Drug-eluting particles in the treatment of HCC: chemoembolization with doxorubicin-loaded DC Bead™
Transcript of Drug-eluting particles in the treatment of HCC: chemoembolization with doxorubicin-loaded DC Bead™

1643
Review
www.expert-reviews.com ISSN 1473-7140© 2008 Expert Reviews Ltd10.1586/14737140.8.10.1643
Randomized trials and meta-ana lysis studies over recent years have clearly demonstrated an advantage of transcatheter arterial chemo-embolization (TACE) over systemic chemo-therapy or best supportive care for the treat-ment of hepatocellular carcinoma (HCC) [1–6]. In addition, it has been demonstrated that the subgroup of patients that will benefit from this treatment are patients of Barcelona Clinic Liver Cancer (BCLC) stage B [1,5]. Since the introduction of TACE, various schemes have been used including embolization with differ-ent chemotherapeutics, bland embolization and TACE with or without lipiodol or particulate embolic material. The TACE procedure most widely applied is the embolization of a tumor with an emulsion of lipiodol with chemothera-peutics followed by the infusion of particulate embolic material. Herein we refer procedure as conventional TACE (c-TACE), while TACE with drug-eluting beads (DEB) loaded with a chemotherapeutic is referred as DEB–TACE, to distinguish it from other TACE procedures.
Until now, increased local delivery of the chemo therapeutic with decreased systemic tox-icity and induction of ischemia to the tumor was achieved by TACE. However, the technique
cannot be standardized; the local and systemic concentrations of the chemotherapeutic are more or less unpredictable, while the devascularization of the tumor is quite variable depending on the type of embolic material used.
Recent research in targeted treatments has been focused on developing suitable agents that may absorb the chemotherapeutic agent, have mechanical properties to navigate in small tumors’ feeding vessels and once the particles have blocked the intratumor vasculature, elute the active substance (chemotherapeutic) in a controlled and predicted manner. Within this context, the first generation of embolic material with drug-eluting properties has been developed. To date, agents available for clinical use include the Hepasphere™ (Biosphere Medical) and DC Bead™ (Biocompatibles, Surrey, UK). The first is currently in clinical research [7–9], while DC Bead is now in advanced clinical trials. Following the Phase I and II studies with DC Bead that have proven its feasibility, safety, efficacy [10–13], randomized trials are now being completed comparing DEB–TACE with c-TACE.
This is a short review of the properties and results of DEB–TACE with DC Bead in the treatment of HCC.
Katerina MalagariUniversity of Athens, 19 Monis Kyccou, 15669 Papagou, Athens, GreeceTel.: +30 210 6510 340; +30 6977 32 60 33Fax: +30 210 6510 [email protected]
The advantage of chemoembolization of the liver as an antineoplastic treatment for hepatocellular carcinoma is that it achieves high intratumoral concentrations of the chemotherapeutic agent locally that cannot be reached with systemic chemotherapy in nontoxic doses. However, chemotherapeutic release and local concentrations cannot be standardized by this technique. Drug-eluting beads have predictable pharmacokinetics and can achieve higher doses of the chemotherapeutic and prolonged contact time with cancer cells. The DC Bead™ is a drug-eluting bead that has proven favorable kinetics and clinical characteristics. This review describes the features of the DC Bead loaded with doxorubicin for the treatment of hepatocellular carcinoma.
Keywords: chemoembolization • drug-eluting embolization agent • HCC • hepatocellular carcinoma • locoregional percutaneous treatment • particulate embolization material • TACE • transcatheter arterial chemoembolization
Drug-eluting particles in the treatment of HCC: chemoembolization with doxorubicin-loaded DC Bead™Expert Rev. Anticancer Ther. 8(10), 1643–1650 (2008)

Expert Rev. Anticancer Ther. 8(10), (2008)1644
Review Malagari
DC Bead descriptionThe DC Bead is a soft, deformable, spherical particle com-posed of a polyvinyl alcohol hydrogel modified with the hydro-philic ionic monomer 2-acrylamido-2-methylpropanesulfonate sodium salt that is able to bind with anthracycline drugs, such as doxorubicin [14,15]. The microspheres are stored in a phosphate packing solution. During preparation, the beads initially increase in diameter with the admixture of water for injection and sub-sequently, upon loading with doxorubicin, they shrink again. Diameter changes are more pronounced with the larger beads; however, they do not exceed 20% [14,15].
Doxorubicin kinetics/elutionThe loading of doxorubicin to the beads is conducted through an ion-exchange mechanism and once completed, doxorubicin is contained within the beads. Doxorubicin loss on bead suspen-sion and mixture of contrast agent is approximately 0.2%, thus minimizing the systemic release of doxorubicin and hence the side effects observed in c-TACE [14,15]. Controlled drug elution only occurs in an ionic environment, such as within the tumor, and in a gradual fashion [14–16]. This kinetic profile suggests that the DC Bead enables the standardization of the procedure.
