Drug Study 3rd Wk
-
Upload
hasing-amado -
Category
Documents
-
view
11 -
download
1
description
Transcript of Drug Study 3rd Wk

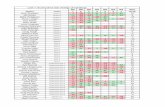
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Acetaminophen Non-Opioid Analgesic/Antipyretic
Mild to moderate pain.
Fever control.
100 mg/mL, 160 mg/5 mL
ROUTE ONSET PEAK DURATIONPO 0.5–1 hr 1–3 hr 3–8 hr†IV w/in 30 min 30 min 4–6 hr
Half-life: Neonates: 2–5 hr. Adults: 1–3 hr.
PO (Adults and Children >12 yr): 325–650 mg q 4–6 hr or 1 g 3–4 times daily or 1300 mg q 8 hr (not to exceed 4 g or 2.5 g/24 hr in patients with hepatic/renal impairment).PO (Children 1–12 yr): 10–15 mg/kg/dose q 4–6 hr as needed (not to exceed 5 doses/24 hr).PO (Infants): 10–15 mg/kg/dose q 4–6 hr as needed (not to exceed 5 doses/24 hr).
Monitor liver and kidney function, and CBC periodically for clients on long-term therapy.
Can cause psychologic dependence. Antidote: Acetylcysteine (Mucomyst)
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Tylenol Analgesia: inhibits formation ofprostaglandins involved with pain. Analgesia also occurs by action of hypothalamus and blocking generation of pain impulses.
Antipyretic: inhibits formation ofprostaglandins in production of fever. It acts on the hypothalamus to produce vasodilation.
Does not have anti-inflammatory or antiplatelet action.
Hypersensitivity Severe hepatic
impairment/active liver disease.
Rash Thrombocytopenia Liver Toxicity (toxicity can occur 2–24 hours after
ingestion)
N/A
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Morphine Sulfate
Opioid Analgesic/ Agonist
Relief of moderate to severe pain.
Preoperative and/or postoperative medication.
Pain relief in MI, relief of dyspnea occurring in pulmonary edema or acute left ventricularfailure.
10 mg/mL, 25 mg/mL
Half-life: Adults: 2–4 hr.
ROUTE ONSET PEAK DURATIONIM 10–30 min 30–60 min 4–5 hrSubcut 20 min 50–90 min 4–5 hrIV rapid 20 min 4–5 hrEpidural 6–30 min 1 hr up to 24 hrIT rapid (min) unknown up to 24 hr
Epidural (Adults): Intermittent injection—5mg/day (initially); if relief is not obtained at 60 min, 1–2 mg increments may be made; (total dose not to exceed 10 mg/day)
Continuous infusion—2–4 mg/24 hr; may ↑by 1–2 mg/day (up to 30 mg/day);
Assess client’s pain before giving medication. Evaluate effectiveness of analgesic including onset and
duration of response to medication. Observe for signs of tolerance with prolonged use. Monitor respiratory rate and depth before giving drug, and
periodically thereafter. Encourage sighing, coughing, and deep breathing. Warn ambulatory clients to avoid activities that require
alertness. Advise client to change position slowly. Check for signs of urinary retention. Keep stool record and institute measures to prevent
constipation - e.g., fluids, foods high in fiber, and activity as tolerated.
Have narcotic antagonist (naloxone[Narcan]) available for reversal of effects if necessary.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
MOS Inhibits the action of histamine at the H2-receptor site located primarily in gastric parietal cells, resultingin inhibition of gastric acid secretion.
Hypersensitivity sedation confusion euphoria impaired coordination dizziness urinary retention constipation hyperglycemia respiratory depression hypotension tachycardia, bradycardia nausea & vomiting allergic reactions pupil constriction
N/A
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Naloxone Hydrochloride
Opioid Anatagonist Postoperative respiratory depression caused by narcotics.
Therapy in suspected orconfirmed narcotic overdose.
0.4 mg/mL, 1 mg/mL
Half-life: 60–90 min (up to 3 hr in neonates).
ROUTE ONSET PEAK DURATIONIV 1–2 min unknown 45 minIM, Subcut 2–5 min unknown >45 min
IV (Adults): 0.02–0.2 mg q 2–3 min until response obtained; repeat q 1–2 hr if needed.
