Drug-eluting stent thrombosis: Results from a pooled analysis including 10 randomized studies
-
Upload
raul-moreno -
Category
Documents
-
view
216 -
download
2
Transcript of Drug-eluting stent thrombosis: Results from a pooled analysis including 10 randomized studies

DRRFJCM
DnSowd(
tspistprhrsi
CAL
2
Journal of the American College of Cardiology Vol. 45, No. 6, 2005© 2005 by the American College of Cardiology Foundation ISSN 0735-1097/05/$30.00P
rug-Eluting Stent Thrombosisesults From a Pooled Analysis Including 10 Randomized Studiesaúl Moreno, MD, FESC, Cristina Fernández, MD, Rosana Hernández, MD, FESC,ernando Alfonso, MD, FESC, Dominick J. Angiolillo, MD, Manel Sabaté, MD, FESC,
avier Escaned, MD, FESC, Camino Bañuelos, MD, FESC, Antonio Fernández-Ortiz, MD, FESC,arlos Macaya, MD, FESCadrid, Spain
OBJECTIVES We compared the risk of stent thrombosis (ST) after drug-eluting stents (DES) versusbare-metal stents (BMS), and tested the hypothesis that the risk of DES thrombosis is relatedto stent length.
BACKGROUND Whether DES increase the risk of ST remains unclear. Given the very low restenosis rate afterdrug-eluting stenting, longer stents are frequently implanted for the same lesion length incomparison to BMS.
METHODS We included in a meta-analysis 10 randomized studies comparing DES and BMS. Overall,5,030 patients were included (2,602 were allocated to DES and 2,428 to BMS). The risk ofthrombosis after DES versus BMS was compared, and the relationship between the rate ofDES thrombosis and stent length was evaluated.
RESULTS Incidence of ST was not increased in patients receiving DES (0.58% vs. 0.54% for BMS; oddsratio: 1.05; 95% confidence interval [CI]: 0.51 to 2.15; p � 1.000). The overall rate of ST didnot differ significantly between patients receiving sirolimus- or paclitaxel-eluting stents(0.57% vs. 0.58%; p � 1.000). We found a significant relation between the rate of ST and thestented length (Y � �1.455 � 0.121 X; 95% CI for beta: 0.014 to 0.227; R � 0.716; p �0.031). In patients with DES, mean stented length was longer in those suffering ST (23.4 �8.1 mm vs. 21.3 � 4.1 mm, p � 0.025).
CONCLUSIONS Drug-eluting stents do not increase the risk of ST, at least under appropriate anti-platelettherapy. The risk of ST after DES implantation is related to stent length. (J Am Coll
ublished by Elsevier Inc. doi:10.1016/j.jacc.2004.11.065
Cardiol 2005;45:954–9) © 2005 by the American College of Cardiology Foundation
P
SdbBp(scrbdCSm(TEn(Dp(
ts
rug-eluting stents (DES) have dramatically reduced reste-osis in comparison with bare-metal stents (BMS) (1–11).ome initial reports warned of a possible increase in the riskf stent thrombosis (ST). However, whether ST is increasedith the use of DES as compared with BMS has not beenemonstrated, at least under appropriate antiplatelet therapy1–11).
Given the very low restenosis rate after DES implanta-ion, longer stents have frequently been implanted, as-uming that optimizing immediate angiographic results asossible—even covering nonsignificant coronary lesions—s followed by better clinical outcomes. Some studies havehown that ST after BMS implantation is related tohe stent length, rather than lesion length (12). We hy-othesized that stented length may be related to theisk of ST and also to the use of DES. To test thisypothesis, we performed a meta-analysis of 10 studies thatandomly compared DES and BMS. We also used thesetudies to compare the risk of ST after DES versus BMSmplantation.
From the Division of Interventional Cardiology, Cardiovascular Institute, Hospitallínico San Carlos, Madrid, Spain. This work was presented in part at the 77thnnual Scientific Sessions of the American Heart Association, New Orleans,ouisiana, November 2004.
CManuscript received September 2, 2004; revised manuscript received October 29,
004, accepted November 2, 2004.