Laboratory and animal studies with the DC Bead have demon-strated a sustained continuous release of doxorubicin from the beads for a period of more than 14 days after injection [14,15]. Moreover, studies using a porcine model of embolization sug-gested doxorubicin was present for at least 3 months [17], which was subsequently confirmed by spectroscopic ana lysis [16,17]. The rate of elution of doxorubicin at the tumor is described mathemat-ically by the Higuschi equation and depends on the osmolality of the tumor and the size of the injected beads (the larger the beads, the slower the local release) [14,15]. The polymerized microsphere of the DC Bead is approximately 90% water and is compressible to approximately 30% in diameter. In sterile water the beads initially swell, while upon loading with doxorubicin 25 mg/dl, the DC Bead undergoes a decrease of 20%. For example, beads with a diameter of 700–900 µm swell to 820–923 µm on exchange of the phosphate packing solution for pure water, with a subsequent shrinkage in average size to 536 µm on uptake of the drug, a fact that enables delivery through small-lumen microcatheters [15,16]. Doxorubicin elution does not occur when the elution medium is pure water, but only when the elution medium contains ions, as shown by the Higushi equation [m
o – m = kt1/2] where m
0 is the
concentration of drug loading into the beads, m is the concentra-tion of drug left within the beads after time, t, and k is a constant, relevant to the initial drug concentration in the beads, diffu-sion coefficient and drug solubility. After 20–100 min (for beads of 100–300 µm to 700–900 µm, respectively) of loading with doxorubicin 25 g/dl, less than 2% will remain in the solution, while the rest has been transferred inside the beads [14–16]. The maximum concentration of doxorubicin in the liver is achieved on day 3 post-embolization while high tumor concentrations are observed for up to 7 days, suggesting continuous elution of doxorubicin from the beads entrapped in the tumor neovascular-ity [16]. By contrast, as demonstrated in the Lewis et al. study,
intra-arterial delivery in controls resulted in no significant levels of intratumoral doxorubicin [16]. Elution of doxorubicin from the DC Bead in the studies of Lewis et al. showed comparable results in vitro and in vivo, confirming that intratumoral concentration depends on drug concentration, osmolality of the tumor and also somewhat on bead size [15,16]. Their pharmacokinetic study
in pigs demonstrated that liver peak concentration (Cmax
) was approximately 15-times higher in the animals treated with small beads versus large beads [16], despite the fact that the relative dose administered was only approximately 1.5-times greater in the small-bead group.
Favorable doxorubicin kinetics in DEB–TACE with DC Bead were also demonstrated in clinical Phase I/II trials [10,13]; Poon et al., in Phase I of their study, found that C
max concentrations
of doxorubicin are reached at 5 min post-endovascular adminis-tration of the loaded beads followed by a rapid decrease within the next 12 h. Low C
max values even at the highest loading doses
of doxorubicin in the beads (150 mg) were observed to reach 52.8 ± 41.5 ng/ml following administration with an average half-life of plasma doxorubicin of 73.5 ± 22.7 h. The levels of plasma doxorubicin in the Poon study were similar in patients treated with low doxorubicin doses to those of patients treated with larger doses, indicating that doxorubicin can be eluted in a controlled manner even in higher loading doses. In addition, the highest plasma concentrations measured by Poon et al. (52.8 ± 41.5 ng/ml) in the DC Bead group were 17-fold lower compared with levels measured after administration of doxorubicin 50 mg in conven-tional chemoembolization (900 ± 300 mg/ml) [13]. Varela et al. measured the concentration of doxorubicin in plasma post-em-bolization and compared this with c-TACE. Blood samples were obtained in 13 patients at 5, 20, 40, 60 and 120 min and 6, 24, 48 and 168 h to determine doxorubicin C
max and area under the
curve. Doxorubicin Cmax
and area under the curve were signifi-cantly lower in DEB–TACE patients (78.97 ± 38.3 ng/ml and 662.6 ± 417.6 ng/ml.min) than in c-TACE (2341.5 ± 3951.9 ng/ml and 1812.2 ± 1093.7 ng/ml.min; p = 0.00002 and p = 0.001, respectively). The peak drug concentration in their study (C
max)
was reached within 5 min after injection in all cases treated with loaded DC Bead at a level of 78.97 ± 38.3 ng/ml, which was found to be statistically significantly higher compared with c-TACE (895.66 ± 653.1 ng/ml) [10].
Doxorubicin loading & doseAlthough doxorubicin bead loading at 45 mg is feasible, the man-ufacturers report a mazimum recommended level of 37.5 mg for reproducible loading and release [18]. In addition, the recommended safety dose range shown by the Precision Study is 25–37.5 mg of doxorubicin per milliliter of hydrated beads (100–150 mg per patient) [10]. This loading range achieves doses of 50–75 mg/m2 of body surface area, which are the clinically recommended treatment doses, with a maximum recommended maximum life-time dose of 450 mg/m2 for systemic delivery [101]. Furthermore, dose adjustments for bilirubin levels may also be used, as in the Varela study (<25.6 mol/l, 75 mg/m2; 25.6–51.3 mol/l, 50 mg/m2; 51.3–85.5 mol/l, 25 mg/m2) [10].

