Digestive MUSTAFA Ppt
-
Upload
mshouli2090 -
Category
Documents
-
view
223 -
download
0
Transcript of Digestive MUSTAFA Ppt
-
8/8/2019 Digestive MUSTAFA Ppt
1/111
MUSTAFA SHOULI
RN,BSN,MPHS
IBN SINA COLLEGE
PALESTINEMEDICAL SURGICAL NURSING
DEPARTMENT
MIDWIFERY STUDENTS
-
8/8/2019 Digestive MUSTAFA Ppt
2/111
Assessment of Digestive and Gastrointestinal
Function(p1121)Learning Objectives
On completion of this chapter, the learner will be able to:
Describe the structure and function of the organs of the
gastrointestinal (GI) tract
Describe the mechanical and chemical processesinvolved in digesting and absorbing foods and eliminatingwaste products.
Use assessment parameters appropriate for determiningthe status of GI function.
Describe the appropriate preparation, teaching, andfollow-up care for patients who are undergoing diagnostic
testing of the GI tract.
-
8/8/2019 Digestive MUSTAFA Ppt
3/111
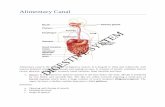
Anatomic and Physiologic
Overview The gastrointestinal (GI) tract is a 23- to
26-foot-long pathway that extends from
the mouth to the esophagus, stomach,small and large intestines, and rectum, to
the terminal structure, the anus (Fig. 34-1)
-
8/8/2019 Digestive MUSTAFA Ppt
4/111
-
8/8/2019 Digestive MUSTAFA Ppt
5/111
-
8/8/2019 Digestive MUSTAFA Ppt
6/111
The esophagus is located in the
mediastinum
in the thoracic cavity, anterior to the
spine and posterior to the trachea and
heart.
-
8/8/2019 Digestive MUSTAFA Ppt
7/111
The stomach can be divided into
four anatomic regions:
-
8/8/2019 Digestive MUSTAFA Ppt
8/111
-
8/8/2019 Digestive MUSTAFA Ppt
9/111
The common bile duct, which allowsfor the passage of both bile and
pancreatic secretions, empties into the
duodenum at the ampulla of Vater.
-
8/8/2019 Digestive MUSTAFA Ppt
10/111
-
8/8/2019 Digestive MUSTAFA Ppt
11/111
-
8/8/2019 Digestive MUSTAFA Ppt
12/111
The large intestine consists of :
1-ascending segment on the right sideof the abdomen.
2- a transverse segment that extends
from right to left in the upper abdomen.
3- a descending segment on the left
side of the
abdomen.
-
8/8/2019 Digestive MUSTAFA Ppt
13/111
-
8/8/2019 Digestive MUSTAFA Ppt
14/111
FUNCTION OF THE DIGESTIVE
SYSTEM
1 The break down of food particles into
Digestion.the molecular form for
2 The absorption into the bloodstreamthe small molecules produced by
digestion.
3 The elimination undigested and
unabsorbed foodstuffs and Other waste
products from the body.
-
8/8/2019 Digestive MUSTAFA Ppt
15/111
Go to p1123
Chewing and swallowing Gastric function
Small intestine function
Colonic function and waste products ofdigestion
-
8/8/2019 Digestive MUSTAFA Ppt
16/111
The stomach can produce about 2.4 L per
day of these gastric secretions.
Intrinsic factor is also secreted by the gastricmucosa.
In the absence of intrinsic factor, vitamin B12
cannot be absorbed and pernicious anemia
results .
Intestinal secretions total approximately:
1) 1 L/day of pancreatic juice.
2) 0.5 L/day of bile.3) 3 L/day of secretions from the glands of
the small intestine.
-
8/8/2019 Digestive MUSTAFA Ppt
17/111
Absorption is the primary function of the
small intestine.
Absorption begins in the jejunum
Absorption of different nutrients takes place
at different locations in the small intestine.
(Give examples). The brown color of the feces results from
the breakdown of bile by the intestinal
bacteria.
Chemicals formed by intestinal bacteria
(especially indole and skatole) are
responsible in large part for the fecal odor.
