Evaluation of Anemia. Hemoglobin below the normal reference level for the age and sex of the...
-
Upload
felix-phelps -
Category
Documents
-
view
223 -
download
1
Transcript of Evaluation of Anemia. Hemoglobin below the normal reference level for the age and sex of the...
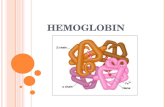
Hemoglobin below the normal reference level for the age and sex of the individual
Reference range: 1-3 days: 14.5 - 22.5g/dl 6 months to 2 years: 10.5 - 13.5g/dl Adult Men: 13-18 g/dl Adult Women: 11.5-15.5g/dl
Clinical Features (symptoms):INFANTS
• Irritability, restlessness• Anorexia, sleepiness• Behavioral changes
Clinical Features (symptoms):ADULTS
Common• Fatigue/Muscle weakness• Headache/Lack of concentration• Faintness/dizziness
Exertional dyspnoea/palpitation
Angina/intermittent claudication
Clinical Features (signs):
Non-specific• pallor, tacycardia, flow mummer
Specific• koilonychia, angular stomatitis, glossitis• neuropathy, dementia, paraplegia• jaundice, bone deformities, leg ulcer
Anemia- Signs/Symptoms
Dyspnea on exertion
Palpitations
Angina pectoris
Intermittent claudication
Headache
SyncopeanorexiaDizziness/vertigoNauseaCold intoleranceAmenorrheaDecrease libido/impotence
History:
Physiological Inadequate
intake Blood loss Malabsorption
Comorbids Drug history Family history
Classification of Anemia (Mean Corpuscular volume):
Microcyctic – MCV < 80 fL
Macrocytic – MCV > 100 fL
Normocytic MCV 80 – 100 fL
Microcytic Anemia
Iron deficiency
Hemoglobinopathy
Lead poisoning Sideroblastic Occasionally chronic disease
If no obvious cause
Serum Ferritin:< 15ug/l : Iron deficiency
Normal or : Serum Iron / Increased (TIBC)
What’s normal?
H/H– Anemia criteria6-23 m 10/31
2-5 y 11/34
6-12 12/37
MCVLower 70 + years in age (2-10)
Upper0.6/year + 84 (up to 96y)
RDW11.5%-14.5%
Reticulocyte count
Corrected 1%
Mentzer indexMCV/RBC
<12 thal trait
>13 Fe deficiency
Clinical Manifestations of Anemia
AsymptomaticSymptoms begin when HgB <7-8g/dLVague symptoms
IrritabilityFatigueDyspnea – especially with exertionWeakness
SignsPallorTachycardiaTachypneaCongestive heart failure
The Approach - HistoryAge:
Newborn period – hemolytic anemia, blood loss, Fe deficiency rare before 4-6mo old3-6mo old – hemoglobinopathy, maybe iron deficiency6-18mo old – iron deficiency most common, consider TEC> 18mo – differential broadens
GenderMale – X-linked disease
RaceAA – Sickle cell diseaseMiddle eastern, southeast asian, southern european – β thalassemiaAA and southeast asians – æ thalassemia
DietExcessive cow’s milk consumption – Fe deficiencyStrict vegetarian – B12 deficiencyGoat’s milk as milk protein source – folate deficiency
Drug historyAntibiotics, anti-inflammatory meds, anticonvulsants
InfectionsFHx
Anemia? Gallstones? Splenectomy? Transfusions?
The Approach – Physical Exam
Abnormal forearm and hand, café-au-lait macules, short stature
Fanconi anemiaTriphalangeal thumb
Diamond-Blackfan anemiaFrontal bossing, maxillary overgrowth
Congenital hemolytic anemiaAortic stenosis, VSD
Microangiopathic hemolytic anemiaSplenomegaly
Inherited hemolytic anemiaAtaxia and posterior column signs
B12 deficiency
Labs are Helpful – Within ReasonCBC with differential
Evaluate all cell lines
Red cell indices
MCV and RDW = critical
Peripheral smear
Reticulocyte count
Coomb’s
If smear indicates hemolysis
MCV and RDW = Critical
Low MCV = microcytosisIron deficiency
Thalassemia trait
Hemoglobin EE disease
(lead poisoning)
(chronic disease)
High MCV = macrocytosisNutritional deficiency
Bone marrow failureAplastic anemia
Drug suppression
Diamond-Blackfan
Increased RDW
Helps distinguish between iron deficiency and thalassemia trait
Making Your Diagnosis
History and physical = most important
LabsCBC with differential and smear
Red cell indicesMCV and RDW = critical
Reticulocyte countNot necessarily needed if H&P strongly suggest Fe deficiency as cause of anemia
If an unusual hx, or age < 6 mo or >18 mo-2y/o, then other labs are needed
Iron Deficiency Anemia Labs
In order of changes that occurRDW increases
Serum Fe levels fall
MCV decreases
HgB/Hct drops
Other labs may be done – but not necessary
Iron studies:FerritinTIBCFEPIron
Hgb electrophoresis:A2 and F quantification
ESR, UA, stool guiacCBC and smear of parents
Additional Labs
Microcytosis & Fe studies
Fe deficiency
Thal trait Lead poisoning
Hgb N
MCV N
RDW N N
FEP N
Serum Fe N N
TIBC N N
Ferritin N N
Evaluation continued..Serum Iron
TIBC Peripheral smear
Iron deficiency
Decreased
Increased Hypochromic
Target cells Basophilic stippling
Normal Increased
IncreasedThallasemia
Diamorphic
NormalIncreasedSideroblast
Hypo/normo chromic
Decreased
Decreased
Chronic disease
Thallesemia Mentzer index: MCV/RBC count. <13 Hb Electrophoresis
Sideroblastic anemia Bone marrow exam
Iron deficiency anemia in men/post menopausal women Gastro-intestinal endoscopy Barium studies
Evaluation continued..
