J Hum Genet. 1957;9(1):17-41.
34. Lurie IW, Kappetein AP, Loffredo C, Ferencz C. Noncardiac malformations in individuals with outflow tract defects of the heart - the baltimore washington infant study (1981-1989). Am J Med Genet. 1995;59(1):76-84.
35. Kolcz J, Pizarro C. Neonatal repair of tetralogy of fallot results in improved pulmonary artery development without increased need for reintervention. European Journal of Cardio-Thoracic Surgery. 2005;28(3):394-9.
36. Samanek M. Children with congenital heart-disease - probability of natural survival. Pediatr Cardiol. 1992;13(3):152-8.
37. Bertranou EG, Blackstone EH, Hazelrig JB, Turner ME, Kirklin JW. Life expectancy without surgery in tetralogy of fallot. Am J Cardiol. 1978;42(3):458-66.
38. Makaryus AN, Aronov I, Diamond J, Park CH, Rosen SE, Stephen B. Survival to the age of 52 years in a man with unrepaired tetralogy of fallot. Echocardiography-a Journal of Cardiovascular Ultrasound and Allied Techniques. 2004;21(7):631-7.
39. Hickey EJ, Veldtman G, Bradley TJ, Gengsakul A, Manlhiot C, William WG, et al. Late risk of outcomes for adults with repaired tetralogy of fallot from an inception cohort spanning four decades. Eur J Cardio-Thorac Surg. 2009;35(1):156-64.
40. van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJM. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. 2011;8(1):50-60.
41. Burchill LJ, Wald RM, Harris L, Colman JM, Silversides CK. Pulmonary valve replacement in adults with repaired tetralogy of fallot. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2011;14(1):92-7.
42. Warnes CA. The adult with congenital heart disease - born to be bad? J Am Coll Cardiol. 2005;46(1):1-8.
43. Siu SC, Colman JM. Heart disease and pregnancy. Heart. 2001;85(6):710-5.

116
44. Khairy P, Ouyang D, Fernandes S, Lee-Parritz A, Economy K, Landzberg M. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006;113(4):517-24.
45. Pedersen LM, Pedersen TAL, Ravn HB, Hjortdal VE. Outcomes of pregnancy in women with tetralogy of fallot. Cardiol Young. 2008;18(4):423-9.
46. Singh H, Bolton PJ, Oakley CM. Pregnancy after surgical-correction of tetralogy of fallot. Br Med J. 1982;285(6336):168-70.
47. Meijer JM, Pieper PG, Drenthen W, Voors AA, Roos-Hesselink JW, van Dijk APJ, et al. Pregnancy, fertility, and recurrence risk in corrected tetralogy of fallot. Heart. 2005;91(6):801-5.
48. Garcia-Enguidanos A, Calle ME, Valero J, Luna S, Dominguez-Rojas V. Risk factors in miscarriage: A review. European Journal of Obstetrics Gynecology and Reproductive Biology. 2002;102(2):111-9.
49. Veldtman GR, Connolly HM, Grogan M, Ammash NM, Warnes CA. Outcomes of pregnancy in women with tetralogy of fallot. J Am Coll Cardiol. 2004;44(1):174-80.
50. Siu SC, Sermer M, Colman JM, Alvarez AN, Mercier LA, Morton BC, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104(5):515-21.
51. Nunley W, Kolp L, Dabinett L, Kitchin J, Bateman B, Craddock G. Subsequent fertility in women who undergo cardiac surgery. Am J Obstet Gynecol. 1989;161(3):573-6.
52. Kovacs AH, Harrison JL, Colman JM, Sermer M, Siu SC, Silversides CK. Pregnancy and contraception in congenital heart disease: What women are not told. J Am Coll Cardiol. 2008;52(7):577-8.
53. Polani P, Campbell M. An aetiological study of congenital heart disease. Ann Hum Genet. 1955;19(3):209-30.
54. Nora JJ. Multifactorial inheritance hypothesis for the etiology of congenital heart diseases. the genetic-environmental interaction. Circulation. 1968;38(3):604-17.
55. Nora JJ, Nora AH. Genetic and environmental factors in the etiology of congenital heart diseases. South Med J. 1976;69(7):919-26.
56. Mitchell S, Sellmann A, Westphal M, Park J. Etiologic correlates in a study of congenital heart disease in 56,109 births. Am J Cardiol. 1971;28(6):653.
57. Nora JJ, Nora AH, Sommervi.Rj, Hill RM, Mcnamara DG. Maternal exposure to potential teratogens. J Am Med Assoc. 1967;202(12):1065.
58. Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, et al. Noninherited risk factors and congenital cardiovascular defects: Current knowledge a scientific statement from the american heart association council on cardiovascular disease in the young. Circulation. 2007;115(23):2995-3014.

117
59. Pitt DB. A family study of fallot's tetrad. Australas Ann Med. 1962;11:179-83.
60. Pacileo G, Musewe NN, Calabro R. Tetralogy of fallot in 3 siblings - a familial study and review of the literature. Eur J Pediatr. 1992;151(10):726-7.
61. Pankau R, Siekmeyer W, Stoffregen R. Tetralogy of fallot in 3 sibs. Am J Med Genet. 1990;37(4):532-3.
62. Wulfsberg EA, Zintz EJ, Moore JW. The inheritance of conotruncal malformations - a review and report of 2 siblings with tetralogy of fallot with pulmonary atresia. Clin Genet. 1991;40(1):12-6.
63. Derkaloustian VM, Ratl H, Malouf J, Hatem J, Slim M, Tomeh A, et al. Tetralogy of fallot with pulmonary atresia in siblings. Am J Med Genet. 1985;21(1):119-22.
64. Werner P, Raducha MG, Prociuk U, Ostrander EA, Spielman RS, Kirkness EF, et al. The keeshond defect in cardiac conotruncal development is oligogenic. Hum Genet. 2005;116(5):368-77.
65. Folger GM. Tetralogy of fallot in twins. South Med J. 1968;61(1):64.
66. Laugel V, Livolsi A, Viville B, Langer B, Messer J, Fischbach M. Tetralogy of fallot in monozygotic twins. Archives De Pediatrie. 2001;8(4):385-8.
67. Alva C, David Gomez F, Jimenez-Arteaga S, Yanez L, Ochoa L. Concordance of congenital heart defects in two pairs of monozygotic twins: Pulmonary stenosis and tetralogy of fallot. Archivos de Cardiologia de Mexico. 2010;80(1):29-32.
68. Nora JJ, Gillilan.Jc, Sommervi.Rj, Mcnamara DG. Congenital heart disease in twins. N Engl J Med. 1967;277(11):568.
69. Caputo S, Russo MG, Capozzi G, Morelli C, Argiento P, Di Salvo G, et al. Congenital heart disease in a population of dizygotic twins: An echocardiographic study. Int J Cardiol. 2005;102(2):293-6.
70. Nussbaum RL, McInnes RR, Willard HF. Thompson & thompson genetics in medicine. Seventh ed. Saunders; 2007.
71. Hastings PJ, Lupski JR, Rosenberg SM, Ira G. Mechanisms of change in gene copy number. Nat Rev Genet. 2009;10(8):551-64.
72. Bassett A, Scherer S, Brzustowicz L. Copy number variations in schizophrenia: Critical review and new perspectives on concepts of genetics and disease. Am J Psychiatry. 2010;167(8):899-914.
73. Beckmann JS, Estivill X, Antonarakis SE. Copy number variants and genetic traits: Closer to the resolution of phenotypic to genotypic variability. Nat Rev Genet. 2007;8(8):639-46.

118
74. Redon R, Ishikawa S, Fitch KR, Feuk L, Perry GH, Andrews TD, et al. Global variation in copy number in the human genome. Nature. 2006;444(7118):444-54.
75. Pinto D, Pagnamenta AT, Klei L, Anney R, Merico D, Regan R, et al. Functional impact of global rare copy number variation in autism spectrum disorders. Nature. 2010;466(7304):368-72.
76. Bassett AS, Costain G, Fung WLA, Russell KJ, Pierce L, Kapadia R, et al. Clinically detectable copy number variations in a canadian catchment population of schizophrenia. J Psychiatr Res. 2010;44(15):1005-9.
77. Bassett AS, Chow EW, O'Neill S, Brzustowicz LM. Genetic insights into the neurodevelopmental hypothesis of schizophrenia. Schizophr Bull. 2001;27(3):417-30.
78. Miles JH. Autism spectrum disorders-A genetics review. Genet Med. 2011;13(4):278-94.
79. Cullum L, Liebman J. The association of congenital heart disease with down's syndrome (mongolism). Am J Cardiol. 1969;24(3):354-7.
80. Rauch R, Hofbeck M, Zweier C, Koch A, Zink S, Trautmann U, et al. Comprehensive genotype-phenotype analysis in 230 patients with tetralogy of fallot. J Med Genet. 2010;47(5):321-31.
81. Driscoll D, Salvin J, Sellinger B, Budarf M, McDonald-McGinn D, Zackai E, et al. Prevalence of 22q11 microdeletions in DiGeorge and velocardiofacial syndromes: Implications for genetic counselling and prenatal diagnosis. Br Med J. 1993;30(10):813.