IV (Children): 0.01 mg/kg; may repeat q 2–3 minuntil response obtained. Additional doses may be given q 1–2 hr if needed.
Emergency resuscitative equipment needs to be available. Monitor VS, especially respirations. Monitor surgical clients for bleeding. Withdrawal symptoms will be seen in client addicted to narcotics
(vomiting, restlessness, abdominal cramps, increased BP, and temperature).
Patients who have been receiving opioids for >1 wk are extremely sensitive to the effects of naloxone. Dilute and administer carefully.
Administer undiluted for suspected opioid overdose. For opioid-induced respiratory depression, dilute with sterile water for injection. For children or adults weighing >40 kg, dilute 0.1 mg of naloxone in10 mL of sterile water or 0.9% NaCl for injection.
Administer over 30 seconds for patients with a suspected opioid overdose. For patients who develop opioid-induced respiratory depression, administer dilute solution of 0.4 mg/10 mL at a rate of 0.5 mL (0.02 mg) direct IV every 2 min.
Assess patient for level of pain after administration when used to treat postoperative respiratory depression. Naloxone decreases respiratory depression but also reverses analgesia.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Narcan Occupies opiate receptor sites and prevents or reverses effects of agonists.
Hypersensitivity hypertension tremors reversal of analgesia hyperventilation increases PTT In too-quick reversal: nausea, vomiting,
sweating, tachycardia.
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Phenobarbital Sodium
Barbiturate/Sedative/Hypnotic/
Anti-convulsant
Pre-operative Sedation
Hypnosis
Seizure disorders
Tablets: 15 mg, 30 mg, 60 mg, 100 mgInjection: 65 mg/mL, 130 mg/mL
Half-life: Neonates: 1.8–8.3 days Infants: 0.8–5.5 days Children: 1.5–3 days Adults: 2–6 days
ROUTE ONSET PEAK DURATIONPO 30–60 min unknown >6 hrIM, subcut 10–30 min unknown 4–6 hrIV 5 min 30 min 4–6 hr
Preoperative sedation—1–3 mg/kg PO/IM/IV 1–1.5 Hours before the procedure.
High doses for long periods of time can cause physical dependence.
IV administration: client must be monitored constantly: take V/S frequently, have emergency equipment available, monitor for extravasation at infusion site.
Will cause restlessness in client in pain.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Luminal Hinders movement
of impulses from the thalamus to the brain cortex, thus creating depression in the CNS, which can range frommild to severe.
Inhibits transmission in the nervous system and raises the seizure threshold.
Considered a long-actingbarbiturate.
Hypersensitivity Comatose patients or
those with pre-existing CNS depression.
Severe respiratory disease with dyspnea or obstruction.
Uncontrolled severe pain.
Dizziness, “hang-over” ataxia drowsiness, anxiety, irritability, hand tremors vision difficulties insomnia bradycardia low blood pressure chest tightness wheezing apnea, respiratory depression nausea, vomiting constipation hypersensitivity reactions
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Diazepam Antianxiety Agents/ Anticonvulsant/
Sedative/HypnoticsSkeletal Muscle Relaxant/
Benzodiazepine
Anxiety disorders
Muscle relaxant
Convulsive Disorders
Preoperative medication (sedation)
5 mg/mL
Half-life: Children 12–16 yr: 18–20 hr Adults: 20–50 hr
ROUTE ONSET PEAK DURATIONPO 30–60 min 1–2 hr up to 24 hrIM w/in 20 min 0.5–1.5 hr unknownIV 1–5 min 15–30 min 15–60 min†
Status Epilepticus/Seizure:IV (Adults): 5–10 mg, may repeat q 10–15 min toa total of 30 mg, may repeat again in 2–4 hr
IM, IV (Children ≥5 yr): 0.05–0.3 mg/kg/dosegiven over 3–5 min q 15–30 min to a total dose of
Do not mix with other drugs in the same syringe. Cautious IV use as drug can precipitate in IV solutions. Parenteral administration can cause low blood pressure,
increased heart rate, muscle weakness, and respiratory depression. Monitor I&O.
