Em hyperplasia-carinoma
-
Upload
prasad-csbr -
Category
Health & Medicine
-
view
497 -
download
3
Transcript of Em hyperplasia-carinoma

Dr.CSBR.Prasad, M.D.
EndometriumHyperplasias - Carcinomas

EM - Hyperplasia
• Increase glands to stromal ratio• Abnormalities of epithelial growth• May progress to EM carcinoma

• Pathogenesis: abnormal prolonged estrogen stimulation / anovulation.
1-Anovulation2-Menopause3-PCOD4-Granulosa cell tumor5-Adrenal cortical hyperplasia6-prolonged administration of estrogens7-inactivation of PTEN
EM - Hyperplasia

Morphology of EM hyperplasia:
1-Low grade (simple)2-High grade (atypical)
Low grade includesLow grade includes: anovulatory epithelium and subtle EIN
High grade includesHigh grade includes: Complex hyperplasia and PTEN mutation of EIN.
EM - Hyperplasia

Simple non-atypical hyperplasias:
1-glands of varying sizes2-glands resemble proliferative endometrium
They rarely progress to carcinomaThey frequently evolve to atrophy of both
glands and stroma
EM - Hyperplasia

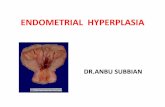
The endometrial cavity is opened to reveal lush fronds of hyperplastic endometrium. Endometrial hyperplasia usually results with conditions of prolonged estrogen excess and can lead to metrorrhagia (uterine bleeding at irregular intervals), menorrhagia (excessive bleeding with menstrual periods), or menometrorrhagia

This uterus is not enlarged, but there is an irregular mass in the upper fundus that proved to be endometrial adenocarcinoma on biopsy. Such carcinomas are more likely to occur in postmenopausal women. Thus, any postmenopausal bleeding should make you suspect that this lesion may be present

This is endometrial hyperplasia in which the amount of endometrium is abnormally increased and not cycling as it should. The glands are enlarged and irregular with columnar cells that have some atypia. Simple endometrial hyperplasias can cause bleeding, but are not thought to be premalignant. However, adenomatous hyperplasia is premalignant.

This is endometrial hyperplasia in which there is pronounced cystic change to the glands, with very little stroma. There is a slight proliferation of glands--a postmenopausal "cystic" atrophy of the endometrium has similar enlarged glands. This condition is not premalignant, like an adenomatous hyperplasia.

Complex hyperplasia:
1-increase in number and size of the EM glands (crowding)
2-epithelial stratification3-nuclear enlargement4-tufting of epithelium5-mitotic figures are common
23% may progress to adenocarcinoma
EM - Hyperplasia

With progesterone Tx:
--50% persisted--25% recurred--25% progressed to carcinoma
Treatment:HysterectomyIn young a trial of progesterones & follow up
Because of low rate of regression with progesterone Tx ultimately patients has to undergo hysterectomy.
EM - Hyperplasia


Endometrial carcinoma

• Occurs mainly in post menopausal women (55-65yrs) (uncommon <40yrs)
• Presents as post menopausal bleeding
It’s more commonly associated with:1-Obesity2-DM3-Hypertension4-Infertility5-EM ca and Breast Ca develop in the same
person
Endometrial carcinoma

• In terms of pathogenesis there are two subgroups of EMca have been identified:
1-EM ca developing in the background of prolonged estrogen stimulation and EM-hyperplasia
2-without hyperplasia / hyperestrinism
Endometrial carcinoma

Endometrial carcinoma
Support comes from the following evidences:1-both hyperplasia and cancer are linked to abdominal
obesity anovulatory cycles2-females with ovarian estrogen secreting tumors develop
carcinoma of EM3-EM ca is rare in women with ovarian dysgenesis4-HRT is associated with increased risk of EM Ca.5-Prolonged administration of DES to lab animals produced
EM polyps and hyperpalsias and carcinomas6-PTEN mutation is common in EM hyperplasia and
carcinoma

• Second subtype – without hyperplasia:
1-old age2-carcinomas are more poorly differentiated
(tumors may resemble serous carcinoma of the ovary)
3-overall these tumors have poor prognosis than estrogen related tumors
Endometrial carcinoma

Morphology:Two types:1-polypoidal2-diffuse (involving whole EM surface)
Spread occurs to: -myometrium-periuterine structures-LN mets-metastasis to lung, liver, bone-serous type of carcinomas may involve
peritoneal cavity due to different way of spread i.e. tubal or lymphatic transmission
Histology: 85% are adenocarcinomas
Endometrial carcinoma


This adenocarcinoma of the endometrium is more obvious. Irregular masses of white tumor are seen over the surface of this uterus that has been opened anteriorly. The cervix is at the bottom of the picture. This enlarged uterus was no doubt palpable on physical examination. Such a neoplasm often present with abnormal bleeding.

The endometrial adenocarcinoma is present on the lumenal surface of this cross section of uterus. Note that the neoplasm is superficially invasive. The cervix is at the right.

The endometrial adenocarcinoma in the polyp at the left is moderately differentiated, as a glandular structure can still be discerned. Note the hyperchromatism and pleomorphism of the cells, compared to the underlying endometrium with cystic atrophy at the right.