www.expert-reviews.com 1645
ReviewChemoembolization with doxorubicin loaded DC Bead™
Poon et al. administered 25, 50, 75, 100 and 150 mg of doxo-rubicin loaded in DC Beads in a dose escalation and observed no toxicity related to doxorubicin. In their study, dose-limiting toxicity was defined as grade 4 in one patient, or grade 3 toxic-ity in two patients in any category of the South West Oncology Group toxicity criteria [13]. Malagari et al. used a dose of 150 mg per patient in both of their studies without the development of doxorubicin-related toxicities [11,12].
Selection of DC Bead diameterRegardless of the technique, the TACE particle diameter is selected on the basis of the vascularity of the lesion(s) to be treated and the presence of an arteriovenous shunt. Fatal complications have been reported in the use of small particles if an arteriovenous shunt is overlooked [19]. In DC Bead studies, Poon et al. used DC Beads of 500–700 µm in diameter and noted that the choice was based on the fact that larger DC Beads elute doxorubicin in the tumor slower than smaller beads, as suggested by in vitro studies [14,15]. Malagari et al. used selective/segmental emboliza-tion to first administer loaded beads of diameters of 100–300 µm and then 300–500 µm [11,12].
The effects of bead diameter have also been studied in vitro and in animal experimental work; Lewis et al., in their study in Yucatan pigs, showed that doxorubicin-loaded beads of diam-eters of 100–300 µm caused widespread pannecrosis of the target and adjacent hepatic tissue with no amount of vasculopa-thy, neutrophilic inflammation, moderate portal fibrosis, and arteriovenous and biliary hyperplasia [16]. The necrosis pattern in this group radiated outwards from centres on clusters of DC Bead with extensive liquefactive and coagulative necrosis sug-gesting both ischemic and toxic causes of cell death. In loaded beads of larger diameters (700–900 µm), necrosis was shown to be less extensive compared with the smaller doxorubicin-loaded beads, not radiating outwards [18]. It is inferred that smaller bead diameters achieve a more distal embolization also obstructing collateral channels, while loaded beads of larger diameters of cause a more proximal embolization that pen-etrates less into the tumor and enables vascular supply through collateral channels that are not blocked by the beads. Recent research on the development of particles that are traceable with CT scan or MRI has demonstrated such differences in distri-bution between large and small diameters of the particles [20]. In this respect, smaller loaded beads may be more efficient in achieving both toxic and ischemic necrosis and are suit-able if the catheter is selective to the tumor but not suitable if embolization is not selective enough and restricted to the tumor-feeding arteries.
Inclusion & exclusion criteriaInclusion criteria are similar to those of c-TACE; patients with documented HCC, BCLC class B and a good Karnofky score, with relatively preserved liver function (Child–Pugh score A or B). Exclusion criteria are BCLC class beyond B, bilirubin above 3 mg/dl, aspartate aminotransferase and/or alanine aminotrans-ferase more than five-time normal values, involvement of more
than 50% of the liver by the tumor, portosystemic shunt or hepatofugal blood flow, any contraindication for doxorubicin administration (white blood cell count < 3000 cells/mm3 and neutrophils < 1500/mm3) or cardiac ejection fraction below 50%. The presence of a portal vein thrombosis at the initial diag nosis of the HCC is not an absolute contraindication for TACE treatment but patients have to be elected carefully with regard to their liver function [21]. In addition, accumulated experience in our center has demonstrated that even in multifocal and bilobar disease, staged procedures treating one lobe at a time, can be performed safely with beads 300–500 µm or larger, provided there is no thrombosis of the portal vein.
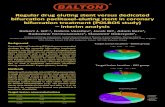
Efficacy Response rates Response rates as surrogates of survival are reported in all clinical tri-als with the DC Bead, since long-term results are still being evaluated and pending. A broad spectrum of HCC diameters are included in the studies completed to date, with a sufficient description of patient characteristics. Figures 1 & 2 demonstrate local response rates.
In the Phase I/II clinical trial by Varela et al. including 27 HCC patients treated with doxorubicin-loaded DEBs at doses adjusted for bilirubin and body surface (range: 47–150 mg), an overall response rate of 75% (66.6% on intention to treat) was reported [10]. The mean diameter of the lesions treated was 4.6 cm, the majority were classified as stage Okuda I (Okuda I/II: 26/1), the relative proportions of the etiology of cirrhosis were 16/7/4 for virus hepatitis C virus (HCV)/alcohol/others and Child–Pugh stage proportions were 27/0 for A/B while embolizations were performed at set time intervals (every 2 months).
Similarly, Malagari et al. included tumors of 3–10 cm in diam-eter (mean: 6.2 cm) in 71 patients, reporting overall complete necrosis in 15.5%, while objective response rates ranged from 66.2 to 85.5% across the four treatments [12]. In this study, the majority of patients were Child–Pugh B (Child–Pugh A/B/C: 27/44/0) while the etiology of cirrhosis was Hepatitis B virus(HBV)/HCV/HBV and HBV in 29/19/23. Tumor necrosis in this study ranged between 28.6 and 100% across sequential treatments at set time intervals. In a previously submitted paper by the same group, embolizations and follow-up were at set time intervals (every 3 months), and 9-month follow-up demonstrated that partial response was maintained in 68.4%, stable disease in 12.2% and complete response in 12.2%, while progressive disease was noted in 7.01% [11].
