Etiology of New-Onset Jaundice: How Often Is It Caused by Idiosyncratic Drug-Induced Liver Injury in...
Transcript of Etiology of New-Onset Jaundice: How Often Is It Caused by Idiosyncratic Drug-Induced Liver Injury in...
American Journal of Gastroenterology ISSN 0002-9270C© 2007 by Am. Coll. of Gastroenterology doi: 10.1111/j.1572-0241.2006.01019.xPublished by Blackwell Publishing
Etiology of New-Onset Jaundice: How OftenIs It Caused by Idiosyncratic Drug-Induced Liver Injuryin The United States?
CME
Raj Vuppalanchi, M.D., Suthat Liangpunsakul, M.D., and Naga Chalasani, M.D.Department of Medicine, Indiana University School of Medicine, Indianapolis, Indiana
BACKGROUND The epidemiology of acute drug-induced liver injury (DILI) in the United States has not been wellAND AIM: studied. We conducted a study of adults with new-onset jaundice at a nonreferral community hospital
to better understand the epidemiology of acute DILI.
METHODS: This is a retrospective study of adult outpatients and inpatients (≥18 yr) with new-onset jaundiceover a 5-yr period (1999–2003) at Wishard Memorial Hospital, Indiana. Patients with new-onsetjaundice were identified using our electronic medical record system and individual medical recordswere reviewed to extract the required clinical data. New-onset jaundice was defined as the presenceof total serum bilirubin >3 mg/dL in patients without a prior total bilirubin >3 mg/dL.
RESULTS: A total of 732 eligible adults constituted our study cohort. Sepsis or altered hemodynamic stateresulting in presumed ischemic liver injury is the single most common cause of jaundice (22%).Acute liver disease as a result of nonalcoholic etiologies caused new-onset jaundice in 97 patients(13%), with acute viral hepatitis in 66 patients (9%) and DILI in 29 patients (4%). Most cases of DILIwere as a result of acetaminophen toxicity with idiosyncratic DILI occurring in only five patients(0.7%). No mortality was observed at 6 wk in patients who developed idiosyncratic DILI.
CONCLUSION: Idiosyncratic DILI appears to be a rare cause of new-onset jaundice in a community hospital setting.
(Am J Gastroenterol 2007;102:558–562)
INTRODUCTION
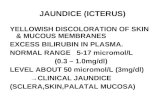
Jaundice, defined as total serum bilirubin >3 mg/dL, is oneof the manifestations of significant liver injury. It could re-sult from a variety of hepatic and extrahepatic etiologies.Although it is a routinely encountered problem by gastro-enterologists and hepatologists, it is much less common ininternal medicine practices. Some studies have highlightedthe discrepancies between gastroenterologists’ and primarycare physicians’ perceptions of common causes of jaundice(1). Several prospective and retrospective studies assessingthe common causes of jaundice in European cohorts found aconflicting pattern in the distribution of etiologies (2–5). Thisdiscrepancy likely resulted from the study design and the in-patient vs outpatient status of the study population. Otherconfounding factors include referral bias, ethnic backgroundof the study population, research interest, and expertise of thehepatologists at the referral center. Few studies that evaluatedthe etiology of new-onset jaundice in patients residing in theUnited States have stemmed from tertiary care centers withreferral bias (6).
To access a continuing medical education exam for this article, please visitwww.acg.gi.org/journalcme.
Over the last decade, it has become clear that drug-inducedliver injury (DILI) is an important health condition affectingdrug development and drug availability in the United States.However, the epidemiology of DILI is poorly understood.With increasing use of prescription drugs and changing epi-demiology of many types of liver diseases (e.g., hepatitis B),the epidemiology of new-onset jaundice at a community levelmay have changed. With these issues in mind, we have con-ducted a cohort study to evaluate the etiology of new-onsetjaundice and to assess how often idiosyncratic DILI causesnew-onset jaundice at a community-based health-care sys-tem.
