Dr Isstelle Joubert 2 nd yr M Sports and Exercise Medicine September 2012.
-
Upload
samir-hench -
Category
Documents
-
view
221 -
download
3
Transcript of Dr Isstelle Joubert 2 nd yr M Sports and Exercise Medicine September 2012.

Dr Isstelle Joubert2nd yr M Sports and Exercise Medicine
September 2012

PATIENT COMPLAINT
• Mr. CG, 27yo
• rugby player playing lock forward – 1st team,
senior club level
• pain at medial aspect of left knee – 6/52 Hx
• pain progressed last 3/52 - VAS 6-7/10

PATIENT COMPLAINT:
• gradual in onset
• daily when standing or sitting for extended periods
• irritated when driving long distances: knee flexed
• aggravated: bending to engage in scrums
• relieved with occasional NSAIDs - returned within
day
PAINPAIN

PATIENT COMPLAINT:
• slight instability in L knee
• “fullness”, especially in fully flexed position
• mid-season - over-reaching during period before
onset of pain
• playing surfaces – not changed
• footwear – not changed

PREVIOUS HISTORY:
partial tear in ACL of L knee – 2 seasons before
• Rx: conservative, limited ROM brace
• no meniscal injuries
No other medical history

CLINICAL EVALUATION:
Observation:Observation:
• standing + supine:
visible diffuse swelling
postero-lateral aspect of popliteal fossa of L
leg
• walking: not much change in size / position
• swelling visible bilateral to patellar tendon ant

CLINICAL EVALUATION:
Active movementsActive movements
• straight leg raise: normal
• knee extension, flexion, tibial rotation: normal
ROM
• some discomfort:
on full extension
medially with tibial rotation
“fullness”: knee full flexed position

CLINICAL EVALUATION:
Passive movementsPassive movements
• extension, flexion, tibial rotation: minimal
discomfort
• hamstring stretch testing: marked discomfort
• quad stretch testing: normal
• Ober’s test: normal
Resisted movementsResisted movements
• tibial rotation, knee flexion: marked discomfort

CLINICAL EVALUATION:
Functional testingFunctional testing
• squatting and forward lunge: cause discomfort
• jumping, hopping, stepping up and down step:
normal

CLINICAL EVALUATION:
PalpationPalpation
• gluteus medius: no trigger points
• patellar tapping: mild ballotability - small
effusion
• patella glide test (all directions): no pain
• palpation of patellar fat pad: normal
• no synovial plica palpable
• patella tracked perfectly within femoral trochlea
• both VMO muscles palpated evenly in mass

CLINICAL EVALUATION:
PalpationPalpation
• posterior popliteal fossa: diffuse swelling noted
• direct pressure:
elicited pain, mainly centrally in fossa
radiated towards medial aspect of knee to
point of pes anserinus bursa
• not pulsating
• auscultation: no vascular bruits

CLINICAL EVALUATION:
Special maneuversSpecial maneuvers
• Stability testing for MCL and LCL: normal
• Lachman’s test
• Anterior Drawer test normal bilateral = ACL normal
• Pivot Shift tests
• Posterior Drawer test + with External Rotation
reproduced pain - stability normal acc to R side
• no posterior sagging

CLINICAL EVALUATION:
• Reverse Lachman: negative - normal PCL
• Patellar Apprehension testing: negative
• Medial and Lateral Translations: not reproduce pain
• McMurray’s test discomfort medial
• Appley’s Posterior Grind test aspect of knee
• Tell Sally test: marked discomfort on medial
rotation
?? medial meniscus pathology

CLINICAL EVALUATION:
Referred Pain testingReferred Pain testing
• Slump test no
• Neural Thomas Stretch test pain
• Straight Leg Raise with added Dorsiflexion
Lumbar SpineLumbar Spine
• Palpation + assessment: no pathology

CLINICAL EVALUATION:
Biomechanical AssessmentBiomechanical Assessment
• failed to show any signs of biomechanical
problems predisposing to pain in L knee

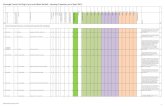
DIFFERENTIAL DIAGNOSISDIFFERENTIAL DIAGNOSIS

• Baker’s Cyst
• Pes Anserinus Bursitis
• Torn Popliteus Muscle / Popliteus Tendinopathy
• Hamstring Insertional Tendinopathy
• Medial Meniscus Tear
• Posterior Cruciate Sprain
• Gastrocnemius Tendinopathy
• Synovial Plica


Soft tissue Ultra-sound
• large cystic mass - typical of Baker’s cyst
• centrally in popliteal fossa
• extending medially towards medial collateral
lig area
X-rays
• no abnormalities detected

