Effectiveness of Deep Pharyngeal Neuromuscular Stimulation Versus Thermal Gustatory Stimulation in...
-
Upload
constantineelia -
Category
Documents
-
view
487 -
download
1
description
Transcript of Effectiveness of Deep Pharyngeal Neuromuscular Stimulation Versus Thermal Gustatory Stimulation in...

Graduate SchoolUniversity of South Florida
Tampa, Florida
CERTtr'ICATE OF APPROVAL
Master's Thesis
This is to certifu that the Master's Thesis of
MARIA H. WILLIS
with a major in Speech Language Pathology has been approved by
the Examining Committee on April 14,1997as satisfactory for the thesis requirement
for the Master of Science degree
Examining Committee:
Member: Arthur

EFFECTIVENE S S OF DEEP PHARYNGEAL NEUROMUSCULAR STIMULATION
VERSUS THERMAL GUSTATORY STIMULATION IN DECREASING LENGTH
OF SWALLOW INITIATION AND IMPROVINGLINGUAL MOVEMENTS
,MARIA H. WILLIS
A thesis submitted in partial fulfillmentof the requirements for the degree of
Master of Science
Department of Communication Sciences and DisordersUniversity of South Florida
Ap,"il 1997
by
Major Professor: Ruth Huntley Bahr, Ph'D.

Dedication
I would like to thank my family for their neverending love, encouragement,
support and prayers, as I have worked to attain this degree and complete this thesis. I
thank my sister for her words when I asked her if I should attempt to write a thesis; she
said "Do it... I will pray for you."
I thank my husband, who has been so patient and encour agn1. I thank him for
having confidence in me when I had none in myself. He never once complained about the
many hours I spent at school, at studying , or atthe computer.
I thank my Lord, Jesus Christ, who placed me in this program for reasons I am
only now beginning to see. I give the credit for my success in this program to the Lord
and trust that He will continue to bless me as I strive to do my best as a clinician.

Acknowledgements
I would like to thank Dr. Bahr for taking on this project. I appreciate the time and
effort she has put into this study. Dr. Bahr has shown genuine interest in seeing this
project succeed and in teaching me the basics of being a researcher. For these things, I
thank her.
I thank Dr. Guilford for his cooperation on this study. I also thank him for
affording me the opportunity to prove myself in graduate school. I greatly appreciate it
and feel that I have succeeded.
A special thanks to Donna Heyen, who over the last several years has helped me to
grow not only professionally but personally as well. Donna selflessly gave of her time and
energy to guide me in this project, and for that I will always be grateful.

Table of Contents

Group Effects...... """"24
Individual Effects...... '"""""""25
Chapter V: Discussion and Conclusions........."... ."""""'""'32
Swallow Initiation... --.--....'...........32
Lingual Movements,..,,.,..,..,,,, .'.."32
Summary of IndividualEflects... ................".....,.........""33
TGS Versus DPNS..... '. """""""35
ComparisonofthePresentFindingswiththeCurrentLiterature..
Factors Influencing the Results of this Study.. .. . '""'""""37
42References

List of Figures
Figure l. Plot of Percent Change of Each Trial Over AII Four Days......... .....................21
Figure 1. Graph of Baseline Dry Swallows Versus Stimulated Swallows for AllParticipants................ 23
Figure 3. Plot of Percent Change of Swallow Response Time for TGS and ModifiedDPNS....... ......2s
lV

EFFECTIVENES S OF DEEP PHARYNGEAL NEUROMUS CULAR STIMULATION
VERSUS THERMAL GUSTATORY STIMULATION IN DECREASING LENGTH
OF SWALLOW INITIATION AND IMPROVTNG LINGUAL MOVEMENTS
MAzuA H. WILLIS
An Abstract
Of a thesis submitted in partial fulfillmentof the requirements for the degree of
Master of Science
Department of Communication Sciences and Disorders
University of South Florida
April 1997
Major Professor: Ruth Huntley Bahr, Ph-D.
by

The purpose of this study was to compare thermal gustatory stimulation (TGS)
and deep pharyngeal neuromuscular stimulation @PNS) to determine which treatment
technique may be more beneficial to the dysphagic patient. TGS and DPNS both involve
stimulation via cold sour swabs, however, the site of stimulation differs between the two
treatments. TGS stimulates the anterior faucial arches, whereas DPNS stimulates the
anterior faucial arches, the tongue, velum, uvula, and pharynx.
Six participants, all of whom suffered a cerebrovascular accident, were treated for
four consecutive days, with an alternating treatment design (ABAB design). The
participants included three men and three women. The data from one female participant
were not included in the analysis as she was diagnosed with a brainstem stroke and was
unable to initiate a baseline dry swallow on command.
Each subject received one treatment session a day for four consecutive days. At
the start of each session, baseline measurements were taken. Baseline measures consisted
of rating lingual movements, including protrusion, elevation, and lateralization, and timing
three dry swallows. Then the treatment, either TGS or DPNS, was administered. One
application of either technique consisted of 20 frozen lemon swabs. After each swab, the
patient was given the command to swallow and the swallow was timed with a stopwatch.
After all20 swabs had been adminstered, lingual movements were rated again.
The dependent variables were swallow initiation time and degree of lingual
movement" The data representing speed of swallow initiation consisted of the average of
the two best dry swallows and of the two best stimulated swallows. These data were then
analyzed using a MANOVA. For the purpose of analysis, lingual movement data were
rated as either "0" if no change occured after stimulation or "1" if change did occur after
stimulation. The Yates corrected Chi-square analysis was conducted to determine
whether or not a significant difference in lingual movements was created by either TGS or
DPNS.
vt

The outcomes of this study did not reveal that one treatment was significantly
more effective than another in treating oropharyngeal dysphagia. However, alarge effect
size was noted, which suggested that DPNS may be more efflective than TGS.
An interesting finding in this study was that modified DPNS made an initial change
in the swallow response time that was greater than the change produced by TGS. By the
second administration of either treatment, both techniques elicited a similar degree of
change in swallow initiation. Although TGS showed great improvement on the second
administration, it is not known whether or not this trend would continue. Modified
DPNS remained constant over two trials, however, it is not known whether or not this
tendency would continue either.
This study has also provided evidence to suggest that lingual movements generally
improve after stimulation. Both treatment techniques caused an improvement in tongue
movement, which may suggest improved swallow function. However, the data from this
study were not sufiicient to indicate that one technique may be more influential in causing
this improvment.
Abstract Approved: #t*Major Professor: Ruth Huntley Bahr, Ph.D,Assistant Professor, Department of Communication Sciences and
Disorders
,', i ,l) r-/'DateApprou"a,,?r, i iK,i7?7
vll

Chapter I
Introduction
One of the most challenging complications of a stroke is the presence of
oropharyngeal dysphagia. Dysphagia affects up to 59Yo of those who have suffered a
stroke (Lugger, 1994). A patient with dysphagiamay present with one or several
symptoms such as a wet vocal quality, oral spillage, pocketing of food in the buccal
cavity, coughing, and the inability to initiate a swallow in a timely manner (Lugger, 1994).
If untreated, a patient with oropharyngeal dysphagia may be placed at risk for multiple
health conditions. These health conditions include malnutrition, dehydration, and
aspiration which may lead to the development of aspiration pneumonia (Lugger,1994). It
is not uncommon for aspiration pneumonia to be fatal in the elderly population.
Aspiration pneumonia results from the penetration of fluids, bodily or foreign, or
particles of matter into the lower respiratory tract (Martin et al., L994). According to
Terry and Fuller (1989), everyone aspirates to some degree. In typically healthy
individuals, this small amount of aspiration does not compromise the respiratory system
(Bartlett & Gorbach, 1975). However, in patients with a diminished health status,
aspiration may lead to further medical complications, such as pneumonia.
There are several categories of aspiration pneumonia. The first category includes
the aspiration of particles of matter, foreign bodies, or large amounts of fluid. The second
category is chemical pneumonitis which commonly is caused by aspiration of gastric
liquids. The third category of pneumonia is drowning and the fourth category is
pneumonia of infectious origin. Infectious pneumonia has several causes, namely,
apiratiori of matter, aspiration of secretions of the oropharynx, or inhalation of chemicals