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

10 mg, repeat q 2–4 hr
Sleletal Muscle Relaxant:IM, IV (Adults): 5–10 mg; may repeat in 2–4 hr
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Valium Depresses the CNS, probably by potentiating GABA, an inhibitory neurotransmitter.
Produces skeletalmuscle relaxation by inhibiting spinal polysynaptic afferent pathways.
Has anticonvulsant properties due to enhanced presynaptic inhibition.
Hypersensitivity Myasthenia gravis Severe pulmonary
impairment Severe hepatic
Angle-closure glaucoma
Dry mouth constipation urinary retention photophobia and blurred vision hypotension tachycardia muscle weakness respiratory depression
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Phenytoin Antiarrhythmic/Anticonvulsant/
Hydantoin
Tonic-clonic and complex partialSeizures
Status epilepticus
Prevention of seizures that accompany neurosurgery
50 mg/mL
Half-life: 22 hr (range 7–42 hr)
ROUTE ONSET PEAK DURATIONPO 2–24 hr 1.5–3 hr 6–12 hrIV 0.5–1 hr rapid 12–24 hr
IV (Adults): Status epilepticus loading dose—15–20 mg/kg. Rate not to exceed 25–50 mg/min.
Tablet can be crushed and should be mixed with food or fluid. Can turn urine pink, red, or red-brown. IM route not recommended. Do not mix with other drugs. Monitor CBC, liver, thyroid, and urine tests. Gingival hyperplasia seen most often in children and
adolescents. Stop drug immediately if a measles like rash occurs. May lead to
renal failure, rhabdomyolysis, or hepatic necrosis.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Dilantin Prevents dissemination of electrical discharges in motor cortex area of the brain.
Antiarrhythmic properties is a result of shortening the actionpotential and decreasing automaticity of the heart.
Hypersensitivity Alcohol intolerance Sinus bradycardia,
sinoatrial block, 2nd- or3rd-degree heart block
Confusion slurred speech slow physical movement blood dyscrasias nausea, vomiting constipation gingival hyperplasia hirsutism rash acne hypotension circulatory collapse cardiac arrest
N/A
Drug StudyGeneric Name Classification Indication Dosage Nursing Responsibilities
Propofol General Anesthetic Induction of general anesthesia in children and adults
Maintenance of balanced anesthesia when used with other agents
Initiation and maintenance of monitored anesthesiacare (MAC)
10 mg/mL
Half-life: 3–12 hr
ROUTE ONSET PEAK DURATION IV 40 sec unknown 3–5 min
IV (Adults ≤55 yr): Induction—40 mg q 10 sec until induction achieved (2–2.5 mg/kg total).Maintenance—100–200 mcg/kg/min. Rates of 150–200 mcg/kg/min are usually required during first 10–15 min after induction
Mac Sed: IV (Adults ≤55 yr): Initiation—100–150 mcg/kg/min infusion or 0.5 mg/kg as slow
Assess respiratory status, pulse, and BP continuouslythroughout propofol therapy (frequently causes apnea lasting 60 sec). Maintain patent airway and adequate ventilation.
Propofol should be used only by individuals experienced in endotracheal intubation, and equipment for this procedure should be readily available.
Assess level of sedation and level of consciousness throughout and following administration.
Do not discontinue abruptly - may cause rapid awakening with anxiety, agitation, and resistance to mechanical ventilation.
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Sedation of intubated, mechanically ventilated patients in intensive care units (ICUs)
injection. Maintenance—25–75 mcg/kg/min infusion or incremental boluses of 10–20 mg.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Short-acting hypnotic.
Produces amnesia.
Has no analgesic properties.
Hypersensitivity to propofol, soybean oil, egg lecithin, or glycerol
dizziness headache APNEA abdominal cramping, nausea, vomiting
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Bupivacaine Epidural Local Anesthetic Local or regional anesthesia or analgesia for surgical,obstetric, or diagnostic procedures.
