Estimating eliminating survival Nordic · 181 Urinarybladder 20430 8870 14222 24084 67606 190...
Transcript of Estimating eliminating survival Nordic · 181 Urinarybladder 20430 8870 14222 24084 67606 190...

Joumal of Epidemiology and Community Health 1997;51:289-298
Estimating potential savings in cancer deaths byeliminating regional and social class variation incancer survival in the Nordic countries
Paul W Dickman, Robert W Gibberd, Timo Hakulinen
AbstractStudy objectives-To examine equity inthe health care system with regard to can-cer patient care by estimating the levelof systematic regional variation in cancersurvival in the Nordic countries. Spe-cifically, those cancer sites which exhibithigh levels ofsystematic regional variationin survival and hence inequity were iden-tified. Estimating the reduction in cancerdeaths which could be achieved by elim-inating this variation so that everyone re-ceives effective care will provide a readilyinterpretable measure of the amount ofsystematic regional variation. A com-prehensive analysis ofregional variation insurvival has not previously been conductedso appropriate statistical methodologymust be developed.Setting and participants-All those aged0-90 years who had been diagnosed withat least one of 12 common malignant neo-plasms between 1977 and 1992 in Denmark,Finland, Norway, and Sweden.Design-A separate analysis was con-ducted for each country. Regression mod-els for the relative survival ratio were usedto estimate the relative risk ofexcess mor-tality attributable to cancer in each regionafter correcting for age and sex. Anestimate of the amount of systematicregional variation in survival was obtainedby subtracting the estimated expected ran-dom variation from the observed regionalvariation. An estimate was then made ofthe potential reduction in the number ofcancer deaths for 2008-12 if regional vari-ation in survival were eliminated so thateveryone received the same level of effect-ive care.Main results-Between 2008 and 2012, anestimated 2.5% of deaths from cancers inthe 12 sites studied could be prevented byeliminating regional variation in survival.The percentage of potentially avoidabledeaths did not depend on country or sexbut it did depend on cancer site. Therewas no relationship between the level ofregional variation in a given country andthe level of survival. The cancer sites forwhich the greatest percentage savingscould be achieved were melanoma (11%)and cervix uteri (6%). The sites for whichthe highest number of deaths could beprevented were prostate, colon, melan-oma, and breast.
Conclusions-This methodology showed asmall amount of systematic regional vari-ation in cancer survival in the Nordiccountries. The cancer sites with high levelsof regional variation identified are po-tential targets for cancer control pro-grammes.
(J Epidemiol Community Health 1997;51:289-298)
Previous components of the Nordic col-laborative project "Cancer in the Nordic coun-tries in the years 1990, 2000 and 2010" (CiN)have predicted cancer incidence and mortalityup to the year 2010.'2 In the current project weexamine regional differences in survival withinDenmark, Finland, Norway, and Sweden andestimate the potential saving in mortality whichcould be achieved by eliminating systematicregional variation in cancer patient survivalsuch that everyone receives effective care.The analysis of geographic variation is a
popular methodology in health services re-search although the statistical methodology forsuch analyses has not been fully developed."4Most methods have been developed for thestudy of regional variation in rates, and havebeen applied to hospital admission rates, sur-gery rates, and in the field of cancer epi-demiology, incidence, and mortality rates.5-9The most appropriate methods for our pur-poses have focused on answering the question:Is there more variation than can be explainedby random factors and, if so, what is the sizeofthe systematic variation?5 We have developeda similar methodology for studying regionalvariation in survival, although the methodologyis complicated by the fact that survival is math-ematically more difficult to estimate than in-cidence or mortality rates.
After estimating the level of systematicregional variation in cancer survival, the po-tential reduction in cancer mortality whichcould be achieved in the years 2008-12 byeliminating this variation is estimated. Anyoverall reduction in mortality is brought aboutby improving the survival in those regions withlow survival such that survival rates in all re-gions are equivalent to what would be expectedif everyone received the same level of effectivecare. This reduction in mortality is additionalto any reduction (or increase) in mortality dueto trends in survival brought about by otherfactors.The Nordic countries consist of Denmark,
Finland, Iceland, Norway, and Sweden. Thepopulation of Iceland (250 000) is too small to
Departnent of CancerEpidemiology,Radiumbemmet,Karolinska Hospital,S-171 76 Stockholm,SwedenP W Dickman
Department ofStatistics, Universityof Newcastle, NSW2308, AustraliaR W Gibberd
Finnish CancerRegistry, Liisankatu21B, 00170 Helsinki,FinlandT Hakulinen
Correspondence to:Mr P Dickman, Departmentof Statistics, University ofNewcastle, Newcastle, NewSouth Wales 2308, Australia.Accepted for publicationSeptember 1996.
289
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Dickman, Gibberd, Hakulinen
facilitate a regional analysis so this study isrestricted to the other four countries. We havetaken the liberty of referring to these four coun-tries as the Nordic countries.
Cancer care refers to that component ofcancer control pertinent to the period followingthe onset of cancer. It consists of three maincomponents diagnosis, treatment, and re-
habilitation. Cancer control is a more generalterm which also encompasses, among otherareas, primary prevention. Cancer care is de-fined as being effective if it accomplishes itspurpose, which is achieving the best possiblepatient survival, given the existing state ofknowledge. The survival time for a cancer
patient is defined as the elapsed time betweendiagnosis and death and is the principal meas-
ure of the effectiveness of cancer care. Effectivecancer care implies effective diagnosis, effectivetreatment, and effective rehabilitation (in termsof survival time).
Equity has been regarded as one of the keyindicators of the quality of health care,'0 al-though not everyone agrees on the definitionsof equity and health."-'5 Equity has beenequated to access to health care, the allocationof resources, the use of health services, andto per capita expenditure on health care. Analternative to these resource based measures ofequity is to use an outcome based measure ofequity, namely patient survival.'6 Using thisdefinition, inequity stems from differences inthe effectiveness of cancer care, where effect-iveness is measured by patient survival.Outcome based equity usually implies re-
source based inequity since population sub-groups will require disparate expenditure ofresources in order to achieve the same outcome.