ATIENTS AND METHODS
tudies included in the analysis. We included 10 ran-omized studies comparing DES and BMS publishedefore June 2004: Randomized study with sirolimus-coatedx VELocity balloon-expandable stent in the treatment ofatients with de novo native coronary artery lesionsRAVEL) (1); SIRolImUS-Eluting balloon-expandabletent in the treatment of patients with de novo nativeoronary artery lesions (SIRIUS) (2); European multicenterandomized double-blind study of the SIRolImUS-Elutingalloon-expandable stent in the treatment of patients withe novo native coronary artery lesions (E-SIRIUS) (3);anadian multicenter randomized double-blind study of theIRolImUS-Eluting balloon-expandable stent in the treat-ent of patients with de novo native coronary artery lesions
C-SIRIUS) (4); Asian Paclitaxel-Eluting Stent Clinicalrial (ASPECT) (5); European evaluation of pacliTaxel-luting Stent (ELUTES) (6); Treatment of de novo coro-ary disease using a single pAclitaXel elUting StentTAXUS)-I, -II, and -IV (7–9); and RX ACHIEVErug-Eluting coronary stent system In the treatment of
atients with de noVo nativE coronaRy lesions (DELIVER)10).
In the RAVEL, SIRIUS, E-SIRIUS, and C-SIRIUSrials, patients were randomly assigned either to slow-releaseirolimus-DES (140 �g/cm2) or BMS (BX Velocity stent,
ordis Corp., Miami Lakes, Florida). In the ASPECT,
Ep1p(toeawetPst(Tp(IacFw(DSsaCssscsi
a(t(0oiStC
Rtu
dbt�wpvs(r(asLhhen
afbW�pe
R
CTsu6sRnr(01sbpDw
sr0D
955JACC Vol. 45, No. 6, 2005 Moreno et al.March 15, 2005:954–9 Drug-Eluting Stent Thrombosis
LUTES, and DELIVER trials, a non-polymericaclitaxel-DES was used (5,6,10). In the ASPECT trial,76 patients were randomized in a 1:1:1 fashion to eitheraclitaxel 1.3 �g/mm2, paclitaxel 3.1 �g/mm2, or BMSSupra-G stent, Cook Inc., West Lafayette, Indiana). Inhat study, 37 patients received cilostazol instead of thien-pyridines in association with aspirin. This subgroup wasxcluded because this regimen is not the currently acceptedntiplatelet course after coronary stenting. Other patientsho did not receive any anti-platelet therapy were also
xcluded (5). In the ELUTES trial, patients were assignedo paclitaxel 0.2, 0.7, 1.4, and 2.7 �g/mm2, or BMS (V-Flexlus coronary stents, Cook Inc.) (6). In the DELIVERtudy, the ACHIEVE paclitaxel-DES (3.0 �g/mm2) andhe Multilink-Penta BMS (Guidant Corp.) were compared10). A polymeric paclitaxel-DES was evaluated in theAXUS trials (7–9). In TAXUS-I, a slow-releaseaclitaxel-DES (1.0 �g/mm2) was compared with BMSNIR, Boston Scientific Corp., Natick, Massachusetts) (7).n the TAXUS-II study, a first cohort of patients compared
slow-release paclitaxel-DES with BMS, and a secondohort evaluated a moderate-release paclitaxel-DES (8).inally, in TAXUS-IV, the slow-release paclitaxel-DESas compared with BMS (Express, Boston Scientific Corp.)
9). Overall, 5,030 patients were included: 2,602 allocated toES, and 2,428 to BMS.
tenting procedure and antiplatelet therapy. In mosttudies, conventional stent implantation was mandated,lthough direct stenting was allowed in some trials (3,4).onversely, most studies allowed post-dilation. In the
tudies in which the implantation of �1 stent was allowed,tents were overlapped in 28% to 36% of cases (2–4,9). Inome studies, intravascular ultrasound was used to guideoronary stenting (5,7,8). In most of them, however, onlyome patients underwent intracoronary ultrasound either bynclusion in a sub-study or at the operator’s discretion.