MRI
• oval shaped, multi-lobulated cyst
• medial in fossa
• small neck: between medial gastroc head
and semi-membranosis tendons
• pressure on Pes Anserinus bursa
• size:
axially 36x15mm
cross sectionally 35mm

• no free fluid accumulation in knee joint
• no bone marrow edema or contusion
• medial and lateral menisci: normal, no tears
• medial and lateral collateral ligaments: normal
• anterior and posterior cruciate ligaments:
normal
• quadriceps tendon, patellar tendon, other:
normal

3 STAGE SUMMARY

3 STAGE SUMMARY
Biological / Clinical
• Baker’s cyst due to unknown cause
Personal / Psychological
• away from work due to post-operative pain
• might be a career-ending injury
Social / Contextual
• letting his team down mid-season


ActiveActive
• Baker’s cyst with Pes Anserinus Bursa pressure
• surgical repair indicated
PassivePassive
• None at this stage

PLAN & PROGRESSION

PLAN
• patient discussed with orthopedic surgeon
• plan: formal excision of cyst
• surgery done in July 2012
• cyst found to be much larger than on MRI report

PROGRESSION
• discharged 1-day post-op with Robert Jones bandage
• referred to physiotherapist
• walking crutches for 5 days
• during this period physiotherapist:
isometric contraction exercises
proprioceptive work
• instructions:
not to fully extend knee – until ROS (day 8 post-op)
scar fully healed
replaces the multi-layered system used
with thetraditional 'Robert Jones Dressing'

PROGRESSION
Week 2 post-op:
• physiotherapist: with Range of Motion (ROM) exercises
• aim: to re-establish full knee extension
active assisted knee slides against wall
progressed to knee flexor stretching
using sport cord and knee flexor stretch against a wall
• after full ROM:
active cycling to maintain aerobic fitness
Isotonic Open-Chain-Kinetic Exercise - straight leg raises

PROGRESSION
Week 3 post-op:
• Closed-Kinetic-Chain Strengthening Exercises
• initial mini squats performed in 0-40 degree range
• progressing to standing wall slides
• followed by straight line lunges
• lunges done at different angles

PROGRESSION
Week 4 post-op:
• start light leg presses in gym
• incorporation of plyometric exercises
Week 5 post-op:
• discharged to biokineticist
• aim:
maintain strength, proprioception and flexibility
testing to return to play

Baker’s CystBaker’s CystDiscussion

DEFINITION
• synovial fluid filled mass
• in popliteal fossa
• enlarged bursa located beneath medial head of gastroc +
semimembranosus muscles
• type of chronic knee joint effusion:
herniates between two heads of gastroc
Brukner & Khan, 2012

DEFINITION
• 1st Baker’s cyst: diagnosed in 1840 (dr Adams)
• Dr William Morrant Baker
1877,(37 y later – published paper)
8 pt’s: peri-articular cysts caused by synovial fluid
from knee joint new sac outside joint space
associated with underlying conditions
osteo-arthritis (OA) & Charcoat’s joints
Baker, 1994

INCIDENCE

INCIDENCE
• 2 peaks of age-incidence: 4-7y and 35-70y (Handy, 2001)
• general population:10-41% (Janzen et al, 1994)
• depends on diagnostic imaging:
5-40% (MRI) in pt with OA or ?internal derangement
23-32% with arthrography in similar population
(Fielding et al, ‘91; Sansone et al, ‘95; Miller et al, ‘96; Hayashi et al, ‘10)
• common associated meniscal lesions (83%)
43% were associated with articular cartilage damage
32% associated with ACL tears (Sansone et al 1995)


factors in development + maintenance of pop cyst
communication between joint and cyst (valve-like effect)
influenced by gastrocnemius-semimembranosus muscle
changes during flexion-extension of kneeLindgren & Rauschning, 1980
intra-articular pressure changes direct flow of synovial fluid
from supra-patellar bursa knee popliteal cystLindgren & Rauschning, 1980
pressure -6mmHg
knee flexion
pressure
16mmHg
knee
extension

repeated micro-trauma of gastroc-semimem bursa:
enlargement
joint capsule herniation into popliteal fossa (Handy, 2001)
trauma causative in 1/3 of cases (Miller et al, 1996)
co-existent joint disease in 2/3 of cases (Miller et al, 1996)
osteo-arthritis
rheumatoid arthritis
meniscal tears
infectious arthritis


most cases:
small, asymptomatic, not found o/e
dx imaging studies for other indications
Sx from associated joint disorders / Kx
Sx & Tx of Cyst itself:
posterior knee pain
knee stiffness
swelling / mass palpable post – in extension
discomfort - prolonged standing / hyperflexion
symptoms worsened by physical activity

due to Kx of the Cyst:
enlargement into lower leg - DVT
nerve entrapment: tibial and peroneal nerve (Jong-Hun Ji and Shafi et al, 2007)
compartment syndrome, ant or post involvement (Klovning and Beadle, 2007)
occlusion of popliteal artery:ischemia of lower limb
(Wachter et al, 2005)
compression of popliteal vein:venous obstruction, pseudo-thrombophlebitis,
thrombophlebitis (Drescher & Smally, 1997)

due to Underlying joint disorders:
instability of knee joint
due to internal derangement:
meniscal tears
+/- ACL deficiencies
joint pain
inflammatory arthritis
osteo-arthritis
cartilage damage