(Finegold, 1991). According to Finegold, individuals who suffer from decreased
consciousness, swallowing difficulties, a disease of neurologic etiology, or a mechanical
hinderance, such as a nasogastric tube, may be at greater risk for developing aspiration
pneumonia. Typically, aspiration pneumonia is characterizedby fever, cough, crackles
upon inspiration, and the generation of sputum. A chest x-ray will most likely show
infiltrates of the lung (Martin, et al., lgg4). Martin and his colleagues further state that
the occurrence of aspiration pneumonia is significantly higher in patients who have
oropharyngeal dysphagia. Additionally, the prevention of continued aspiration is
piramount to the return of a healthy respiratory system. Martin and others suggest that in
patients with oropharyngeal swallowing difficulties, prevention of further aspiration may
be achieved by remediating the impaired swallow function.
A delay in the initiation of the swallow reflex is the most corlmon characteristic of
dysphagia in cerebrovascular accident (CVA) patients and is also the most common cause
of aspiration (Veis & Logemann, 1985). Hence, effective treatment of dysphagia is
necessary to decrease the delayed onset of swallow initiation in patients with
oropharyngeal dysphagia. By increasing the rate at which the swallow is initiated, the risk
of aspiration decreases.
According to Lugger (1994), the process of swallowing involves four stages: the
oral preparatory stage, the oral stage, the pharyngeal stage, and the esophageal stage. In
the oral preparatory phase, food is masticated and a bolus is formed for propulsion into
the phar5mx. During the oral phase, lingual elevation presses the bolus against the hard
palate which results in posterior movement of the bolus into the pharynx. The pharyngeal
stage occurs when the bolus enters the pharynx, triggering the swallow reflex which
propels the bolus into the esophagus. The final phase, the esophageal stage, consists of
the bolus being carried to the stomach via the esophagus.
The treatment of dysphagia may be direct or indirect. Direct treatment of
dysphagid refers to compensatory techniques such as tucking the chin, performing a head-

turn, tilting the head, or swallowing twice to increase the safety of the swallow. A chin-
tuck increases the size of the valleculae, which in turn catches the bolus as it spills into the
pharynx. By trapping the bolus until the swallow is triggered, the risk of aspiration before
the swallow is reduced (Logemann, 1986). Similarly, a head turn may be employed in
patients with unilateral damage. Another technique is tilting the head toward the
stronger side of the body. This allows gravity to pull the bolus toward the stronger oral
and pharyngeal musculature, resulting in a more efficient and safer swallow (Logemann,
1 e86).
Maneuvers are another type of direct treatment which may be employed to
increase the safety of the swallow. Maneuvers may include a supraglottic swallow or a
Mendelsohn maneuver (Neumann et al., 1995). A supraglottic swallow is performed by
taking in a breath and holding it. While the breath is being held, the patient should
swallow. After the swallow is complete, the patienl should cough before inhaling agun.
This maneuver causes the larynx to close which ensures protection of the airway from the
bolus (Logemann, 1986). The Mendelsohn manuever is often used with patients who
exhibit decreased laryngealelevation during the swallow (Logemann, 1995). Decreased
laryngeal elevation results in incomplete closure of the laryngeal vestibule and therefore
inadequate airwayprotection. The Mendelsohn maneuver is performed holding the larynx
in its elevated position for several seconds during the swallow, instead of allowing it to
immediately fall. By prolonging laryngeal elevation during the swallow, increased
protection is provided for the airway (Logemann,1993).
Indir:ect treatment of dysphagia refers to sensory stimulation which focuses on the
sensorimotor impairment. As such, stimulation techniques may be used to augment the
swallowing reflex (Neumann, et al, 1995) This is accomplished by providing extra
sensory input to the swallowing areas in the brain stem to alert the system that the need to
swallow is approaching. According to Logemann (1986), treatment for the latent
swallow reSponse normally involves thermal stimulation. Thermal stimulation or thermal

gustatory stimulation (TGS) is the treatment technique for pharyngeal dysphagia which
has received the most research attention (Rosenbek, Robbins, Fishback & Levine, l99L;
Lazzara,Lazarus & Logemann, 1986;Neumann et al., 1995). According to Logemann
(1983), thermal stimulation is accomplished by placing a size 00 laryngeal mirror in ice
water for 10 seconds and then applying the mirror to the anterior faucial arches. The
application consists of five or six strokes to the base of each arch. According to
Pommerenke (1928), the anterior faucial pillars are the most sensitive area in the oral
cavity and are involved in facilitating a swallow response. As Logemann (1986) stresses,
the contact of a laryngeal mirror or swab to the anterior faucial pillars does not trigger a
swallow. It does, however, provide stimulation so that when a swallow is initiated, it will
execute more quickly. The purpose of thermal stimulation then, is to increase sensation
and increase the initiation of the swallow response (Selinger, Prescott & Hoffinan, 1994).
More recently, a new technique known as deep pharyngeal neuromuscular
stimulation (DPNS), has been developed as a treatment for pharyngeal dysphagia
(Stefanakos,1994). DPNS consists of stimulating the mucosa of the velum, tongue,
uvula, and pharynx with cold lemon swabs. This technique is based on the idea that reflex
action may be restored in the pharynx through stimulation of cranial nerves V, VIL IX, X,
and )(II. It is hypothesized that this technique will stimulate a swallow reflex, not simply
initiate an already defective swallow (Stefanakos, 1994).
The purpose of this study is to compare TGS and DPNS as treatments for
pharyngeal dysphagia. To date, no efficacy studies have been published on DPNS.
Therefore, it is necessary to determine the effectiveness of DPNS. In comparing DPNS
to TGS, outcomes should reveal which treatment technique may be more beneficial to the
dysphagic patient.

Chapter II
Review of the Literature
Dysphagia is defined as difficulty with the act of swallowing (Zemlin,1988), and it
occurs as the result of numerous physiological and anatomical conditions (Logemann,
1986). Dysphagia may be caused by a stroke, atraumatic brain injury, or an illness such
as multiple sclerosis or Parkinso ntsm (Lazzara etal., 1986) Swallowing dysfunction is
characterized by wet vocal quality, pocketing of food in the sulci of the oral cavity, a
delay in the initiation of the swallow, and coughing (Lugger, 1994). Additionally,
reduced control of the bolus in the oral cavity, a latent swallow reflex, the presence of
residue in the pharynx after the swallow, and aspiration, which refers to a substance
infiltrating the airway beyond the level of the vocal folds (Veis & Logemann, 1985), are
all common characteristics of dysphagia (Lugger,1994).
Dysphagia may be diagnosed through either a bedside swallow evaluation or a
modified barium swallow study (MBS), but often both assessments are utilized. A
bedside swallow evaluation consists of gathering a history of the patient's swallowing
difficulties, current diet, and respiratory status. Then, oral and laryngeal examinations are
performed. These procedures focus on lingual and labial movements related to the
movement of a bolus through the oral phase of swallowing, the quality of the voice, how
productive the cough or clearing of the throat appears to be, clarity of /a/ when phonated,
and presence of delay in swallow initiation (Logemann,1,995). On the other hand, the
modified barium swallow study is a radiographic study. It focuses on the etiology of the
swallowlng problem and guides the clinician in determining the safest diet and planning

treatment of swallowing dysfunction (Logemann, 1986). The fundamental purpose of
completing a modified barium swallow study is to determine the presence or absence of
aspiration during intake, and which, if any, modifications in diet or posture, or the use of
maneuvers will be beneficial in eliminating the occurence of aspiration (Martin, et al.,
1994). The MBS documents exactly what occurs in each stage of the swallow.
According to Logemann (1986), a bedside swallow evaluation alone is not ample since it
is possible for a patient to present without any clinical signs of swallowing difficulty while
silently aspirating: This idea received further support in a study by Lugger (1994). She
identified 18 participants who were aspirating during a bedside swallow evaluation, yet,
all participants (N:43) were found to be aspirating when a modified barium swallow
study was conducted.
Although the act of swallowing involves several stages, the oral preparatory
phase, the oral phase, the pharyngeal phase, and the esophageal phase (Lugger, 1994) ,
this study will focus on the oral and pharyngeal stages. According toLazzara,Lazants,
and Logemann (1986), the oral stage, which is voluntary, begins with the bolus being
moved posteriorly in the oral cavity by the tongue. This stage ends with the triggering of
the swallow reflex as the bolus meets the anterior faucial pillars. The pharyngeal stage,
which is involuntary, consists of the bolus moving through the pharynx and concludes
with the passage of the bolus into the esophagus. The pharyngeal phase was chosen as
the primary focus of this study since both techniques purport to treat pharyngeal
dysphagia. Since the impact of these treatment regimes on lingual movements is also
being investigated, the oral phase of swallowing is being considered due to the nature of
the relationship between lingual movement and the efiiciency.of the oral phase.
Kahrilas (1993) described the swallowing process in two steps. the oral and
pharyngeal phases, During the oral phase of the swallow, the groove of the tongue
becomes the carrier of the bolus which has been formed from the masticated food. The
tongue piopels the'bolus posteriorly where it will enter the pharynx. As the bolus

contacts the tongue posteriorly, the pharyngeal phase of the swallow is initiated. In this
view, the pharyngeal phase consists of four distinct steps. Initially, the velum elevates and
retracts. The larynx then moves up and forward, closing offthe laryngeal vestibule and
providing protection to the airway. The upper portion of the esophagus opens to allow
the bolus to enter. Lastly, the bolus is moved into the esophagus. Tongue movement is
vital to the functional swallow. Lingual manipulation of the bolus is necessary for
chewing, clearing the bolus from the oral cavity, and initiating the onset of the swallow
reflex by propelling the bolus into the pharynx (Logemann, 1993).
This study focuses on TGS and DPNS, two treatment techniques designed to
improve swallowing function. Both techniques utilize cold sour stimuli, but target
different oral areas. TGS provides stimulation to the anterior faucial arches, while DPNS
provides stimulation to the anterior faucial arches, tongue, velum and uvula to elicit a
reflexive swallow. Since DPNS directly stimulates the lateral portion of the tongue,
where taste is controlled by CN VII, it may be inferred that DPNS would produce a more
efficient oropharyngeal swallow than TGS, which focuses primarily on the stimulation of
the anterior faucial arches. It is possible that thermal stimulation elicits a dysfunctional
swallow and, therefore, perpetuates an ineffective swallow (Stefanakos, 1994). Hence,
TGS utilizes inefficient muscle action to stimulate reflex function in the pharyrx. Perhaps
providing more input to those areas which stimulate a reflex within the pharynx will
improve swallowing function. According to Capra (1995), sensory nerves present in the
oral mucosa and those located pharyngeally contribute to the stimulation and execution of
motor behaviors. Furthermore, the pharynx is heavily innervated at the point of the oral
and nasal cavity divisions. Cranial nerve (CN) IX, the glossopharyngeal nerve, is the
primary sensory receptor for incoming stimuli in the pharynx. Additionally, Stefanakos
(1994) and others report that CN IX is responsible for the stimulation of reflexes such as
swallow, gag, velar movement, and lingual retraction.