Aspirin was given to all patients indefinitely. Addition-lly, clopidogrel was given for one (5), two (1–4), three6,10), or six (7–9) months. The duration of clopidogrelherapy tended to be longer after paclitaxel than sirolimus4.2 � 2.1 months vs. 2.0 � 0.0 months, respectively, p �.056). Glycoprotein IIb/IIIa inhibitors were used at theperator’s discretion in most studies (1–4,6,8,9), althoughn some of them it was either not used or discouraged (5,7).tatistical analysis. The review was conducted according
o the Quality of Reports of Meta-Analyses of Randomized
Abbreviations and AcronymsBMS � bare-metal stentsCI � confidence intervalDES � drug-eluting stentLST � late stent thrombosisOR � odds ratioST � stent thrombosis
linical Trials (QUOROM) recommendations (13). The (
eviewer Manager 4.1 (2000 Cochrane Collaboration) andhe SPSS 10.0 (Chicago, Illinois) statistical packages weresed.Quantitative variables are expressed as mean � standard
eviation, and discrete variables as percentages. Associationsetween categorical variables were studied by the chi-squareest or the Fisher exact test (in case any expected value is
5). Comparisons between two mean values were evaluatedith the Student t or the Mann-Whitney tests, as appro-riate (normally distributed and not normally distributedariables, respectively). The odds ratio (OR) for ST and latetent thrombosis (LST), and their 95% confidence intervalCI) were calculated comparing DES with BMS rates usingaw data for each study and for the pooled populationintention-to-treat basis). The ST was classified as earlynd late (within or after more than one month aftertenting). The fixed-effect model or the Der Simonian andaird random-effect model (when p � 0.05 for Q test foreterogeneity) were used. The combined effect for theeterogeneity was calculated by taking the inverse variancestimated. The effect of each study was weighted for itsumber of patients.To evaluate associations between two continuous vari-
bles, the curve fit regression analysis was used, weightingor the number of patients from each study. The estimatedeta-coefficient as well as its 95% CI was also calculated.
e contacted the principal investigator of all trials in which1 DES ST occurred in order to compare DES ST with
atients not suffering DES ST. Associations were consid-red statistically significant when p � 0.05.
ESULTS
haracteristics of the studies included for analysis.able 1 provides the number of patients included in each
tudy. Prevalence of diabetes ranged from 14% to 31%. These of glycoprotein IIb/IIIa inhibitors ranged from 0% to4%. Data from quantitative coronary analysis for eachtudy are shown in Table 2.isk of ST with DES versus BMS. The rate of ST didot differ between DES and BMS (0.58% vs. 0.54%,espectively; OR: 1.05; 95%CI: 0.51 to 2.15; p � 1.000)Fig. 1A). The rate of LST was also similar (0.23% vs..25%, respectively; OR: 0.99; 95%CI: 0.35 to 2.84; p �.000) (Fig. 1B). After excluding non-polymeric paclitaxeltudies (ASPECT, ELUTES, and DELIVER), the risk ofoth ST (0.65% vs. 0.55%; OR: 1.19; 95%CI: 0.51 to 2.77;� 0.831) and LST (0.27% vs. 0.27%, respectively, forES and BMS; OR: 0.99; 95%CI: 0.29 to 3.43; p � 1.000)as not different.The rate of DES ST ranged from 0% to 2% among
tudies (Table 2), and it did not differ between patientseceiving sirolimus and paclitaxel (0.57% [5 of 878] vs..58% [10 of 1,724], respectively; p � 1.000). Of the 15ES ST cases, 9 (60%) occurred within 30 days, whereas 6
40%) were LST. The rate of LST did not differ signifi-

c8ptlWD(0rpoa0RUoatic2l8m
psw(�pt�s�
D
D
DpaBaihrlbN
TG
RSECAETTTD
D
Ti
RSECAETTTT
M
956 Moreno et al. JACC Vol. 45, No. 6, 2005Drug-Eluting Stent Thrombosis March 15, 2005:954–9
antly between sirolimus- and paclitaxel-DES (0.11% [1 of78] vs. 0.29% [5 of 1,724]; p � 0.670). Of the five lateaclitaxel-DES ST, two occurred in the TAXUS-II, two inhe TAXUS-IV, and one in the DELIVER trial. The onlyate sirolimus-eluting ST occurred in the SIRIUS trial.