82. Trevino V, Falciani F, Barrera-Saldana HA. DNA microarrays: A powerful genomic tool for biomedical and clinical research. Mol Med. 2007;13(9-10):527-41.
83. Lam CW, Lau KC, Tong SF. Microarrays for personalized genomic medicine. Adv Clin Chem. 2010;52:1-18.
84. Greenway SC, Pereira AC, Lin JC, DePalma SR, Israel SJ, Mesquita SM, et al. De novo copy number variants identify new genes and loci in isolated sporadic tetralogy of fallot. Nat Genet. 2009;41(8):931-5.
85. Goldmuntz E, Clark BJ, Mitchell LE, Jawad AF, Cuneo BF, Reed L, et al. Frequency of 22q11 deletions in patients with conotruncal defects. J Am Coll Cardiol. 1998;32(2):492-8.
86. Johnson MC, Hing A, Wood MK, Watson MS. Chromosome abnormalities in congenital heart disease. Am J Med Genet. 1997;70(3):292-8.
87. Goodship J, Cross I, LiLing J, Wren C. A population study of chromosome 22q11 deletions in infancy. Arch Dis Child. 1998;79(4):348-51.
88. Matsuoka R, Kimura M, Scambler PJ, Morrow BE, Imamura S, Minoshima S, et al. Molecular and clinical study of 183 patients with conotruncal anomaly face syndrome. Hum Genet. 1998;103(1):70-80.

119
89. Scambler PJ. The 22q11 deletion syndromes. Hum Mol Genet. 2000;9(16):2421-6.
90. Bassett AS, Marshall CR, Lionel AC, Chow EW, Scherer SW. Copy number variations and risk for schizophrenia in 22q11.2 deletion syndrome. Hum Mol Genet. 2008;17(24):4045-53.
91. Carlson C, Sirotkin H, Pandita R, Goldberg R, McKie J, Wadey R, et al. Molecular definition of 22q11 deletions in 151 velo-cardio-facial syndrome patients. Am J Hum Genet. 1997;61(3):620-9.
92. Morrow B, Goldberg R, Carlson C, Das Gupta R, Sirotkin H, Collins J, et al. Molecular definition of the 22q11 deletions in velo-cardio-facial syndrome. Am J Hum Genet. 1995;56(6):1391-403.
93. Shaikh TH, O'Connor RJ, Pierpont ME, McGrath J, Hacker AM, Nimmakayalu M, et al. Low copy repeats mediate distal chromosome 22q11.2 deletions: Sequence analysis predicts breakpoint mechanisms. Genome Res. 2007;17(4):482-91.
94. Demczuk S, Levy A, Aubry M, Croquette MF, Philip N, Prieur M, et al. Excess of deletions of maternal origin in the Digeorge/velo-cardio-facial syndromes - a study of 22 new patients and review of the literature. Hum Genet. 1995;96(1):9-13.
95. Scambler PJ. 22q11 deletion syndrome: A role for TBX1 in pharyngeal and cardiovascular development. Pediatr Cardiol. 2010;31(3):378-90.
96. Waldo K, Zdanowicz M, Burch J, Kumiski DH, Stadt HA, Godt RE, et al. A novel role for cardiac neural crest in heart development. J Clin Invest. 1999;103(11):1499-507.
97. Kirby ML, Waldo KL. Neural crest and cardiovascular patterning. Circ Res. 1995;77(2):211-5.
98. Bassett AS, Chow EWC, Husted J, Weksberg R, Caluseriu O, Webb GD, et al. Clinical features of 78 adults with 22q11 deletion syndrome. American Journal of Medical Genetics Part a. 2005;138A(4):307-13.
99. Ryan AK, Goodship JA, Wilson DI, Philip N, Levy A, Seidel H, et al. Spectrum of clinical features associated with interstitial chromosome 22q11 deletions: A european collaborative study. J Med Genet. 1997;34(10):798-804.
100. Shprintzen RJ. Velo-cardio-facial syndrome: 30 years of study. Developmental Disabilities Research Reviews. 2008;14(1):3-10.
101. Fung WLA, McEvilly R, Fong J, Silversides C, Chow E, Bassett A. Elevated prevalence of generalized anxiety disorder in adults with 22q11.2 deletion syndrome. Am J Psychiatry. 2010;167(8):998-.
102. Bassett AS, Chow EWC. 22q11 deletion syndrome: A genetic subtype of schizophrenia. Biol Psychiatry. 1999;46(7):882-91.