In many situations, outcome based equity isan unreachable goal since not everyone can beguaranteed the same level of good health (egthose with congenital defects). It is for thisreason that most definitions of equity are basedon the principle of equality of access ratherthan equality of "health". An outcome basedmeasure, however, is appropriate for cancer
care since we can control for general mortalityand it is not unreasonable to aim for nationwideequality of survival (within age/sex/site groups)following a diagnosis of cancer. It still may not
be possible to achieve complete equity ofcancersurvival within each age/sex/site group sincefurther subgroups can usually be identified(based on, for example, smoking habits or eth-nic origin) which are subject to dissimilar gen-
eral mortality. Nevertheless, a target ofnationwide equality of survival (within age/sex/site groups) following a diagnosis of cancer
provides a useful and realistic baseline fromwhich to assess equity of cancer care.
If there is a state of equity, there should beno systematic differences in cancer survivalbetween patient groups (within each age/sex/site) defined by social class or place of res-
idence. Inferences can therefore be made aboutequity in a health care system by comparingcancer survival across geographic regions andsocial classes. Karjalainen" '7 lists three factorswhich may account for observed differences incancer patient survival: inequity, confounding
variables, and random variation. The aim of thisanalysis is to estimate the amount of systematicvariation in regional survival by controlling forconfounding variables and estimating the levelof random variation. The amount of systematicvariation in regional survival will provide ameasure of the level of inequity in the healthcare system for cancer patients and can high-light areas where there is potential for cancercontrol programmes to be effective.
MethodsCase specific data were obtained from the cent-ral cancer registry in each country for casesdiagnosed from 1977 until the most recent yearavailable, which was 1991 for Denmark andSweden and 1992 for Finland and Norway.Cases were followed up for deaths to the endof 1991 in Denmark and Sweden, 1992 inNorway, and 1993 in Finland. Notification ofnew cancer cases is compulsory in each countryand the data maintained by each of these popu-lation based, nationwide registries is consideredto be of the highest quality.2 Collaborative pro-jects and annual meetings of the Nordic cancerregistries ensure that data collection and followup procedures are comparable between theNordic countries.Each cancer registry also supplied general
population mortality rates, obtained from theircentral statistical offices, which were requiredfor the analysis of relative survival. For Finland,population mortality rates were also providedfor each of 12 counties and each of six socialclasses in addition to the nationwide rates. TheOncologic Centre in Umea, Sweden, providedstandardised mortality ratios for each county,sex, and age group which enabled calculationof region specific population mortality rates forSweden. Incidence and mortality rates wereobtained from computer disks accompanyingthe CiN la' and lb2 publications, as wereage/sex population figures for 1983-87 andpredictions for 2008-12. For Finland, in-formation on social class was available for eachcase and was used to analyse social class differ-ences in survival in addition to the analysis ofregional differences. Social class informationwas not available for the present study for anyof the other three countries. Region specificmortality data were not available for Norwayand Denmark.
SITESThe 12 cancer sites, their corresponding ICD-7 codes, and the number of incident cases foreach country are given in table 1. The siteswere chosen so as to obtain a range of survivalrates and potential for successful diagnosis andtreatment. Sites with a high incidence wereprimarily chosen in order to reliably estimatethe region specific survival. The 12 chosen sitesaccount for 63% of the total number of cancerdeaths during 2008-12 predicted by CiN lb.2
290
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Regional variation in cancer survival
Table 1 Number of cases included in the analysis for each cancer site
ICD-7 code Site Denmark Finland Nonvay Sweden All
151 Stomach 11 261 18036 14394 23278 66969153 Colon 27 590 13 523 24 007 39 118 104 238154 Rectum 15 924 9969 12 959 23 485 62 337161 Larynx (male) 2897 1926 1777 2765 9365162-163 Lung 41 371 33 899 21602 34 891 131 763170 Breast (female) 39224 32545 27735 65857 165361171 Cervix uteri 8511 2746 5875 7946 25 078172 Corpus uteri 9234 7692 6262 13 859 37 047177 Prostate 18 916 18 373 26 771 60 156 124 216180 Kidney 8279 7799 7297 15 274 38 649181 Urinary bladder 20 430 8870 14 222 24 084 67 606190 Melanoma of skin 8689 6342 10 492 16 357 41 880
Total 212 326 161 720 173 393 327 070 874 509
Table 2 Number of cases excluded from the analysis
Counny No Age Autopsy DCO* Previous Total % ofregion >9Oy tumourt excluded total
Denmark 8 2506 11740 2400 887 17 541 7.6Finland 2 1285 4201 1092 824 7404 4.4Norway 0 2082 1709 1334 2081 7206 4.0Sweden 11 4375 18491 Ot 3939 26816 7.6
* DCO: infornation available from death certificate only.t Excluded because of a previous primary tumour in the same site.t DCO cases already excluded by the cancer registry.
REGIONSThe regions had to be large enough to allowaccurate estimation of survival, yet smallenough to reflect regional differences. Regionswere defined using pre-existing administrativeborders and consisted of22 health care districtsin Finland, 24 counties (lan) in Sweden, 16counties (amter) in Denmark, and 19 counties(fylker) in Norway. The average regional popu-lations were 226, 359, 321, and 226 thousand,respectively. It could be argued that it is sci-entifically more valid to define the regions suchthat they are homogeneous with respect todemographic or geographic characteristicswhich are of direct interest (such as socio-economic status or some measure of access tohealth care). However, any future action whichmay be taken to reduce regional variation willrequire action by the regional health au-thorities, thus making it perhaps more ap-propriate to use these administratively definedregions.
