EDITORIAL - Sebbin Deutschland · EDITORIAL The Asia Pacific region includes many poorly exploited...
Transcript of EDITORIAL - Sebbin Deutschland · EDITORIAL The Asia Pacific region includes many poorly exploited...

Issue19
The plastic surgery newsletter from Groupe SEBBIN
L’EXPANDER
www.sebbin.com
ISSN
227
4-32
51
O c t o b e r 2 0 1 6
(by Brice Vignon, Director of Sebbin Asia
EDITORIALThe Asia Pacific region includes many poorly exploited
countries in the field of restorative and reconstructive surgery. The Sebbin Group today affirmed its commitment to accelerate its development with the creation of a new office in Bangkok in July 2016. Surgeons and patients from India, Japan, Australia and the 600 million inhabitants of the ASEAN bloc (Vietnam, Malaysia, Thailand, Singapore, Indonesia, Cambodia and
Laos), the latest global economic blocs, will benefit from our innovative solutions.
With high-quality products, the Sebbin Group aims to provide optimal security for its partner surgeons and their patients. The imminent launch of our new range of round implants with Integrity high-strength gel illustrates
our ethical approach. To reinforce our commitment, we have begun a new 10 years study with the largest cohort of patients ever studied in Europe.The opening of our Asian subsidiary will also share the knowledge of our highly experienced “Sebbin University” faculty with local experts. I am very proud to have the opportunity to contribute to this new subsiduary of the Sebbin Group by bringing the fruit of my international Asia-focused experience in the field of aesthetic medicine.
We will be delighted to present our projects at the iSAP Congress in Kyoto (Japan) and during other events in the Asia-Pacific region in the near future. Meanwhile, you can find more information in the columns of this issue of the Expander.
I hope you enjoy l'Expander.

2
from Doctor Julien GlicensteinTHE WORD
The one-hundred year anniversary of the facelift. For nearly half a century, it consisted of excising the skin after subcutaneous loosening (to a greater or lesser degree). Mitz and V. M. Peyronie studied the superficial fascial muscular system of the face (SMAS) and its role in 1974, and showed that deep features were involved in facial ptosis. The results of rejuvenation operations have improved, but even though several modern techniques are able to correct facial wrinkles, the neck remains wrinkled, as can be observed when looking at older stars on television.Correcting neck wrinkles is still a difficult task.
Daniel Labbé, who has a great knowledge of facial anatomy, analyses the causes of cervical ptosis and offers highly satisfactory personalised solutions.
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Neck liftDocteur Daniel Labbé .................................... p3
Eponyms :McGregor's flap and Millard's flap............................................................................ p8
The ideal buttock ......................................... p9
Yesterday / Today:Syndactyles ................................................... p10
Flashback on the historyof breast augmentation:The first silicone implants ......................... p11
CO
NTE
NTS
OF
Issue 19
(

3
NECK LIFTDoctor Daniel Labbé, Plastic Surgeon
4 place Fontette, Centre hospitalier privé, Saint Martin Ramsay GDS
L’EXPANDERInvited guest of(
INTRODUCTION
The neck lift has evolved over the last thirty years, going from a simple subcutaneous facelift to under platysmal facelifts with a large platysma and SMAS flap and transferred sections of the same muscle. Many authors continue to believe in platysma incisions, resections and flaps.
In recent years, we have returned to simpler and safer solutions that consist primarily of lateral repositioning of the muscle, more or less associated with the area under the chin. This is a return to SMAS plications and lateral repositioning originally described by Aufricht (1) and Guerrero Santos (2).This is a conservative treatment which aims to reconstruct the original anatomy and reposition the various structures to their original place.
We propose, in the short article that follows, a summary of techniques and indications
TECHNIQUES
1. Lateral repositioning or platysma suspension
Still useful, it can be performed alone or in combination with other rejuvenation techniques. Its aim is to reposition the platysma to its original position from where it had slipped by reconstructing the platysma-auricular ligament (3)
which laterally suspends the platysma.This technique is based on anatomical studies (4) and literature data (5) (6) (7).