Solution for injection (preservative-free):0.25%, 0.5%, 0.75%. In combination with: epinephrine 1:200,000
Half-life: 1.5–5 hr (after epidural use)
ROUTE ONSET PEAK DURATIONEpidural 10–30 min unknown 2-8 hr
Epidural (Adults and Children ≥12 yr): 10–20 mL of 0.25% (partial to moderate block), 0.5% (moderate to complete block), or 0.75% (complete block) solution. Administer in increments of 3–5 mL allowing sufficient time to detect toxic signs/symptoms of inadvertent IV or IT administration. A test dose of 2–3 mL of 0.5% with epinephrine solution is recommended prior to epidural blocks
Monitor for sensation during procedure and return of sensation after procedure.
Assess for systemic toxicity (circumoral tingling and numbness, ringing in ears, metallic taste, dizziness, blurred vision, tremors, slow speech, irritability, twitching, seizures, cardiac dysrhythmias) each shift. Report to health care professional.
Monitor BP, heart rate, and respiratory rate continuously while patient is receiving this medication. Mild hypotension is common because of the effect of local anesthetic block of nerve fibers on the sympathetic nervous system, causing vasodilation. Significant hypotension and bradycardia may occur, especially when rising from a prone position or following large dose increases or boluses.
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Marcaine Local anesthetics inhibit initiation and conduction ofsensory nerve impulses by altering the influx of sodiumand efflux of potassium in neurons, slowing or stopping pain transmission.
Epidural administrationallows action to take place at the level of the spinalnerve roots immediately adjacent to the site of administration.
Hypersensitivity circumoral tingling and numbness ringing in ears metallic taste dizziness and blurred vision tremors slow speech irritability twitching seizures cardiac dysrhythmias nausea, vomiting urinary retention CARDIOVASCULAR COLLAPSE,
arrhythmias, bradycardia, hypotension,tachycardia.
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Hydralazine Antihypertensive/Vasodilator
Moderate to severe hypertension
20 mg/mL
Half-life: 2–8 hr
ROUTE ONSET PEAK DURATIONIM 10–30 min 1 hr 3–8 hrIV 5–20 min 15–30 min 2–6 hr
IM, IV (Adults): Hypertension—5–40 mg repeated as needed. Eclampsia—5 mg q 15–20 min; if no response after a total of 20 mg, consider an alternative agent.
Monitor BP and pulse frequently during initial dose adjustment and periodically during therapy.
May be administered concurrently with diuretics or beta blockers to permit lower doses and minimize side effects.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Apresoline Direct-acting peripheral arteriolar vasodilator
Hypersensitivity sodium retention, edema tachycardia drug-induced lupus syndrome dizziness, drowsiness, headache diarrhea, nausea, vomiting
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Dantrolene Skeletal Muscle Relaxant PO: Treatment of spasticity associated with: Spinal cord injury, Stroke, Cerebral palsy, Multiple sclerosis.
Prophylaxis of malignant hyperthermia.
IV: Emergency treatment of malignant hyperthermia.
Capsules: 25 mg, 50 mg, 100 mgPowder for injection: 20 mg/vial
Half-life: 8.7 hr
ROUTE ONSET PEAK DURATIONPO 1 wk unknown 6–12 hrIV rapid rapid unknown
IV (Adults and Children): Treatment of malignant hyperthermia—at least 1 mg/kg (up to 3 mg/kg), continued until symptoms decrease or a cumulative dose of 10 mg/kg has been given. If symptoms reappear, dose may be repeated. Prevention of malignant hyperthermia—2.5 mg/kg before anesthesia.
Assess bowel function periodically. Persistent diarrhea may warrant discontinuation of therapy.
Assess neuromuscular status and muscle spasticity before initiating and periodically during therapy to determine response.
Assess previous anesthesia history of all surgical patients. Also assess for family history of reactions to anesthesia (malignant hyperthermia or perioperative death).
Monitor ECG, vital signs, electrolytes, and urine output continuously when administering IV for malignant hyperthermia.
Reconstitute each 20 mg with 60 mL of sterile water for injection Shake until solution is clear. Solution must be used within 6 hr. Administer without further dilution. Protect diluted solution from direct light.
Administer each single dose by rapid continuous IV push through Y-tubing or 3-way stopcock. Follow immediately with subsequent doses as indicated. Medication is very irritating to tissues; observe infusion site frequently to avoid extravasation.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Dantrium Interferes with calcium release from the muscle, which causes a decrease in muscle contraction.
Prevents intense catabolic process associated with malignant hyperthermia.