120
103. Bassett AS, Chow EWC, AbdelMalik P, Gheorghiu M, Husted J, Weksberg R. The schizophrenia phenotype in 22q11 deletion syndrome. Am J Psychiatry. 2003;160(9):1580-6.
104. Zaleski C, Bassett AS, Tam K, Shugar AL, Chow EWC, McPherson E. The co-occurrence of early onset parkinson disease and 22q11.2 deletion syndrome. American Journal of Medical Genetics Part a. 2009;149A(3):525-8.
105. Digilio MC, Angioni A, De Santis M, Lombardo A, Giannotti A, Dallapiccola B, et al. Spectrum of clinical variability in familial deletion 22q11.2: From full manifestation to extremely mild clinical anomalies. Clin Genet. 2003;63(4):308-13.
106. Cohen E, Chow EWC, Weksberg R, Bassett AS. Phenotype of adults with the 22q11 deletion syndrome: A review. Am J Med Genet. 1999;86(4):359-65.
107. Goodship J, Cross I, Scambler P, Burn J. Monozygotic twins with chromosome 22q11 deletion and discordant phenotype. J Med Genet. 1995;32(9):746-8.
108. Marino B, Digilio MC, Toscano A, Anaclerio S, Giannotti A, Feltri C, et al. Anatomic patterns of conotruncal defects associated with deletion 22q11. Genetics in Medicine. 2001;3(1):45-8.
109. Maeda J, Yamagishi H, Matsuoka R, Ishihara J, Tokumura M, Fukushima H, et al. Frequent association of 22q11.2 deletion with tetralogy of fallot. Am J Med Genet. 2000;92(4):269-72.
110. Lewin MB, Lindsay EA, Jurecic V, Gaytia V, Towbin JA, Baldini A. A genetic etiology for interruption of the aortic arch type B. Am J Cardiol. 1997;80(4):493-7.
111. Wilson DI, Cross IE, Goodship JA, Coulthard S, Carey AH, Scambler PJ, et al. DiGeorge syndrome with isolated aortic coarctation and isolated ventricular septal defect in three sibs with a 22q11 deletion of maternal origin. Br Heart J. 1991;66(4):308-12.
112. John AS, McDonald-McGinn DM, Zackai EH, Goldmuntz E. Aortic root dilation in patients with 22q11.2 deletion syndrome. American Journal of Medical Genetics Part a. 2009;149A(5):939-42.
113. Bassett AS, Chow EWC, Husted J, Hodgkinson KA, Oechslin E, Harris L, et al. Premature death in adults with 22q11.2 deletion syndrome. J Med Genet. 2009;46(5):324-30.
114. Zhang Z, Cerrato F, Xu HS, Vitelli F, Morishima M, Vincentz J, et al. Tbx1 expression in pharyngeal epithelia is necessary for pharyngeal arch artery development. Development. 2005;132(23):5307-15.
115. Merscher S, Funke B, Epstein JA, Heyer J, Puech A, Lu MM, et al. TBX1 is responsible for cardiovascular defects in velo-cardio-facial/DiGeorge syndrome. Cell. 2001;104(4):619-29.
116. Jerome LA, Papaioannou VE. DiGeorge syndrome phenotype in mice mutant for the T-box gene, Tbx1. Nat Genet. 2001;27(3):286-91.

121
117. Zhang Z, Baldini A. In vivo response to high-resolution variation of Tbx1 mRNA dosage. Hum Mol Genet. 2008;17(1):150-7.
118. Liao J, Kochilas L, Nowotschin S, Arnold JS, Aggarwal VS, Epstein JA, et al. Full spectrum of malformations in velo-cardio-facial syndrome/DiGeorge syndrome mouse models by altering Tbx1 dosage. Hum Mol Genet. 2004;13(15):1577-85.
119. Gong W, Gottlieb S, Collins J, Blescia A, Dietz H, Goldmuntz E, et al. Mutation analysis of TBX1 in non-deleted patients with features of DGS/VCFS or isolated cardiovascular defects. J Med Genet. 2001;38(12):E45.
120. Yagi H, Furutani Y, Hamada H, Sasaki T, Asakawa S, Minoshima S, et al. Role of TBX1 in human del22q11.2 syndrome. Lancet. 2003;362(9393):1366-73.
121. Zweier C, Sticht H, Aydin-Yaylaguel I, Campbell CE, Rauch A. Human TBX1 missense mutations cause gain of function resulting in the same phenotype as 22q11.2 deletions. Am J Hum Genet. 2007;80(3):510-7.
122. Paylor R, Glaser B, Mupo A, Ataliotis P, Spencer C, Sobotka A, et al. Tbx1 haploinsufficiency is linked to behavioral disorders in mice and humans: Implications for 22q11 deletion syndrome. Proc Natl Acad Sci U S A. 2006;103(20):7729-34.
