Dupilumab)is)associated)with)disease)worsening)or ... · Background+&+Objec1ves+ • Initial...
Transcript of Dupilumab)is)associated)with)disease)worsening)or ... · Background+&+Objec1ves+ • Initial...

Background & Objec1ves
• Initial improvement: from Th2 suppression, as well as rise in Th1 tumor suppressive effect via secretion of interferon-γ.4,5
• Subsequent worsening: from progression of malignant T-cell (Red Circle) clone due to depletion of the “inflammatory” yet tumor-suppressive tumor infiltrating lymphocytes (Blue Circle).
Methods
Table 1. Pa1ent Characteris1cs and response to dupilumab
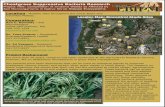
Figure 1: Case 5 Clinical Photographs Possible mechanisms
Conclusions
Dupilumab is a fully human monoclonal an1body that binds the interleukin-‐4 receptor alpha (IL-‐4Rα) subunit and inhibits signaling of IL-‐4 and IL-‐13. It was approved by the Food and Drug Administra1on for the treatment of moderate-‐to-‐severe atopic derma11s (AD) in adults and adolescents with efficacy in reducing pruritus.1 The two most common subtypes of cutaneous T-‐cell lymphoma (CTCL) are mycosis fungoides (MF) and Sézary syndrome (SS). MF/SS and AD are similarly driven by T-‐helper 2 (TH2) cytokine profiles2 and may present with similar morphology (i.e. erythema, lichenifica1on, fissuring) with pruritus,3 disrup1on of the skin barrier, and impe1giniza1on. Thus, it has been hypothesized that dupilumab may be effec1ve in trea1ng CTCL.4 We aimed to assess the effects of dupilumab on the disease course of pa1ents diagnosed with CTCL.
Cutaneous T-‐cell lymphoma progression on dupilumab: 67-‐year-‐old man with a history of mycosis fungoides IIIB A) prior to receiving dupilumab and B) worsened erythroderma aYer 3 months on dupilumab.
We performed chart reviews of 7 pa1ents who were treated with dupilumab and diagnosed with CTCL following ini1al diagnosis of AD, or experienced rapid progression of previously diagnosed CTCL.
Case Sex/ Age (yr)
Diagnosis Prior to dupilumab
Total treatment 1me on dupilumab (mo)
Length of 1me improved (months); Type of improvement
Worsening on dupilumab CTCL diagnosis upon dupilumab discon1nua1on
1 M/64 Presumed AD (retrospec1vely diagnosed as CTCL-‐NOS Stage IB)
8 1; Decrease in BSA (40% to 32%) and pruritus
Increased erythroderma, palmoplantar desquama1on, impe1giniza1on with S. aureus
CTCL-‐NOS Stage IIIA
2 M/72 Presumed AD
4 1.5; Decrease in BSA (80% to 60%) and pruritus
Thickening of plaques with superimposed papules
MF Stage IB
3 F/59 Presumed AD
27 8; Decrease in BSA neck down (40% to 5%), decreased pruritus
Enlargement of facial plaque and onset of fa1gue and weight loss
MF Stage IA
4 F/40 Presumed AD 15 4; Decrease in BSA (unclear %)
Development of erythroderma, blepharoconjunc1vi1s, worsening pruritus
MF Stage IIIA
5 M/67 MF, Stage IIIB 3 2; Decrease in BSA (80%+ to 60%+), decreased pruritus
Increased erythroderma, palmoplantar desquama1on, LAD, worsening pruritus, impe1giniza1on with S. aureus
MF/SS Stage IVA and death.
6 M/58 MF, Stage IIA 3 1.75; Improved asthma and mild decrease in BSA (15%+ to 13%+)
Increased erythroderma, LAD, worsening pruritus
MF/SS Stage IVA and death.