It involves reconstructing the platysma-auricular ligament
which is the posterior lateral suspensory ligament of the platysma, lying between the posterior and upper edge of the muscle and Lore's fascia or the tympano parotid fascia which is one of the ways of fixing the parotid and located in front of the inter tragienne notch.
Docteur Daniel Labbé
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
IN PRACTICE:
After an approach more or less forward and up, depending on the associated facelift, the subcutaneous detachment is classic. The key point identified preoperatively and drawn on the first skin fold of the neck, is looked for in the plan of skin detachment using a hook (stronger than a Gillies hook). A key point is a non-absorbable suture placed below and above the platysma through a straight needle, (to obtain a progressive folding effect accordion platysma) and it is set after shaping the right needle to make it curve to the Lore' fascia. Lore's fascia is located in front of the ear, or more specifically, before the inter tragienne incision. It is taken together without entering the cartilage leads, about 10 mm in depth (the trunk of the facial nerve at this level is 25 mm deep), ensuring that the downward pull on this point does not entail any displacement of the earlobe (8). A second key point of plicature is placed on the SMAS in the manner of Tonnard and Verpaelle when the cervical lift is integrated in a cervico facial lift.
With these two key points, the plicature of SMAS and platysma can be achieved: for the neck, starting on the Lore's fascia, ahead of the inter tragienne incision with barbed threads (to better distribute the tensions, being less ischemiant) in a single suture.

4
As seen in Figure 1 (a and b), the lateral repositioning of Platysma will rebuild the platysma-auricular ligament of the digastric and recreate the anterior edge of the sterno-mastoid.
The key point, which is found by using a hook, is consistently on the first skin fold neck which has dropped through ageing but originally located at the heights of the hyoid bone, that is, say at the apex of the chin neck angle.
The lateral fastening suture begins at the level of the Loré fascia where it is inserted and fixed to the posterior edge of the platysma membrane, on the anterior edge of the sternomastoid cleido up to the limits of subcutaneous detachment.
Then, on top, the plication of the platysma is anchored on the parotid fascia which is fixed, without need for resection of SMAS, especially when using the barbed thread.
Then, excess skin is redraped conventionally and using Pollok points modified by continuous suture which thanks to the barbed absorbable thread avoids the use of drainage.Cutaneous suture is classic (9).
2. The digastric corset
This involves rebuilding the floor of the mouth which has become distended over time and protrudes between the two anterior abdominals of the digastric.
It is indicated whenever there exists a distension of the mouth floor and / or a false appearance of double chin. It may be associated, of course, to a build up of superficial sub platysmal fat (fat which when, pinched between two fingers, does not escape during contraction of the platysma) and / or resection of fat under platysmal (fat which when, pinched between thumb and forefinger, escapes during the contraction of the platysma).
An under-chin approach of 4 cm, typically moved by 3 mm in respect to the fold under the chin, gives very good prospects for the region; detachment after hydrodissection (10) with adrenaline serum of 1mg for 1000 (about 120 cc) is made with Trepsat scissors within the sub platysmal.
Then the two platysmas, interdependent at the midline
by merging their membranes, are separated to allow detachment under platysmal approximately 20 mm laterally to uncover the previous mid-section of digastric muscles.This lateral separation does not exceed to the level of the hyoid bone.
To increase the prominence of the region, the platysma can be incised on each side, right under the 10mm mandibular insertions. It will be re-sutured after effecting the digastric corset.
Depending on the type of neck, inter digastric fat (under platysmal) will be resected in a light or aggressive manner, leading to a hemostasis and leaving some tissue on the mylohyoid to avoid lymphatic leakage during later operations.
The two anterior abdominals of the digastric are sutured to each other starting at the bottom just above the hyoid bone and fixing both to the sub hyoid membrane. The first key point brings the two abdominals to the full height of the region under the chin (11); it is sufficient to consolidate the corset by achieving a continuous nylon suture or better a barbed thread (which hooked on each pass reduces the cutting effect on the muscle). This suture brings together the anterior abdominals of the digastric and the mylohyoid muscle in depth to rebuild the mouth floor and avoids dead space
Fig. 2a and 2b: on an anatomical dissection of the region under chin, we see the effect of the key point between the previous two anterior abdominals of the digastric and its attachment to the sub hyoid membrane and above the point of the suture fixed in depth to the mylohyoid.