Parameters Affecting Swallow Function
Early research in the stimulation of a swallow response was conducted by
Pommerenke in 1928. His study attempted to determine which areas of the oral cavity
were most likely to elicit a swallow. He stimulated different areas by probing with a glass
rod. These areas included the base of the tongue, tonsils, anterior pillars, uvula, velum,
posterior pharynx, deep posterior pharynx, and posterior pillars. He found
overwhelmingly that the anterior faucial arches stimulated a swallow reflex more
Consistently than any other area, and did so in more people. Of his participants, TTYI
initiated a swallow when the anterior faucial pillars were stimulated. He further stated
that the velum and the uvula were the least sensitive areas for stimulating a swallow.
When the anterior faucial arches were covered with a cocaine solution to numb them,
100% of the participants displayed difficulty swallowing. In subjects whose velum and
uwla were painted with the same solution, only 13 Yo displayed difficulty swallowing.
Finally, 26Yo of those whose tongue base was covered with the cocaine solution had
difiiculty initiating the swallow. Pommerenke concluded from his research that there was
no location in the oral mucosa which consistently stimulated a swallow in all members of
the population, however, in most people, a swallow was initiated by stimulation of the
anterior faucial pillars. This body of research has provided support for TGS in that it
shows the anterior faucial pillars to elicit a swallow most often in most subjects.
However, Pommerenke's study does not yield any evidence in support of DPNS since
Pommerenke concludes that the velum and uvula were the least sensitive areas in
triggering a swallow reflex.
Pommerenke's study (1928) was not the only evidence to support the effectiveness
of thermal stimulation administered to the anterior faucial arches. Research byLazzara
and colleagues (1986) also provided evidence in support of TGS, Their study focused on
the efficacy of the outcomes of thermal stimulation on25 patients with varying types of
neuroiogibal impairment, including left and right CV{ Parkinsonism, multiple sclerosis

(M S ) and head trauma. Swallow latency was measured for boluses before and after
thermal stimulation was administered. Participants were given three ll3 teaspoon
swallows of each of two consistencies: liquid barium and barium paste. After the second
swallow of each consistency, thermal stimulation was applied to the base of the anterior
fauoial pillars and the third bolus was introduced. The duration of the second and third
swallows was record ed. Lazzara, et al. (1986) stated that the delay of the initial swallow
was not recorded because of clinical evidence suggesting that the first swallow of a
substance may display more reflex delay than subsequent swallows. The results of this
study were obtained through videofluoroscopic study and revealed that in 23 of 25
patients, the delay in swallow initiation was reduced following thermal stimulation. The
mean pharyngeal transit time for liquids before stimulation was 4.2 seconds" Following
stimulation, the mean pharyngeal time for liquids was 2.4 seconds. The mean transit times
for paste consistencies displayed improvement as well. Without stimulation, the mean
pharyngeal transit time for paste was 4.1 seconds; after stimulation it was decreased to
1.6 seconds. The two patients who did not show improvement had extremely delayed
pharyngeal response times -- over 20 seconds. According toLazzara, et al. (1986), some
severely impaired patients may have an absent swallow reflex, even when thermal
stimulation is applied. In such patients, thermal stimulation may need to continue several
times a day for several months in order to restore the swallowing function to a level at
which it is safe to resume oral intake.
Although the research conducted by Pommerenke (1923) andLazzata arrd
colleagues (1986) provide support for the use of TGS, not all recent studies in this area
had similar results. A study conducted by Rosenbek et al. (1991), did not showthat
thermal application caused improvement in swallowing function. Seven adult males who
had suffered multiple ischemic CVAs, as evidenced by either Magnetic Resonance
Imaging (IVRI) or Computed Tomography (CT) scan, were utilized in this study' In
addition, six of the seven participants presented with liquid spillage into the valleculae

andlor pyriform sinuses prior to the onset of hyo-laryngeal excursion. Thermal
stimulation was conducted by stroking the anterior faucial pillars from the base upward
toward the midline. Three strokes were applied to each pillar, the participant then
completed a dry swallow or was given water or ice chips to swallow; this constituted one
trial. One week of treatment with thermal stimulatiofl was alternated with one week of no
treatment continuously for four weeks. Re-evaluation of the swallow response was
conducted via videofluoroscopy once a week for four consecutive weeks (2 weeks of
treatment and 2 weeks of no treatment) to measure change in the swallow function. One
month after treatment was discontinued, a videofluroscopic study was conducted to
assess treatment maintenance. The outcomes of this study did not present strong
evidence of thermal stimulation improving dysphagia when a period of treatment was
alternated with a period of no treatment. A decrease was reported for two patients in the
duration of stage transition which is a measure of pharyngeal response time. This
decrease was directly related to treatment with thermal application. In addition, it was
observed that one particular participant aspirated less when thermal stimulation was
applied. Outcomes of this study may have been more favorable toward the benefits of
thermal application had only single-infarct participants been studied. Additionally,
Logemann (1983) recommends five to six strokes be applied to each faucial pillar,
whereas only 3 strokes were applied to eachpillar in this study conducted by Rosenbek
and colleagues (1991). Therefore, the limited lenglh of stimulation per trial may have
impacted the outcomes.
Selinger, Prescott, and Hoffrnan (1994) explain that the use of cold stimulation
most likely arose from early studies such as Pommerenke's (1928) which investigated the
role of touch and temperature receptors. The addition of a sour taste to the iced stimulus
may further increase the sensory input to the portion of the medulla that recognizes when
a swallow is being stimulated (Logemann et al., 1995). The taste buds located laterally
on the tongue are more responsive to sour stimuli, hence, an increase in salivation should
Itr,4l
Llrill
h!,r{l
iitill
llL

occur which would initiate the swallow response in a more timely manner (Logemann et
a1., 1995). Increased salivation coresponds to the function of CN VII, the facial nerve.
Although CN VII is primarily motor, it contains sensory functions as well, which includes
saliva production for the oral cavity as well as taste sensation for the anterior portion of
the tongue. The increase in salivation further correlates with the idea that sensory input is
provided to the medulla to recognize that a swallow is being stimulated since the medulla
also contains the salivary nucleus which controls secretions. CN VII transports sensory
input from the taste buds on the anterior two-thirds of the tongue to the brainstem which
further transmits the information to the sensory cortex. Furthermore, CN WI innervates
the buccinator which prevents pocketing of food during consumption by pulling the
cheeks inward to prevent residue from collecting in the lateral sulci (Bhatnagar & Andy.
I ees).
Logemann and colleagues (1995) conducted a study which provides further
support for the use of a sour stimulus. Their study focused on the effect of a cold sour
bolus on the pharyngeal swallow. This idea arose from the clinical observations made by
Kagel and Leopold (1992). They noticed an increase in the organization of the oral stage
of the swallow, as well as a more efiicient reflex in the pharyngeal phase. The
participants of the study conducted by Logemann, et a1.(1995) included two groups.
Group I was made up of 19 CVA patients, Group 2 included eight patients with other
unspecified neurogenic diagnoses. The participants were given three boluses of 1 ml
liquid barium and three boluses of 3 ml liquid barium, swallowing after each bolus.
Additionally, the participants were given a mixture composed of 5OYoreal lemon juice
and 50Yo liquid barium to swallow in measurements of I ml and 3 ml. Three boluses of
each amount (lml and 3 ml) were given to each patient, with a swallow after each bolus.
A videofluorographic study was conducted during each swallow and tapes were analyzed
for the temporal aspects of the pharyngeal swallow. Outcomes indicated that a cold
sour bolus resulted in a reduction in the latency of swallow initiation in CVA patients. In