Poon et al. included patients with larger tumors (sum diam-eters of 10.0 ± 5.8 cm) and observed a 50% objective response rate at 1 month after the first treatment (complete response: 0%; partial response: 50%) by Response Evaluation Criteria in Solid Tumors (RECIST) criteria and and 70% (complete response: 6.7%; partial response: 63.3%) by the modified RECIST criteria–European Association for the Study of the Liver (EASL) [13]. At 4 months after the completion of two treatments the response rates were 35.7% by RECIST criteria (complete response 0%; partial response 35.7%) and 42.9% by EASL (complete response 14.3%; partial response 28.6%). In

Expert Rev. Anticancer Ther. 8(10), (2008)1646
Review
Baseline After first embolization
After second embolization
Pre-embolization 2 months post-embolization
Malagari
their study, Poon et al. enrolled only patients with Child–Pugh A cirrhosis and the remaining inclusion criteria were identical to those of other DC Bead studies. Frequency of embolization procedures was similar to the aforementioned studies (i.e., at set time intervals, every 2 months); however, recorded data included a total of two procedures per patient.
These results are high compared with response rates in pro-spective conventional chemoembolization studies that report 16–35% [1,2,22,23].
SurvivalSurvival data on DEB–TACE are restricted to less than 4 years and longer term follow-up results will be published soon. Varela et al. reported a 1- and 2-year survival of 92.5 and 88.9%, respec-tively, after a median follow-up of 27.6 months [10]. Similarly, in the study of Malagari et al. survival was 97.05, 91.1 and 88.2% at 12, 24 and 30 months, respectively [12]. The recently reported disease-specific 3-year survival was 67.4% [24]. In a previously submitted paper, 1-year survival was not available (follow-up was 9 months at the time of ana lysis of results) [11].
Likewise, high survival rates are observed only in c-TACE treatment of small tumors that are now treated either with radiofrequency ablation (RFA) or combined RFA and TACE. In the c-TACE arm of their study (n = 80) with small HCCs of median diameter of 4 cm (range: 0.5–20 cm) Yuen et al.
observed high cumulative survival rates of 93.8, 86.3, 78.8, 57.5 and 51.3%, respectively at 6 months, 1, 2, 3 and 4 years [25]. In a paper from Matsui et al. (which was misquoted previously [11,12]) in which TACE was applied prospectively to potential RFA candidates, survival was 100, 92, 78 and 67% at 1, 2, 3 and 4 years, respectively [26]. They also achieved histologically proven complete response in four of the seven patients (57.14%) and 50–80% necrosis in four of 11 patients who underwent resection (36.36%) [26]. In a study including tumors smaller than 5 cm in diameter, survival rates at 1, 2 and 3 years were 93.3, 77.1 and 77.1%, respectively [27]. In a prospective cohort of 8510 Japanese patients with small tumors treated with c-TACE, Takayasu et al. observed overall survival rates of 82, 47, 26 and 16% at 1, 3, 5 and 7 years, respectively, and median survival of 34 months [28]. In their study, 51% were Child–Pugh score A, while 39 and 10% were B and C, respectively. HCC diameters treated were 2.1–3 cm (24%), 3.1–5 cm (28% and more than 5 cm (25%).
In c-TACE of HCC with diameters similar to those in the studies of Varela, Malagari and Poon, the results of survival are less favorable taking into account differences in patient population and specific protocol variability. Comparison with studies on Western population survival data with loaded beads shows a clear advantage; survival rates of c-TACE in the study of Bronowicki et al. reach 64, 38, 27 and 27% at 1, 2, 3 and 4 years, respectively [29]. Overall survival in the randomized trial conducted by Lo et al. at 1, 2 and 3 years was 57, 31 and 26%, respectively, in the c-TACE arm of their study [2], while in the randomized trial of Llovet et al. survival rates of the c-TACE arm at 1 and 2 years were 82 and 63%, respectively [1]. The French multicenter trial with advanced HCC patients showed survival rates with c-TACE of 64 and 38% at 1 and 2 years [4]. Brown et al. demonstrated survival rates of 61, 42 and 32% at 1, 2 and 3 years, respectively [30]. Eastern population studies have similarly less favorable data; the 1-, 2- and 3-year cumu-lative survival rates of HCC patients treated with two combi-nations of conventional chemoembolization with Child–Pugh
grades A and B were 59.1–79.2, 26.7–51.8 and 14.9–34.9%, respectively [31]. In a Korean study with 905 HCC patients treated with c-TACE, the reported 3-year survival ranged from 5.0 to 67.4% for dif-ferent UICC stages (I to IVa), while for Child–Pugh class A patients with stage I and II the 3-year survival was 69.6% [32]. Ha et al., in a cohort of 345 patients (Okuda I: 68%; II:31%; III: 1%), reported overall survival rates of 69, 46, 39 and 30% at 1, 2, 3 and 4 years, respec-tively [33]. In the chemoembolization arm of Change et al.’s study involving HCC patients who were mostly Child–Pugh A cirrhosis not amenable to surgery, 1–2-year survival rates of 52.5 and 26.2% were recorded [34]. In their protocol,
Figure 1. Hepatocellular carcinoma near the diaphragmatic dome. Complete necrosis after two superselective embolizations with doxorubicin-loaded DC Bead™.