This suture must take the anterior abdominals of the digastric over a more or less large area and the mylohyoid muscle to rebuild the mouth floor and avoid dead space where a hematoma or a lymphatic leakage may occur
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Fig. 1a Fig. 1b
Fig. 2a Fig. 2b

5
3. Indications
Only a precise pre-operative examination will give appropriate indications:
- It must include an analysis of deformations and comparison with previously taken photos (at around age 30), noting the depth of the neck-chin angle, identify the first fold of the neck which is the level of original neck/ chin angle, indicate the degree of smoking and also any scarring on the neck that might have an impact on the skin's vascularisation.
- A comparative analysis of the right and left sides at rest and in contraction, often very different, especially for the platysmal bands.
- An analysis of changes in fat distribution (pre and retro platysmal fat in the region under chin).
- A simulation of the lateral repositioning platysma noting the effect it has under the chin (Fig 4), by asking the patient to swallow to see the effect on the mouth floor (Fig 5).
Facing the patient, the first skin fold of the neck can be identified. The key point can be found in this first fold which will allow the simulation of the lateral repositioning of the platysma by performing a traction in the axis of the platysma-auricular ligament; if there is good definition of the neck and chin neck angle, reliefs and, in
particular, the mandibular edge and the front edge of the sternocleidomastoid muscle, it will support a suspension platysma.
If, on the other hand the region under chin is not well treated by this lateral repositioning, that is a first indication of an access point under the chin and for the use of a digastric corset.
Fig. 4: it can be seen in this picture that the lateral repositioning has a clearly insufficient effect on the region under chin, an indication for a digastric corset.
This indication is confirmed by the simple manoeuver of asking the patient to swallow, then raise the base of his mouth and improve his chin neck angle, confirming the indication of digastric corset and platysmal.
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Fig. 3a and 3b: schematic representation of the reconstruction of the mouth floor of the digastric and platysmal corset and the filling of dead space.
Then, the platysma is reinserted by a corset on the digastric, before reconstructing the retaining ligaments between the platysma and digastric (12) which were severed during the lateral separation and also to avoid any inter muscular dead space.The incision under the chin is then closed with a continuous intra-dermal suture for 8 days (13).
Fig. 3a Fig. 3b
Fig. 4
(

6
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Fig. 5a: side reposition simulation showing an insufficient result on the chin neck angle.
Fig. 5b: shows good definition of chin neck angle after asking the patient to swallow.
Of course, as we have seen, the indication of an isolated cervical facelift is relatively rare because of neck ageing is most often linked with ageing of the face and will be associated, from case to case, with a SMAS facial plication and its attachment to the parotid fascia.
Fig. 5a Fig. 5b
4. Associated gestures
We also use botulinum toxin to prepare the intervention and rest the muscles of the angle of the mouth and platysma before surgery, and also to ease them a little during the healing phase, avoiding excessive traction on deep sutures during this period.
Fig. 6 (a, b, c, d): cervico facial lift pre and post operative, front and profile, before and after digastric corset and platysmal by under chin approach and lateral repositioning by platysma suspension attached to the fascia of Lore's fascia and the reconstruction of the platysma-auricular ligament.
Of course, as we have seen, the most common associated motions are: aspiration of more or less extensive superficial cervical fat but also lipostructure of the chin (this can often improve the chin neck angle increasing discreetly chin projection) lipostructure the rest of the face, especially blepharoplasty increase and cheekbones.
Fig. 6a Fig. 6b Fig. 6c Fig. 6d
CONCLUSION
We repeat that only a specific pre operative examination can allow an accurate diagnosis and therefore an effective rejuvenation of the neck.This clinical study will enable us to choose between the techniques of isolated or associated lateral repositioning, and an under chin approach (called open technique) for
the reconstruction of a distended mouth floor, using the digastricus corset and the “refixation” of the platysma on this corset to fix the position and depth of the chin neck angle, guaranteeing the resulting stability.