addition, the oropharyngeal swallow was observed to be more efficient with the cold sour
bolus, as evidenced by a decrease in swallow latency, and improved oral and pharyngeal
transit times. Logemann, et al. (1995) hypothesized that these results stemmed from the
heightened sensory imput provided to the brainstem and the coftex by the sour taste.
Since the sour flavor is a marked oral stimulus, the strong taste alerts the cortical
swallowing areas to the need to swallow. For participants in Group I (CVA), a decrease
in pharyngeal response time (PRT) was noted with a sour bolus as the bolus volume
increased. Participants in the study who had a neurogenic diagnosis other than CVA were
observed to have a reduction in aspiration resulting from application of a cold sour bolus.
Therefore, by providing a sour bolus, the efficiency of the resulting swallow may be
increased. Likewise, in this study all stimulation consisted of swabs frozen in lemon-
flavored ice. The idea behind this being that a lemon-flavored stimulus would provide the
most opportune environment for the elicitation of a quicker swallow response.
Deep Pharyngeal Neuromuscular Stimulation
A sour stimulus (frozen lemon swabs) is also utrlized during DPNS. The primary
areas which are targeted for stimulation are the lingual base, velar musculature, and
pharyngeal constrictors (Stefanakos, 1994). Nine steps are involved, each which
stimulates a different area of the oral structures. Each oral area is quickly swabbed with
the sour stimulus in a specific sequence. According to Stefanakos, gains toward the
restoration of the functional swallow are evident within 4 to 6 weeks.
The use of DPNS is recommended for patients with diagnoses including CVA,
early stage M.S., Parkinsonism, and Alzheimer's disease, closed head injury, and
neuromuscular insufficiency due to age. Patients who are not candidates for this program
include those who suffer from seizure disorders, patients who have experienced
abdominal surgery, patients with advanced Alzheimer's Disease or an advanced
degenerative neuromuscular disease, myasthenia gravis, patients treated with extensive
radiadion,'those with movement disorders, and those who are agitated Although
i rll
{{
llll
,ll{
ilI,1ri
{,,,

available materials on DPNS did not speciff as to why patients with these particular
diagnoses should not be treated with DPNS, it may be hypothesizedthx it is due to the
progressive degenerative nature of most of these illnesses. Additionally, it is believed that
those patients with seizure disorder should not participatein aDPNS program due to the
likelihood that it may serve as a catalyst for another seizure. DPNS may be a lengthy
process, hoWever, it would seem that it would provide stimulation to a variety of oral
structures which play an active role in the swallowing process.
Rationale for Current Study
' This study is necessary due to the fact that thermal stimulation is currently the
treatment technique most often used to treat dysphagia (Stefanakos, 1994). Its efficacy
has been neither completely proven nor disproven. Furtherrnore, no known efficacy
studies have been published on DPNS. By conducting efiicacy studies on the various
treatments utilized in therapy, we will be better able to serve the patients and provide
them with the treatmentthat is the most efficient and effective. In addition, efficacy
studies allow us to better educate patients, families, and physicians as to the nature of the
disorder and to provide more comprehensive services in remediating the problem" By
comparing DPNS to TGS, it may be determined which technique is more ef;Fective in
treating dysphagia without denying treatment to the patient.

Chapter III
Methods and Procedures
" In an effort to provide data on the effectiveness of a modified DPNS protocol, a
comparison was made between its effects and those of TGS. Two parameters were
compared. First, the delay in the initiation of the swallow reflex was timed to determine
which treatment method results in a more efficient triggering of the swallow. Second, the
difference in the rarrge of motion of lingual movements was judged to determine which
treatment method results in an improvement in the movement of the lingual musculature"
The idea of improvement of the lingual movement comes from the theoretical basis of
DPNS. Swallowing involves multiple cranial nerves including V, VII, IX, X, and )ilI
(Lugger, 1gg4). DPNS stimulates not only the faucial pillars, but also the tongue, palate,
uvula, and pharynx. Therefore, it may be inferred that since more cranial nerves are being
stimulated, DPNS will result in visible improvement in other areas of the swallowing
process, in addition to a more efficient triggering of the swallow.
Participants
This study utilized six participants. In an attempt to treat patients with similar
problems with dysphagia, criteria were established to guide the selection of participants in
this study. These criteria included an age of at least 60 years, a diagnosis of a single
CVA, the diagnosis of oral and pharyngeal dysphagia, a delay in swallow initiation of 4
seconds or greater, and the ability to follow commands. The limited sample size utilized
in this study was due to difficulty securing participants who met all criteria' For instance,
four other. stroke patients were considered for this study. Due to complicating factors

which ma;z have influenced their performance, such as extreme lethargy, the inability to
follow commands, and a new diagnosis of Parkinsonism, three of these candidates were
not chosen. The forth participant began the protocol, but was subsequently hospitalized.
All those who participated in this study had a diagnosis of cerebrovascular
accident (CVA), a diagnosis of oral and pharyngeal dysphagia, and a delay in swallow
initiation, The diagnosis of oral and pharyngeal dysphagia was determined through the
use of a modified barium swallow study. The participants were aged72 to 86, with a
mean age of 76 years. Three participants were male and three were female. Four subjects
(two males and two females) had suffered only a single CVA. Of these, two were left
hemisphere CVAs, one was a right hemisphere CV,\ and one had suffered a brainstem
stroke. The data collected on this last subject was not utilized in the statistical analysis
due to her inability to initiate a dry swallow on command and the absence of lingual
movements. Two participants had previous CVAs which occurred in the same area of the
br4in as the more recent insults. Both participants had been living independently prior to
the most recent insult, and had no overt effects of the first incident. However, it is
possible that amild dysphagia could have been present and the participants were able to
compensate for it without realizing its presence.
Participants were randomly divided into two groups. Both groups were given two
treatments of TGS and two treatments of a modified version of DPNS alternated over
four consecutive days. Group A received TGS on the first day. Group B received DPNS
on the first day. The two alternating groups were created to eliminate any chance that the
order of administration of the techniques might have over the results (Ventry &
Schiavetti, 1986). Therefore, the influence of treatment order had been minimized.
IMaterials
The materials required for TGS included one 4 oz. cup,2 oz. lemon italian ice,
and twenty 6" Q-tip swabs. The italian ice was melted and poured into the cup' The
swabs were inserted. The cup was wrapped in a plastic bag and frozen fot 24 hours'

Before use, the ice was placed in a microwave for 12 seconds to allow the swabs to be
separated.
Although Stefanakos (1994), recommends using frozen lemon glycerine swabs to
administer DPNS, for the purposes of this study the same materials and preparation
procedures were used for DPNS as were used for TGS. The reason for this modification
in'materials is due to clinical experience which would suggest that lemon glycerine swabs
may dry out the oral mucosa.
Procedures
TGS was accomplished by stroking each anterior faucial pillar five times with one
iced swab, beginning at the upper portion of the pillar nearest the uvula and stroking
downward. The TGS treatment consisted of twenty swabs'
According to Stefanakos (1994), DPNS consists of 9 stimulation steps: 1) Glide
swab across palatal pharyngeal musculature. The movement should begin on the weaker
side and cross overto the stronger side. Stimulate 1-3 seconds. 2) Beginning at midline,
swab the faucial arches laterally and down, then swab the uvula. Stimulate 1-2 seconds'
3) Swab across the tongue where the bitter taste buds are located. Stimulate 1-3 seconds
4) Stabilize tongue with gauze. Swab lateraltongue anterior to posterior' Stimulate 2-4
seconds. 5) Swab to the lingual apex along the lingual septum. Move posterior to
anterior. stimulate 2 seconds. 6) Swab the posterior pharyngeal wall. Stimulate 1-2
seconds. 7) Swab down the urula. Stimulate 1-2 seconds. 8) Swab from the base of the
anterior faucial pillars across the velum and down the lateral aspect of the uvula'
9) Apply swab to nasal spine, assess palatalreflex' The weaker side of the musculature
should be stimulated first on all steps. Pilot testing had revealed that some patients were
not able to complete all of the steps involved in DPNS" Therefore, for the purposes of
this study, DPNS was modified to include those steps which the patient was able to
tolerate. The steps the patients were able to tolerate were noted and analyzed as
necessary.

Baseline Measurements
A baseline measure of range of motion of lingual movements was judged by the
clinicians at the start of each session. Lingual movements which were judged included
lingual protrusion, lateralization to the labial corners, elevation, and lateralization to the
' buccal cavity,'' Lingual movements were judged on a scale of I to 4 signifying (1) as no
movement, (2) as mild movement, (3) as moderate movement, or (4) as signiflcant
movement.
A baseline measure of the delay in swallow initiation was collected over 3 dry
swallows. The baseline measure was collected immediately before the treatment was
administered on both days. Each swallow, including dry swallows, was timed using a
Sportline stopwatch (Model 220). Dry swallows were timed from the point that the
command to swallow was given until the larynx returned to resting position after the
swallow had been completed. Laryngeal elevation and return to rest was noted by the
clinician's index finger being placed on the larynx to detect laryngeal elevation and return
to rest. The best two baseline swallows were averaged for each day.
Techniques
At the initiation of each session, baseline measures were collected. This included
the rating of lingual movements and the timing of three dry swallows. The treatment
technique was then applied. Each treatment technique utilized twenty swabs. After each
swab was applied, the participant was given the command to swallow. Timing began
when the swab was removed from the anterior faucial pillars and the command to swallow
was given. Timing ended when the larynx returned to rest after the swallow had been
completed. Each swallow time was recorded. The average duration of swallow initiation
delay for the best two swallows was calculated for each treatment. After the stimulation
technique had been administered, the lingual movements were judged againto determine
if any'improverneni was visible. Improvement was judged utilizing the same scale as used