Figure 2. Post-embolization image demonstrates complete necrosis. Note the absence of liver damage next to the treated lesion.

www.expert-reviews.com 1647
ReviewChemoembolization with doxorubicin loaded DC Bead™
embolization was performed every 2–3 months until either the lesion disappeared, the patient could not sustain further embo-lization or the patient died; with an average of two to three procedures per patient [34].
Serum a-fetoprotein levels Good response and a drop or normalization of a-fetoprotein (AFP) values was noticed in all studies using doxorubicin-loaded beads; serum AFP levels dropped significantly in the studies with doxorubicin-loaded DC Bead. In the study by Poon et al., AFP levels were measured at 1, 3 and 6 months after the first treatment [13]. Among the patients who had elevated AFP (above 20 ng/ml) a reduction of more than 30% was mea-sured in 69.2, 65.4 and 42.3% of patients at 1, 3 and 6 months, respectively. In a study by Malagari et al. AFP levels showed a mean decrease of 1123 ng/ml (95% confidence inteval [CI]: 846–1399; p = 3 × 10–11) after the first session and remained stable after the second and third embolizations (42 and 70 ng/ml decrease, respectively) [11]. Similar changes were observed by Varela et al. [10].
Combined treatmentsIn June 2007 SHARP, a large, randomized, double-blind, placebo-controlled, multicenter, Phase III trial (n = 602) using sorafenib in patients with advanced HCC (82% BCLC stage C) reported a 44% improvement in median survival from 7.9 to 10.7 months [35]. In this study, oral sorafenib administered in doses of 400 mg twice daily resulted at a median time to radiologic progression of 5.5 months in the sorafenib group and 2.8 months in the placebo group (p < 0.001) [35]. Sorafenib is a small-molecule multikinase inhibitor of the VEGF receptor pathway and PDGF RAF/MEK/ERK cascade [34]. The use of this treatment in HCC patients of BCLB stage C is adopted currently in medical practice. It is yet to be determined whether this agent can be administered to improve survival and prolong time to progression in BCLC stage B patients if used combined with DEB–TACE. A number of tri-als are currently underway to investigate this hypothesis. This hypothesis is further supported by the results of a randomized, double-blind, Phase II study (n = 96) in which median dura-tions of overall and progression-free survival were significantly longer with sorafenib plus doxorubicin than with doxorubicin alone [36].
The use of RFA combined with TACE has shown promis-ing results; Cheng et al. showed that patients treated with TACE–RFA had better overall survival than those treated with TACE (hazard ratio [HR]: 1.87; 95% CI: 1.33–2.63; p < 0.001) or RFA alone (HR: 1.88; 95% CI: 1.34–2.65; p < 0.001) [37]. Similarly advantageous results have been demonstrated in other studies [38,39].
SafetyLiver functionA sight increase of liver enzymes for the first 3–4 days post-embolization was observed in all human studies with DC Beads with return to pre-embolization levels within a few days [10–13].
An increase of liver enzymes post-embolization is also a fre-quent finding in c-TACE [40]. Similar observations with DC Bead embolization were made in animal studies in which a tran-sient increase of liver enzymes was present until day 14 post-embolization and returned to near or below pretreatment levels by days 28–90 [14]. By contrast, in the group with nonloaded beads a slight increase was observed but returned to normal by day 7. Increase of liver enzymes was more pronounced with the smaller bead diameters compared with the larger ones [14]. Similar patterns of liver enzyme levels were also recorded for alanine transferase and alkaline phosphatase, although not as high. The higher elevation of liver enzymes with smaller loaded beads was attributed to the more distal nature of the embolization and the elimination of collaterals.
Complications In the clinical studies published using DC Beads, complica-tions ranged between 4.2 and 11.4%, including pleural effu-sion, gastric ulcer bleeding, esophageal variceal bleeding, liver failure, cholocystitis and abscess formation [10–13]. Severe procedure-related complications not including postemboliza-tion syndrome (PES) were observed in 4.2% of patients in Malagari et al. (cholocystitis, liver abscess, pleural effusion). Liver abscess and cholocystitis were considered serious adverse events (2.8%) and clearly related to the procedure. Two of the 27 patients included in Varela et al. developed liver abscess, one of whom died (treatment-related death: 3.7%). The rates of this complication in c-TACE are similar, ranging from 0.26 to 3.12% [40–42]. The patients who developed abscess did not receive any predisposing factors, the most important of which is bilioenteric anastomosis [41].
In Malagari et al., PES of various severities was observed in all patients [12]. Clinically relevant PES developed in 37% of embo-lized patients of in patients Varela et al.; PES is also a complication of c-TACE [43]. All the aforementioned complications are also known to occur in c-TACE as well, with none of them repre-sents systemic toxicity [40,43]. Accurate comparison of c-TACE and DEB–TACE is yet to be performed in randomized control trials of the two methods.