EXCLUSIONSSome cases were excluded from the analysisin order to obtain a more uniform material,primarily across regions within each country,but also across the different countries (table 2).Reasons for exclusion were region of residenceinformation not available, age at diagnosisgreater than 90 years, diagnosis first made atautopsy, and information available from deathcertificate only (DCO). The survival time willbe zero when the diagnosis is first made atautopsy or on the basis of death certificate only.When a registry receives a death notification
for a patient (or tumour) which was not pre-viously known to the registry, the registry con-tacts the appropriate hospital or physician in anattempt to ascertain the true date of diagnosis.Sometimes it is not possible to ascertain thetrue date of diagnosis and it is these caseswhich were excluded. When multiple primarytumours were registered in the same site for
the same person, only information relating tothe first tumour was included in the analysis.Multiple primary tumours in different siteswere included independently in each site, pro-vided other selection criteria were met.For the Danish material, 5473 cases were
excluded due to the diagnosis being first madeat autopsy. An additional 6267 cases whereonly information from the autopsy report wasavailable were excluded and are also reportedin this category. The true diagnosis date forthese 6267 cases may have been earlier butno additional information is available. Theregional distribution ofthe excluded cases fromeach country were examined for systematicpatterns which may introduce biases. The ana-lysis was also repeated without excluding anycases as a means of testing the sensitivity ofthe results to the exclusions.
Statistical methodsThe methodology developed for the currentstudy of regional variation in survival can bedescribed in three broad steps:
* Step 1-estimate survival for each region bymodelling relative survival as a function ofrelevant predictor variables (age, sex, andregion) for each cancer site
* Step 2-estimate the amount of systematic(as opposed to random) regional variationin survival
* Step 3-estimate the reduction in mortalitywhich could be achieved if this variation wereeliminated such that everyone receives thesame level of effective care
Statistical models for relative survival ana-lysis (step 1) are reasonably well developed,although little research has been conductedon methods for studying regional variation insurvival (step 2). We have developed methodsfor examining regional variation in survivalwhich have been applied in the current study.
STEP 1: MODEL FITTINGThe analysis of survival from population basedcancer registries with long term follow up isoften performed using relative survival ana-lysis. 18-20 We used the regression model de-veloped by Hakulinen and Tenkanen,2' whichmodels the total mortality (number of deathsdivided by the person-time at risk) for personsdiagnosed with cancer, ,u, as the sum of theknown baseline mortality, p*, and the excessmortality due to a diagnosis of cancer, v. Thatis,
(1)
The subscripts indicate that the excess mor-tality of the patients (and hence their totalmortality) depends on region (r), age (i), sex(s), and follow up interval (j). The baselinemortality depends on age, sex, and possiblyregion. The model was fitted individually toeach of the 12 cancer sites in each of the fourcountries using the predictor variables region,
291
Xw p mi,+ Vw
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Dickman, Gibberd, Hakulinen
age, sex, and an age by follow up interactionterm (for the first five years of follow up only).The age variable contained three levels andwas defined separately for each site. Each regionwas represented by a dummy variable in theregression model and an estimate ofthe relativerisk of excess mortality due to cancer was ob-tained for each region. The age by follow upinteraction term was required in order to obtainan acceptable fit to the data and indicates thatthe age specific hazards are non-proportionalfor the first five years of follow up.The excess mortality component is assumed
to be a multiplicative function ofthe covariates,such that
Vi=ep(B reg+ #B age + # sex+ fl ige.ful)) 2v,,:--. e p l i(2)
The individual model parameters (the fl's)are interpreted as log relative risks of excessmortality due to cancer. As such, the relativerisk of excess mortality due to cancer for res-idents of region r is given by RRr= exp(flr),where the superscript reg has been omitted forsimplicity. Mortality after t years of follow up,ji (t), is directly related to the survival rateS(t) through S(t) = exp [ -p (t) ]. The annual(interval specific) relative survival ratio for fol-low up interval j (and other covariates at levelsr, i, and s) is given by
r,jsj= exp( V,i,j) (3)
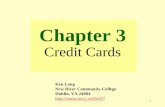
Estimated regioR specific relative risks forSweden, given by RR,= exp(,Br), where fr is theestimate for frs are presented in figure 1 as anexample. A relative risk of 1.4 for a given regionindicates that the risk ofdeath due to the cancer
in question is 1.4 times higher in that regionthan it is according to the average of all regionspecific excess mortalities. Each relative riskrepresents the ratio of the risks of cancer mor-tality after correcting for mortality due to othercauses.
EXPECTED SURVIVALThe relative survival ratio (also called the rel-ative survival rate) at time t is the ratio of theobserved survival of the cases to the expectedsurvival for a comparable group in the generalpopulation. That is, r(t) = S(t)/S*(t), whereS(t)=exp[-,u(t)] and S*(t)=exp[-,u*(t)].Hence for the current model (1), we have r(t) =exp[-,u(t)+u*(t)]=exp[-v(t)], where r(t),,u(t), ,u*(t), and v(t) are assumed to be constantfor all values of t within each annual follow upintervalj and subscripts for the other covariatesare omitted.When conducting a relative survival analysis,
it is standard practice to estimate the expectedsurvival rate S*(t) using age/sex specific mor-tality tables for the entire (nationwide) popu-lation. We would not expect the baselinemortality to be identical in all regions, so usingnationwide life tables to estimate the expectedsurvival will create bias. This bias is not ofgreat concern when analysing nationwide databut may be important when we wish to estimatesurvival in individual regions or social classgroups.
In order to study the effect of this bias, wecalculated expected survival for the Finnishand Swedish material using region specificpopulation life tables. In addition, we also es-timated the expected survival for Finland using
0
0
0
0 0 0
0 0° -0
0~~~ ~ ~ l ri~ ~
0 ~~~~~~~~~~0
8
0
0
-
RectumLarynx
Lung CervixBreast
Cancer
CorpusProstate
KidneyBladder
Melanoma
Figure 1 Region specific estimates of the relative risks of excess mortality due to cancer in relation to site for 24 regionsin Sweden, 1977-91. Estimates are from the regression model controlling for age, sex follow up, and an age* follow upinteraction.
1.8 r
1.6 H
1.4 H
1.2 e
1.0o
crccU)
EC,,wn
0.8
0.6 K
0.4 H
0.2Stomach
Colon
292
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Regional variation in cancer survival
social class specific life tables. The differencesbetween these three methods of estimating theexpected survival and the effect on the finalresults were studied. For the Norwegian andDanish material, we had no option other thanusing nationwide life tables to calculate ex-pected survival. The additional analyses forFinland and Sweden were used to assess themagnitude of the bias due to using nationwidelife tables.