for the baseline measures. Whenever possible, the treatment was conducted with the
participant seated in a chair. However, in the case of patients who were confined to bed,
the position of the patient was documented for consideration during the analysis of the
treatment outcomes.
Reliability
. : The judges consisted of a speech-language pathologist with a certificate of clinical
competency in speech-language pathology and a graduate student clinician. Guidelines
for the rating of lingual movements were established by the judges. A rating of I was
defined as no movement observed across the lingual motions being judged. A rating of 2
was defined by mild movement, particularly movements performed with the blade of the
tongue rather that the tongue tip and a failure to approximate the target of the movement.
The third rating was defined as consisting of moderate movement with decreased range of
movement, uncoordination, and failure to approximate the target. A rating of 4 was
indicated by significant range of movement, coordination, and approximation of the
target.
Each judge individually marked a score sheet during baseline measures of lingual
movements and again after the stimulation treatment had been applied and lingual
movements were repeated. The judges then compared their findings. If a discrepancy
existed between the judges scores, the two scores were averaged.
Reliability, was established among the judges by individually rating the lingual
movements of a single participant. This participant's lingual movements were judged with
100% reliability. Subsequently, ten subjects were rated individually by the judges. These
data were utilized to determine the inter-rater reliabiliry of the judges, which was
determined tobe 82%o.
Method of Analysis
The dependent variables (the delay in swallow initiation and the range of motion
of the lingual movements) were compared across treatment types: DPNS and TGS. The

comparison was conducted using a multivariate analysis of variance (MANOVA). This
parametric test was chosen due to its use in comparing the variability of effects of
multiple factors between the treatments as well as within the treatments (Pannbacker &
Middleton, 1994). In addition, a Chi-square analysis was conducted to determine whether
or not a significant difference existed between the impact of TGS and DPNS on lingual
movements.

Chapter IV
Results
Data from five of the six subjects were analyzed to determine whether or not one
treatment technique was more effective than the other with respect to length of delay of-
swallow initiation and change in lingual movements . Datafrom the sixth subject were not
analyzeddue to the diagnosis of brainstem stroke and the inability of the participant to
initiate a dry swallow on command for baseline measures. However, all treatments were
completed with this participant and her individual findings will be discussed in detail.
Delay in Swallow Initiation
The averages of the two best baseline dry swallows were calculated for each
participant for each day. Likewise, the averages of the two best stimulated swallows were
computed for each participant for each day. From these averages, the percent ofchange
from baseline dry swallow to stimulated swallow was attained. This percent of change
was utilized in the MANOVA calculations (Statistica, 1995).
The results of the MANOVA revealed no significant diffFerence between TGS and
the modified DPNS protocol for improvement of delay in swallow initiation (see Table 1).
Nevertheless, all participants displayed some degree of improvement in speed of swallow
initiation, with the exception of subject # 3, whose percentages of change were basically
negative or 0 (see TableZ).

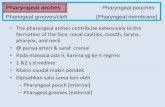
Table I
M NOVA Summary-of Effects for l\elay in Swallow Initiation
Effect dfEffect MS Effect df Error MS Error
TGS 1
DPNS I
Interaction 1
.0t4045
.00364s
.01300s
.044207
.034208
.053842
.317706
.106556
.241538
.603089
.760466
.648845
4
4
4
of
ch
ange
52
51
50
49
48
47
46
45
Dbyl DaY2 DaY3 Da
{- Series 1
Figure 1. Plot of Percent Change of Each Trial Over All Four Days

Table 2
-nasaine S *Af
SubjectAge Technique Baseline Yo Change
75 DPNS
TGS
DPNS
TGS
DPNS
TGS
DPNS
TGS
TGS
DPNS
TGS
DPNS
DPNS
TGS
DPNS
TGS
TGS
DPNS
TGS
DPNS
15.7 sec.
14.1 sec.
14.45 sec.
19.14 sec.
L56 sec.
1.7 sec.
1.45 sec.
1.47 sec.
1.85 sec.
6.8 sec.
2.8 sec.
2.3 sec.
3.7 sec.
4.2 sec.
1.25 sec.
2.0 sec.
7.5 sec.
4.15 sec.
13.2 sec.
9.6 sec.
3.9 sec,
6.85 sec.
2.15 sec.
9.7 sec.
1.61 sec.
2.35 sec.
1.45 sec.
T.62 sec.
1.85 sec.
2.25 sec.
1.5 sec.
1.75 sec.
.7 sec"
.65 sec.
.65 sec.
.75 sec.
2.55 sec.
1.4 sec.
2.7 sec.
1.25 sec.
75
51
85
49
-3
-38
0
-5
0
67
46
24
81
85
48
63
66
66
80
87
74

The lack of a significant interaction suggests that the difference between daily
outcomes was not significant..Nevertheless, an improvement in swallow response time
was exhibited on the third day, as shown in Figure 1. This improvment is not attributed to
either TGS or modified DPNS, since the two treatments were alternated between all test
days.
Figure 2 displays the average of all baseline dry swallows with the average of all
stimulated swallows of all participants, A large difference was evident between the
baseline dry swallows and those swallows which were produced immediately following
stimulation. Whilethis graph does not distinguish between treatment techniques, it does
demonstrate the amount of improvement achieved in swallow function after stimulation
was applied.
TI'6
me
4i
n3
S
92.c
Day 2
IDryDay3 Day4
ffi stimulated
Figure 2. Graph of Baseline Dry Swallows Versus Stimulated Swallows for All
Participants

Change in Lingual Movements
Change in lingual movements, for the purpose of analysis, was rated as 0 if no
change occurred or I if change did occur after stimulation. Improvement in lingual
movement was evident after stimulation, however, change did not seem to occur
consistently with either treatment. All participants exhibited improvement in lingual
movements with either TGS or modified DPNS except for subject #2,who was not able
to initiate a dry swallow on command, and whose data were excluded from analysis.
A Chi-square analysis of the lingual movement data was conducted. For each
treatment technique, a score of l0 was possible since there were five participants and each
participant received each treatment twice. Change in tongue movement occurred on7ll0
opportunities with TGS and on 6lT0 opportunities with the modified DPNS protocol.
The Yates corrected Chi-square revealed a calculation of 0,00 (p:1 0) (Statistica, 1995).
This finding would suggest stimulation did influence lingual movement; however, one
treatment was not necessarily more effective than the other in promoting this change.
Group Effects
As a group, no treatment technique was significantly better than the other in
improving the delay in swallow initiation or lingual movements. However, both
techniques did have an effect on the swallow response. The average change in swallow
response time for all participants was 43.6% for TGS and 49Yo for DPNS. A large effect
size (.80) was calculated for the modified DPNS protocol. The large effect size reveals
that modified DPNS created more change in the swallow response initially than TGS, and
had the sample size been larger, the results of the MANOVA may have been different.
As noted in Figure 3, the first modified DPNS treatment created a greater change
in swallow response than the first TGS treatment. The initial TGS treatment stimulated a
swallow response at a slower rate than modified DPNS. The results of the second
modified DPNS trial were consistent with those of the first trial. For TGS, improved
results wbre noted'on the second trial. Clinically, this indicates that a patient might

o/o
of
ch
ange
perform better with modified DPNS because it creates a greater change on the first use.
Eventually, TGS's perfbrmance approximates that of modified DPNS. Therefore, it
would benefit the patient to start offbetter and remain at a high level, than to start of at a
lower level and eventually attain a quicker swallow response;
52
48
46
44
42
40
38TRIAL 1 TRIAL 2
Day 1 & 2 of Treatment Each Tech.
-}* TGS _I- DPNS
Figure 3. Plot of Percent Change of Swallow Response Time for TGS and Modified
DPNS
Individual Effects
Table 3 summarizes information about each participant which is pertinent to
understanding some of the outcomes of this study. For instance, it provides lesion
location, time post onset, age, and whether or not the subject had sufFered a previous
CVA. These facts may account for some of the results of this study which are discussed
later.