hen comparing sirolimus-DES with polymeric paclitaxel-ES, no significant differences were found in the rate of ST
0.57% [5 of 878] vs. 0.73% [7 of 959], respectively; p �.776) and LST (0.11% [1 of 878] vs. 0.42% [4 of 959],espectively; p � 0.377). Non-polymeric and polymericaclitaxel-DES showed no significant differences in the ratef ST (0.39% [3 of 765] vs. 0.73% [7 of 959], p � 0.527)nd LST (0.13% [1 of 765] vs. 0.42% [4 of 959], p �.390).elationship between stent length and risk of DES ST.sing the curve fit regression analysis, the best fit wasbtained with linear regression. We found a significantssociation between the incidence of ST and stented lengthhat remained after weighting by the number of patientsncluded in each study (Y � �1.455 � 0.121 X; 95% CI foroefficient beta: 0.014 to 0.227; R � 0.646; p � 0.031) (Fig.). Among patients allocated to DES, the mean stentedength was significantly larger in those suffering ST (23.4 �.1 mm vs. 21.3 � 4.1 mm, p � 0.025; difference of 3.1m, 95% CI for the difference: 1.05 to 5.15 mm).There was also a significant association between the
able 1. Studies Included in the Pooled Analysis, Including Typelycoprotein IIb/IIIa Inhibitors and IVUS Guidance Among Th
Study Drug StentN
(Total)
AVEL (1) Sirolimus BX Velocity 238IRIUS (2) Sirolimus BX Velocity 1,058-SIRIUS (3) Sirolimus BX Velocity 352-SIRIUS (4) Sirolimus BX Velocity 100SPECT (5) Paclitaxel Supra-G 138LUTES (6) Paclitaxel V-Flex Plus 192AXUS-I (7) Paclitaxel NIR 61AXUS-II (8) Paclitaxel NIR 536AXUS-IV (9) Paclitaxel Express 1,314ELIVER (10) Paclitaxel Multilink Penta 1,041
ES � drug-eluting stent; IVUS � intravascular ultrasound; NA � not available.
able 2. Rate of Thrombosis in Each Study, as Well as Data Fron Each Study
StudyDES
Thrombosis
Mean LesionLength(mm)
Mean StentedLength(mm)
StenteLeng
AVEL (1) 0.0% 9.6 18.0IRIUS (2) 0.4% 14.4 21.5-SIRIUS (3) 1.1% 14.9 23.0-SIRIUS (4) 2.0% 14.5 26.2SPECT (5) 0.0% 11.1 15.0LUTES (6) 0.7% 10.8 16.0AXUS-I (7) 0.0% 10.7 15.0AXUS-II (8) 1.1% 10.40 15.9AXUS-IV (9) 0.6% 13.40 21.7AXUS-IV (10) 0.4% 11.7 19.8
LD � minimum lumen diameter; RVD � reference vessel diameter; other abbreviation
roportion of patients suffering ST and the mean number oftents placed per patient, which remained significant aftereighting by the number of patients included in each study
Y � �1.765 � 2.080 X; 95% for beta: 0.439 to 3.722; R0.752; p � 0.020). The mean number of stents placed in
atients with DES ST was 1.33 � 0.62 (vs. 1.11 � 0.32 inhose without ST; p � 0.190) (difference 0.22; 95%CI:
0.12 to 0.56). A strong correlation was found betweentent length and the number of stents placed (R � 0.875, p
0.001).No significant association was found between the rate ofES ST and other variables studied (Table 3).
ISCUSSION
ES thrombosis. The overall rate of ST after DES im-lantation was �0.6%, and did not differ between sirolimusnd paclitaxel DES. This incidence is comparable to that ofMS (14). Owing to the possibility of delayed endotheli-lization and enhanced platelet aggregation after DESmplantation, initial reports warned about the possibility ofigher risk of ST (15,16). However, recent studies haveeported a low incidence of DES thrombosis under pro-onged therapy with aspirin plus thienopyridines, compara-le to that of BMS, even in unstable clinical settings (17).o differences were found between sirolimus and paclitaxel-
ES, Number of Patients, and Percentage of Use ofllocated to DES
NES) Follow-Up Diabetes
GlycoproteinIIb/IIIa IVUS
20 12 months 16% 10% 40%33 12 months 25% 60% 24%75 9 months 19% 14% 17%50 12 months 24% 58% NA90 6 months 21% 0% 100%53 12 months 17% 31% NA31 12 months 23% 0% 100%66 12 months 14% 16% 100%62 9 months 31% 58% 23%22 9 months 31% 64% NA
e Quantitative Coronary Analysis in Patients Allocated to DES
siontio
No. of StentsPer Patient
Mean RVD(mm)
Mean MLDPost-Procedure
(mm)Mean StenosisPost-Procedure
1.00 2.60 2.43 11.90%1.40 2.80 2.67 5.40%1.50 2.55 2.43 7.70%1.60 2.65 2.53 6.10%1.00 2.94 2.84 3.00%1.07 2.90 2.70 9.60%1.00 2.99 2.95 13.56%1.06 2.75 2.53 10.90%1.08 2.75 2.26 19.10%1.11 2.85 2.86 2.7%
of Dose A
(D
151
1
265
m th
d/Leth Ra
1.881.491.701.81.351.481.401.521.581.69
s as in Table 1.

