Employee Benefit Manual
Transcript of Employee Benefit Manual

Employee Benefit Manual
2021-2022

Employee Benefits Manual – Medical Insurance
UST Medical Insurance
This manual has details of insurance coverage to UST employees and dependents for expenses related to hospitalization due to illness, disease or injury.
The manual covers the following:
• What’s New/Enhanced this year – Employee and Dependents
• Coverage Details For Employee Base Policy
• Maternity Benefits For Employee Base Policy
• Top Up Employee Policy

What’s New/Enhanced – Employee and Dependents
• Co-Pay reduction by 5% for all categories
• Home care treatment package for COVID – Up to INR 5,000 per member and INR 10,000 per
family.
• Zero Co-Pay for COVID claims
• ICU charges cover doubled for COVID hospitalisation
• Introduced Non-Medical Expense (NME) coverage for COVID hospitalisation up to INR
40,000 per family
• Room Rent eligibility for employees increased to 150% for those who avail Top Up of 10 Lakh
INR at Subsidised Premium of INR 3406 + Taxes
• Enhance your Family Policy up to 24 Lakhs SI with subsidised premium from ranging from
INR 1175 to INR 7635
• Introduced New Top Up options of 15 Lakh and 20 Lakh for employees
• Ambulance services enhanced: INR 5,000/ event; COVID-19 ambulance up to 10,000 per
family

Coverage Details For Employee Base Policy
Policy Parameter
Insurer The New India Assurance Company Limited
TPA Medi Assist Insurance TPA Pvt. Ltd.
Policy Start Date 31st May 2021
Policy End Date 30th May 2022
Coverage Type Family Floater (1+4) - Employee, Spouse, 3 Dependent Children
Sum Insured INR 4 Lac Floater
Maximum no of Members insured in a family
1 + 4
Employee Yes
Spouse Yes
Children Yes
Siblings No
Others No
Mid Term enrollment of existing Dependents Disallowed
Mid Term enrollment of new joiners (New employees +their Dependents) Allowed
Mid term enrollment of new dependents (Spouse/Children) Allowed
Note:
• New born and Newly married spouse should be added in the Medibuddy portal within 30 days of event. Death of any dependent should be informed within 30 days to deactivate from portal
• Mid-term addition/deletion of Top-up for employee and parents policy are disallowed
• Total annual premium will be deducted from your salary in 3 equal instalments in 3 consecutive months.”

Coverage Details For Employee Base Policy
Benefits / Extensions Coverage
Domiciliary Hospitalization Not Covered
Pre-Post Hospitalization Exp. 30 days and 60 days
Pre and Post Natal IPD cover of 10,000 & OPD cover of 5,000. OPD payable only if medically recommended by a gynecologist in a registered hospital
Well Baby Expenses Within maternity limit
Room Rent Capping including boarding and nursing expenses, DMO/RMO charges
Normal – INR 4,000/- for Kerala and 5,000/- for rest of the states. ICU is INR 8,000/ per day. In case of Covid, ICU limit is INR 16,000/- per day
Copay 5% Co- pay for employee ; 10% Co-pay for spouse & child on all claims. In case of Covid, no co-pay applicable
Benefits / Extensions Coverage
Standard Hospitalization Yes
TPA services Yes
Pre existing diseases Yes
Waiver on 1st year exclusion Yes
Waiver on 1st 30 days excl. Yes
Maternity benefits Normal 50k & C-Sec 70K
Baby cover day 1 Yes
Ambulance ServicesINR 5,000/- per event, Covid Ambulance INR 10,000 per family
Existing Employees + Dependents
Commencement Date 31st May 2021
Termination Date 30th May 2022
New joiners + Dependents
Commencement Date
Date of joining
Termination Date 30th May 2022
New Dependents (Marriage/Birth)
Commencement Date Date of event
Termination Date 30th May 2022