No contraindications to IV form in treatment of hyperthermia
drowsiness muscle weakness malaise diarrhea hepatotoxicity (in extended use at high
doses)
N/A
Drug Study
Generic Name Classification Indication Dosage Nursing Responsibilities
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Epinephrine Nonselective (Alpha and Beta) Agonists/
Bronchodilators/Vasopressor/
Adrenergic
Treatment of anaphylaxis andbronchospasm
Cardiac resuscitation
Control or prevention of low blood pressure during spinalanesthesia, lengthening effects of local anesthesia
Promotion of mydriasis,
Treatment of acute hypotension
0.1 mg/mL (1:10,000), 1 mg/mL (1:1000)
Half-life: Unknown
ROUTE ONSET PEAK DURATIONSubcut 5–10 min 20 min <1–4 hrIM 6–12 min unknown <1–4 hrIV rapid 20 min 20–30 min
IV (Adults): Severe anaphylaxis—0.1–0.25 mgq 5–15 min; may be followed by 1–4 mcg/min continuous infusion; cardiopulmonary resuscitation1 mg q 3–5 min; bradycardia - 2–10 mcg/min
IV (Children): Severe anaphylaxis—0.1 mg (lessin younger children); may be followed by 0.1 mcg/kg/min continuous infusion (may give up to 1.5mcg/kg/min); symptomatic bradycardia/pulselessarrest 0.01 mg/kg, may be repeated q 3–5 min higher doses (up to 0.1–0.2 mg/kg) may be considered.
Use great caution in preparing and calculating doses as this is a potent drug.
Protect solutions from light, heat, and freezing. Have a fast-acting alpha-adrenergic blocker such as
phentolamine (Regitine) or vasodilator such as nitrite available for excessive hypertensive reaction.
Have an alpha-adrenergic blocker available for pulmonary edema.
Have a beta-adrenergic blocker available for cardiac arrhythmias.
Monitor BP, pulse, ECG, and respiratory rate frequently during IV administration. Continuous ECG, hemodynamic parameters, and urine output should be monitored continuously during IV administration.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Adrenaline It increases the force of myocardial contraction
Increases systolic blood pressure, cardiac rate and output
Relaxes bronchial smooth muscle
Inhibits histamine release Prevents insulin release and
raises blood sugar Constricts arterioles in kidneys,
mucous membranes, and skin Dilates blood vessels in
skeletal muscle Lowers intraocular pressure
and decreases formation of aqueous humor
Hypersensitivity nervousness restlessness tremor angina arrhythmias hypertension tachycardia
N/A
Drug Study
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Generic Name Classification Indication Dosage Nursing Responsibilities
Norepinephrine Vasopressor Revives blood pressure in acute hypotensive states (sympathectomy, spinalanesthesia, poliomyelitis, septicemia, bloodtransfusion, drug reactions) Adjunct in treatment of cardiac arrest.
1 mg/mL in 4-mL ampules
Half-life: Unknown
ROUTE ONSET PEAK DURATIONIV immediate rapid 1–2 min
IV (Adults): 0.5–1 mcg/min initially, followed by maintenance infusion of 2–12 mcg/min titrated by BP response (average rate 2–4 mcg/min, up to 30mcg/min for refractory shock have been used).
Do not mix drug in 100% saline solutions (NS) as oxidation will occur. Mix in 5% dextrose solution or 5% dextrose in salinesolution.
Give into large vein to prevent extravasation. Check blood pressure every 2 minutes after start of infusion until
desired blood pressure is attained; then check blood pressure every 5 minutes if infusion continued.
Monitor IV site for extravasation. Have phentolamine (Regitine) available in case of extravasation.
5–10 mg of phentolamine (Regitine) in 10–15 mL of saline should be infiltrated into area.
Drug solution should be clear and colorless.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Levophed Is an alpha and beta-1 receptor agonist and has no effect on beta-2 receptors.
Its biggest action is seen on the cardiovascular system, where the following happens: -an increase in total peripheral resistance -increased force, rate, and impulse conduction of the heart, which is usually overridden by activation of baroreceptors, thus causingbradycardia.