Physical Examination:
palpable fullness
at medial aspect of popliteal fossa
at or near origin of medial head of gastroc muscle
if injured medial meniscus: McMurray test positive

Plain radiography
is not modality of choice
other intra-articular pathologies, i.e.
calcification / loose bodies in joint space(Brukner & Khan, 2012)

Ultrasonography
great value (size1-2 cm)
easy, quick, inexpensive, non-invasive
not Dx of other intra-articular pathology (B & K, 2012)
1st U/S-dx: 1972 (McDonald & Leopold, 1972)
Baker Cyst

Ultrasonography
sonographic diagnosis of Baker’s cyst
presence of cystic soft tissue mass post of knee
visualising of communicating anechoic or hypo-
echoic fluid between semimembranosus and
medial gastrocnemius muscles
(Ward and Jacobson, 2001)
distinguish Baker’s cyst from
ganglion cysts
popliteal aneurysm
other popliteal masses

Magnetic Resonance Imaging (MRI)
diagnosis Baker’s cyst
and intra-articular pathologies (Brukner & Khan, 2012)
indicated
if ?internal derangement
evaluate anatomical relationship to joint and
surrounding tissues
surgery is considered
uncertain ultrasound-diagnosis (Marra et al, 2008)
gold standard: MRI
Baker Cyst

Baker Cyst

Baker Cyst
intra-articular body in cyst

Baker Cyst
ruptured cyst

MANAGEMENT

diagnosed incidentally: no treatment
advice:
small risk of rupture
seek medical advice if symptomatic
diagnosed incidentally: no treatment
advice:
small risk of rupture
seek medical advice if symptomatic
MANAGEMENT
prevention not possible
advice on activities:
regular exercise and weight Mx for OA
no squatting, kneeling, heavy lifting, climbing
prevention not possible
advice on activities:
regular exercise and weight Mx for OA
no squatting, kneeling, heavy lifting, climbing

initial Rx:
arthrocentesis of knee
aspiration
intra-articular glucocorticoid injection of cyst
expect ↓ in size and discomfort of cyst (two-thirds of pt) within 2 to 7 days
• ↓ risk of recurrence
• improvement of symptoms
• controlling inflammation by glucocorticoid injections (Acebes et al, 2006)
initial Rx:
arthrocentesis of knee
aspiration
intra-articular glucocorticoid injection of cyst
expect ↓ in size and discomfort of cyst (two-thirds of pt) within 2 to 7 days
• ↓ risk of recurrence
• improvement of symptoms
• controlling inflammation by glucocorticoid injections (Acebes et al, 2006)
MANAGEMENT

review diagnosis
?persistent underlying knee pathology
repeat of glucocorticoid injection
arthroscopic knee surgery
non-communicating cysts:
non-responsive to intra-articular injections
direct aspiration and glucocorticoid injection
no joint pathology: surgical excision
review diagnosis
?persistent underlying knee pathology
repeat of glucocorticoid injection
arthroscopic knee surgery
non-communicating cysts:
non-responsive to intra-articular injections
direct aspiration and glucocorticoid injection
no joint pathology: surgical excision
MANAGEMENT
Ultrasound-guided
direct cyst corticoid injection indicated
intra-articular injection of gluco-corticoids
failed to relief symptoms
non-communicating Baker’s cysts

indicated (if injections):
++ painful
↓ joint mobility
lengthy procedure
open procedure to excise cyst (Fritschy et al, 2006)
arthroscopic procedures
repair of intra-articular pathology
removal of cyst
debridement of capsular openings (Ahn et al, 2010)
indicated (if injections):
++ painful
↓ joint mobility
lengthy procedure
open procedure to excise cyst (Fritschy et al, 2006)
arthroscopic procedures
repair of intra-articular pathology
removal of cyst
debridement of capsular openings (Ahn et al, 2010)
MANAGEMENT