Table 3
Individual Subject Information
Subject Site ofLesion Time Post Onset Prior CVA
1
2
J
4
5
6
75
72
77
74
77
86
Left Hemisphere
Brainstem
Right Hemisphere
Left Hemisphere
Right Hemisphere
Left Hemisphere
7 Weeks
2 Weeks
2 Weeks
2 Weeks
2 Weeks
6 Weeks
Yes
No
No
No
Yes
No
Subject #1 suffered a left hemisphere CVA. He also had a previous history of a
Ieft hemisphere CVA" but had no lasting effects from it, and had been lMng independently
prior to the most recent insult. This participant had a very effiortful swallow. Due to this,
he was able to elicit some, but not all of the dry swallows necessary for baseline measures.
The extreme effort required by this participant to initiate a swallow may be connected to
his inability to complete all stimulated swallows. When TGS was administere d, 6.6yo
(2130) of swallow opportunities were not completed. This finding would suggest that the
participant was not able to initiate a swallow reflex even after stimulation. On the other
hand, all of the swallow opportunities were completed when DPNS was administered.
This participant tolerated DPNS to step #4. Further steps were not completed due to the
participant's inability to tolerate the stimulus within the oral cavity for a lenEhier amount
of time. When applying TGS a tongue depressor was utilized to stabilize the tongue in
order to approximate the anterior faucial arches with the swab. As a result, the arches
could ncit always be stimulated as much as at other

27
times and this may have contributed to more of a swallow delay with TGS. Overall, this
participant'was highly sensitive to all stimuli. This would account for his inability to
complete all steps of the modified DPNS, and his inability to tolerate TGS to the anterior
faucial arches.
Change in lingual movements after stimulation was observed on Days I and 3
(modified DPNS) for particip ant #1. Improvement was noted particularly in lingual
protrusion. Overall, this participant's swallow response appeared to be quickest and his
lingual movements improved only when modified DPNS was administered, even though
he Could not tolerate the length of the entire stimulation procedure.
Particip ant#3had a diagnosis of a single right hemisphere CVA. This
participant's delay in swallow initiation was greater after stimulation than during baseline
dry swallows. This was true for TGS, as well as modified DPNS. The judges felt that
subject #3's decreased ability to focus attention on the task, which was a result of the
right hemisphere stroke, may have contributed to an increase in the delay of the swallow
reflex. In addition, this subject was treated in the evenings, while other participants were
treated during the day. Fatigue due to the time of day may have impacted his swallow
response. Overall, his swallow intiation appeared to be quickest when modified DPNS
was applied.
Participant #3 displayed a change in lingual movements with TGS on both
occasions and with modified DPNS on one occasion. Although tongue motion did
improve with both techniques, neither procedure appeared to be significantly more
influential than the other in causing the change. Again, attention to the task may have
affected his performance on lingual movements.
Participant #4, suffered a single left hemisphere stroke This subject tolerated
modified DPNS through step 8, although step 6 (swabbing of the pharyngeal wall) was
not tolerated due to a strong gag reflex. His baseline dry swallows ranged from 1.3
seconds to 13.4 seconds. This participant produced a dry swallow on command
ill
.H
ili{
lllnt
flrll
{l
f,

28
consistently over the four day period, indicating that his swallow may not be as effortful
or difficult to elicit as those of participants who could not produce consecutive dry
swallows. Stimulated swallows ranged from 1.2 seconds to 7 .7 seconds with TGS, and
from 1.7 seconds to 6.gseconds,with modified DPNS. Participant #4's swallow response
appeared to be marginallybetter with TGS than with modified DPNS, even though a
tongue depressor was utilized to allow the clinician access to the anterior faucial arches.
,ds a.result,,it was sometirnes difficult to fully approximate the arches with the swab. It
would seem that this may have a negative effect on the results of TGS, however, this does
not appear to be the case.
, A change in lingual movements for subject #4 wasnoted with TGS and modified
DPNS on Days 3 and 4. Improvement in the tongue motion was most obvious in the
lateralization. TGS may have been most beneficial for this participant since his swallow
response was quicker with TGS and it also resulted in an improvement in lingual
movements.
Participant #5 suffered arightmiddle cerebral artery stroke. This subject had
suffered an earlier CVA in this same area, but was unaware of it. The previous stroke
was discoveted when the participant underwent a CT scan of the brain for the more recent
incident when the old infarct was discovered. Prior to the latest insult, this woman lived
independently. Her swallow was similar to that of participant #2, who will be discussed
Iater. Their swallows were similar in that the oral phase was the most impaired. Subject
#5 could not tolerate her own secretions and had a highly sensitive gag reflex.
Upon stimulation, paticipant #5's swallow reflex was quite rapid, another similarity
between this participant and subject #2. When TGS was administere d,3}yo (L2la$ ot
the swallows were initiated before stimulation was completed. Twenty-five percent
(l0l3g) of the swallows during modified DPNS were initiated before stimulation was
completed. The information collected during this study was not sufiicient to determine
t:
why this occurred. It is possible that she had a natural need to spontaneously swallow
_
..11i
lii
iltlin
riI
li{
lltt
-iltillfl
iN
il

before stimulation was complete. It is also possible that the added sensory stimulation
had an effect on the swallow reflex. Modified DPNS stimulation was completed through
step 8 with the exception of step 6 due to the participant's highly sensitive gag reflex.
Overall, her swallow was quickest when modified DPNS was provided.
Change in lingual movements was noted each day after stimulation. This
improvement was noted primarily in tongue elevation and lateralization. Since her
swallow-was quickest with the modified DPNS protocol and lingual movements improved
equally with both techniques, modified DPNS may be the most beneficial treatment for
this participant.
Participant #6, was diagnosed with a left hemisphere stroke. She tolerated
modified DPNS through step 7, with the exception of step 6 (swabbing of the pharymgeal
wall). Stimulation caused the greatest change in the length of swallow initiation from
baseline swallows on Days 3 and 4. However, this change could have been due to
spontaneous recovery especially since this patient was six weeks post onset. This
paiticipant's dry swallows ranged from 1.2 seconds to'19 seconds. Stimulated swallows
ranged from 1.2 seconds to 15 seconds. Her swallow response appeared to be quickest
when DPNS was administered.
Change in lingual movements was noted only with TGS. This is surprising since
TGS provided no lingual stimulation. Improvement was noted primarily in lateralization
ofthe tongue.
As mentioned previously, the data collected on participant #2were excluded from
analysis based on the subject's diagnosis of a brainstem CVA and the inability to initiate a
dry swallow on command. She presented with a highly sensitive gag reflex aqd the
inability to tolerate secretions orally; in fact, she suctioned her oral secretions.
This participant's treatment began with TGS. On Days I and2, no dry swallow
was initiated on command. On Day 3, a dry swallow was initiated in 9.6 seconds. She
was not able to initiate another dry swallow during that session. On Day 4, she was able

to produce three dry swallows. When stimulated with TGS or modified DPNS, her
pharyngeal swallow reflex was rapid and ranged from 0.5 seconds to 18.4 seconds. The
average delay in swallow initiation was2.39 seconds when stimulated with TGS, and2.84
seconds when modified DPNS was administered. Step 7 was the furthest this subject
' tolerated in thdmodified DPNS protocol. This was partly due to the severity of her gag
and, for this reason, step 6 (swabbing pharyngeal wall) was omitted. Another possible
reason for lack of toleration for steps beyond step 7, was the rapid rate of her swallow
and the inability to prevent the swallow once stimulated. On 3.7Yo of stimulated
swalldws, she initiated a swallow before the stimulation was completed. The cause of this
occurrence cannot be determined from the data collected in this study, but may be due to
the sensory input from the stimulation or simply due to the natural need to spontaneously
swallow, however, spontaneous swallows were not frequent with this participant and
contributed to her difficulty managing oral secretions. A swallow before stimulation was
completed occurred only on Days 3 and 4, which indicates that it may have been due to
spontaneous reiovery or improvement caused by the stimulation over the previous two
days. Spontaneous recovery is likely since stimulation was initiated at two weeks post
onset. Overall, her swallow response appeared to be quickest when stimulated with TGS.
Participant #2 presented with virtually no lingual movement. No change was
noted in lingual movement as a result of stimulation on any day This may be due in part
to the severity of this participant's oral phase. This idea is supported by this patient's
diagnosis of a brainstem stroke and the fact that cranial nerve )([I, the hypoglossal which
is responsible for tongue movement, is located in the brainstem. TGS may be the most
beneficial treatment technique for this participant since neither treatment appeared to
affect her tongue movement and TGS stimulated the quickest swallow response.
There were several trends noted in the discussion of the individual data Age did
not appear to be associated with the participants' performance with either procedure' The
two female subjects displayed marginally more change between baseline swallows and

stimulated swallows than the males, however, it was probably not a significant difference.
The participants *ho suffered right hemisphere infarcts displayed improvement in lingual
movements'more frequently than those who suffered left hemisphere CVAs. There may
be two possible explanations for this occurrence. The first possibility is that the left
hemisphere p'articipants had a mild oral apraiawhich had not been identified due to the
limited exainination of tongue motion. This oral apraia may have interfered with the
precision of the tongue movements. Secondly, the difference between the lesion sites may
have impacted lingual movement. Those with a left hemisphere lesion may have had more
motor damage than those with a right hemisphere lesion. Nevertheless, further testing
will be needed to see if these observations hold across large subject groups.