Macrocytic anemia (evaluation):
Peripheral film & Reticulocyte count
Macrocytes absent
Normal reticulocyte artifactual (hyperglycemia/natremia,
cold agglutinin, and extreme leucocytosis)
High reticulocyte hemolysis, bleeding or nutritional
response to folate/B12/iron
Evaluation continued...
Macrocytes present
With megaloblast MCV>120B12 deficiency, Folic acid deficiency
Drugs (cytotoxic, anticonvulsant, antibiotic)
Without megaloblast MCV 100-120Liver disease, Alcoholism
Hypothyroidism, Myelodysplastic disorders
Normocytic anemia (causes):
Increased RBC loss/destructionacute blood loss, hypersplenism, hemolytic
disease
Decreased RBC productionprimary cause i.e bone marrow disorders
secondary cause i.e CRF, liver disease, chronic disease
Over-expansion of plasma volumepregnancy, overhydration
Normocytic anemia (evaluation):
CBC, Peripheral smear & Retic count
Normal retic and mild anemia >9gm/dl chronic disease
Normal or decreased retic with leucopenia/thrombocytopenia/blast cell
bone marrow exam
Elevated retic count Direct Coombs test: +ve autoimmune HA
-ve mechanical or other HA
Conclusion:
Evaluation based on MCV
Microcytosis is due to iron deficiency unless proven otherwise
Megaloblast help in differentiating cause of macrocytosis
CBC and reticulocyte count essential for normocytic anemia
The Medical Student’s Approach to Anemia
1. Check the reticulocyte count to determine if the anemia is from decreased production (“hypoproliferative”, “reticulocytopenic”) or increased destruction (“hemolytic”)/acute blood loss (“reticulocytosis”)
2. If decreased production, narrow down the causes in terms of the MCV-
If the MCV is low, then do iron studies then Hb electropheresisIf the MCV is normal, check the serum creatinine and TSH, if they are WNL then consider bone marrow exam
If the MCV is high check a folate and vitamin B12 level3. If the the reticulocyte count is increased-
Check a direct Coomb’s test4. Look at the peripheral blood smear to confirm/support the diagnosis
Anemia Algorithm
Patient with anemia and decreased reticulocyte count-
What is the MCV ??
Microcytic
Fe
def.
Thal
Other: sideroblastic anemia (meds,PB,Zn excess,Cu def)
NormocyticMacrocytic:
•Vitamin-related
B12, Folate
•Non-vitamin:
•MDS
•EtOH/Liver Disease
•Hypothyroidism
Systemic Diseases
Diseases in Bone Marrow
•MDS
•Solid Tumor
•Myeloma
•Aplastic anemia
Renal vs. Liver vs. Endocrine vs.
Anemia of Inflammation
Anemia Algorithm, continuedPatient with anemia and increased reticulocyte count-
What is the result of a Coomb’s test ??
Extrinsic red cell defect
Vessel
Valve
Toxin
Negativ
Positive (autoimmune hemolytic
anemia)
Intrinsic red cell defect
Membrane
Hemoglobin
Cytoplasm
“Warm” “Cold”
The Attending’s Approach to Anemia
1. Stool guiacs x 3
2. If the MCV is low, then prescribe iron
3. If the MCV is high, then check a folate level and vitamin B12 level
if folate level returns low or “indeterminate”, then begin folic acid 1 mg po qd
if B12 level returns low or “indeterminate”, then begin IM vitamin B12
Blood Loss Anemia
Excessive bleeding InjurySurgery Problem with the blood's clotting mechanism (inherited)
Ie hemophilia
Heavy menstrual periods in teen girls and women (most common problem)
Slower, long-term blood loss Ie Intestinal bleeding and inflammatory bowel disease
http://www.innvista.com/health/ailments/anemias/bloodlos.htm
Physiologic Reactions to Blood Loss
Acute – Peripheral vasoconstriction and central vasodilatation
If blood loss continues – small vessel dilatation with compensatory decreased PVR, resulting in increased CO.
Chronic - Increased plasma volume keeps intravascular volume normal
Erythropoietin released by kidneys – reticulocytes in 3-7 days.
POST HEMORRHAGIC ANEMIA
BP
ACTIVATES SNS VASCULAR RESISTANCE, HR, STROKE VOLUME
RR TO IMPROVE OXYGENATION
Anemia of Acute Blood Loss
Trauma or GI tract loss most commonMenstrual/vaginal lossUrinary tractNosebleeds leading to anemia, but not because of it!Tachycardia and hypotension are common findingsHistory helps the most for these
Signs and Symptoms
Depend uponRate of blood loss
Amount of blood lost
Age
Overall Health
Comorbid disease states
Physical Exam Findings
+ Orthostatic BP’s
Tachycardia
Pallor
Systolic ejc. murmur
Widened pulse pressure
GI bleeding/Uterine bleeding
Altered Mental Status