Coverage Details For Employee Base Policy
Benefits / Extensions Coverage
Room Rent Limits including boarding and nursing expenses, duty medical officer/resident medical officer charges
Normal – INR 4,000/- for Kerala and 5,000/- for rest of the states. ICU is twice the sum insured. If the member is compelled to move to a higher category of room, proportionate clause waiver upto 20,000/- of the proportionate expenses or actuals, whichever is lower
Covid Home Care TreatmentTreatment availed by the Insured Person at home for Covid on positive diagnosis of Covid in a Government authorized diagnostic Centre, which in normal course would require care and treatment at a hospital but is actually taken at home upto a maximum up to 14 days. Per member limit of INR 5,000/- and family limit of INR 10,000. Applicable for all employees and dependents
NME for Covid Hospitalization NME shall be payable upto a maximum of INR 40,000/- per member
Emergency care for employee Coverage of OPD treatment/emergency care if the employee falls sick during the workplace (Annual limit of 2,000/- per employee)
Genetic Treatment Covered upto 50% of sum insured, hospitalization is mandatory
Sleep Apnea Covered with 50% copay, machine cost shall not be covered
Biodegradable Stent Covered under hospitalization
Kidney Transplant Donor expenses covered
Cochlear Implant Covered with 50% copay
Surrogacy Cover Covered upto maternity sum insured
Medical Termination of pregnancy Covered upto 10k over and above maternity limit, medically certified by gynecologist

Coverage Details For Employee Base Policy
Benefits / Extensions Coverage
Life Threatening Cases Life threatening cases for Maternity claims coverage upto family sum insured
Cancer BenefitFirst Time Cancer Detection: In addition to the current benefit of INR 25,000 Employees can avail for the treatment in the subsequent year policy for INR 25,000 , Benefit can be claimed only once in a year and maximum twice in two years. (This extension is not given for Dependents, they are eligible for First Time Detection Cover of Rs.25000/- only)
HIV Treatment HIV Disease Covered Up to INR 100,000
Infertility Treatment Infertility coverage upto INR. 50,000 on IPD basis only
Stem Cell Treatment Stem Cell covered upto INR. 50,000 per family, Applicable on IPD basis only
Psychiatric Treatment Psychiatric & Psychosomatic disorders covered upto INR. 50,000 on IPD basis only, Applicable only for Employees
Ayurvedic Treatment INR 50,000 on registered Ayurvedic Hospitals on admission only
Coverage for Siblings Mentally physically challenged siblings are covered under the policy
Power Correction Vision correction cover +/- 7 power correction done by Lasik surgery is covered
Bariatric SurgeryBARIATRIC surgery for age less than 35 years is covered under the policy. Limit upto family sum insured. Only for those employees whose body mass index is over 35. Not applicable to dependents.
Oral Chemotherapy Oral Chemo Covered upto INR 50,000 including Hormonal Therapy. Applicable only for Employees
Congenital ExternalExternal Congenital 10% of the sum insured i.e. Rs.40,000/- per family for a maximum of 50 families per policy period (over and above the sum insured)

Maternity Benefits For Employee Base Policy
Benefit Details
Benefit Amount INR 50k For Normal & INR 70k For C-section
Restriction on no of children Maximum of 2 children
9 Months waiting period Waived off
Pre and Post NatalIPD cover of Rs.10,000 and OPD cover restricted to Rs.5,000 only per family. OPD Scan payable only if medically recommended by gynecologist in a registered hospital
Well Baby Expenses Within maternity limit
• These benefits are admissible in case of hospitalization in India.
• Covers first two children only. Those who already have two or more living children will not be eligible for this benefit.
• Expenses incurred in connection with voluntary medical termination of pregnancy during the first 12 weeks from the date of conception are not covered.

Top Up Employee Policy
• The sum insured is INR 1 Lac, 2 Lacs, 3 Lacs, 6 Lacs, 10 Lacs, 15 Lacs & 20 Lacs for Employee, Spouse & Children
• The top up plan is placed with the same insurer and TPA who underwrites the Group Medical Policy for operational efficiency
• Nomination for top up policy is done once a year & not in between the policy period except for the new joiners
• When the main medical plan sum insured is exhausted, only then the top up plan pays for the claim (amount over and above it).
• The top up sum insured could be utilized for ailments, except for Maternity
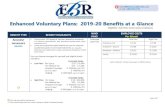
Employee Top Up Premium Chart (2021-22)
Additional Sum Insured Annual Premium (Exclusive of GST)
INR 1,00,000 INR 1,175
INR 2,00,000 INR 1,762
INR 3,00,000 INR 2,056
INR 6,00,000 INR 2,545
INR 10,00,000 INR 3,406
INR 15,00,000 INR 6,069
INR 20,00,000 INR 7,635
Kindly note that the room rent limit shall be enhanced by 0.5% of your base policy limit if you opt for 10 lac, 15 lac or 20 lac cover*** Total annual premium will be deducted from your salary in 3 equal instalments in 3 consecutive months.”