STEP 2: ESTIMATING THE SYSTEMATICCOMPONENT OF REGIONAL VARIATIONThe estimates presented in figure 1 are un-biased estimates of the effect of living in eachregion and, like all estimates, are subject torandom variation. For any given cancer site infigure 1, it is possible that all of the observedvariation among the region specific estimatesis due to random variation, or it may be dueto a combination of random variation and sys-tematic differences in relative survival betweenthe regions. It is possible to estimate the mag-nitude ofthe expected random variation, whichdepends on the number of cases and the sur-vival rate. We developed an estimator V toestimate the magnitude of the systematicregional variation in survival by subtracting theestimated random variation from the observedvariation in the estimates bl, ..., b, An ap-pendix contains mathematical details of V,which is an estimator for
p_ I (flr wf)2r=l
the variance of the ensemble of true regionaleffects. The value of Vwill be zero (or negative)if no systematic regional variation in survivalexists and will increase in magnitude as thelevel of systematic variation increases.As was noted earlier, the estimated region
specific relative risks presented in figure 1 aresubject to both systematic and random vari-ation. It is possible to calculate new estimates,so called second stage estimates (or shrinkageestimates), which differ solely due to systematicregional variation. That is, the estimates areadjusted to remove the effect of random vari-ation. Second stage estimates were calculatedby shrinking the crude relative risks towardsthe mean value (RR= 1) such that the amountof variation in the second stage estimates wasequal to the estimated level of systematicregional variation in survival estimated by V Alinear shrinkage of the form b* = Obr was used,where br is the original (crude) estimate and b*rthe second stage estimate for region r= 1, . . .,p. Since var(b*) =02 var(b) we have 0 =(VIS2),where S2 is the sample variance of the ensembleof parameter estimates. If Vs< 0 then b* = 0 forall regions, otherwise b* =- br is the secondstage estimate of fir and exp(b*) is the secondstage estimate of the relative risk.
STEP 3: POTENTIAL MORTALITY SAVINGSWe can use V to identify those cancer sites thatexhibit systematic regional variation (the larger
the value of V, the larger the systematic vari-ation), but it is difficult to grasp the practicalimplications ofa given value of V By estimatingthe number of deaths "saved" by eliminatingany regional variation in survival, we are ableto present results with a more concrete in-terpretation. The number of cancer deaths(deaths attributable to cancer) in an interval isdefined as the number of deaths in the intervalminus the number of expected deaths ac-cording to mortality in a comparable group inthe general population. We define the numberof deaths "saved" by removing regional vari-ation in survival as the reduction in the numberof cancer deaths during the first 10 years offollow up (15 years for breast cancer). Thelonger time frame was used for breast cancerbecause a significant number of breast cancerdeaths occur in the period 10-15 years afterdiagnosis.24Applying equations (2) and (3) to the es-
timated parameters from the regression model,it is a simple matter to estimate the relativesurvival ratio and the predicted number ofdeaths due to cancer for any combination ofage, sex, and follow up year. The number ofcancer deaths across all regions in follow upinterval j (and given levels of age and sex) isthen defined as the number of deaths in theinterval minus the number of expected deathsaccording to mortality in a comparable groupin the general population and is given by
(4)
where rj is the (model based) interval specificannual relative survival ratio (for given levelsof age and sex), lj is the number alive at thestart of follow up interval j, and p*' is theexpected survival probability, taken from age/sex specific population life tables.The number of cancer deaths was calculated
for each follow up year and summed across thefirst 10 follow up years (15 for breast cancer)to obtain an estimate of the total number ofcancer deaths for each country, age group, andsex. The number of cancer deaths was thenrecalculated under the assumption that anyexisting systematic regional variations wereeliminated and relative survival in all regionswas equivalent to what would be expected ifeveryone received the same level of effectivecare. The percentage difference between thesetwo quantities is an estimate of the percentageof cancer deaths potentially "savable" by re-moving systematic regional variation in sur-vival. A percentage equal to 0.0% indicates thatthere was no evidence of systematic regionalvariation in survival so no deaths can be savedby eliminating such variation. A percentage of,say, 1.6% indicates that eliminating regionalvariation in survival would save an estimated1.6% of cancer deaths. In calculating thesepercentages, it was assumed that everyonecould be followed up for at least 10 years (15years for breast cancer) in order to eliminateany potential bias due to differential withdrawalpatterns.
293
C.= lp'. (1 rj)1 7 1
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Dickman, Gibberd, Hakulinen
The excess mortality under the assumptionthat everyone receives the same level of effectivecare (no regional variation in survival) is givenby
v-Kew .vj for j=1, 5new= sVrisj=(5
nsfor j>5(5
where vn5 is the model based estimate of theexcess cancer mortality for age i, sex s, andfollow up interval j averaged over all regionsand RRECw is the estimated relative risk re-flecting the reduction in excess mortality wewould observe if there was no regional variationin survival and everyone received the same levelof effective care. Estimation of vn,3 is carriedout by fitting a model without region. Therewas no evidence of regional variation in survivalin follow up intervals 6-15 so we assumedthe excess mortality due to cancer would beunchanged after the fifth year of follow up.The central issue in estimating the per-
centage of potentially savable deaths is how toestimate RRRflCw =exp(/#new). Simply assumingthat every region will attain the same relativesurvival ratio as the best (or even second best)region is not appropriate since these estimatesare subject to random variation. The estimateV represents the estimated variance of the en-semble of region specific parameters (log rel-ative risks). If we assume that this ensemble isa sample from a normal distribution, then 95%of the parameters should lie in the interval(-1.961/[V], 1.961/[V]) and hence 95%of the relative risks in the interval(exp(- 1.96E/[V]), exp(1.96,/[V])). We usedRlEeW=exp(-1.96,/[V]) as the relative riskestimate corresponding to effective treatmentand assumed that all regions would obtainthis level if regional variation in survival wereeliminated.The percentages ofpotentially savable cancer
deaths were then applied to the CiN lb2 pre-dictions of the number of cancer deaths forthe period 2008-12 in order to estimate thenumber of potentially savable deaths during2008-12. This time period was used sinceincidence and mortality predictions have pre-viously been made for it.' 2
In the CiN lb project, predictions of thenumbers of cancer deaths for the period2008-12 were adjusted for time trends in excessmortality where appropriate. If these trends areattributable to trends in the level of regionalvariation, our method for estimating the num-ber of savable deaths may be erroneous, sincethe CiN lb prediction of the number of cancerdeaths during 2008-12 has already been (atleast partially) adjusted for changes in the levelof regional variation. To investigate if this wasa problem we instead predicted the numberof cancer deaths during 2008-12 under theassumption that excess mortality rates re-mained unchanged over time while making useof previously predicted changes in incidencerates and population distribution. The resultsobtained were very similar for the two methodsso we decided to use the CiN lb predictionsfor the number of deaths during 2008-12 since
the results obtained from this method have amore straightforward interpretation and weremore relevant to the CiN project.