It is worth noting that no doxorubicin-related systemic compli-cations were noted in the published clinical series using doxoru-bicin-loaded DC Bead for the treatment of HCC [10–13]. Systemic toxicities caused by doxorubicin include:
Neurological effects (seizures)•
Cardiovascular (sinus, artrioventricular and bundle–branch •block arrythmias in the acute phase; delayed cardiomyopathy with reduction of the ejection fraction)
Pulmonary (pulmonary edema)•
Gastrointestinal (nausea and vomiting)•
Bone marrow suppression (dose-dependent leukopenia and •thrombocytopenia in approximately 60%)
General (alopecia and stomatitis) • [19]

Expert Rev. Anticancer Ther. 8(10), (2008)1648
Review Malagari
The probability of developing impaired myocardial function is cumulative and dose dependent ranging from 1–2% at a life dose of 300 mg/m2of doxorubicin, to 21% at 728 mg/m2 . The absence of systemic doxorubicin toxicity is attributed to the low peripheral concentrations of doxorubicin in the DC Bead series, a fact that represents one of the major advances of this treatment.
Fields yet to be coveredRandomized trials to compare DEB–TACE with other TACE techniques are currently underway. However, a number of other issues must also be studied:
Histology data in humans from patients who undergo post-•downstaging resection or transplantation
The precise role of DEB–TACE as a neoadjuvant procedure in •patients undergoing resection or transplantation
Accurate and objective volumetric techniques to measure •response to treatment
A consensus on the preferred imaging method to follow-up •response to treatment
Quality of life•
Parameters such as disease progression rates, time to progression •and probability of developing local or extrahepatic recurrence
Treatment schedule and repetitions•
Demonstration of consistency or results in all geographical areas•
ConclusionsClinical studies of DEB–TACE demonstrate that treatment of BCLC stage B patients with HCC results in good response rates, increased survival up to 3 years and presents low complication rates without systemic toxicity. Randomized studies currently underway will demonstrate the additional value of this technique over other established methods of TACE.
In addition, the DC Bead provides a method of accurate doxoru-bicin loading and tumor release, and can be used as a model device for the controlled and precise local delivery of chemotherapy
intra-arterially (standardized technique).
Expert commentaryDC Beads are DEBs that, loaded with doxorubicin, have favor-able kinetics achieving high tumor concentrations with low plasma levels.
Clinical trials have shown good response (objective response: 66–85%), high survival (76.4% at 3 years) and low complica-tion rates none of which were related to doxorubicin toxicity. In addition, the DC Bead is a device that enables standardization of TACE, achieving local ischemia and toxic death of tumor cells with one device, and low complication rates without systemic toxicity.
Five-year viewThis decade has proved to be a cascade of new issues in TACE. However, open issues remain to be explored:
The development of a gold standard imaging technique to •objectively and volumetrically assess local treatment results is yet to be achieved;
After the results of randomized studies of DEB–TACE in com-•parison with c-TACE are released, the development of studies that will further identify patients group that will best respond to this treatment;
The comparison of DEB–TACE with bland embolization;•
The full development of DEBs that can be detected with CT •scans or MRI since these materials are still undergoing labora-tory development;
The determination of the exact role of antiangiogenic drugs •since HCC is known to have high VEGF expression. The use of antiangiogenic agents such as bevacizumab (AvastinTM, Gen-tech, Inc., CA, USA) has already proven advantageous, prolong-ing survival in advanced HCC (BCLC stage C). Trials inves-tigating the potential advantage in combination with c-TACE and DEB–TACE are currently underway;
The release of results with other drug-eluting particles, such as •Hepasphere, is expected soon;
Results from other targeted agents, such as 3-bromopyruvate, •are also expected.
Financial & competing interests disclosureThe author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Key issues
Randomized trials and meta-ana lysis studies performed within this decade have proved the role of transcatheter arterial • chemoembolization (TACE) in improving survival for patients with hepatocellular carcinoma (HCC).
The development of drug-eluting devices that can be delivered to the tumor with selected embolization is a challenge of targeted • locoregional anticancer treatment of HCC.
Of the drug-eluting devices, DC Bead™ is one that is now in advanced clinical trial stages. Phase I and II trials have demonstrated • effectiveness and safety, and a larger randomized multicenter trial comparing DC Bead loaded with doxorubicin versus conventional TACE will be released at Cardiovascular and Interventional Radiological Society of Europe 2008. The latter will address response and complication results.