Dtblr
sttcIeDrmhBsRm
Frr
F
957JACC Vol. 45, No. 6, 2005 Moreno et al.March 15, 2005:954–9 Drug-Eluting Stent Thrombosis
ES. However, the duration of thienopyridines treatmentended to be longer with paclitaxel; thus, a higher throm-ogenicity of paclitaxel that might have been mitigated by aonger duration of dual anti-platelet treatment cannot beuled out.
All study patients were under thienopyridines. The mosttriking factor associated with DES thrombosis is absence ofreatment with ticlopidine/clopidogrel. In the ASPECTrial, the rate of DES thrombosis in patients receivingilostazol instead of thienopyridines was 14.8% (4 of 27) (5).n another study, 30% of patients withdrawing ticlopidinearly after DES implantation suffered ST (18). Of the 15ES thrombosis cases, 6 (40%) were LST. This could be
elated to a delayed stent endothelialization (14), late stentalapposition (8), aneurysm formation, and even a localized
ypersensitivity to the polymer (19). In comparison withMS, late stent malapposition occurs more frequently after
irolimus-DES (9% in the SIRIUS trial and 21% in theAVEL trial). However, in the TAXUS-II trial, late stent
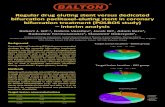
igure 1. (A) Comparison between the rate of stent thrombosis in patieandomized studies and in the pooled population. (B) Comparison betweeandomized studies and in the pooled population. CI � confidence interv
nts allocated to drug-eluting stents (DES) or bare-metal stents (BMS) in then the rate of late stent thrombosis in patients allocated to DES or BMS in theal; OR � odds ratio.
alapposition was not more frequent with paclitaxel-DES(�
igure 2. Relation between stent length and the rate of drug-eluting stent
DES) thrombosis in the different studies included in the meta-analysis. CIconfidence interval.

tppTmRrtliqmil(sask
tTitateprDDadooSad1D
oteowTpoiaiwm
AWtpsb
RDCr
R
958 Moreno et al. JACC Vol. 45, No. 6, 2005Drug-Eluting Stent Thrombosis March 15, 2005:954–9
han with BMS (8). Thus, these data should encourage us torescribe prolonged combined antiplatelet therapy of aspirinlus thienopyridines, perhaps for at least one year. In theAXUS-II trial, 2 of the 3 STs occurred between 6 and 12onths after DES implantation (8).elationship between stent length and risk of ST. The
isk of DES thrombosis ranged from 0% to 2% among therials. This incidence was significantly related to stentength. This also occurs with BMS, and has importantmplications, given the potential serious clinical conse-uences of ST (12). Probably, as stent length increases, it isore difficult to ensure that the stent is fully deployed and
n contact with the vessel wall. In the TAXUS-II trial,esion length was a predictor of late stent malapposition20). In a very recent study, the total stent length wasignificantly associated with the risk of intra-procedural STfter sirolimus-DES implantation (21). Additionally, totaltented length is also an independent predictor for creatineinase-MB fraction after DES implantation (22).When using DES, interventional cardiologists may be
empted to implant stents that are too long. In theAXUS-IV trial, for example, it was recommended to
mplant a stent 2 to 4 mm longer than the lesion. However,he stent length was 8.5 mm longer than the lesion (9). Thisttitude is probably based on two arguments: First, one ofhe limitations of intra-coronary brachytherapy is edge-ffect, and the first reports on DES also warned of theossibility of edge effect with the use of DES. However,andomized trials have not shown an edge-effect caused byES. Second, given the very low rate of restenosis afterES, stent length probably has few implications in the
bsolute rate of subsequent restenosis. In view of the hereinemonstrated relationship between stent length and the riskf DES thrombosis, it could be recommended not to useverly long DES if it is not necessary.tudy limitations. This study has some limitations. First,s with other meta-analyses (23), inclusion criteria may beifferent among studies. Second, follow-up was limited to2 months in most trials. The possibility of very LST after
Table 3. Relationship Between the ProportionClinical and Angiographic Characteristics (LinNumber of Patients Allocated to DES in Each
Variable Regre
% of patients with diabetes Y � 0.6Use of glycoprotein IIb/IIIa Y � 0.4% of IVUS guidance Y � 0.5Lesion length Y � �1Stented length Y � �1Stented/lesion length Y � �1Number of stents per patient Y � �1RVD Y � 6.9MLD post-procedure Y � 3.1% stenosis post-procedure Y � 0.7Duration of clopidogrel therapy Y � 0.7
Abbreviations as in Tables 1 and 2.