123. Griffin HR, Toepf A, Glen E, Zweier C, Stuart AG, Parsons J, et al. Systematic survey of variants in TBX1 in non-syndromic tetralogy of fallot identifies a novel 57 base pair deletion that reduces transcriptional activity but finds no evidence for association with common variants. Heart. 2010;96(20):1651-5.
124. Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med. 2000;6(4):389-95.
125. Liang D, Chang JR, Chin AJ, Smith A, Kelly C, Weinberg ES, et al. The role of vascular endothelial growth factor (VEGF) in vasculogenesis, angiogenesis, and hematopoiesis in zebrafish development. Mech Dev. 2001;108(1-2):29-43.
126. Stalmans I, Lambrechts D, De smet F, Jansen S, Wang J, Maity S, et al. VEGF: A modifier of the del22q11 (DiGeorge) syndrome? Nat Med. 2003;9(2):173-82.
127. Lambrechts D, Devriendt K, Driscoll DA, Goldmuntz E, Gewillig M, Vlietinck R, et al. Low expression VEGF haplotype increases the risk for tetralogy of fallot: A family based association study. J Med Genet. 2005;42(6):519-22.
128. Griffin HR, Hall DH, Topf A, Eden J, Stuart AG, Parsons J, et al. Genetic variation in VEGF does not contribute significantly to the risk of congenital cardiovascular malformation. PLoS One. 2009 MAR;4(3):e4978.
129. Digilio MC, Marino B, Capolino R, Angioni A, Sarkozy A, Roberti MC, et al. Familial recurrence of nonsyndromic congenital heart defects in first degree relatives of patients with deletion 22q11.2. Am J Med Genet A. 2005;134A(2):158-64.

122
130. Worthington S, Turner A, Elber J, Andrews PI. 22q11 deletion and polymicrogyria - cause or coincidence? Clin Dysmorphol. 2000;9(3):193-7.
131. Mefford HC, Sharp AJ, Baker C, Itsara A, Jiang Z, Buysse K, et al. Recurrent rearrangements of chromosome 1q21.1 and variable pediatric phenotypes. N Engl J Med. 2008;359(16):1685-U130.
132. Christiansen J, Dyck JD, Elyas BG, Lilley M, Bamforth JS, Hicks M, et al. Chromosome 1q21.1 contiguous gene deletion is associated with congenital heart disease. Circ Res. 2004;94(11):1429-35.
133. Walsh T, McClellan JM, McCarthy SE, Addington AM, Pierce SB, Cooper GM, et al. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science. 2008;320(5875):539-43.
134. Brunetti-Pierri N, Berg JS, Scaglia F, Belmont J, Bacino CA, Sahoo T, et al. Recurrent reciprocal 1q21.1 deletions and duplications associated with microcephaly or macrocephaly and developmental and behavioral abnormalities. Nat Genet. 2008;40(12):1466-71.
135. Cheroki C, Krepischi-Santos ACV, Szuhai K, Brenner V, Kim CAE, Otto PA, et al. Genomic imbalances associated with mullerian aplasia. J Med Genet. 2008;45(4):228-32.
136. Razzaque MA, Nishizawa T, Komoike Y, Yagi H, Furutani M, Amo R, et al. Germline gain-of-function mutations in RAF1 cause noonan syndrome. Nat Genet. 2007;39(8):1013-7.
137. Costain G, Silversides CK, Marshall CR, Shago M, Costain N, Bassett AS. 13q13.1-q13.2 deletion in tetralogy of fallot: Clinical report and a literature review. Int J Cardiol. 2011;146(2):134-9.
138. Thienpont B, Mertens L, de Ravel T, Eyskens B, Boshoff D, Maas N, et al. Submicroscopic chromosomal imbalances detected by array-CGH are a frequent cause of congenital heart defects in selected patients. Eur Heart J. 2007;28(22):2778-84.
139. Baekvad-Hansen M, Tumer Z, Delicado A, Erdogan F, Tommerup N, Larsen LA. Delineation of a 2.2 mb microdeletion at 5q35 associated with microcephaly and congenital heart disease. Am J Med Genet A. 2006;140A(5):427-33.
140. Goldmuntz E, Geiger E, Benson DW. NKX2.5 mutations in patients with tetralogy of fallot. Circulation. 2001;104(21):2565-8.
141. Andelfinger G. Genetic factors in congenital heart malformation. Clin Genet. 2008;73(6):516-27.
142. Schott JJ, Benson DW, Basson CT, Pease W, Silberbach GM, Moak JP, et al. Congenital heart disease caused by mutations in the transcription factor NKX2-5. Science. 1998;281(5373):108-11.