This is endometrial adenocarcinoma which can be seen invading into the smooth muscle bundles of the myometrial wall of the uterus. This neoplasm has a higher stage than a neoplasm that is just confined to the endometrium or is superficially invasive.





• Staging• Grading (figo)
Endometrial carcinoma

Clinical features:
1-Irregular vaginal bleeding2-Excessive leucorrhea3-Uterine enlargement
Prognosis: Stage of the diseaseHistological grade and type
Endometrial carcinoma

• Carcinosarcoma• Adenosarcoma• Stromal nodule to stromal sarcoma
Tumors of Endometrium with stromal differentiation
(stromal tumors)

Tumors of Myometrium
• Leiomyoma • Leiomyosarcoma

Leiomyoma
• Most common tumor of humans• Commonly called as ‘FIBROIDS’• More than one genetic abnormality can
lead to leiomyomatous growth – t(12, 14); 7q del; Trisomy 12.

Morphology:
• Well circumscribed• Discrete, round, firm• Grayish white• Variable sizes (a few mm to very large
tumors)• Types (Subserosal, Intramural, Submucosal)• c/s whorled pattern• Red degeneration in large tumors• Other degenerative changes
Leiomyoma





In the upper fundus of the uterus protruding into the endometrial cavity is a nodule that proved to be a leiomyoma. Thus, this is a submucosal leiomyoma. Such benign smooth muscle tumors of the myometrium are very common--perhaps at least 1 in 5 women has one. They may be the cause of irregular bleeding if present in a submucosal location, as seen here. Larger leiomyomas may also produce bleeding or pelvic discomfort

Smooth muscle tumors of the uterus are often multiple. Seen here are submucosal, intramural, and subserosal leiomyomata of the uterus.

Here is a very large leiomyoma of the uterus that has undergone degenerative change and is red (so-called "red degeneration"). Such an appearance might make you think that it could be malignant. Remember that malignant tumors do not generally arise from benign tumors, which is a good thing, because leiomyomas are so common (at least 20% of women will have one). Postmenopausally, leiomyomas tend to regress in size and become fibrotic.

Here is a bifid (septate) uterus. Sometimes even the cervix and/or vagina may be double as well. This is of no major consequence except that in pregnancy a bifid uterus may not enlarge normally and lead to fetal loss, or a normal vaginal delivery may not be possible with a double cervix or vagina. Note that there is also a small intramural leiomyoma on the septum at the left.

Whorled appearance – c/s

This large squamous carcinoma (yellow square) has obliterated the cervix and invaded the lower uterine segment. The uterus also has a round leiomyoma up higher (Red arrow).

Microscopy:
1-Whorled bundles of smooth muscle cells2-Spindle cells with ‘CIGAR’ shaped nucleus3-Long slender cytoplasmic extensions4-Cytolpalsm is eosinophilic5-Necrosis, hemorrhages, calcification,
ossification, cartilage, hyalinization et.c.
Leiomyoma


Here is the microscopic appearance of a benign leiomyoma. Normal myometrium is at the left, and the neoplasm is well-differentiated so that the leiomyoma at the right hardly appears different. Bundles of smooth muscle are interlacing in the tumor mass



• Most of the leiomyosarcomas arise in the uterus• Peak incidence at 40-60yrs of age• Two distinct growth patterns 1-Buky fleshy masses that invade the uterine wall & 2-Polypoidal masses that project into the lumen
• Soft fleshy tumors with a whitish cut surface• Areas of hemorrhage and necrosis• Periphery of the tumor is not sharply defined
Leiomyosarcoma


This is a leiomyosarcoma protruding from myometrium into the endometrial cavity of this uterus that has been opened laterally so that the halves of the cervix appear at right and left. Fallopian tubes and ovaries project from top and bottom. The irregular nature of this mass suggests that is not just an ordinary leiomyoma.

Microscopy:
• Apperances vary from resemblence of leiomyoma to anaplastic tumors
• All smooth muscle tumors with mitotic figures fewer than 2 / 10hpf are considered benign (Hendrikson and Kempson)
• Note: Leiomyomas in young and pregnant females may show mitotic activity and may be mistaken for leiomyosarcoma
• There may be areas of myxoid change• Extensive necrosis is also an ominous sign
Leiomyosarcoma

Here is the microscopic appearance of a leiomyosarcoma. It is much more cellular and the cells have much more pleomorphism and hyperchromatism than the benign leiomyoma. An irregular mitosis is seen in the center.

As with sarcomas in general, leiomyosarcomas have spindle cells. Several mitoses are seen here, just in this one high power field.

Sarcomas, including leiomyosarcomas, often have very large bizarre giant cells along with the spindle cells. A couple of mitotic figures appear at the left and lower left



Metastasis thru blood stream to lung, bone and brain
Dissemination also occur thru abdominal cavity
5yr survival for patients with uterine leiomyosarcomas is < 40%
Leiomyosarcoma

E N DE N D



![Endometrium presentation - Dr Wright[1] · Endometrial Hyperplasia Simple hyperplasia Complex hyperplasia (adenomatous) Simple atypical hyperplasia ... Progression of Hyperplasia](https://static.fdocuments.us/doc/165x107/5b8a421e7f8b9a50388bc13d/endometrium-presentation-dr-wright1-endometrial-hyperplasia-simple-hyperplasia.jpg)