ES implantation necessitates a more extended follow-up
f these patients to better understand the problem of DEShrombosis (19). However, some studies with DES havextended the follow-up at two years, with no or very low riskf additional ST (24,25). Finally, intravascular ultrasoundas not performed in cases suffering DES thrombosis.herefore, the underlying mechanisms contributing to thehysiopathology of DES thrombosis were not provided. Atur center, we have performed a prospective study usingntracoronary ultrasound in a series of patients suffering STfter BMS implantation. Stent under-expansion (75%),ncomplete apposition (33%), and edge-dissection (17%)ere frequently found (26). We can hypothesize that theseechanisms are also involved in DES thrombosis.
cknowledgmentse are indebted to the principal investigators of all of the
rials included in this meta-analysis for their contribution toublishing these trials and, in some cases, for providing usome unpublished data from patients suffering stent throm-osis in these studies.
eprint requests and correspondence: Dr. Raúl Moreno,ivision of Interventional Cardiology, Hospital Clinico Sanarlos, Martín Lagos, s/n. 28040 Madrid, Spain. E-mail:
EFERENCES
1. Morice MC, Serruys PW, Sousa JE, et al. A randomized comparisonof a sirolimus-eluting stent with a standard stent for coronary revas-cularization. N Engl J Med 2002;346:1773–80.
2. Moses JW, Leon MB, Popma JJ, et al., SIRIUS Investigators.Sirolimus-eluting stents versus standard stents in patients with stenosisin a native coronary artery. N Engl J Med 2003;349:1315–23.
3. Schofer J, Schluter M, Gershlick AH, Wijns W, Garcia E, Scham-paert E, Breithardt G, E-SIRIUS Investigators. Sirolimus-elutingstents for treatment of patients with long atherosclerotic lesions insmall coronary arteries: double-blind, randomised controlled trial(E-SIRIUS). Lancet 2003;362:1093–9.
4. Schampaert E, Cohen EA, Schluter M, et al., C-SIRIUS Investiga-tors. The Canadian study of the sirolimus-eluting stent in thetreatment of patients with long de novo lesions in small nativecoronary arteries (C-SIRIUS). J Am Coll Cardiol 2004;43:1110–5.
atients Suffering DES Thrombosis andegression Equation After Adjusting for the
dy)
Equation R p Value
0.0004 X 0.098 0.9940.022 X 0.663 0.1010.002 X 0.269 0.751
� 0.208 X 0.632 0.070� 0.121 X 0.716 0.031� 1.348 X 0.380 0.329� 2.080 X 0.752 0.0202.238 X 0.526 0.1520.916 X 0.344 0.3840.009 X 0.123 0.8480.0002 X 0.098 0.999
of Pear RStu
ssion
94 �83 �56 �.681.455.432.76524 �96 �77 �02 �
5. Hong MK, Mintz GS, Lee CW, et al., ASian Paclitaxel-ElutingStent Clinical Trial Investigators. Paclitaxel coating reduces in-stent

1
1
1
1
1
1
1
1
1
1
2
2
2
2
2
2
2
959JACC Vol. 45, No. 6, 2005 Moreno et al.March 15, 2005:954–9 Drug-Eluting Stent Thrombosis
intimal hyperplasia in human coronary arteries: a serial volumetricintravascular ultrasound analysis from the Asian Paclitaxel-ElutingStent Clinical Trial (ASPECT). Circulation 2003;107:517–20.
6. Gershlick A, De Scheerder I, Chevalier B, et al. Inhibition ofrestenosis with a paclitaxel-eluting, polymer-free coronary stent: theEuropean evaLUation of pacliTaxel Eluting Stent (ELUTES) trial.Circulation 2004;109:487–93.
7. Grube E, Silber S, Hauptmann KE, et al. TAXUS I: six- andtwelve-month results from a randomized, double-blind trial on aslow-release paclitaxel-eluting stent for de novo coronary lesions.Circulation 2003;107:38–42.