METHODS
This is a retrospective study of adult patients (≥18 yr) whopresented with new-onset jaundice over a 5-yr period (1999–2003) to Wishard Memorial Hospital (400-bed innercity aca-demic hospital) and 30 affiliated primary care clinics scat-tered around the inner city of Indianapolis. New-onset jaun-dice was defined as the presence of total serum bilirubin >3mg/dL in patients without a prior total bilirubin >3 mg/dL.This cohort consisted of both inpatients and outpatients seenat our facilities during the study period. Patients who had
558
DILI and New-Onset Jaundice 559
new-onset jaundice during the study period were identifiedusing the Regenstrief Medical Record System (RMRS). TheRMRS is a well-recognized electronic medical record systemthat captures patient information from a number of clinicsaffiliated with Wishard Hospital. The RMRS links individ-ual medical records with laboratory, radiology, pathology,and prescription information using unique patient identifiers.This study was reviewed and approved by the InstitutionalReview Board at Indiana University School of Medicine.
The electronic medical records of each eligible patient werereviewed in a systematic fashion by the authors (R.V. and S.L)and the data were extracted onto a standardized datasheet. Theetiology of jaundice was determined using the standard clini-cal definitions. When the etiology of jaundice was not obviousor when multiple potential etiologies existed, the case recordswere independently reviewed by two authors and a diagnosiswas arrived at by consensus. Patients in whom the etiology ofjaundice could not be ascertained because of lack of optimaldata (e.g., patients leaving against medical advice) were con-sidered ineligible. The cohort’s mortality rate was assessed at6 wk after the initial presentation with new-onset jaundice.The quality of data retrieval and diagnosis ascertainment wassystematically verified by random and independent review ofthe medical records by the senior author (N.C.).
STATISTICAL ANALYSES
Basic descriptive statistics, including mean, standard devia-tions (SD), and ranges were used to characterize the studypatients. The number of patients with different etiologieswas tabulated and percentages were calculated to reflect theproportion of the total cohort. The Roussel Uclaf CausalityAssessment Method (RUCAM) was used to determine thecausality of the offending drug in each case of suspectedidiosyncratic DILI (7).
RESULTS
Seven hundred seventy-eight patients had new-onset jaun-dice during the study period. After excluding 46 ineligiblepatients, 732 eligible adults constituted our study cohort. Se-lected demographic and clinical characteristics are shown inTable 1. During this period, 53,989 patients were inpatientsat the Wishard Memorial Hospital, 189,679 were seen in theemergency department, and 98,861 were seen in the primarycare clinics.
The various etiologies for new-onset jaundice in this cohortof patients are shown in Table 2. Fifty-five percent of patients(N = 406) had jaundice because of hepatic etiology and theremaining 45% of patients (N = 326) developed jaundicefrom an extrahepatic etiology (Table 2).
The decompensation of pre-existing chronic liver diseaseand acute alcoholic liver disease were the most common hep-atic etiologies for new-onset jaundice accounting for 37% oftotal cases. Acute liver disease as a result of nonalcoholic
Table 1. Demographics and Selected Biochemical Parameters ofStudy Cohort (N = 732)
Age (Yr, Mean ± SD) 45.7 ± 14.6
Male 62%Ethnicity
Caucasian 52%African American 32%Hispanic 7%Asian 1%Native American 0.2%Undocumented 7%
Serum liver biochemistries (Mean ± SD)Total bilirubin (mg/dL) 8.3 ± 6.8AST (U/L) 781 ± 2,289ALT (U/L) 520 ± 1,206Alkaline phosphatase (U/L) 285 ± 322
etiologies caused new-onset jaundice in 98 patients (13%)with acute viral hepatitis in 66 patients (9%) and DILI in 29patients (Table 2). Most cases of DILI were as a result ofacetaminophen toxicity and idiosyncratic DILI was the etiol-ogy in only five patients (0.7%). The clinical characteristicsof patients with idiosyncratic DILI are shown in Table 3.
Sepsis or altered hemodynamic state resulting in presumedischemic liver injury caused new-onset jaundice in 159 pa-tients (22%). These were hospitalized patients and a majorityof them suffered from severe burn injuries or had sustainedsevere traumatic wounds. Their mean age was 49 ± 17 yr andtheir peak biochemical parameters were: serum total biliru-bin 7.1 ± 5.2 mg/dL, aspartate transaminase (AST) 910 ±2,488 U/L, alanine transaminase (ALT) 360 ± 1,030 U/L,and alkaline phosphatase (ALP) 228 ± 222 U/L.