www.expert-reviews.com 1649
ReviewChemoembolization with doxorubicin loaded DC Bead™
ReferencesPapers of special note have been highlighted as:•ofinterest••ofconsiderableinterest
Llovet JM, Real MI, Montana X1 et al. Barcelona Liver Cancer Group. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomized controlled trial. Lancet 359, 1734–1731 (2002).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Lo CM, Ngan H, Tso WK2 et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35, 1164–1161 (2002).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Llovet JM, Bruix J. Systematic review of 3
randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 37, 429–424 (2003).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Pelletier G, Ducreux M, Gay F4 et al. Treatment of unresectable hepatocellular carcinoma with lipiodol chemoembolization: a multicenter randomized trial. J. Hepatol. 29, 129–121 (1998).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Gamma C Schepis F, Orlando A 5 et al. Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology 224, 47–45 (2002).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Bruix J, Sherman M, Llovet JM6 et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona–2000 EASL Conference. European Association for the Study of the Liver. J. Hepatol. 35, 421–424 (2001).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Osuga K, Khankan AA,Hori S 7 et al. Transarterial embolization for large hepatocellular carcinoma with use of superabsorbent polymer microspheres: initial experience. J. Vasc. Interv. Radiol. 13, 929–929 (2002).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Hori S, Okada A, Sakamoto K8 et al. A new embolic material: superabsorbent polymer microsphere and its embolic effects. Jpn. J. Intervent. Radiol. 11, 375–373 (1996).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Kankan AA, Osuga K, Hori S, Morii E, 9
Murakami T, Nakamura H. Embolic effects of superabsorvent polymer midrospseres in rabbit renal model: comparison with tris-acryl gelatine microspheres and polyvinyl alcohol. Radiat. Medicine 22, 384–383 (2004).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Varela M, Real MI, Burrel M 10 et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J. Hepatol. 46(3), 474–481 (2007).
Important clinical study using the DC •Bead™ in clinical practice.
Malagari K, Chatzimichael K, 11
Alexopoulou E et al. Transarterial chemoembolisation of unresectable hepatocellular carcinoma (HCC) with drug eluting beads (DEB); results of an open label study of 62 patients Presented at ECR 9–13 (2007). Cardiovasc. Intervent. Radiol. 31(2), 269–280 (2008).
Important clinical study using the DC •Bead in clinical practice.
Malagari K, Alexopoulou E, 12
Chatzimichail K et al. Transcatheter chemoembolization in the treatment of HCC in patients not eligible for curative treatments: midterm results of doxorubicin-loaded DC Bead. Abdom. Imaging 33(5), 512–519 (2008).
Important clinical study using the DC •Bead in clinical practice.
Poon RN, Tso WK, Pang RWC13 et al. A Phase I/II trial of chemoembolization for hepatocellular carcinoma using a novel intra-arterial drug-eluting bead. Clin. Gastroenterol. Hepatol. 5, 1100–1101 (2007).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Hong K, Khwaja A, Liapi E14 et al. New intra-arterial drug delivery system for the treatment of liver cancer: preclinical assessment in a rabbit model of liver cancer. Clin. Cancer Res. 12, 2563–2567 (2006).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Lewis AL, Gonzalez MV, Lloyd AW15 et al. DC Bead: in vitro characterization of a drug-delivery device for transarterial chemoembolization. J. Vasc. Interv. Radiol. 17, 335–334 (2006).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Lewis AL, Taylor RR, Hall B16 et al. Pharmacokinetic and safety study of doxorubicin-eluting beads in a porcine model of hepatic arterial embolization. J. Vasc. Interv. Radiol. 17(8), 1335–1343 (2006).
Experimental work in the evaluation of •the DC Bead.
Namur J, Wassef M, Millot J-M 17 et al. Doxorubicin eluting beads for liver embolization: pathological findings and correlation with drug distribution in tissue. Presented at: 35th Annual Meeting and Exposition of the Controlled Release Society. NY, USA, 12–16 July 2008 (Abstract 109).
Gonzalez MV, Tang Y, Philips GJ 18 et al. Methods for evaluating drug elution and in vitro-in vivo correlation. J Mater. Sci. Mater. Med. 19, 767–775 (2008).
Experimental work in the evaluation of •the DC Bead.
Brown KT. Fatal pulmonary complications 19
after arterial embolization with 40–120- micro m tris-acryl gelatine microspheres J. Vasc. Interv. Radiol. 15(2 Pt 1), 197–200 (2004).
Barnett BP, Liapi E, Kim GK 20 et al. PEGDA based spheres – chemospheres. Presented at: SIR Annual Meeting. DC, USA, 15–20 March 2008.
Herber S, Pitton M, Mönch C 21 et al. Transarterial chemoembolization (TACE) of the hepatocellular carcinoma (HCC) in patients with portal vein thrombosis – experiences. Zentralbl. Chir. 132(4), 306–315 (2007).

Expert Rev. Anticancer Ther. 8(10), (2008)1650
Review Malagari
Raoul JL, Heresbach D, Bretagne JF. 22
Chemoembolization of hepatocellular carcinomas. A study of the biodistribution and pharmacokinetics of doxorubicin. Cancer 70(3), 585–590 (1992).
Groupe D’Etude et de Traitment du 23
Carcinome Hepatocellulaire. A comparison of lipiodol chemoembolization and conservative treatment for unresectable hepatocellular carcinoma. N. Engl. J. Med. 332, 1256–1261 (1995).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Malagari K, Pomoni M, Pomoni A 24 et al. Long term results of doxorubicin-loaded DC Bead in the treatment of HCC survival, recurrence free interval and quality of life. Presented at: EASL Monothematic Liver Conference. Liver Cancer: From Molecular Pathogenesis to New Therapies. Prague, Czech Republic, 12–14 June 2008.