Other actions are mydriasis andelevated blood glucose and insulin
Vascular, mesenteric, or peripheral thrombosis
bradycardia cardiac arrhythmias headache
N/A
Drug Study
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Generic Name Classification Indication Dosage Nursing Responsibilities
Phenylephrine Non – Selective Beta agonist Stabilizes blood pressure duringAnesthesia, vascular failure in shock
Subdues paroxysmal supraventricular tachycardia
For IV infusion, check blood pressure, pulse, and central venous pressure every 2–5 minutes.
IV overdose can cause ventricular arrhythmias. Phentolamine (Regitine) should be available for hypertensive crisis seen in IV administration.
Wash hands after handling drug as blurred vision and unequal pupil size can result if drug-contaminated finger rubs eye.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Neo-Synephrine Produces vasoconstriction and increased bloodpressure
Hypersensitivity headache, browache blurred vision increased sensitivity to light palpitations, tachycardia, bradycardia (overdose) hypertension trembling, sweating feeling of fullness in the head sleeplessness dizziness, light-headedness tingling in extremities
N/A
Drug Study
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Generic Name Classification Indication Dosage Nursing Responsibilities
Dopamine Non – Selective Beta agonist Adjunct to standard measures to improve: BP, cardiac output, urine output in treatment of shock unresponsiveto fluid replacement.
Increase renal perfusion(low doses).
200 mg/250 mL, 400 mg/250 mL
Half-life: 2 min
ROUTE ONSET PEAK DURATIONIV 1–2 min up to 10 min <10 min
IV (Adults): Dopaminergic (renal vasodilation) effects—1–5 mcg/kg/min. Beta-adrenergic (cardiac stimulation) effects—5–15 mcg/kg/ min. Alpha- adrenergic (increased peripheral vascular resistance) effects—>15 mcg/kg/min- infusion rate may be increased as needed.
Must be administered cautiously as even small errors can produce deleterious effects.
Do not mix with other drugs. Protect drug from light. Infuse into large vein. Monitor for extravasation and
have phentolamine (Regitine) available if this occurs. Closely check blood pressure, urine output, and
cardiac output. Infusion must be administered via infusion pump to
ensure precise amount delivered. Titrate to response (BP, heart rate, urine output, peripheral perfusion, presence of ectopic activity, cardiac index). Decrease rate gradually when discontinuing to prevent marked decreases in BP.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Intropin Small doses (0.5–3 mcg/kg/min) stimulate dopaminergic receptors, producing renal vasodilation
Larger doses (2–10 mcg/kg/min) stimulate dopaminergic and beta1-adrenergic receptors, producing cardiac stimulation and renal vasodilation.
Doses greater than 10 mcg/kg/min stimulate alpha-adrenergic receptors and may cause renal vasoconstriction.
Hypersensitivity Tachyarrhythmias Pheochromocytoma
tachycardia palpitations hypotension nausea, vomiting dyspnea headache
N/A
Chong Hua HospitalDon Mariano Cui St. corner J. Llorente St., Cebu City, Philippines 6000Office of the Critical Care Services Tel. # 255.8000 loc. 7465Education, Training & Research

Drug StudyGeneric Name Classification Indication Dosage Nursing Responsibilities
Dobutamine Inotropic/Adrenergic
Short-term (<48 hr) management of heart failurecaused by depressed contractility from organic heartdisease or surgical procedures.
250 mg/250 mL, 500 mg/250 mL
Half-life: 2 min.ROUTE ONSET PEAK DURATIONIV 1–2 min 10 min brief (min)
IV (Adults and Children): 2.5–15 mcg/kg/min titrate to response (up to 40 mcg/kg/min)
Monitor BP, heart rate, ECG, cardiac output, CVP, and urinary output continuously during the administration. Report significant changes in vital signs or arrhythmias.
Palpate peripheral pulses and assess appearance of extremities routinely throughout dobutamine administration. Notify physician if quality of pulsedeteriorates or if extremities become cold or mottled.
Trade Name Mechanism of Action Contraindication Adverse Effects Actual Patient Response
Dobutrex Stimulates beta1 adrenergic receptorswith relatively minor effect on heart rate or peripheral blood vessels
Hypersensitivity hypertension, increased heart rate, premature ventricular contractions
N/A