Voluntary Parental Plan
UST Voluntary Medical Insurance
This manual has details of voluntary insurance coverage to UST Employee’s Parents and Parents-In-Law for expenses related to hospitalization due to illness, disease or injury.
The manual covers the following:
• What’s New/Enhanced this year – Parents / Parents In Law
• Coverage Details For Parental Base Policy & Premium Rates
• Parental Top Up Policy

What’s New/Enhanced this year
•Co-Pay reduction by 5%
•Home care treatment package for COVID – Up to INR 5,000 per member
•Non-Medical Expense (NME) coverage for COVID hospitalisation up to INR 7,500 per parent
•Reduced Co-Pay limits
•Increase in Room Rent eligibility
•Reduced Top Up Premiums
•Ambulance services enhanced: INR 5,000/ event; COVID-19 ambulance up to 10,000 per family

Coverage Details For Parents Base Policy
“*** Total annual premium will be deducted from your salary in 3 equal instalments in 3 consecutive months.”
Policy Parameter
Insurer The New India Assurance Company Limited
TPA Medi Assist Insurance TPA Pvt. Ltd.
Policy Start Date 31st May 2021
Policy End Date 30th May 2022
Coverage Type Dependent Parents / Dependent Parent In Laws
Sum Insured Option of 2 lacs, 3 lacs & 4 lacs
Parental Base Premium Chart (Annual Premium Excl GST)
Sum Insured 31-35 35-40 41-45 46-50 51-55 56-60 61-65 66 & Above
INR 2,00,000 3,712 3,712 4,638 6,525 7,521 8,530 9,713 10,754
INR 3,00,000 5,180 5,180 6,465 9,288 10,749 12,226 14,004 15,705
INR 4,00,000 6,459 6,459 8,799 11,840 14,989 15,654 17,978 19,971

Coverage Details For Parents Base Policy
Benefits / Extensions Coverage
Covid Home CareCovid Home Care Upto INR 5,000 per member (Only on reimbursement mode. On submission of proper doctor recommendation & prescriptions along with all proper bills)
Room Rent Capping including boarding and nursing expenses, duty medical officer/resident medical officer charges
Room rent of 1.5 % for normal subject to minimum of INR 3,000 andmaximum of INR 5,000 and 2.0% for ICU in Kerala and 1.75% normalsubject to minimum of INR 3,000 and maximum of INR 5,000 and2.0% ICU for rest of the states with proportionate clauseapplicability
Copay
1. The Employees who have not opted either Parents or Parent inlaws previously now opt to Cover Either Parents or Parent in laws orboth as a combination - Copay applicable will be 20%.
2. The Employees who have opted in the expiring policy to coverparents, if now opt to Cover Parent in laws also - Copay applicablewill be 15% for Parent in laws.
3. The Employees who have opted in the expiring policy to coverparent in laws, if now opt to Cover Parents also - Copay applicablewill be 15% for Parents.
4. For new Joinees who opt for either Parents or Parent In laws orboth Copay will be 15%. Those who doesn't opt at the time ofJoining will not get another option during the policy period.
Benefits / Extensions Coverage
Standard Hospitalization Yes
TPA services Yes
Pre existing diseases Yes
Waiver on 1st year exclusion Yes
Waiver on 1st 30 days excl. Yes
Cataract Limit 24,000/- per eye
Ambulance ServicesINR 5,000/- per event, Covid Ambulance upto INR 10,000/- per family
Existing Employees + Dependents
Commencement Date 31st May 2021
Termination Date 30th May 2022