The purpose of this rejuvenating cosmetic surgery is, to paraphrase H. Gillies, to reposition the tissues in their anatomical position in a lasting fixation.

7
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Ref. 1. Aufricht, G. Surgery of excess skin of the face and neck. Presented at the 2nd International Congress of Plastic Surgery. London: Churchill Livingstone, 1960. 2. Guerrero-Santos, J. The role of the platysma muscle in rhytidoplasty.3. Furnas DW. The retaining ligaments of the cheek. Plast Reconstr Surg 1989; 83(1); 11-6. Clin. Plast. Surg. 5: 29, 1978.4. Gardetto, A., Dabering, J., Rainer, C., Piegger, J., Piza-Katzer, H., and Fritsch, H. Does a superficial musculoaponeurotic system exist in the face and neck? An anatomical study by the tissue plastination technique. Plast. Reconstr. Surg. 111: 664,2003.5. De Castro, C. C. The changing role of platysma in face lifting. Plast. Reconstr. Surg. 105: 764, 2000.6. Mejia JD, Nahai FR, Nahai F, et al. Isolated management of the aging neck. Semin Plast Surg 2009; 23(4):264–73.7. Ellenbogen R, Karlin JV. Visual criteria for success in restoring the youthful neck. Plast Reconstr Surg 1980;66(6):826–37. 8. Loré, J. M. An Atlas of Head and Neck Surgery, Vol. 1 and Vol. 2, 2nd Ed. Philadelphia: Saunders, 1973.9. Labbé D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: anatomical study and analysis of 30 cases. Plast Reconstr Surg 2006;117(6):2001–7 [discussion: 2008–10].10. Jones, B. M., and Grover, R. Reducing complications in cervicofacial rhytidectomy by tumescent infiltration: A comparative trial evaluating 678 consecutive face lifts. Plast. Reconstr. Surg. 113: 398, 2004.11. Daniel Labbé, MDa, Jean-Philippe Giot : Open Neck Contouring, MDb Clin Plastic Surg 41 (2014) 57–63.12. Michael G. Brandt, MD, HBSc Agnieszka Hassa, MD, BSc Kathryn Roth, MD Bret Wehrli, MD Corey C. Moore: The Hypoplatysmal Ligament : Characterization and Biomechanical Properties, MD, MSc, FRCSC ARCH FACIAL PLAST SURG/VOL 14 (NO. 5), SEP/OCT 2012.13. Labbé D, Giot JP, Kaluzinski E. Submental area rejuvenation by digastric corset: anatomical study and clinical application in 20 cases. Aesthetic Plast Surg 2013;37(2):222–31.
NVPC: on October 6 & 7th 2016 in Rotterdam, Netherlands
ISPRES: from October 6 to 8th 2016 in Marseille, France
OGPARC: from October 6 to 8th 2016 in Innsbruck, Austria
BAAPS: on October 7 & 8th 2016 in London, United Kingdom
EUROPHARMAT: from October 11 to 13th 2016 in Bordeaux, France
GÄCD: on October 14 & 15th 2016 in Koln, Germany
ISAPS: from October 24th to 27th 2016 in Kyoto, Japan
AECEP: from November 10 to 12th 2016 in Madrid, Spain
RBSPS: on November 19th 2016 in La Hulpe, Belgium
BAPRAS: from November 23 to 25th 2016 in London, United Kingdom
SOFCPRE: from November 24 to 26th 2016 in Montrouge, France
SETGRA: on November 27th 2016 in Barcelona, Spain
NVPC: on December 12th 2016 in Rotterdam, Netherlands
Join theGROUPE SEBBIN(

8
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
McGregor's flap (groin flap)
The groin flap is a skin autoplasty focused on superficial circumflex iliac vessels. Published by McGregor in 1972 after an anatomical study [1]. It was not the first flap of this type. Bakamdjian described the Delto pectoral [2] flap in 1965, Shaw and Payne described a flap focused on superficial epigastric vessels in 1965 [3]. Boo Koo Chai discovered that the technique was used by John Wood in 1869 [4].McGregor developed his theory, following his discovery of the specificity of axial flaps [5], which led to the first free transfer of a micro-surgical fragment of the skin [6].