SOCIAL CLASS VARIATIONCancer survival for many sites in Finland hasbeen shown to depend on social class.2526 Eachcase in the Finnish material contained a meas-ure of social class, based on occupational class,obtained from the 1970 population census byrecord linkage using the unique personal iden-tification number allocated since 1967 to allFinnish residents. The social class variable con-tained six levels as defined by Valkonen et al;27namely professional and higher administration,lower administration, skilled workers, unskilledworkers, farmers, and others. These social classcategories were also used to construct the socialclass specific population life tables for Finland.The aim of the social class analysis was to
estimate the potential mortality savings ifevery-one had the same survival as the highest socialclass (professional and higher administration).The analysis proceeded identically to theregional analysis up to the stage where equation(5) was applied to estimate the excess cancermortality under the assumption that every re-gion received the same level of effective care(no regional variation in survival). The nextstep in the social class analysis was morestraightforward, we re-estimated the numberof deaths under the assumption that everyonehad the same relative survival as the highestsocial class and estimated the potential savingsin deaths under this assumption.
ResultsEXPECTED MORTALITYThere were small differences in the estimatedrelative survival ratios (RSRs) calculated usingthe three different baseline mortality tables (na-tionwide, region specific, and social class spe-cific) for calculating expected mortality. Thesedifferences were not large enough to causeconcern about using nationwide life tables forcalculating expected survival. For example,breast cancer is more common in the uppersocial classes so we would expect the estimatedRSR for breast cancer using the social class lifetable to be less than the RSR estimated usingthe general life table. The five year relativesurvival ratio for all 14 216 breast cancer casesin Finland was 0.744 using the region specificlife table, 0.743 using the social class specificlife table, and 0.745 using the general popu-lation life table. The corresponding RSRs forthe 1439 cases diagnosed in the highest socialclass were 0.797, 0.786, and 0.797, re-spectively. These differences due to usingdifferent population life tables were minorwhen compared to the differences in RSRsbetween the regions or between the socialclasses. Relative survival ratios for all breastcancer cases (not adjusted for age and sex)ranged from 0.70 to 0.80 across the socialclasses and from 0.69 to 0.81 across the regions.We therefore had no serious concerns in using
294
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Regional variation in cancer survival
1.8 r0 Crude estimate. Shrunken estimate
0
0
0
0. 0 0:o00 °° 0
- 2 l @ W g 0 Q1: ~Os:*
IStomach
ColonRectum
LarynxLung Cervix
Breast
Cancer
CorpusProstate
KidneyBladder
Melanoma
Figure 2: Crude and shrunken region specific estimates of the relative risk of excess mortality due to cancer in relation tosite for 24 regions in Sweden, 1977-91. Estimates are from the regression model controlling for age, sex, follow up, andan age* follow up interaction. (Values of exp(- 1.961[V]) and exp(l. 961/[V]) are represented by *.)
the general population life tables to estimaterelative survival for regions and social classgroups within each country.
REGIONAL VARIATIONDetailed results for Sweden are presented infigure 2 and table 3. The open circles (0) infigure 2 represent the crude estimates of therelative risks of excess mortality due to cancer
and are identical to those presented in figure1. The closed circles (0) represent the secondstage estimates of the relative risks, shrunkensuch that the amount of variation in theseestimates is equal to the estimated level ofsystematic regional variation in survival es-
timated by V The estimated numbers of saveddeaths are calculated under the assumptionthat on removing systematic regional variationin survival, all regions will have the same
Table 3 Significance of the region term in the regression model, variation in the crudeestimate (sD), estimated V total cancer deaths (CiN lb prediction2), and number andpercentage ofpotentially savable cancer deaths in Sweden, 2008-12 due to removingregzonal variation in survival
Site Pt s2 V Total Savable %deaths deaths
Melanoma 0.00 731 507 2317 408 17.6Prostate 0.00 141 105 12 449 390 3.1Colon 0.00 91 66 7699 382 5.0Breast 0.00 96 46 10 809 284 2.6Lung, trachea 0.00 57 37 16 576 249 1.5Urinary bladder 0.02 130 38 4457 149 3.3Rectum 0.03 59 20 5053 127 2.5Stomach 0.00 28 17 5385 74 1.4Corpus uteri 0.00 504 244 1401 16 1.1Larynx 0.19 610 -486 479 0 0.0Cervix uteri 0.60 166 -42 795 0 0.0Kidney 0.71 34 -17 3980 0 0.0Total 71 400 2079 2.9
t p value is based on comparing the change in deviance on removing the region term from themodel to a %2 distribution with 23 df.
(effective care) relative risk, equal to RR,W =exp(- 1.96,1[V]), which is represented by thelower of the two stars in figure 2.There was no evidence of systematic regional
variation in survival for cancers of the larynx,cervix, and kidney as indicated by a negativevalue of V The second stage estimates of therelative risks for these sites are therefore allequal to one (fig 2). Cancer of the larynxinitially appeared to exhibit the highest level ofregional variation in survival, but this was
shown to be consistent with (or even less than)what we would expect due to random variation.