Chapter V
Discussion and Conclusions
Although a definite difference between TGS and modified DPNS was nqt clearly
evident, the data presented some interesting trends. Also, the lack of a difference
between the two treatments may be due to uncontrolled factors this study. These trends
andinfluencingfactorswillbediscussedbelow.-
Swallow Initiation
Although a significant difference was not oUr.*.a bet*e", TGS and modffied
DPNS with respect to decreasing the delay in swallow initiation, both techniques certainly
impacted the swallow. The majority of participants (a/5) showed some change in the
swallow response when stimulated with either technique. It was not too surprising that
modified DPNS had a greater effect on the swallo* response early in the recovery
process because it presumably stimulates more cranial nerves. In addition, it may provide
more sensory awareness to the brainstem that a swallow needs to be produced' However,
it does not stimulate the anterior faucial arches for as long a period as TGS. It is this area
that Pommerenke (lgll)states creates a swallow response in the most people, most
often.
Lingual Movements
The Chi-square analysis failed to identify any one treatment technique as being
more effective than the other in improving lingual movements. A change in tongue
movement was noted after both treatments at various times during data collection' In
other words, although both treatment techniques stimulated an improvement in tonguet?

movement, the results were not sufficient as to attribute the improvement to one
technique and not the other. This variability in linguat response may be attributed to the
fatigue the participant may have been experiencing as a result of stimulation. TGS and
the modified DPNS protocol both require the participant to swallow 23 times
ionsbcritively. Many of the subjects had effortful swallows which required extra tongue
'movement to pfoduce the swallow. All of this necessary tongue movement during the
swallowing process may have fatigued the lingual muscles and affected the lingual
outcomes after stimulation.
Attentioii to task may have also been an influencing factor. Those who had
difiiculty focusing their attention on the task may not have performed the tongue
movements as well as physically possible. However, this hypothesis is flawed by the fact
that the right hemisphere participants, who would be expected to have attention deficits,
actually displayed improvement more frequently than the left hemisphere participants.
Furthermore, time of day may have influenced the results of participant #3 He was the
only participant who did not show improvement in swallow delay after stimulation. He
was also the only subject who was treated in the evening. All other subjects were treated
in the morning. Due to the time of day, this participant may have been experiencing
fatigue.
All patients were able to perform the lingual movements on coflrmand, however, a
mild oral apraiamay have also influenced the adequacy of these movements, at least for
those with left heirisphere lesions. This could be why those participants who had right
hemisphere'lesions displayed improved lingual movements more often than those who had
suffered a left hemisphere lesion.
Summary of Individual Effects
The results ofthe individual participants was quite interesting. Most participants
had a quicker swallow response when modified DPNS was administered. This is
interestihg since modified DPNS provides less stimulation to the faucial arches than TGS,

and, as Pommerenke's (1928) research indicates the anterior faucial arches stimulate a
swallow in more people more often than any other area in the oral cavity. The uvula and
velum, which are stimulated in modified DPNS are believed to be much less sensitive.
Another interesting finding of this study was that none of the participants could
toleiate the entire'modified DPNS treatment and it had, for the purposes of this study,
already been moclified from the original DPNS technique into a shorter version. The
complete modified DPNS technique was not tolerated for two reasons. First, most
participants could not maintain the stimulus within the oral cavity for the length of time
which was required to complete all steps. If the stimulus was in the mouth too long, it
usually resulted in lingual retraction or the patient pulling away from the clinician.
Secondly, most patients had a sensitive gag reflex which prevented any stimulation
beyond the anterior faucial arches, so step six could not be completed. Finally, the
original DPNS technique called for stimulation of each oral area for I to 3 seconds
depending on the structure (Stefanako s,1994). This procedure was not followed as such
in this study because pilot testing revealed that the participants could not tolerate the
stimulus being in the mouth that long. Therefore, for the purposes of this study, each area
(i.e. velum, uvula, anterior faucial arches) was swabbeJ momentarily, stimulation was not
maintained.
All participants except one, the subject who had suffered a brainstem CVA,
displayed some change in lingual movement at least once with either techniqug. A
similarity that occurred among all participants with respect to tongue motion was that
improvement typically occured inlateralization and protrusion. This was to be expected
on days when modified DPNS was applied since the tongue is stroked laterally in that
technique. Additionally, protrusion is promoted with the modified DPNS procedure since
the lateral stroking motion is in an anterior-posterior direction which also facilitates
protrusion. However, these same similarities in improvement of lingual movement were
noteil on days when TGS was administered. This was not expected and was not noted

35
during pilot testing for this study. Therefore, it is hypothesized that the improvement in
lingual movement noted during TGS was due to the stimulation provided to the tongue
simply during the act of swallowing. The tongue motion required to produce the swallow
during TGS may have stimulated the tongue enough to create an improvement in the
overall lingual movements.
TGS Versus DPNS'
Eachtechnique has its advantages and disadvantages. The merits of TGS are that
it'is a quick procedufe. It does not require the patient to tolerate a stimulus for a lengthy'',,,'
amount of time. This'may be beneficial in that the patient would not feel the urge to pull
away from the clinician as was sometimes the case with modified DPNS. Modified DPNS
is a lengthy procedure and not all participants were able to tolerate the stimulation for the
necessary duration. This may create anxiety and discomfort for the patient, if they were
not able to complete the procedure.
TGS directly stimulated the anterior faucial arches, which has been purported to
be the most influential area of the oral cavity in eliciting a swallow response
(Pommerenke, 1928). Modified DPNS stimulated the anterior faucial arches as well, but
it was for a shorter amount of time. Further investigation is needed to determine what
effects the length of stimulation to the anterior faucial arches has on the swallow.
A disadvantage to TGS was that it was sometimes difficult to directly approximate
the anterior faucial arches with a swab, A tongue depressor was used which may have
been uncomfortable for the patient.
Also, TGS focuses only on the pharyngeal swallow response, while oral sensation
is also important to initiating a pharyngeal swallow reflex. On the other hand, modified
DPNS stimulates both the oral and the pharyngeal phases of the swallow. In addition,
several participants indicated that they preferred having the tongue swabbed, particularly
because their mouths were dry and swabbing provided some moisture.
rt

III:-
I
i3
II1,.. .,i"iI
I
d
i"- t -
i
A drawback of DPNS is that the population it is recommended for is limited.
Stefanakos (1994) advises against the use of this procedure with advanced Alzheimer's
patients, those with seizure disorder, advanced neuromuscular disease, myasthenia gravis,
or those who have movement disorders or who have received radiation treatment to name
'. ' " a few. The literature on TGS did not indicate a population with which it should not be
used.
" : Cirmpdrison of the Present Findings with the Current Literature
The results of TGS found in this study concur with those in the current literature
in thiat TGS did have an immediate impact on the swallow. In the study byLazzura and
her colleagues (1986), it was determined that thermal stimulation created an improvement
in the swallow reflex in 23 out of 25 participants. Similarly, in this study stimulation to
' ' the anterior faucial arches improved the swallow response in the majority of participants.
" Rosenbek and others (1991) explained that in their study, an immediate effect of
cold stimulation was evident on the swallow reflex. This study provided evidence of an
imrnediate change in the swallow as well. The change was manifested-statistically as
percentages of change in the speed of the swallow. The measurements used to calculate
the percentages of change were collected immediately after stimulation was administered;
thus indicating that the speed of the swallow was immediately impacted by the stimulation
when compared to swallows performed without stimulation.
Pommerenke's research (1928) provided a foundation for TGS since he found that
the anterior faucial arches stimulated a swallow most frequently in most people. He also
found that the velum and uvula, which are stimulated in modified DPNS, were not very
effective in stimulating a swallow. The results of this study indicated that both TGS and
modified DPNS stimulated a quicker swallow reflex and that one technique did not do so
significantly more than the other. Therefore, this study did not completely concur with
the research completed by Pommerenke. One reason for this outcome may be because
modified DPNS stimulated the anterior faucial arches, just not to the same extent as TGS.
l4
iI

However, perhaps this limited amount of stimulation was enough to create a change in the
swallow response.
To date, no data had been published on DPNS. Some indication of its
effectiveness is necessary since clinicians are using this technique daily. This study
presents a basic finding that the modified DPNS protocol creates an immediate change in
the swallow response; however, further research is needed in this area. Future studies
'fshodd target the effectiVeness of the complete DPNS procedure, not the modified version
utilized in this study. Additional investigation should be made into why none of the
participants in this study could complete all the steps of the modified version.
Factors Influencing the Results of this Study
There are several possible reasons for the lack of a significant difference between
-these two techniques. The first is the sample size. The small sample size used in this
study was due to difficulty finding participants who met the criterion for participation.
Criteria such as a diagnosis of only one stroke omitted many possible candidates.
Participants with only a single CVA are ideal for a study such as this. If multiple stroke
patients were used, it would be more difficult to rule out the lasting effects the previous
CVA may have had on the swallow. Most potential participants had suffered more than
one stroke so that a previous history of dysphagia could not be ruled out. Additionally,
attrition of the potential sample population occurred for several reasons. Participants
were hospi talizedfor medical complications unrelated to this study. Other possible
candidates were unable to follow commands. Additionally, influencing diagnoses, such as
Parkinson's disease, were made. Degenerative diseases such as Parkinson's disease were
not utilized in this study due to the nature of the illness. It is a progressive disease and
improvement is not expected. Four possible candidates for this study were not utilized
due to these factors.
Having only a single CVA diagnosis was also important to this study. When a
participaht had multiple CVAs it was difficult to rule out the effects the previous stroke