Ian Mc Gregor (1921-1998)
He was born in 1921 in Glasgow where he studied medicine and where he became head of department of the West Glasgow plastic surgery unit. He was president of the British Association of Plastic Surgeons (BAPS). He wrote two books “Fundamental techniques of Plastic Surgery” and “Cancer of the face and mouth.”
Ref. 1. Mc Gregor IA, Jackson IT. The groin flap. Brit J Plast Surg 1972; 25: 2-16.2. Bakamdjian VY. A two stage method for pharyngeal reconstruction with a primary pectoral skin flap. Plast Reconstr Surg 1965; 36: 173-84.3. Shaw DT, Payne RL. One stage abdominal flap. Surg Gynec Obst 1946; 83: 205.4. Boo Chai K. John Wood and his contribution to plastic surgery. The first groin flap. Brit J Plast Surg 1977; 30: 9.5. Mc Gregor I, Morgan G, Axial and random pattern flaps. Brit J Plast Surg 1973; 26: 202-13.6. Taylor GI, Daniel RK. The free flap. Composite tissue transfer by vascular anastomosis. Aus NZ J Surg 1973: 24: 255.
Millard's flap
Millard's technique to repair unilateral facial clefts, by using an advancement and rotation flap, was described during a presentation at the International Plastic Surgery Congress in Stockholm in 1955, when Millard was only 35 years old. Millard's technique, sometimes slightly modified, is currently widely used.
Ralph Millard (1919-2011)
He was a leading plastic surgeon of the twentieth century. Very athletic, with strong features reminiscent of the actor Lee Marvin, Ralph Millard showed his powerful personality early on. Having studied at the Harvard Medical School, he continued in Europe with Gillies. He served in the Army in Korea in 1954, and it was while looking after Korean children that he developed his way of correcting the cleft lip [1], after returning to Europe with Gillies with whom he wrote a remarkable book [2], showing the passion surgeons had for reconstructive surgery in the fifties.
Millard moved to Miami in 1956, where he divided his time between private practice, teaching, and publication, especially a large work divided into 2 volumes on the labial maxillofacial clefts [3].
Ref. 1. Millard DR. Camouflage of the unilateral hare look. Trans Int. Soc. Plast Surg 1st Congress Baltimore Williams Wilkins 1957.2. Gillies HD, Millard DR. The principles and art of plastic surgery. London Butterworths 1957.3. Millard R. Clef craft T.1. The evolution of its surgery. The unilateral deformity. T2: Bilateral and rare deformities. Boston Little Brown 1977.
Eponyms(

9
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
The ideal buttock
Regardless of the preferred technique to augment the buttock (an intervention that is increasingly in demand), the goal is not to “pump up” the buttock with fat injections or implants but to obtain “ideal” shapely buttocks. The authors undertook a long and methodical study by creating different photographic models designed by computer and changing the proportions of the gluteal region between the waist and the sulcus gluteus.In the past, the ideal ratio between the waist and the hips, determined by studying the winners of the Miss America contest and playmates of Playboy, was 0.70. The authors submitted their pictures to a group of individuals (50% men and women) whose age (18/24, 25/34, 35/49, 50/64 and 65 years old), ethnicity and nationality were determined. The photographs submitted were the following: a posterior view with waist/hips proportion, a rear view (position of the top of the buttock curve), a lateral view (centre of the buttock) and another lateral view (with width of the waist and hips).The general preference for the rear view was a proportion that ranges from 0.65 to 0.60. The chosen waist-hip ratio was 0.70 when looking at it from the profile view and the gluteal prominence is halfway up. There were no significant differences in terms of gender and ethnicity.This technical study (which is explained in more detail in the electronic version of the magazine), does not intend to determine the required criteria of the ‘beautiful’ buttock. It does not include the lumbosacral curvature or shape of the crease that is under the buttocks (the existence of buttock dimples etc.), the infrastructure (bone, subcutaneous fat, skin) or the thighs (shape, etc.). However, it can help with placement of implants and fat injections to avoid a resulting buttock that is increased in volume but abnormally-shaped and unattractive.