Co Pay & Proportionate Clause
What is co-pay? How does it work? Co-payment is the portion of the claim which associates needs to bear and remaining balance would be paid by the insurance company •A co-pay of 15% shall be applicable on the differential claim amount where the aggregate of all admissible claims if employee has covered the parents in previous year policy •A co-pay of 20% shall be applicable on the differential claim amount where the aggregate of all admissible claims if employee has not covered the parents in previous year policy
Room Rent Eligibility Norms & Proportionate Deductions
Room rent will have an upper limit of 1.5% of the SUM INSURED and ICU rentals to 2.5% of the SUM INSURED and applicability of proportionate clause if higher room rents are opted.(eg: if 2 lac sum insured is opted, 1.5% of 2 lac is INR 3000. So room rent per day will be INR 3000 inclusive of nursing and DMO charge). If some hospitals charges, nursing and duty medical officer charges (DMO) separately, this will be summated with room rent and considered as room rent. Eg: Room rent alone is INR 3000, nursing charge INR 500 and DMO charge INR 250, the room rent will be considered as INR 3000 + 500 +250 =INR 3750. Kindly note, so proportionate clause will be applicable as it exceed the room rent eligibility as per terms and conditions as mentioned above.▪ Basic sum insured of 3 lacs (1.5%), room rent is INR 4500/day.▪ Basic sum insured of 4 lacs (1.5%), room rent is INR 6000/day, but maximum capping INR 5000/day only.▪ Top-up if opted, will be utilized if the basic sum insured is exhausted. (will not be a part of room rent calculation)▪ Associates opting for a higher category of room shall have to bear the room rent difference as well as the proportionate expenses. This shall apply to cashless and reimbursement claims.
Proportionate Clause Or Deduction Applicability:There are circumstances when an associate’s parents or in-laws uses a room or ICU above the eligibility norm as defined in the above section. This can be either due to the employee’s discretion or by virtue of the fact that only
such facilities are available at that point of time in the hospital. In this circumstance, a deduction on account of Proportionate Clause will be applied on the insurance claim on below headings as detailed below:• Room Rent.• Medical Lab Test Charges/investigations.• Doctor Consultation Charges.• Surgery Costs. (If applicable).
• The example illustrates the arithmetic of proportionate deductions
Scenario Claim Type Total Claimed Amount Deduction after non medical expenses
Total Admissible amount
Ailment Copay Payable Amount after Copay (in INR)
Parents covered last year
1 Hospitalization 1,00,000 90,000 90,000 Accident 13,500 76,500 Yes then 15% Applied
2 Hospitalization 1,00,000 90,000 90,000 Accident 18,000 72,000 No then 20% Applied
Parental Sum Insured INR 2,00,000 x 1.5% = 3000(eligible room rent)
Availed Room Charges INR 6,000/- per day
Eligible Room Charges INR 3,000/- per day
Proportionate % 3000/6000 = 50% with weighted average

Top Up Parents Policy
• The sum insured is INR 1 Lac, 2 Lacs & 3 Lacs for Parents
• The top up plan is placed with the same insurer and TPA who underwrites the Group Medical Policy for operational efficiency
• Nomination for top up policy is done once a year & not in between the policy period except for the new joiners
• When the main medical plan sum insured is exhausted, only then the top up plan pays for the claim (amount over and above it).
• The top up sum insured could be utilized for ailments
Parental Top Up Premium Chart (2020-21)
Additional Sum Insured Annual Premium (Exclusive of GST)
INR 1,00,000 INR 2,866
INR 2,00,000 INR 4,413
INR 3,00,000 INR 5,527
Kindly note that the room rent limit (including boarding and nursing expenses, duty medical officer/resident medical officer charges) shall be restricted as
per your base policy and top up amount shall not enhance your room rent eligibility“*** Total annual premium will be deducted from your salary in 3 equal instalments in 3 consecutive months.”

Details of your Insurance Policy

Hospitalization Coverage Expenses
Please Note:
A) The expenses are payable provided they are incurred in India and within the policy period. Expenses will be reimbursed to the covered member depending on the level of cover that he/she is entitled to.
B) Expenses on Hospitalization for minimum period of 24 hours are admissible.
However this time limit will not apply for specific treatments i.e. Dialysis, Chemotherapy, Radiotherapy, Eye surgery, Lithotripsy (kidney stone removal), Tonsillectomy, D & C taken in the Hospital/Nursing home and the insured is discharged on the same day of the treatment will be considered to betaken under Hospitalization Benefit.
➢ Room and Boarding including boarding and nursing expenses, duty medical officer/resident medical officer charges
➢ Doctors/Medical Practitioner fees
➢ Intensive Care Unit
➢ Nursing expenses
➢ Surgical fees, operating theatre, anesthesia and oxygen and their administration
➢ Drugs and medicines consumed on the premises
➢ Hospital miscellaneous services (such as laboratory, x-ray, diagnostic tests)
➢ Radiotherapy and chemotherapy
➢ Surrogacy benefit covered up till maternity limit.