143. McElhinney DB, Geiger E, Blinder J, Benson DW, Goldmuntz E. NKX2.5 mutations in patients with congenital heart disease. J Am Coll Cardiol. 2003;42(9):1650-5.

123
144. Stallmeyer B, Fenge H, Nowak-Gottl U, Schulze-Bahr E. Mutational spectrum in the cardiac transcription factor gene NKX2.5 (CSX) associated with congenital heart disease. Clin Genet. 2010;78(6):533-540.
145. Benson DW, Silberbach GM, Kavanaugh-McHugh A, Cottrill C, Zhang YZ, Riggs S, et al. Mutations in the cardiac transcription factor NKX2.5 affect diverse cardiac developmental pathways. J Clin Invest. 1999;104(11):1567-73.
146. Elliott DA, Kirk EP, Yeoh T, Chandar S, McKenzie F, Taylor P, et al. Cardiac homeobox gene NKX2-5 mutations and congenital heart disease - associations with atrial septal defect and hypoplastic left heart syndrome. J Am Coll Cardiol. 2003;41(11):2072-6.
147. Gioli-Pereira L, Pereira AC, Mesquita SM, Xavier-Neto J, Lopes AA, Krieger JE. NKX2.5 mutations in patients with non-syndromic congenital heart disease. Int J Cardiol. 2010;138(3):261-5.
148. MacGrogan D, Nus M, Luis de la Pompa J. Notch signaling in cardiac development and disease. Notch Signaling. 2010;92:333-65.
149. Li LH, Krantz ID, Deng Y, Genin A, Banta AB, Collins CC, et al. Alagille syndrome is caused by mutations in human Jagged1, which encodes a ligand for Notch1. Nat Genet. 1997;16(3):243-51.
150. Krantz ID, Smith R, Colliton RP, Tinkel H, Zackai EH, Piccoli DA, et al. Jagged1 mutations in patients ascertained with isolated congenital heart defects. Am J Med Genet. 1999;84(1):56-60.
151. Oda T, Elkahloun AG, Meltzer PS, Chandrasekharappa SC. Identification and cloning of the human homolog (JAG1) of the rat Jagged1 gene from the alagille syndrome critical region at 20p12. Genomics. 1997;43(3):376-9.
152. Oda T, Elkahloun AG, Pike BL, Okajima K, Krantz ID, Genin A, et al. Mutations in the human Jagged1 gene are responsible for alagille syndrome. Nat Genet. 1997;16(3):235-42.
153. Eldadah ZA, Hamosh A, Biery NJ, Montgomery RA, Duke M, Elkins R, et al. Familial tetralogy of fallot caused by mutation in the jagged1 gene. Hum Mol Genet. 2001 JAN;10(2):163-9.
154. Bauer RC, Laney AO, Smith R, Geffen J, Morrissette JJD, Woyciechowski S, et al. Jagged1 (JAG1) mutations in patients with tetralogy of fallot or pulmonic stenosis. Hum Mutat. 2010;31(5):594-601.
155. Pizzuti A, Sarkozy A, Newton AL, Conti E, Flex E, Digilio MC, et al. Mutations of ZFPM2/FOG2 gene in sporadic cases of tetralogy of fallot. Hum Mutat. 2003;22(5):372-7.
156. Svensson EC, Huggins GS, Lin H, Clendenin C, Jiang F, Tufts R, et al. A syndrome of tricuspid atresia in mice with a targeted mutation of the gene encoding fog-2. Nat Genet. 2000;25(3):353-6.

124
157. Tevosian SG, Deconinck AE, Tanaka M, Schinke M, Litovsky SH, Izumo S, et al. FOG-2, a cofactor for GATA transcription factors, is essential for heart morphogenesis and development of coronary vessels from epicardium. Cell. 2000;101(7):729-39.
158. De Luca A, Sarkozy A, Ferese R, Consoli F, Lepri F, Dentici ML, et al. New mutations in ZFPM2/FOG2 gene in tetralogy of fallot and double outlet right ventricle. Clin Genet. 2010 Aug (Epub ahead of print).
159. Peng T, Wang L, Zhou S, Li X. Mutations of the GATA4 and NKX2.5 genes in chinese pediatric patients with non-familial congenital heart disease. Genetica. 2010;138(11-12):1231-40.
160. Zhang W, Li X, Shen A, Jiao W, Guan X, Li Z. GATA4 mutations in 486 chinese patients with congenital heart disease. Eur J Med Genet. 2008;51(6):527-35.