may have on the outcomes of the study. For instance, a patient may have had limited
tongue movement from a previous stroke and may not have even been aware. Also, they
may have had a prior degree of dysphagia, for which they naturally compensated.
However, this factor limits the improvement in the swallow function or tongue movement
which can be expected with treatment.
'Two of the participants in this study had suffered previous CVAs. To the best of
the judges'knowledge, these participants did not have previous swallowing difficultieS, -
To verifi this hypothesis, information was collected through medical history and interview
of the participants. However, it is possible that the participants may have had a mild
dysphagia and had been compensating for it witho ut realizinga problem existed.
The duration of stimulation is another factor which may have influenced the -.
outcome of this study. Each participant received each technique for two days. However,
more frequent stimulation, perhaps two or three times per day, and stimulation which
took place over time, perhaps several weeks, may have provided results that differed from
those obtained in this study.
Twenty swabs per treatment session was a randomly chosen number of stimuli.
Treating a participant with more or less swabs per session may reveal different results.
Twenty swabs may fatigue the patient and negatively affect the swallow. On the other
hand, too few swabs may not provide enough stimulation to cause improvement. Further
study is needed to determine what effects more or less stimllation may have on the
swallow.
Additionally, treating a participant with only one treatment technique may yield
distinctive results. The consistency of a single technique may improve the function of the
swallow. When treatments are alternated, the same nerves and muscles may not be
continually stimulated and may not recover as fully as if they were stimulated regular$'
Another possible cause for the lack of differing results may be the participants'
The partlcipants in this study varied widely in their abilities. The oral phase (i'e', the

lingual movements) of some participants were much worse than those of others.
Therefore, since the deficit was greater, the opportunity for displaying improvement may
have been hampered by weakness. Had this study continued for a longer period of time,
more improvement may have been noted in lingual motion. Also, it could be stated that
since the deficit was greater, the participant had more room to improve and so they
should have a more marked increase in performance than the milder patients.
Likewise, the pharyngeal phase of the swallow was affected in the same manner.
Some participants could not elicit a dry swallow on cofltmand, others produced a
swallow with ease. Furthermore, increased effort may have impacted the ability to
produce a stimulated swallow in a timely manner since the ability to generate a swallow
was more dfficult for some participants than for others.
The rating of lingual movements was a factor in the lack of a significant outcome
in changing tongue movement. Although the ratings were based on guidelines, they were
subjective, nonetheless. Videotaping the lingual movement portion of each session may
have resulted in more accurate ratings. Likewise, although the same clinician
administered all stimulation techniques, each patient varied in the amount of stimulation
they would allow. Some patients had a strong gag reflex which hampered stimulalion;
others'could not tolerate a stimulus for the necessary amount of time. Differences in
either of the latter two factors would result in some participants receiving stimulation for
a longer time period than others. Increased stimulation could possibly result in a quicker
swallow.
Conclusions
Although this study did not reveal a significant difference between TGS and
DPNS, it did suggest several areas for continued investigation. Directions for future
research would include controlling more specifically for site of lesion in CVA patients.
This type of control would allow for more similarity in the presenting dysphagia
symptonis. It would also simplify the interpretation of results since change could be more

directly attributed to the treatment technique as opposed to differences that could be'
related to site of lesion.
Future research may eventually focus on expanding the selection criteria for TGS
and DPNS to include patients with other neurological diagnoses. DPNS is not
recommended for patients with seizure disorder, movement disorders, myasthenia gravis,
and other illnesses (Stefanakos, 1994). The literature on TGS did not indicate specific
populations that it should not be used with. Nevertheless, a large portion of the
dysphagia population includes those with neurologically based diseases. These
neurological diagnoses include Parkinson's Disease, Multiple Sclerosis, Alzheimer's
Disease and traumatic brain inju.y among others. Some form of treatment is needed for
these patients. The effects of TGS and modified DPNS must be investigated in subjects
with these illnesses in order to effectively treat dysphagia.
An interesting finding in this study was that modified DPNS made an initial change
in the swallow response time that was greater than the change produced by TGS. By the
second administration of either treatment, both techniques elicited a similar degree of
change in swallow initiation. Although TGS showed great improvement on the second
administration, it is not known whether or not this trend would continue. Modified
DPNS remained constant over two trials, however, it is not known whether or not this
tendency would continue either. Further research is necessary to determine whether or
not these two treatments continue to maintain similar changes in swallow function over
time. It is possible that one or the other may continue to increase the speed of the
swallow reflex. It is also possible that one or the other treatment technique may not
continue to be as effective over time. Research taking place over an extended period of
time is necessary to make known the long-term effects of these two treatment techniques.
Future research also needs to focus on lingual movements. This study has
provided evidence to suggest that lingual movements generally improve after stimulation.
::

4t
Further research must focus on what aspect of oral stimulation created the noted change
in tongue movement.
Finally, this study did not investigate the long-term ef[ects of either technique.
Immediate impact on the swallow is irrelevant unless stimulation is being provided during
meals. Long-term studies are needed to determine whether or not stimulation has a
lasting effect on overall swallow efficiency. Do these techniques facilitate improvement of
the swallow that lasts even when stimulation is not provided directly? This is a question
which must be answered.
TGS and DPNS are being used in the daily treatment of dysphagic patients, In
order to best treat those patients we must investigate these techniques further. This study
provided a basis for further research in this area. It raised additional questions about TGS
and DPI.[S. Namely, why could none of the participants tolerate the entire DPNS
procedure? Also, both treatments were similar in their effect on the swallow by the
second treatment. Will those results continue over time? These questions may be
answered by future studies. To justify treatment of the dysphagic patient with stimulation
techniques, we must continue to search for the best possible treatment procedure.

42
References
Bartlett, J. G. & Gorbach, S. L. (1975). The triple threat of aspiration pneumonia
Chest, 68,560-565.
Bhatnagar, s. c. & Ardy, o. J. (1995). Nerrroscience for the studv ofcommunicative disorders. Baltimore: williams and wilkins.
capra,N. F. (1995). Mechanisms of oral sensation. Dysphaqia, 10, 235-247.
cohen, J. (1992). A power primer. psychological Bulletin, I 12, 155-159.
Finegold, S' M. (1991). Aspiration pneumonia. Reviews of Infectious Diseases,
LL3737-742
Kagel, M: & I eopold, N. A. (L992). Dysphagia in huntington's disease: A 16 year
retrospective. Dysphagia, 7- 106-l l4
Kahrilas, P. J. (1993) Pharyngeal structure and function. Dysphagia, 8, 303-307 .
Lazzara, G. L.,Lazarus, c., k Logemann, J. A. (19g6) Impact of thermal
stimulation on the triggering of the swallowing reflex, Dysphagia, l, 73-77.
Logemann, J. A. (1983). Evaluation and treatment of swallowing disorders. San
Diego: College Hill Press.
Logemann, J. A. (1986). Treatment for aspiration related to dysphagia: An
overview. Dysphagia, l- 34-38,
Logemann, J. A. (1993). Manual for the videofluorograohic study of swallo
(2nd ed.). Austin, Texas: Pro-Ed.
Logemann, J. A. (October, 1995). Swallowing disorders: Diagnosis and treatment
strategies. Symposium conducted at Seattle, Washington.

43
Logemann, J.A., Pauloski, B.R., Colangelo, L.,Lazarus, C., Fujiu, M., &
Kahrilas, P. J. (1995). Effects of a sour bolus on oropharyngeal swallowing measures in
patients with neurogenic dysphagia. Journal of Speech and Hearing Research, 38, 556-
563.
Lugger, K. E. (1994). Dysphagia in the elderly stroke patient. Journal of
Neuroscience Nursing, 26, 78-84.
Martin, B. J., Corlew, M. M., Wood, H., Olson, D., Golopol, L. A., Wingo, M.,
&-'Kirnidni, N. (1994):' The association of swallowing {y.sfunct-io-n and aspiration
pneumonia. Dysphagia, 9, l-6.
Neumann, S., Bartolome, G., Buchholz, D., & Prosiegel, M. (1995). Swallowing
therapy of neurologic patients: Correlation of outcome with pretreatment variables and
therapeutic methods. Dy:;phagia, 10, 1-5.
Pannbacker, M. H. & Middleton, G. F. (1994). Introduction to clinical research
in communication disorders. San Diego: Singular Publishing Group, Inc.
Pommerenke, W. T. (1928). A study of the sensory areas eliciting the swallowing
reflex. American Journal of Physiology, 84, 36-4T.
Rosenbek, J. C., Robbins, H., Fishback, 8., & Levine, R. L. (1991). Ef;tects of
thermal application on dysphagia after stroke. Journal of Speech and Hearing Research,
L4*1257-1268.
Selinger, M., Prescott, T. E., & Hoffinan,I, (1994). Temperature acceleration in
cold oral stimulation. Dysphagia, 9, 83-87.
Statistica [Computer software]. (1995). Tulsa, OK: Statsoft, Inc.
Stefanakos, K. H. (1994, March). Deep pharyngeal neuromuscular stimulation,
Symposium conducted at the meeting of the Dysphagia Workshop on Deep Pharyngeal
Neuromuscular Stimulation, Tampa, Florida.
Terry, P. 8., & Fuller, S. D. (1989). Pulmonary consequences of aspiration'
Dysphagia,3, 179-183"

44
. ' -. ' . - .' Veig S, L. & Logemann, J. A. (1985). Swallowing disorders in persons with
cerebrovascular accident. Archives of Physical and Medical Rehabilitation, 66, 372-374.
and audiology (2nd ed.). New York: Macmillan Publishing Company.
ed.). Englewood Cliffs, NJ: Prentice Hall.