8. Colombo A, Drzewiecki J, Banning A, et al., TAXUS II Study Group.Randomized study to assess the effectiveness of slow- and moderate-release polymer-based paclitaxel-eluting stents for coronary arterylesions. Circulation 2003;108:788–94.
9. Stone GW, Ellis SG, Cox DA, et al., TAXUS-IV Investigators. Apolymer-based, paclitaxel-eluting stent in patients with coronary arterydisease. N Engl J Med 2004;350:221–31.
0. Lansky A, Costa RA, Mintz GS, et al., for the DELIVER ClinicalTrial Investigators. Non-polymer-based paclitaxel-coated coronarystents for the treatment of patients with de novo coronary lesions.Angiographic follow-up of the DELIVER Clinical Trial. Circulation2004;109:1948–54.
1. Moreno R, Hernandez R, Sabate M, Angiolillo DJ, Macaya C.Situacion actual del tratamiento con stents coronarios recubiertos defármacos antiproliferativos (I). Cardiol Pract (Barc) 2003;12:31–41.
2. Cutlip DE, Baim DS, Ho KKL, et al. Stent thrombosis in the modernera. A pooled analysis of multicenter coronary stent clinical trials.Circulation 2001;103:1967–71.
3. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF.Improving the quality of reports of meta-analysis of randomised con-trolled trials: the QUOROM statement. Lancet 1999;354:1896–900.
4. Orford JL, Lennon R, Melby S, et al. Frequency and correlates ofcoronary stent thrombosis in the modern era: analysis of a single centerregistry. J Am Coll Cardiol 2002;40:1567–72.
5. Virmani R, Farb A, Kolodgie FD. Histopathologic alterations afterendovascular radiation and antiproliferative stents: similarities and
differences. Herz 2002;27:1–6.6. Babinska A, Markell MS, Salifu MO, Akoad M, Ehrlich YH,Kornecki E. Enhancement of human platelet aggregation and secre-tion induced by rapamycin. Nephrol Dial Transplant 1998;13:3153–9.
7. Lemos PA, Lee C, Degertekin M, , et al. Early outcome aftersirolimus-eluting stent implantation in patients with acute coronarysyndromes. Insight from the Rapamycin-Eluting Stent Evaluated AtRotterdam Cardiology Hospital (RESEARCH) Registry. J Am CollCardiol 2003;41:2093–9.
8. Pasceri V, Granatelli A, Pristipino C, Pelliccia F, Pironi B, RichichiG. High-risk of thrombosis of Cypher stent in patients not takingticlopidine or clopidogrel (abstr). Am J Cardiol 2003;92:91L.
9. Virmani R, Guagliumi G, Farb A, et al. Localized hypersensitivity andlate coronary thrombosis secondary to a sirolimus-eluting stent.Should we be cautious? Circulation 2004;109:r38–42.
0. Serruys PW. Insights from the intravascular ultrasound analysis inTAXUS-II. Transcatheter and Cardiovascular Interventions 2003.Available at: http://www.tctmd.com/display/expert/pdf/83343/serruys2-DESS-taxus.pdf. Accessed October 29, 2004.
1. Chieffo A, Bonizzoni E, Orlic D, et al. Intraprocedural stent throm-bosis during implantation of sirolimus-eluting stents. Circulation2004;109:2732–6.
2. Stankovic G, Orlic D, Chieffo A, et al. Predictors of creatinine kinaseMB enzyme elevation after percutaneous coronary intervention usingsirolimus-eluting stents (abstr). Am J Cardiol 2003;92:182L.
3. Moreno R, Fernandez C, Alfonso F, et al. Coronary stenting versusballoon angioplasty in small vessels. A meta-analysis of eleven ran-domized studies. J Am Coll Cardiol 2004;43:1964–72.
4. Sousa JE, Costa MA, Sousa A, et al. Two-year angiographic andintravascular ultrasound follow-up after implantation of sirolimus-eluting stents in human coronary arteries. Circulation 2003;107:381–3.
5. Holmes DR, on behalf of the SIRIUS Trial Investigators. Two-yearfollow-up of the SIRIUS study: a randomised study with thesirolimus-eluting Bx Velocity in the treatment of patients withde-novo native coronary artery lesions. Available at: http://www.tctmd.com/display/expert/pdf/95156/Holmes-DESS.pdf. Ac-cessed October 29, 2004.
6. Alfonso F, Suarez A, Angiolillo DL, et al. Findings of intravascular
ultrasound during acute stent thrombosis. Heart 2004;90:1455–9.