Acute gall bladder disease caused jaundice in 103 patients(14%). The mean ± SD values in this group were: age 43 ±18 yr, total bilirubin 5.9 ± 3.3 mg/dL, AST 360 ± 405 U/L,
Table 2. Etiology of New-Onset Jaundice (N = 732)
Hepatic Etiology Extra-Hepatic Etiology(N = 406, 55%) (N = 326, 45%)
Decompensation 20.5% Sepsis/abnormal 22%of pre-existing chronic hemodynamicsliver disease
Gilbert’s syndrome 5.6% Gall stone disease 14%Alcoholic hepatitis 16% Hemolysis 2.5%Acute viral liver disease Malignancy
HBV 5% Pancreato-biliary 2.7%HCV 2% Metastatic 3.5%HAV 1%EBV 0.5%HIV 0.3%
DILIAcetaminophen 3.3%HAART 0.4%Valproate 0.1%Metabolife 0.1%
Acute autoimmune hepatitis 0.3%
Percentages reflect proportion of the total cohort.
560 Vuppalanchi et al.
ALT 379 ± 306 U/L, and ALP 304 ± 254 U/L. Nearly halfof them had acute cholecystitis while others had documentedcholedocholithiasis.
In 46 patients (6%), the new-onset jaundice was causedas a result of malignancy; pancreatic or biliary cancer in 20patients (2.7%) and liver metastases in 26 patients (3.5%)(Table 2). The mean ± SD values in this group were: age 55± 14 yr, total bilirubin 11.5 ± 7.0 mg/dL, AST 520 ± 1,187U/L, ALT 224 ± 256 U/L, and ALP 759 ± 675 U/L.
Gilbert’s syndrome was the etiology in 41 patients (6%),and hemolysis caused by Sickle cell anemia caused jaundicein another 18 patients (2.5%). Serum bilirubin in these twogroups of patients was predominantly unconjugated in nature.While patients with Gilbert’s syndrome had normal amino-transferases, patients with sickle cell disease often had mildlyelevated aminotransferases (AST 56 ± 24 U/L, ALT 33 ± 15U/L) suggesting that they may have some undocumented un-derlying liver disease (e.g., iron deposition, vasculopathy).Autoimmune hepatitis causing new-onset jaundice was no-ticed in two patients (0.3%).
The RUCAM score for all the cases of idiosyncratic DILIwas calculated with the data obtained from the chart review tofurther ascertain the causality (Table 3). The RUCAM scoresranged from 6–8, thus qualifying for the category of probablehepatotoxicity.
The 6-wk mortality rate of this cohort was 12.4% (N = 91)and a majority of the deaths were as a result of underlyingsepsis/abnormal hemodynamics (58%) and decompensatedliver disease (28%) (Table 4).
DISCUSSION
Physicians’ perception of common causes of jaundice isprimarily based on their anecdotal experience or publishedepidemiological studies. The studies reporting the commoncauses of jaundice are predominantly European and con-founded by study design, referral bias, ethnic background ofthe study population, research interest, and expertise of thehepatologists at the referral center (2, 4, 5). To our knowl-edge, this is the first study from the United States reportingthe frequency of various etiologies of new-onset jaundice inan unselected patient population. The predominance of the
Table 4. Six-Week Mortality: Total Cohort and Specific Etiologies
Number of NumberPatients (%)
Total cohort 732 91(12.4%)Decompensation of chronic 150 25 (17%)
liver diseaseSepsis or hemodynamic alterations 59 52 (33%)Alcoholic hepatitis 117 9 (8%)DILI 29 4 (14%)
Caucasian and African-American (84%) population in ourstudy cohort portrays many typical urban city populations inthe midwestern United States. The biochemical data acquiredat emergency room visits, hospital admissions to an innercityacademic hospital, and visits to its affiliated primary careclinics minimize any referral bias.
Sepsis or altered hemodynamic state resulting in presumedischemic liver injury appears to be the most common causeof new-onset jaundice (22%). A majority of these patientssuffered from severe burn injuries or had sustained fatal trau-matic wounds. These patients developed jaundice during thehospital stay rather than presenting to hospital with jaundice.The decompensation of pre-existing chronic liver disease andacute alcoholic liver disease were the other common hepaticetiologies for new-onset jaundice accounting for 21% and16% of total cases, respectively (Table 2).