161. Tomita-Mitchell A, Maslen CL, Morris CD, Garg V, Goldmuntz E. GATA4 sequence variants in patients with congenital heart disease. J Med Genet. 2007;44(12):779-83.
162. Wat MJ, Shchelochkov OA, Holder AM, Breman AM, Dagli A, Bacino C, et al. Chromosome 8p23.1 deletions as a cause of complex congenital heart defects and diaphragmatic hernia. Am J Med Genet A. 2009;149A(8):1661-77.
163. Barber JCK, Maloney VK, Huang S, Bunyan DJ, Cresswell L, Kinning E, et al. 8p23.1 duplication syndrome; a novel genomic condition with unexpected complexity revealed by array CGH. European Journal of Human Genetics. 2008;16(1):18-27.
164. Kodo K, Nishizawa T, Furutani M, Arai S, Yamamura E, Joo K, et al. GATA6 mutations cause human cardiac outflow tract defects by disrupting semaphorin-plexin signaling. Proc Natl Acad Sci U S A. 2009;106(33):13933-8.
165. Lin X, Huo Z, Liu X, Zhang Y, Li L, Zhao H, et al. A novel GATA6 mutation in patients with tetralogy of fallot or atrial septal defect. J Hum Genet. 2010;55(10):662-7.
166. Maitra M, Koenig SN, Srivastava D, Garg V. Identification of GATA6 sequence variants in patients with congenital heart defects. Pediatr Res. 2010;68(4):281-5.
167. Kamath BM, Krantz ID, Spinner NB, Heubi JE, Piccoli DA. Monozygotic twins with a severe form of alagille syndrome and phenotypic discordance. Am J Med Genet. 2002;112(2):194-7.
168. Biesecker BB. Goals of genetic counseling. Clin Genet. 2001;60(5):323-30.
169. Hoess K, Goldmuntz E, Pyeritz RE. Genetic counseling for congenital heart disease: New approaches for a new decade. Curr Cardiol Rep. 2002;4(1):68-75.
170. Nora JJ, Dodd PF, Mcnamara DG, Hattwick MA, Leachman RD, Cooley DA. Risk to offspring of parents with congenital heart defects. J Am Med Assoc. 1969;209(13):2052.

125
171. Boon AR, Roberts DF, Farmer MB. Family study of fallots tetralogy. J Med Genet. 1972;9(2):179.
172. Zellers TM, Driscoll DJ, Michels VV. Prevalence of significant congenital heart defects in children of parents with fallot's tetralogy. Am J Cardiol. 1990;65(7):523-6.
173. Whittemore R, Hobbins JC, Engle MA. Pregnancy and its outcome in women with and without surgical treatment of congenital heart disease. Am J Cardiol. 1982;50(3):641-51.
174. Digilio MC, Marino B, Giannotti A, Toscano A, Dallapiccola B. Recurrence risk figures for isolated tetralogy of fallot after screening for 22q11 microdeletion. J Med Genet. 1997;34(3):188-90.
175. Burn J, Brennan P, Little J, Holloway S, Coffey R, Somerville J, et al. Recurrence risks in offspring of adults with major heart defects: Results from first cohort of british collaborative study. Lancet. 1998;351(9099):311-6.
176. Nora JJ, Meyer TC. Familial nature of congenital heart diseases. Pediatrics. 1966;37(2):329.
177. Nora JJ, Nora AH. Recurrence risks in children having one parent with a congenital heart disease. Circulation. 1976;53(4):701-2.
178. Nora JJ, Nora AH. Maternal transmission of congenital heart-diseases - new recurrence risk figures and the questions of cytoplasmic inheritance and vulnerability to teratogens. Am J Cardiol. 1987;59(5):459-63.
179. Benson DW. Advances in cardiovascular genetics and embryology: Role of transcription factors in congenital heart disease. Curr Opin Pediatr. 2000;12(5):497-500.
180. Benson DW. The genetics of congenital heart disease: A point in the revolution. Cardiol Clin. 2002;20(3):385,94.
181. Marden PM, Smith DW, Mcdonald MJ. Congenital anomalies in newborn infant including minor variations - study of 4412 babies by surface examination for anomalies + buccal smear for sex chromatin. J Pediatr. 1964;64(3):357.
182. Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: Changing prevalence and age distribution. Circulation. 2007;115(2):163-72.
183. Ermis C, Gupta-Malhotra M, Titus JL. An obstructive bicuspid aortic valve in the setting of tetralogy of fallot with pulmonary atresia: A rare combination. Cardiol Young. 2004;14(1):99-101.