7 F/77 MF, Stage IB 3 0; N/A Increased erythroderma, LAD, worsening pruritus MF/SS Stage IVA
References
Dupilumab is associated with disease worsening or unmasking of cutaneous T-‐cell lymphoma
Maria L Espinosa BS1; Morgan T Nguyen BA1; Amaia Saenz Aguirre MD1; Maria Estela Mar1nez-‐ Escala MD,PhD1; Jane Kim, RN1; Chris1na J Walker MD1; David S Pontes BS1; Jonathan I Silverberg MD, PhD, MPH2; Jaehyuk Choi MD, PhD1,3,4; Barbara Pro MD5; Laura B Pincus MD6; Joan Guitart MD1; Xiaolong Alan Zhou MD, MSc1
1Department of Dermatology, Northwestern University Chicago, IL, USA. 2Department of Dermatology, The George Washington University, Washington D.C., USA. 3Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago, IL, USA. 4 Department of Biochemistry and Molecular GeneMcs Northwestern University, Chicago, IL, USA. 5Division of Hematology/ Oncology Northwestern University, Chicago, IL, USA.6 Department of Dermatology, University of California, San Francisco, San Francisco, CA, USA.
The ini1al improvement may be from the transient blockage of Th2 inflamma1on with shiYing to a Th1 tumor-‐suppressive effect via secre1on of interferon-‐γ, however the nature of subsequent events is unknown.5 One theory behind the worsening could be from the progression of the malignant T-‐cell clone being directly linked to the deple1on of tumor-‐suppressive, tumor infiltra1ng lymphocytes. Alterna1vely, tumor cells may also escape targe1ng by dupilumab and lead to emergence of a dupilumab-‐resistant clone. We postulate that some CTCL cells may be resistant to IL-‐4 and IL-‐13 blockade, and it is possible that our cohort happened to be a selec1ve subset of CTCL pa1ents that were largely resistant to the IL-‐13 and IL-‐4 blockade.
While dupilumab seems to temporarily relieve pruritus and erythema, our experience suggests that long-‐term use leads to worsening or progression of CTCL. Our observa1ons highlight the need for cau1on when using dupilumab in pa1ents with atypical derma11s presenta1ons without prior exclusion of CTCL via skin biopsy, tes1ng for TCR gene rearrangement, and flow cytometry of the blood. Warning signs sugges1ve of CTCL for pa1ents with presumed atopic derma11s while on dupilumab therapy include new eczematous plaques in loca1ons different than original sites, worsening pruritus, lymphadenopathy and new onset moderate-‐severe “atopic derma11s” in the elderly. As dupilumab becomes more commonplace in the treatment of AD and atopic disease, we an1cipate seeing a greater number of cases of unmasked CTCL in pa1ents ini1ally diagnosed with atypical AD.
1. Gooderham MJ, Hong HC-‐h, Esh1aghi P , Papp KA. Dupilumab: A review of its use in the treatment of atopic derma11s. Journal of the American Academy of Dermatology 2018;78:S28-‐S36. 2 Saulite I, Hoetzenecker W, Weidinger S, Cozzio A, Guenova E , Wehkamp U. Sezary Syndrome and Atopic Derma11s: Comparison of Immunological Aspects and Targets. Biomed Res Int 2016;2016:9717530. 3. Serrano L, Mar1nez-‐Escala ME, Zhou XA , Guitart J. Pruritus in Cutaneous T-‐Cell Lymphoma and Its Management. Dermatologic Clinics 2018;36:245-‐58. 4. Gusman-‐Yassky E, Bissonnese R, Ungar B, Suarez-‐Farinas M, Ardeleanu M, Esaki H et al. Dupilumab progressively improves systemic and cutaneous abnormali1es in pa1ents with atopic derma11s. J Allergy Clin Immunol 2019;143:155-‐72. 5. Krejsgaard T, Lindahl LM, Mongan NP, Wasik MA, Litvinov IV, Iversen L et al. Malignant inflamma1on in cutaneous T-‐cell lymphoma-‐a hos1le takeover. Seminars in immunopathology 2017;39:269-‐82.