Drug-induced hepatotoxicity is a well-publicized cause ofacute liver disease but its epidemiology is not well studied. Aprospective study conducted by the Acute Liver Failure StudyGroup at several tertiary care centers reported that 13% ofthe cases of acute liver failure resulted from idiosyncraticdrug reaction (Table 5) (8). Because many cases of DILI donot progress to acute liver failure, a pilot study by the samegroup used broader criteria to identify 307 cases of severeliver injury defined as acute hepatic illness of <26 wk witheither bilirubin >10 mg/dL or coagulopathy (INR [interna-tional normalized ratio] >1.5) with bilirubin >4 mg/dL (9).Sixty-one cases (20%) of the severe liver injury were seenresulting from idiosyncratic drug reaction (Table 5). Galenet al. in a retrospective study reported a frequency 0.8% of id-iosyncratic drug-induced hepatitis from a population of 4,039outpatients referred for evaluation of liver disease over a 10-yr period (Table 5) (10). As this study was conducted at areferral center, the true frequency of idiosyncratic DILI re-sulting in jaundice in the Unites States has not been reporteduntil now. Most cases of DILI in our study cohort were as aresult of acetaminophen toxicity (N = 24) and idiosyncraticDILI was the etiology in only five patients (0.7%). Assessingcausality in a retrospective study is usually a challenge asadequate history is frequently lacking. However, in our studymany of the patients with idiosyncratic DILI were hospital-ized and adequately evaluated for other causes of hepatotoxi-city. Their RUCAM score was calculated with the data avail-able from the chart review to further ascertain the causality(Table 3).
The late Hyman Zimmerman observed that elevations intransaminases in combination with jaundice signal seriousliver injury and carry a significant fatality rate. This observa-tion was discussed at the Fogarty International Center Confer-ence on Hepatotoxicity held in 1978 at the National Institutesof Health in Bethesda, Maryland. It was a consensus at thisconference that elevations in liver enzymes (AST or ALTmore than three times the upper limit of normal [ULN] oralkaline phosphatase more than 1.5 times ULN) in combina-tion with an elevated bilirubin (more than three times ULN)
DILI and New-Onset Jaundice 561
Table 3. Peak Biochemical Values in Patients with Idiosyncratic DILI
Peak
Age (Yr) Sex Race Drug RUCAM Score AST (U/L) ALT (U/L) ALP (U/L) Total Bili (mg/dL) Outcome (6 wk)
43 F AA Metabolife 8 3,448 4,700 133 20.3 Alive50 M AA HAART 7 429 307 264 14.9 Alive37 M C HAART 8 1,419 1,891 150 20.2 Alive32 F C HAART 8 78 121 92 3.2 Alive19 M AA Valproate 6 56 58 N/A 3.4 Alive
AST = aspartate aminotransferase; ALT = alanine aminotransferase; ALP = alkaline phosphatase; Total Bili = total bilirubin; AA = African American; C = Caucasian; HAART= highly active antiretroviral therapy; N/A = not available.
Table 5. Historically Reported Frequency of Idiosyncratic DILI in United States
Patient ProportionPopulation Sample Study With Idiosyncratic
Studied Study Design Size Period DILI
Ostapowicz et al. (9) Acute liver failure Multiple referral centers 308 1998–2001 13%Ostapowicz et al. (8) Severe liver injury Multiple referral centers 307 Not reported 20%Galan et al. (10) Referrals for evaluation of acute Tertiary care 4,039 1993–2002 0.8%
and chronic liver disease referral centerCurrent study Total bilirubin >3 mg/dL Community health-care system 732 1999–2003 0.7%
at any time after starting a new drug should be consideredto be a serious liver injury and the implicated drug shouldbe discontinued (11). These criteria are now popularly de-scribed as Hy’s Rule for monitoring drug hepatotoxicity. The14% 6-wk mortality observed in patient’s with DILI in ourstudy cohort is consistent with previously reported mortalityrates associated with Hy’s rule (12, 13). However, no mortal-ity was reported among the five cases of idiosyncratic DILIat 6 wk.