Systematic regional variation in cancer sur-
vival existed in each of the countries studied,although the level of variation differed ac-
cording to site. All countries contained at leastone site where there was no evidence of sys-tematic regional variation. There were onlyminor differences in the results for males andfemales. Eliminating regional variation in sur-
vival in all countries would save an estimated5271 (2.5%) cancer deaths in the 12 study sitesduring the five year period 2008-12 (table 4).The corresponding number ofdeaths was 1282(2.1 %) for Denmark, 1185 (2.9%) for Finland,724 (1.9%) for Norway, and 2079 (2.9%) forSweden.The sites in which the highest number of
deaths could be saved are prostate, colon,melanoma, and breast (table 4). The largestpercentage savings could be achieved formelanoma (11%) and cervix uteri (6%). Al-though the total percentage of savable deathswas similar for each country, there were differ-ences between the countries within each site.No one country, however, was systematicallyhigher or lower than the others. The differences
1.6 F-
1.4 H
1.2 Ic:
V
a)
E
w
1.0
0.8
0.6 [
0.4 [
0.2
295
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Dickman, Gibberd, Hakulinen
Table 4 Total cancer deaths (CiN lb prediction2) andnumber and percentage ofpotentially savable cancerdeaths during 2008-12 due to removing regional variationin survival (all countries)
Site Total Savable %deaths deaths
Prostate 29 510 961 3.3Colon 24 331 846 3.5Melanoma 6132 709 11.6Breast 32 011 708 2.2Lung, trachea 59 285 535 0.9Rectum 14 450 483 3.3Urinary bladder 12 465 409 3.3Stomach 15 713 210 1.3Cervix uteri 2255 137 6.1Corpus uteri 3920 120 3.1Larynx 1830 80 4.4Kidney 11 344 73 0.6Total 213 246 5271 2.5
Table S Colon cancer: number (%/6) ofpotentially savablecancer deaths during 2008-12 due to removing regionalvariation in survival
Country Savable deaths
Males Females
Denmark 101 (2.9) 151 (3.8)Finland 84 (4.4) 96 (4.6)Norway 13 (0.5) 18 (0.7)Sweden 166 (4.4) 217 (5.5)Total 363 (3.15) 482 (3.8)
Table 6 Number and percentage ofpotentially savablecancer deaths during 2008-12 obtained by eliminatingregional and social class variation in cancer survival inFinland
Site Region Social class
Savable % Savable %deaths deaths
Stomach 88 2.0 167 3.9Colon 180 4.5 101 2.5Rectum 137 6.5 138 6.5Larynx 5 1.8 27 8.7Lung, trachea 71 0.6 0 0Breast 187 2.7 248 3.5Cervix uteri 16 9.1 21 11.6Corpus uteri 30 3.5 147 17.5Prostate 173 3.3 57 1.1Kidney 0 0.0 78 2.6Urinary bladder 65 4.3 137 9.0Melanoma 231 24.3 95 10.1Total 1185 2.9 1217 3.0
between countries for colon cancer (table 5)are shown as an example. A complete set ofresults is available from the authors upon re-
quest.
SOCIAL CLASS VARIATION
Eliminating social class variation in Finlandwill save an estimated 2.9% of cancer deathsduring 2008-12. The savings are similar tothose obtainable by eliminating regional vari-ation, with the exceptions being cancer of thecorpus uteri and melanoma (table 6). We wouldexpect the results to be somewhat similar sincethere is an association between social class andregion of residence. For melanoma there are
greater differences in survival between regionsthan can be ascribed to social class differencesand for corpus uteri the opposite is true. Thisimplies cancer control strategies are importantfor melanoma at the regional level, while cancer
of the corpus uteri requires strategies aimed atlower social classes
DiscussionThe study objective was to examine equity inthe health system by estimating the magnitudeof systematic regional and social class variationin cancer survival. The results indicate thatsystematic regional variation (and hence in-equity) exists in each of the countries studied.Results have been presented primarily in termsof the number of cancer deaths which couldbe saved by removing such variation. It isunlikely that regional variation in survival willbe eliminated in the near future such thatall regions obtain the "effective care"" relativesurvival ratio assumed in the calculations. Thisis not to say, however, that the assumed "effect-ive care" relative survival ratio is an un-reasonable goal, since it has already beenachieved by some regions for every site. Theestimated number of savable deaths provides aready method of quantifying the amount ofsystematic variation, thereby enabling iden-tification of those sites where cancer controlprogrammes may be most effective.Note that we are not concerned with high-
lighting individual regions with high or lowsurvival, but rather in finding the magnitudeof the systematic variation in survival across allregions. It is for this reason that individualregions have not been identified in figure 1. Itis possible to assess the statistical significanceof the regional variation using the change indeviance when the region term is omitted fromthe regression model.23 The regional effect isalmost always significant due to the large num-ber of regions and the large sample size so welearn little from this test (table 3). The level ofstatistical significance is dependent on samplesize so cannot be used to rank the sites in termsof the level of systematic regional variation, ascan be done with the statistic VThere was a weak association between the
relative survival ratio and the amount ofregional variation in the 12 sites-sites withhigh relative survival generally had higher levelsof regional variation. We could not, however,find any systematic pattern to explain whythe level of regional variation differed betweencountries within each site. It may have beenthought that, within a given site, the countrywith the highest survival may have a higherlevel of systematic regional variation but thiswas not the case. There was no associationbetween the level of survival and the level ofregional variation for the four countries withineach site.
Potential bias due to regional differences inlead time was minimised by calculating thenumber of saved deaths from life tables cov-ering long follow up intervals (10 or 15 years).This long follow up will not, however, over-come potential problems due to differentialover diagnosis. If a particular cancer were, forexample, over diagnosed in the higher socialclasses, these social classes would exhibit ahigher incidence due to the over diagnosis andsuperior survival due to increased lead time.28It would not be possible to raise the survivalof the entire population to this level of survivalsince the level is somewhat artificial.