Active Line of Treatment
Instances wherein claims under this category shall not be payable
➢ Hospitalized and administered only with oral medication/injections, even if prescribed by a doctor
➢ Hospitalized only for investigations but no positive outcome of any ailment
➢ Treatment which would be done as out patient and admission not required
➢ Hospitalization only for physiotherapy
➢ Hospitalization only for evaluation purposes
Any hospitalization claim shall be admissible only if there is an active line of treatment during the course of hospitalization i.e. any investigations or treatment consistent and
incidental to the diagnosis of positive existence and treatment of any ailment, sickness or injury, for which confinement is required at a Hospital or Nursing Home shall be
payable under the policy.

Pre & Post Hospitalization
Post- Hospitalization Expenses
Definition
• If the Insurer accepts a claim under Hospitalization and immediately following the Insured Member’s discharge,further medical treatment directly related to the same condition for which the Insured Member was Hospitalized isrequired, the Insurer will reimburse the Insured member’s Post-Hospitalization Expenses for up to 60 day period.
Covered • Yes
Duration • 60 Days
Pre- Hospitalization Expenses
Definition
• If the Insured member is diagnosed with an Illness which results in his / her Hospitalization and for which the Insureraccepts a claim, the Insurer will also reimburse the Insured Member’s Pre-Hospitalization Expenses for up to 30 daysprior to his / her Hospitalization.
Covered • Yes
Duration • 30 Days

Cashless Process
Hospitals in the network (please refer to the website for the updated list)
For Updated List visit to Medi Assist link as below:
Cashless means the Administrator may authorize upon a Policyholder’s request for direct settlement of eligible
services and it’s according charges between a Network Hospital and the Administrator. In such case the
Administrator will directly settle all eligible amounts with the Network Hospital and the Insured Person may not
have to pay any deposits at the commencement of the treatment or bills after the end of treatment to the extent
as these services are covered under the Policy.
Note : Patients seeking treatment under cashless hospitalization are eligible to make claims under pre and post
hospitalization expenses. For all such expenses the bills and other required documents needs to submitted
separately as part of the claims reimbursement.
https://network.medibuddy.in/

Emergency Hospitalization
Step 1: Get Admitted
In cases of emergency, the member should get admitted in the nearest network hospital by showing their ID card.
Member gets admitted in the hospital in case of emergency
by showing his ID Card
Administrator verifies applicability of the claim to be registered and issue pre-
authorization
Member gets treated and discharged
after paying all non medicalexpenses like refreshments,
etc..
Hospital sends complete set of claims documents
for processing to the Administrator
Non cashless
Hospitalization
Process
Pre-authorization given by the
Administrator
Step 2: Pre-Authorization by hospital
Relatives of admitted member should inform the call centre within 24 hours about the hospitalization & Seek pre authorization. The preauthorization letter would be directly given to the hospital. In case of denial member would be informed directly
Step 3: Treatment & Discharge
After your hospitalization has been pre- authorized the employee is not required to pay the hospitalization bill in case of a network hospital. The bill will be sent directly to, and settled by Administrator
PR
OC
ESS
Member/Hospital applies for pre- authorization to the
Administrator within 24 hrs of admission
YES
NO

Planned Hospitalization
Step 1: Pre-Authorization
All non-emergency hospitalization instances must be pre-authorized with the Administrator , as per the procedure detailed below. This is done to ensure that the best healthcare possible, is obtained, and the patient/employeeis not inconvenienced when taking admission into a Network Hospital.
Member intimatesAdministrator of the plannedhospitalization in a specifiedpre-
authorization format at- least 48 hours in advance
Member produces ID card at the network hospital and gets
admitted
Please Note: At the time of discharge when the Administrator receives the final bill, they try to renegotiate with the Hospital for a better price. Hence it may take some time for Administratorto revertback withfinalapproval.Thisexercise checks the hospital to overcharge you and helps keep your sum insured utilization optimized for any future exigencies .. Please be patient
Follow non cashless process Pre-Authorization Completed
Claims Processing & Settlement by
Administrator & Insurer
Administrator authorizes cashless as per SLA for
planned hospitalization to the hospital
Hospital sends complete set of claims documents for
processing to Administrator
Claim Registered by the Administrator on
same day
Step 2: Admission, Treatment & discharge
After your hospitalization has been pre-authorized, you need to secureadmission to a hospital. A letter of credit will be issued by Administrator to the hospital. Kindly present your ID cardat the Hospital admission desk. The employee is not required to pay the hospitalization bill in case of a network hospital. The bill will be sent directly to, and settled by Administrator
YES
NO
Member gets treated and discharged after paying all non entitled benefits
like refreshments, etc..