Ref. Wong W.W., Motokef et al. Redefining the ideal buttock. A population analysis. Plast Reconstr Surg 2013; 137: 1739-47.
(SOLUTIONS FOR
FAT TRANSFER ANDLIPOSUCTIONSterile for single use
NEW (
• Premium and Standard kits for the lipofilling of the face; • Handpiece cannulas for liposuction;• Luer lock cannulas for the lipofilling: infiltration, harvesting and injection.
(
A whole range o f new too ls to reshape faces and s i lhouettes in harmony.

10
SYNDACTYLESThe treatment of congenital syndactyly is currently well studied. The interdigital space is filled by a flap. The separation incisions are designed as a zig zag pattern, these areas are sometimes closed but more often are grafted.The congenital joining of two or more fingers was not considered to be a terrible deformity in the past. Ambroise Paré (1510-1590) [1] thought that the fingers could be separated by a sharp razor if there was a webbing but it was better to avoid this if the syndactyly was “tight”. Two centuries later, Pierre Dionis (1643-1718) described the operation to separate fingers using a scalpel. He added that a gauntlet bandage is needed to separate the fingers but did not specify how long it should stay in place [2] (Fig. 1).
The secondary retraction of the interdigital space was inevitable and, until the mid-nineteenth century, surgeons have tried different ways of limiting recurrence of the abutment (threads with weights, lead pipe, tight bandage tied to the wrist) (fig. 1 and 2).The first, Zeller from Vienna, advocated, in 1810, to cut on the dorsal skin a folded triangular flap towards the webbing (fig. 3) [3].
In 1850, the Belgian Didot, proposed to cover the fingers by a large digital flaps (fig. 4) [4]. This seemingly attractive technique is actually impossible. It is, however, found in surgical technique treaties a century later. The Swedish Lennander, was the first to place skin grafts on digital tissue losses in 1891 [5]. The Italian Pieri, advocated Z-shaped incisions to break the retraction lines in 1949.
In the 1990's, tests using expanders were inconclusive. More recently, removal of fat negates the need for skin grafts in some cases.
Ref. 1. Paré A. Des doigts superflus et de ceux qui sont ensemble. Les œuvres d’Ambroise Paré chez Gabriel Buon, 1585, p VI – XXV – VI.2. Dionis P. Cours d’opérations de chirurgie démontrées au jardin du Roy. 8e ed. Paris Vve d’Ouri, 1777 pp. 571-2.3. Zeller S. Neuen operation. Methoden, die angebornen verwachsenen Finger. Wien JB Binz 1810.4. Didot A. Note sur la séparation des doigts palmés et sur un nouveau procédé anaplastique destiné à prévenir la reproduction de la difformité. Bul Ac Roy Belg 1949; 9: 351.5. Lennander KG. Fall of kongenital syndakyli operaedt med help af
Thiersch’s hudtransplantation metod. Upsala lakaref forhandlingar 1891; 26: 151.6. Pieri G. Processo operatorio per la cura sindattila grave. Chir Ital 1949; 3-4: 258.
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Fig. 1: Maintenance of separation of fingers
using a bandage
Fig. 2: Maintaining separation by weight
Fig. 3: Zeller flap
Fig. 4: Didot procedure
COMPOSITE BREAST AUGMENTATION
On December 2 & 3rd 2016
Speakers:
Rika Deraemaecker, MD (Belgium)Dr. Cédric George, MD (Suisse)
Dr. Éric Auclair, MD (Switzerland)Dr. Fabrice Dubrulle, MD (Belgium)
LIV
E SU
RGERY u
MA
STER CLASS u
TODAYYESTERDAY

11
FLASHBACKON THE HISTORY OF BREAST AUGMENTATION(
CHAPTER IV : THE F IRST S IL ICONE IMPLANTS
Editor-in-Chief: Dr J.Glicenstein / Director of Publication: Olivier Pérusseau / Artistic Management: Plate ou GazeuseL’Expander is a publication of GROUPE SEBBIN SAS - 39 parc d’activités des Quatre Vents - 95650 Boissy l’Aillerie.