296
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Regional variation in cancer survival
Cases were excluded from the analysis ifthe diagnosis was first made at autopsy or ifinformation was available from DCO. DCOcases are not included in data maintained bythe Swedish cancer registry so were excludedfrom all data in order to maintain com-parability. The effect of DCO cases on survivalis not well defined and requires an under-standing ofthe mechanism by which these casesare generated.29 It is generally accepted that ifthe true diagnosis dates of all DCO cases wereknown, the survival time of these cases wouldbe considerably less than that of the "non-DCO" cases. Pollock and Vickers30 showed thisempirically by tracing the true diagnosis datesofDCO registered cases in south east England.The percentage of DCO cases in a given
region depends upon the effectiveness of diag-nostic, detection, and reporting procedures andthe effectiveness ofretrospective follow up (alsocalled follow back) at the cancer registry. Re-gions with ineffective diagnostic, reporting, andretrospective follow up systems will generallyhave a higher proportion of DCO and autopsycases (which have zero survival time) and acorrespondingly lower proportion of cases withlow survival times. Survival rates for such re-gions will be overestimated (compared to sur-vival rates for other regions) if DCO andautopsy cases are excluded but underestimatedif these cases are included in the analysis. Themain issue, therefore, is not whether DCO andautopsy cases are included or excluded froman analysis but whether these cases are evenlydistributed across regions. Examination of theregional distribution ofDCO and autopsy casesshowed no evidence of regional heterogeneity.To test further the effect of excluding thesecases, the data were analysed without ex-clusions (apart from those cases where regionof residence was not known). The estimatedlevel of regional variation did not depend onwhether or not cases were excluded. Therewere differences in the DCO rates between thefour countries (table 2) although this will notaffect the results since the analysis was con-ducted separately for each country.
Neither stage of disease at diagnosis nor yearof diagnosis were included in the regressionmodel. Stage is, of course, an important pre-dictor of survival for all cancers, but it is not,however, justifiable to adjust survival rates forstage if the aim is to study the effect of thehealth care system on cancer survival.22 If weassume that stage depends mainly on diagnosticdelay, stage is not a confounding factor butrather an outcome variable of interest (i.e. achain in the causal link).
Year of diagnosis is a predictor of survivalfor many cancers but the amount of regionalvariation in survival is not heavily dependent onyear of diagnosis. We fitted models containingpredictor variables for year of diagnosis (twolevels) and a year of diagnosis by region inter-action term to all 12 sites for Finland andSweden. As expected, year of diagnosis wasstatistically significant for nine of the 12 sitesfor both countries. It was not statistically sig-nificant for cancers of the larynx, lung, cervixuteri (Sweden), and corpus uteri (Finland).
The year by region interaction was significantin four of the 12 sites for each country, namelycancers of the stomach, colon, prostate, andkidney for Finland and cancers of the larynx,lung, female breast, and prostate for Sweden.Including these additional terms in the modelhad little effect of the estimates of regionalvariation, even for the sites where the yearby region interaction term was significant. Wedecided to report the results using models with-out year of diagnosis as we wanted to minimisethe number of strata in order to estimate theregional differences as efficiently as possible.
It must be noted that although the lack ofregional variation in survival for a given cancersite is a positive indicator, it does not meanthat survival cannot be improved. It is quitepossible for a given country to have the lowestamount of regional variation in survival com-pared to other countries yet have the worstsurvival, or vice versa. The presence of regionalvariation is an indicator of possible inequity,which points towards a potential for im-provement in survival. The absence of regionalvariation does not necessarily preclude the pos-sibility of improving survival, but it may bemore effective to initially focus on those cancerswhere regional variation exists.The Nordic countries offer unique op-
portunities for conducting this type of researchdue to the high quality of the cancer registrydata and the existence of civil registration sys-tems which enable linking ofthe cancer registrydatabase to obtain individual patient level in-formation on education, occupation, and socialclass. This makes the Nordic countries an idealplatform for developing and testing the currentmethodology. The Nordic countries are jus-tifiably proud of their health care systems, in-cluding the access to and quality of careavailable to all inhabitants. One concern at thestart of this study was that we would not findany regional variation and would not be ableto test the methodology properly, but this hasnot been the case.The ability to study regional and social class
variation in survival will greatly facilitate theevaluation of cancer control. The results fromthis study enable the identification of siteswhere variation, and hence possible inequityexists. These sites should be further studied inan effort to understand the underlying causesof the variation, followed by cancer controlprogrammes to reduce the variation. Themethodology developed for use in this studycan be applied to future data in order to studychanges in the level of regional variation overtime.
This research was supported in part by the Swedish CancerFoundation and the Nordic Cancer Union CiN project. We aremost grateful to the staff of the Nordic cancer registries forsupply of the data and comments on the methodology. DrMike Kenward contributed to the discussion of the statisticalmethodology and wrote a GWM macro used in the study.We wish to thank the anonymous referees, whose commentssubstantially improved the paper.
1 Engeland A, Haldorsen T, Tretli S, et al. Prediction ofcancer incidence in the Nordic countries up to the years2000 and 2010. A collaborative study of the five Nordiccancer registries. APMIS 1993;101(suppl 38):000-000.
2 Engeland A, Haldorsen T, Tretli S, et al. Prediction ofcancer mortality in the Nordic countries up to the years
297
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from

Dickman, Gibberd, Hakulinen298
2000 and 2010. A collaborative study of the five Nordiccancer registries. APMIS 1995;103(suppl 49):000-000.
3 Cain K, Diehr P. Testing the null hypothesis in small areaanalysis. Health Serv Res 1992;27:267-93.
4 Diehr P, Cain K, Connell F, Volinn E. What is too muchvariation? The null hypothesis in small-area analysis.Health Serv Res 1990;24:741-71.
5 Westerling R. Components of small area variation in deathrates: a method applied to data from Sweden. J EpidemiolCommunity Health 1995;49:214-21.
6 Boyle P, Muir CS, Grundmann E, eds. Cancer mapping.Berlin: Springer-Verlag, 1989.
7 Walter SD, Birnie SE. Mapping mortality and morbiditypatterns: an international comparison. Int 7 Epidemiol1991 ;20:678-89.