184. Morales DLS, DiBardino DJ, Vick W, Fraser CD, McKenzie ED. Tetralogy of fallot and hypoplastic aortic arch: A novel perspective. J Thorac Cardiovasc Surg. 2005;129(6):1448-50.
185. Niwa K. Aortic root dilatation in tetralogy of fallot long-terrn after repair - histology of the aorta in tetralogy of fallot: Evidence of intrinsic aortopathy. Int J Cardiol. 2005;103(2):117-9.

126
186. Lewin MB, McBride KL, Pignatelli R, Fernbach S, Combes A, Menesses A, et al. Echocardiographic evaluation of asymptomatic parental and sibling cardiovascular anomalies associated with congenital left ventricular outflow tract lesions. Pediatrics. 2004;114(3):691-6.
187. Hinton RB, Jr., Martin LJ, Tabangin ME, Mazwi ML, Cripe LH, Benson DW. Hypoplastic left heart syndrome is heritable. J Am Coll Cardiol. 2007;50(16):1590-5.
188. Brenner JI, Berg KA, Schneider DS, Clark EB, Boughman JA. Cardiac-malformations in relatives of infants with hypoplastic left-heart syndrome. Am J Dis Child. 1989;143(12):1492-4.
189. Cripe L, Andelfinger G, Martin LJ, Shooner K, Benson DW. Bicuspid aortic valve is heritable. J Am Coll Cardiol. 2004;44(1):138-43.
190. Huntington K, Hunter AGW, Chan KL. A prospective study to assess the frequency of familial clustering of congenital bicuspid aortic valve. J Am Coll Cardiol. 1997;30(7):1809-12.
191. Garg V, Muth AN, Ransom JF, Schluterman MK, Barnes R, King IN, et al. Mutations in NOTCH1 cause aortic valve disease. Nature. 2005;437(7056):270-4.
192. Kappetein AP, Gittenbergerdegroot AC, Zwinderman AH, Rohmer J, Poelmann RE, Huysmans HA. The neural crest as a possible pathogenetic factor in coarctation of the aorta and bicuspid aortic-valve. J Thorac Cardiovasc Surg. 1991;102(6):830-6.
193. Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria: Reliability and validity. Arch Gen Psychiatry. 1977;34(10):1229.
194. Andreasen NC, John R, Jean E, Theodore R, William C. The family history approach to diagnosis: How useful is it? Arch Gen Psychiatry. 1986;43(5):421.
195. Ottman R, Barker-Cummings C, Leibson CL, Vasoli VM, Hauser WA, Buchhalter JR. Accuracy of family history information on epilepsy and other seizure disorders. Neurology. 2011;76(4):390-6.
196. Hay JD. Population and clinic studies of congenital heart disease in liverpool. Br Med J. 1966;2(5515):661.
197. Census families by number of children at home, by province and territory (2006 census) [Internet]. Ottawa: Statistics Canada; 2006.
198. Live births, mean age of mother, provinces and territories, Canada, annual [Internet]. Ottawa: Statistics Canada; 2007. Available from: http://www4.hrsdc.gc.ca/[email protected]?iid=75.
199. Hinton RB,Jr. The family history: Reemergence of an established tool. Crit Care Nurs Clin North Am. 2008;20(2):149,58.
200. Wijdenes-Pijl M, Henneman L, Cross-Bardell L, Timmermans DR, Qureshi N. How does a simple enquiry compare to a detailed family history questionnaire to identify coronary heart disease or diabetic familial risk? Genet Med. 2011 Feb (epub ahead of print).

127
201. Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol. 2010;55(25):2789-800.
202. Billett J, Cowie MR, Gatzoulis MA, Muhll IFV, Majeed A. Comorbidity, healthcare utilisation and process of care measures in patients with congenital heart disease in the UK: Cross-sectional, population-based study with case-control analysis. Heart. 2008;94(9):1194-9.
203. Gropman AL, Batshaw ML. Epigenetics, copy number variation, and other molecular mechanisms underlying neurodevelopmental disabilities: New insights and diagnostic approaches. J Dev Behav Pediatr. 2010;31(7):582-91.
204. Bentham J, Bhattacharya S. Genetic mechanisms controlling cardiovascular development. Ann NY Acad Sci. 2008;1123:10-9.
205. Fallin MD, Lasseter VK, Liu Y, Avramopoulos D, McGrath J, Wolyniec PS, et al. Linkage and association on 8p21.2-p21.1 in schizophrenia. Am J Med Genet B. 2011;156B(2):188-97.
206. Chico TJA, Milo M, Crossman DC. The genetics of cardiovascular disease: New insights from emerging approaches. J Pathol. 2010;220(2):186-97.