Post-op Risks:
wound sepsis
synovial fistulae
recurrence: 2y post-op f/u on MRI-study (Calvisi et al, 2007)
disappeared: 64%
reduced: 27%
persisted: 9%
Post-op Risks:
wound sepsis
synovial fistulae
recurrence: 2y post-op f/u on MRI-study (Calvisi et al, 2007)
disappeared: 64%
reduced: 27%
persisted: 9%
MANAGEMENT

POST-OP REHABILITATION

aim: ↑ knee function
knee immobilizer
for comfort, with weight bearing
day 1 post-op:
isometric exercises + straight leg raises
knee range of motion exercises
wound stable
post-op inflammation subsided (Gonzalez & Lavernia, 2010)
wound healing complete before maximal extension
aim: ↑ knee function
knee immobilizer
for comfort, with weight bearing
day 1 post-op:
isometric exercises + straight leg raises
knee range of motion exercises
wound stable
post-op inflammation subsided (Gonzalez & Lavernia, 2010)
wound healing complete before maximal extension
POST-OP REHAB
Supportive Management:
P.R.I.C.E. regime
physical therapy: ↓ pain, preserve ROM
muscle strengthening: quads, patellar lig


PROGNOSIS
most asymptomatic – NO complications
some resolve spontaneously
most respond to Mx of associated disorders of knee
most asymptomatic – NO complications
some resolve spontaneously
most respond to Mx of associated disorders of knee


differential diagnosis !!differential diagnosis !!NOT only Baker’s cyst / DVT
• pleomorphic sarcoma
• malignant giant cell tumors
• myxoid liposarcomas (Arumilli et al, 2008)
early accurate / delayed dx
affect overall prognosis
unnecessary use of anti-
coagulation therapy (if mistaken
for DVT) could be dangerous!


1. Acebes JC, Sanchez-Pernaute O, Diaz-Oca A, et al.
Ultrasonographic assessment of Baker’s cysts after inatr-
articular corticosteroid injection in knee osteoarthritis. J
Clin Ultrasound. 2006;34:113
2. Ahn JH, Lee SH, Yoo JC, et al. Arthroscopic treatment of
popliteal cysts: clinical and magnetic resonance imaging
results. Arthroscopy. 2010;26:1340
3. Arumilli BRB, Babu VL, Paul AS. Painful swollen leg -
think beyond deep vein thrombosis or Baker’s cyst.
World Journal of Surgical Oncology. 2008;(6):6
4. Baker WM. On the formation of the synovial cysts in the
leg in connection with disease of the knee joint. 1877.
Clin Orthop Relat Res. Feb 1994;(299):2-10

5. Calvisi V, Lupparelli S, Giuliani P. Arthroscopic all-inside
suture of symptomatic Baker’s cysts: a technical option for
surgerical treatment in adults. Knee Surgery, Sports
Traumatology, Arthroscopy. 2007;15(12):1452-1460
6. Brukner P, Khan K. Clinical Sports Medicine.4th Ed. 2012. p
731-732
7. Drescher MJ, Smally AJ. Thrombophlebitis and
pseudothrombo-phlebitis in the emergency department. Am J
Emerg Med. 1997;15:683-685
8. Fielding JR, Franklin PD, Kustan J. Popliteal cysts: a
reassessment using magnetic resonance imaging. Skeletal
Radiol. 1991;20:433


15.Miller TT, Staron RB, Koenigsberg T, et al. MR imaging of Baker
cysts: association with internal derangement, effusion, and
degenerative arthropathy. Radiology. 1996;201:247
16.Hayashi D, Roemer FW, Dhina Z, et al. Longitudinal assessment
of cyst-like lesions of the knee and their relation to radiographic
osteoarthritis and MRI-detected effusion and synovitis in patients
with knee pain. Arthritis Res Ther. 2010;12:R172
17.Klovning J, Beadle T. Compartment Syndrome secondary to
spontaneous rupture of a Baker’s cyst. J La State Med Soc.
2007;159(1):43-44
18.Lindgren PG, Rauschning W. Radiographic investigation of
popliteal cysts. Acta Radiol Diagn (Stockh). 1980;21:657
19.Marra MD, Crema MD, Chung M, et al. MRI features of cystic
lesions around the knee. Knee. 2008;15:423

20.McDonald DG, Leopold GR. Ultrasound B-scanning in the
differentiation of Baker’s cyst and thrombophlebitis. Br J Radiol.
1972;45:729
21.Sansone V, De Ponti A, Palluello GM, et al. Popliteal cysts and
associated disorders of the knee. Critical review with Magnetic
Resonance Imaging. Int Orthop. 1995;19(5):275-9
22.Ward EE, Jacobson JA. Sonographic detection of Baker’s cysts:
Comparison with MR imaging. Am J Roëntgenol.
2001;176(2);373-80