8 Walter SD. The analysis of regional patterns in health data.I Distributional considerations. Am .7 Epidemiol 1992;136:730-41.
9 Walter SD. The analysis of regional patterns in healthdata. II The power to detect environmental effects. Am 7Epidemiol 1992;136:742-59
10 World Health Organization. Plan of action implementing theglobal strategy for health for all. WHO Technical Report.Geneva: World Health Organization, 1982.
11 Karjalainen S. Geographical variation in cancer patient sur-vival in Finland: chance, confounding, or effect of treat-ment. I Epidemiol Community Health 1990;44:210-14.
12 Karjalainen S, Pukkala E. Social class as a prognostic factorin breast cancer survival. Cancer 1990;66:819-26.
13 Mooney G. Equity in health care: confronting the confusion.Effective Health Care 1983;1:179-85.
14 Mooney G. What does equity in health mean? World HealthStat Q 1987;40:296-303.
15 National Health Strategy. Enough to make you sick: Howincome and environment affect health. Research paper No1. Melbourne: National Health Strategy, 1992.
16 Hakama M, Karjalainen S, Hakulinen T. Outcome basedequity in the treatment of colon cancer patients in Finland.International3tournal of Technology Assessment in Health Care1989;S:619-30.
17 Karjalainen S. Equity and cancer patient survival. Tampere:University of Tampere, 1991, PhD Thesis. Acta Un-iversitatis Tamperensis 1991;316Series A.
18 Buckley JD. Additive and multiplicative models for relativesurvival rates. Biometrics 1984;40:51-62.
19 Esteve J, Benhamou E, Croasdale M, Raymond L. Relativesurvival and the estimation of net survival: elements forfurther discussion. Stat Med 1990;9:529-38.
20 Henson DE, Ries LA. The relative survival rate. Cancer1995;76: 1687-88.
21 Hakulinen T, Tenkanen L. Regression analysis of relativesurvival rates. Applied Statistics 1987;36:309-17.
22 Hakulinen T. A comparison of nationwide cancer survivalstatistics in Finland and Norway. World Health Stat Q1983;36:35-46.
23 Dobson A. An introduction to generalized linear modelling.London: Chapman and Hall, 1990.
24 Hakulinen T, Pukkala E, Hakama M, Lehtonen M, SaxenE, Teppo L. Survival of cancer patients in Finland in1953-1974. Ann Clin Res 1981;13(suppl 31):000-000.
25 Rimpela A, Pukkala E. Cancers of affluence: positive socialclass gradient and rising incidence trend in some cancerforms. Soc Sci Med 1987;24:601-6.
26 Auvinen A, Karjalainen S, Pukkala E. Social class andcancer patient survival in Finland. Am I Epidemiol 1995;142:1089-102.
27 Valkonen T, Martelin T, Notkola V, Savela S. Socio-economicmortality differences in Finland 1981-90. Helsinki: StatisticsFinland, 1993.
28 Saxen E, Hakama M. Cancer illnesss in Finland, with anote on the effect of age adjustment and early diagnosis.Annales Medicinae Experimentalis et Biologiae Fenniae 1964;42(suppl 2):1-28.
29 Berrino F, Esteve J, Coleman M. Basic issues in estimatingand comparing the survival of cancer patients. In: BerrinoF, Sant M, Verdecchia A, Capocaccia R, Hakulinen T,Esteve J, eds. Survival of cancer patients in Europe: TheEUROCARE study. IARC Scientific Publications No. 132.Lyon: International Agency for Research on Cancer, 1995.
30 Pollock A, Vickers N. The impact on colorectal cancer
survival of cases registered by "death certificate only":implications for national survival rates. Br3 Cancer 1994;70: 1229-31.
31 Francis B, Green M, Payne C, eds. The GLIM system:generalized linear interactive modelling. Release 4 manual.Oxford: Oxford University Press, 1993.
AppendixTHE VARIABILITY INDEX VLet fi = [f fl,*2. . .flP] represent the regionallog relative risk of excess mortality correctedfor age, sex, and follow up time for the p regionsand b = [b,, b2, . . ., bp] be an estimator of fiwith fixed but unknown covariance matrix W.Our aim is to use the regression model2' to
estimate the amount of systematic variation inthe fixed effects ,B.
The estimated parameters are a realisationof b, with estimated covariance matrix W. Thesame notation is used for the estimators andthe estimates, namely, b,, b2, . . ., bp. Maximumlikelihood estimation is used (using GLIM3)so b is an asymptotically unbiased estimator of.We chose the parameter
=2 1
E (fir-/f)2r= I
wherep
r= I
as the measure of the systematic regional vari-ation and it is this parameter we wish to es-timate. In effect, we are assuming that theensemble of parameters fi', . . ., ,,p has a priordistribution with variance a' and we wish toestimate U2 . No assumptions are made aboutthe form of the prior distribution. For thecurrent application we have forced the meanof the firs to zero so that the parameters havea ready interpretation but this property is notrequired in general.An unbiased estimator for C2 is given by V=
sb- VI +V2, where
sb2 I E"(br_ b)2
is the sample variance of the ensemble of es-timates;
V, =-Evar(br)p r=
is the average of the variances of the estimators;and
2V2 = ( - > cov(b, b5)
is the average of the covariances of the es-timators.We do not know V, and V2 so these must be
estimated from the data. 17 is estimated by theavAerage variance of the parameter estimates(V,) and V2 is estimated by the av,erage co-variance of the parameter estimates (142), whichare estimated by GLIM using the estimatedexpected information matrix.
If there is no systematic regional variation insurvival between the regions (m2 = 0), thenE(V) =0 and the estimate for U2 can be eithernegative or positive. If regional variation doesexist (.r2>0), then E(V)>O and the estimate isless likely to be negative. A negative estimatefor r2 means that we have observed less vari-ation than would be expected due to chanceso we conclude that there is no evidence ofsystematic variation.
on April 28, 2020 by guest. P
rotected by copyright.http://jech.bm
j.com/
J Epidem
iol Com
munity H
ealth: first published as 10.1136/jech.51.3.289 on 1 June 1997. Dow
nloaded from