Idiosyncratic DILI is often difficult to diagnose, requiringparticularly thorough history taking. It is likely to be under-diagnosed and therefore might be over-represented in the 46cases excluded from this study. However, these cases weremainly excluded for lack of adequate clinical history andlaboratory workup for reasons unknown to us. Nevertheless,even if 100% of the ineligible cases were attributed to DILI,the proportion of patients with new-onset jaundice as a resultof DILI would only reach 9.8%, and the subset as a resultof idiosyncratic DILI, 6.5%. Additionally, the absence of an-tibiotics as a cause is in striking contrast to the findings ofGalan et al. (10)
In summary, idiosyncratic DILI appears to be a rare causeof new-onset jaundice in the community. In this retrospectivestudy, it was not associated with mortality at 6 wk from thetime of onset of jaundice.
ACKNOWLEDGMENTS
This work was in part supported by NIH grant U01DK065211. The authors would like to thank Ms. EvgeniaTeal of the Regenstrief Institute for Health Care for her as-sistance with data retrieval and management.
STUDY HIGHLIGHTS
What Is Current Knowledge
� Drug-induced liver injury (DILI) is a much publicizedcause of liver disease but its epidemiology has not beenwell studied.
� Few studies from the tertiary care centers that estimatedthe burden of DILI carry significant referral bias.
What Is New Here
� In this study, authors have examined the etiology ofnew-onset jaundice in a large cohort of patients seen ata community hospital system.
� DILI accounted for 4% of patients with new-onsetjaundice. Most cases of DILI were as a result of ac-etaminophen toxicity, with idiosyncratic DILI account-ing for only 0.7% of total cases.
Reprint requests and correspondence: Naga Chalasani, M.D., In-diana University School of Medicine, WD OPW 2005, 1001 West10th Street, Indianapolis, IN 46202.
Received August 28, 2006; accepted October 10, 2006
REFERENCES
1. Whitehead MW, Hainsworth I, Kingham JG. The causes ofobvious jaundice in South West Wales: Perceptions versusreality. Gut 2001;48:409–13.
2. Sgro C, Clinard F, Ouazir K, et al. Incidence of drug-inducedhepatic injuries: A French population-based study. Hepatol-ogy 2002;36:451–5.
562 Vuppalanchi et al.
3. Pasanen P, Pikkarainen P, Alhava E, et al. Value of serumalkaline phosphatase, aminotransferases, gamma-glutamyltransferase, leucine aminopeptidase, and bilirubin in thedistinction between benign and malignant diseases causingjaundice and cholestasis: Results from a prospective study.Scand J Clin Lab Invest 1993;53:35–9.
4. Friis H, Andreasen PB. Drug-induced hepatic injury: Ananalysis of 1100 cases reported to the Danish Committee onAdverse Drug Reactions between 1978 and 1987. J InternMed 1992;232:133–8.
5. Bjornsson E, Ismael S, Nejdet S, et al. Severe jaundice inSweden in the new millennium: Causes, investigations, treat-ment and prognosis. Scand J Gastroenterol 2003;38:86–94.
6. Bach N. The significance of alcoholic liver disease to con-temporary clinical hepatology. Hepatology 1996;24:959–60.
7. Benichou C, Danan G, Flahault A. Causality assessment ofadverse reactions to drugs–II. An original model for vali-dation of drug causality assessment methods: case reportswith positive rechallenge. J Clin Epidemiol 1993;46:1331–6.
8. Ostapowicz G, Samuel G, Larson AM, et al. Identificationof drug-induced liver injury among 307 cases of severeliver injury: A retrospective multi-center study. Hepatology2001;34:454A.
9. Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results ofa prospective study of acute liver failure at 17 tertiary carecenters in the United States. Ann Intern Med 2002;137:947–54.
10. Galan MV, Potts JA, Silverman AL, et al. The burdenof acute nonfulminant drug-induced hepatitis in a UnitedStates tertiary referral center [corrected]. J Clin Gastroen-terol 2005;39:64–7.
11. Vuppalanchi R, Teal E, Chalasani N. Patients with elevatedbaseline liver enzymes do not have higher frequency of hep-atotoxicity from lovastatin than those with normal baselineliver enzymes. Am J Med Sci 2005;329:62–5.
12. Andrade RJ, Lucena MI, Fernandez MC, et al. Drug-inducedliver injury: An analysis of 461 incidences submitted to theSpanish registry over a 10-year period. Gastroenterology2005;129:512–21.
13. Bjornsson E, Olsson R. Outcome and prognostic mark-ers in severe drug-induced liver disease. Hepatology2005;42:481–9.
CONFLICT OF INTEREST
The authors have declared no conflict of interest.