Yuen MF, Chan AOO, Chun-Yu B 25 et al. Transarterial chemoembolization for inoperable, early stage hepatocellular carcinoma in patients with Child–Pugh grade A and B: results of a comparative study in 96 Chinese patients. Am. J. Gastroenterol. 98(5), 1181–1185 (2003).
Matsui O, Kadoya M, Yoshikawa J26 et al. Small hepatocellular carcinoma: treatment with subsegmental transcatheter arterial embolization. Radiology 188, 79–78 (1993).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Saccheri S, Lovaria A, Sangiovanni A27 et al. Segmental transcatheter arterial chemoembolization treatment in patients with cirrhosis and inoperable hepatocellular carcinomas. J. Vasc. Interv. Radiol. 13, 995–999 (2002).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Takayasu K, Arii S, Ikai I28 et al. Prospective cohort study of transarterial chemoembolization for unresectable hepatocellular carcinoma in 8510 patients. Gastroenterology 131, 461–464 (2006).
Documents the value of chemoembolization ••compared with systemic chemotherapy or best supportive care.
Bronowicki JP, Vetter D, Dumas F29 et al. Transcatheter oily chemoembolization for hepatocellular carcinoma: a 4-year study of 127 French patients. Cancer 74, 16–24 (1994).
Brown DB, Pilgram KT, Darcy MD 30 et al. Hepatic arterial chemoembolization for hepatocellular carcinoma: comparison of survival rates with different embolic agents. J. Vasc. Interv. Radiol. 16, 1661–1661 (2005).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Chen MS, Li J-Q, Zhang Y-Q31 et al. High-dose iodized oil transcatheter arterial chemoembolization for patients with large hepatocellular carcinoma. World J. Gastroenterol. 8(1), 74–78 (2002).
Park KW, Park JW, Cho SH 32 et al. Survival analysis for patients with hepatocellular carcinoma according to stage, liver function and treatment modalities]. Korean J. Hepatol. 12(1), 41–54 (2006).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Ha BY, Ahmed AD, Sze DY 33 et al. Long-term survival of patients with unresectable hepatocellular carcinoma treated with transcatheter arterial chemoinfusion. Aliment. Pharmacol. Ther. 26, 839–846 (2007).
Chang JM, Tzeng WS, Pan HB34 et al. Transcatheter arterial embolization with or without cisplatin treatment of hepatocellular carcinoma. A randomized controlled study. Cancer 74, 2449–2442 (1994).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Llovet JM, Ricci S, Mazzaferro V 35 et al. SHARP Investigators Study Group.Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 359(4), 378–390 (2008).
Simpson D, Keating GM. Sorafenib: in 36
hepatocellular carcinoma. Drugs 68(2), 251–258 (2008).
Cheng BQ, Jia CQ, Liu CT37 et al. Chemoembolization combined with radiofrequency ablation for patients with
hepatocellular carcinoma larger than 3 cm: a randomized controlled trial. JAMA 299(14), 1669–1677 (2008).
Veltri A, Moretto P, Doriguzzi A38 et al. Radiofrequency thermal ablation (RFA) after transarterial chemoembolization (TACE) as a combined therapy for unresectable non-early hepatocellular carcinoma (HCC). Eur Radiol. 16(3), 661–669 (2006).
Lencioni R, Crocetti L, Petruzzi P39 et al. Doxorubicin-eluting bead-enhanced radiofrequency ablation of hepatocellular carcinoma: a pilot clinical study. J. Hepatol. 49(2), 217–222 (2008).
Ramsey DE, Kernagis LY, Soulen MC40 et al. Chemoembolization of hepatocellular carcinoma. J. Vasc. Interv. Radiol. 13(Suppl.), S211–S221 (2002).
Kim W, Clark TW, Baum RA, Soulen MC. 41
Risk factors for liver abscess formation after hepatic chemoembolization. J. Vasc. Interv. Radiol. 12, 965–969 (2001).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Chung JW, Park JH, Han JK42 et al. Hepatic tumors: predisposing factors for complications of transcatheter oily chemoembolization. Radiology 198, 33–40 (1996).
Wigmore SJ, Redhead DN, Thomson BN43 et al. Postchemoembolization syndrome: tumour necrosis or hepatocyte injury? Br. J. Cancer 89, 1423–1422 (2003).
Documents the value of ••chemoembolization compared with systemic chemotherapy or best supportive care.
Patent
Doxorubicin HCl Labeling. Adriamycin™ 101
RDF (Pharmacia and Upjojn), Rubex® (Bristol Myers Squibb) NDA 50–467.
AffiliationKaterina Malagari, MD •Associate Professor of Radiology, University of Athens, 19 Monis Kyccou, 15669 Papagou, Athens, Greece Tel.: +30 210 6510 340; +30 6977 326 033 Fax: +30 210 6510 340 [email protected]