One of the first meetings of the 3rd International Congress of Plastic Surgery, held in Washington DC (USA) from 13 to 18 October 1963 was dedicated to breast surgery [1]. Of the lectures, three were about breast augmentation. The Argentinian Malbec supported the Ivalon® prostheses, the Canadian Paule Regnault was in favour of the Ivalon® implants. Their results were not convincing. The third lecture was exceptionally well received. Two Houston (Texas) surgeons explained and put forward the characteristics of a prosthesis made of a new material: silicone [2]. This material had already been used in the manufacture of shunts implanted in patients with hydrocephalus. Thomas Cronin (1906-1993) and his resident doctor Frank Gerow (1929-1993), with support from the Dow Corning Company (formed through the merger of two giant groups Dow Chemical and Corning Corporation, to manufacture medical silicone) studied the tolerance to silicone capsules filled with saline, dextran or liquid silicone on 12 dogs. They then sought to establish the form of the prosthesis that could be implanted in women. During one of his shifts, Gerow had the idea of using a similar bag as that used for blood transfusions. Cronin, made the prosthesis out of clay with a shape similar to that of a breast (an "anatomical" prosthesis!)
The initial prosthesis filled with saline was not satisfactory. Cronin chose to fill it with silicone gel;
Once the prosthesis was made and ready, he needed a volunteer for the first implantation. It all came down to luck. Ms. Timmie Lee Lindsay, a 30 year old cleaning lady, divorced, mother of 6 children, came to see Dr. Gerow for the removal of a rose-shaped tattoo placed on the right breast. Shyly, she asked if the surgeon could correct her protruding ears.
Gerow, thought it was an ideal case for breast implantation. He offered to operate on her for free if she agreed to be the first to undergo breast augmentation using silicone implants.The operation took place on March 20, 1962. The results, as well as those of two other women who had been operated on, were presented at the International Congress. Two years later, Timmie Lee Lindsay was examined and photographed again [3].
In 2012, English journalists found Lindsay, aged 80. Although the consistency of her breasts had become hard, the prostheses, covered with calcifications appeared intact, fifty years after being implanted...Cronin and Gerow's lecture had a great impact and very quickly, silicone implants became the only way to increase breast size.
Ref. 1. “Breast” in Transactions of the third International Congress of Plastic Surgery. Excerpta Medica Amsterdam 1961 pp. 41-96.2. Cronin T, Gerow FJ. Augmentation mammaplasty: a new feel prosthesis. Trans Third Intern Congress Plast Surg. Excerpta Medica Amsterdam 1964, p 41-9.3. Bradley SA. The use of silicone in plastic and reconstructive surgery – a retrospective view. Plast Reconstr Surg 1973, 51: 280-8
The plast ic surgery newsletter from GroupeL’EXPANDERIssue 19/ October 2016
Continued on Chapter V: First complications.
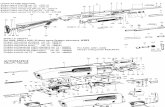
The first silicone prostheses. Dacron “patches” were placed on the posterior surface of the prosthesis.
Ms Lindsay. Preoperative state. Immediate outcome. Outcome after 2 years.

This document is intended for health professionals .
Find the previous issues of the scientific newsletter L'EXPANDER by connecting to the private space at:
www.sebbin.com
According to the Directive concerning medical devices 93/42 / EEC, the cannulas for infiltration, liposuction, harvesting and injection as well as the kits are class IIa medical devices, manufactured by INEX and distributed by Groupe SEBBIN. They are intended to be used in plastic, reconstructive and aesthetic surgery. These devices are CE marked by EZU notified body number 1014. GROUPE SEBBIN reserves the use of its devices to physicians trained in plastic, reconstructive and aesthetic surgery. Please read carefully the instructions on labels and IFU if any before using these devices.