Non Cashless Hospitalization
Admission procedure
• In case you choose a non-network hospital you will have to liaise directly with the hospital for admission.
• However you are advised to follow the pre authorization procedure to ensure eligibility for reimbursement of hospitalization expenses from the insurer.
Discharge procedure
• In case of non network hospital, you will be required to clear the bills and submit the claim to Mediassist for reimbursement from the insurer. Please ensure that you collect all
necessary documents such as – discharge summary, investigation reports etc. for submitting your claim.
Submission of hospitalization claim
• You must submit the final claim with all relevant documents within 60 days from the date of discharge from the hospital.

Non Cashless Process
Member intimates Mediassist before or as soon as hospitalization occurs
Insured admitted as per hospital norms. All payments made by member
Claim registered by Mediassist after receipt of claim intimation
Insured Submits relevant documents the Help desk within 60 days of discharge
Is document received within 30 days from discharge
Claim Rejected
No
Mediassist performs medical scrutiny of the documents
Is claim payable?
Yes
Mediassist checks document sufficiency
No
Yes
Claims processing done as per SLA
Receives mail about deficiency and document requirement
A
A
Payment to be done to Employee account
Yes
No
•Insured will create the summary of Bills (2 copies) and attach it with the original bills
•The envelope should contain clearly the Employee ID & Employee e-mail
Is documentation
complete as required

Claim Document Checklist
➢ Completed Claim form with Signature
➢ Hospital bills in original (with bill no; signed and stamped by the hospital) with all chargesitemized and the original receipts
➢ Discharge Report/Certificate/card (original)
➢ Attending doctors’ bills and receipts and certificate regarding diagnosis (if separate fromhospital bill)
➢ Original reports or attested copies of Bills and Receipts for Medicines, Investigations along withDoctors prescription in Original and Laboratory
➢ Follow-up advice or letter for line of treatment after discharge from hospital, from Doctor.
➢ Provide Break up details including Pharmacy items, Materials, Investigations even though it isthere in the main bill
➢ In case the hospital is not registered, please get a letter on the Hospital letterhead mentioningthe number of beds and availability of doctors and nurses round the clock.
➢ In non- network hospital, you may have to get the hospital and doctor’s registration number inHospital letterhead and get the same signed and stamped by the hospital, if required.

Standard Exclusions
•Injury or disease directly or indirectly caused by or arising from or attributable to War or War-like situations
•Circumcision unless necessary for treatment of disease
•Congenital external diseases or defects/anomalies
•Hospitalization for convalescence, general debility, intentional self-injury, use of intoxicating drugs/ alcohol.
•Venereal diseases
•Injury or disease caused directly or indirectly by nuclear weapons
•Naturopathy and AYUSH
•Any non-medical expenses like registration fees, admission fees, charges for medical records, cafeteria charges,
telephone charges, etc
• Dental surgery, dental cosmetics, tooth extraction, dental implant etc
•Any cosmetic or plastic surgery except for correction of injury
•Hospitalization for diagnostic tests only
•Vitamins and tonics unless used for treatment of injury or disease
•Voluntary termination of pregnancy during first 12 weeks (MTP)
• OPD Claims not payable under the base Group Mediclaim Policy
• Claims (of high value) submitted without prescriptions/diagnosis
• Health foods
• Costs incurred as a part of membership/subscription to a clinic or health centre
• Naturopathy
• Cost of appliances, spectacles and contact lenses.
• Non-medical expenses like Hospital surcharge, telephone bills, cafeteria bills

Contact Details
TPA : Medi Assist India TPA Pvt. Ltd.
Exclusive Hotline: 080-46855369
Exclusive E-Mail ID for Queries: [email protected]
Escalation Matrix
Level Name Contact No. Email Id
Level 1 Jerin Joseph 7411500621 [email protected]
Level 2 Sathish 9952933099 [email protected]
Level 3 Santhosh 7358556888 [email protected]
Level 4 Anand Sridhar 9566116633 [email protected]
Exclusive UST Global E-Mail ID for Any Other Queries: [email protected]
Exclusive Marsh E-Mail ID for Premium Receipts /Insurance Queries: [email protected]

Helpdesk Schedule

THANK YOU