-
8/8/2019 Digestive MUSTAFA Ppt
18/111
The internal sphincter iscontrolled by the autonomic
nervous system.
the external sphincter is
under the conscious control
of the cerebral cortex
-
8/8/2019 Digestive MUSTAFA Ppt
19/111
Assessment
HEALTH HISTORY AND CLINICALMANIFESTATIONS:
complete history
any previous GI disease .
past and current medication .
Information pertaining to medications
is of particular interest, Why?a dietary history.
-
8/8/2019 Digestive MUSTAFA Ppt
20/111
tobacco and alcohol
changes in appetite
stool characteristics
questions about psychosocial,
spiritual, or cultural factors that may beaffecting the patient.
-
8/8/2019 Digestive MUSTAFA Ppt
21/111
Assess Clinical Manifestations
Pain
-
8/8/2019 Digestive MUSTAFA Ppt
22/111
Indigestion (Dyspepsia)
Intestinal Gas(2 types).
Nausea and Vomiting
Change in Bowel Habits andStool Characteristics
-
8/8/2019 Digestive MUSTAFA Ppt
23/111
PHYSICAL ASSESSMENT
includes assessment of the mouth,abdomen, and rectum.
The patient lies supine with kneesflexed slightly auscultation, palpation,and percussion of the abdomen. (Fig.34-4).
The nurse performs inspection firstThe nurse performs auscultation before
percussion and palpation. Why?
-
8/8/2019 Digestive MUSTAFA Ppt
24/111
It is important to documentthe frequency of the sounds
The final part of the
examination is inspection ofthe anal and perineal area
-
8/8/2019 Digestive MUSTAFA Ppt
25/111
Diagnostic Evaluation
Blood tests are ordered initially
a) Common blood tests include complete
blood count (CBC).
b) PT, PTT
c) Amylase, Lipase.
d) carcino embryonic antigen (CEA).
e) liver function tests.f) serum cholesterol, and triglycerides.
-
8/8/2019 Digestive MUSTAFA Ppt
26/111
STOOL TESTS
ABDOMINAL ULTRASONOGRAPHY
-
8/8/2019 Digestive MUSTAFA Ppt
27/111
Imaging studies include:
1- x- ray and contrast studies2- computed tomography (CT) scans
3- magnetic resonance imaging (MRI)
4- scintigraphy (radionuclide imaging).
-
8/8/2019 Digestive MUSTAFA Ppt
28/111
Fluoroscopic examination
-
8/8/2019 Digestive MUSTAFA Ppt
29/111
Lower Gastrointestinal Tract
Study
-
8/8/2019 Digestive MUSTAFA Ppt
30/111
-
8/8/2019 Digestive MUSTAFA Ppt
31/111
When barium is instilled rectally to
visualize the lower GI
tract, theprocedure is called a barium enema.
The purpose of a barium enema is to
detect the presence of polyps, tumors,
and other lesions of the large intestineand to demonstrate any abnormal
anatomy or malfunction of the bowel.
-
8/8/2019 Digestive MUSTAFA Ppt
32/111
Computed Tomography
-
8/8/2019 Digestive MUSTAFA Ppt
33/111
Magnetic Resonance Imaging
-
8/8/2019 Digestive MUSTAFA Ppt
34/111
ENDOSCOPIC PROCEDURES
Fibroscopy/esophagogastroduodenoscopy
(EGD).
Anoscopy
Proctoscopy
Sigmoidoscopy
Colonoscopy
Small-bowel enteroscopyEndoscopy through ostomy.
-
8/8/2019 Digestive MUSTAFA Ppt
35/111
esophagogastroduodenoscopy
(EGD)
-
8/8/2019 Digestive MUSTAFA Ppt
36/111
Endoscopic retrograde
Cholangiopancreatography
(ERCP)uses the endoscope in combination
with radiographic techniques to view
the ductal structures of the biliary tract.ERCP is helpful in evaluating jaundice,
pancreatitis, pancreatic tumors,
common duct stones, and biliary tractdisease.
-
8/8/2019 Digestive MUSTAFA Ppt
37/111
LAPAROSCOPY
(PERITONEOSCOPY)P1139
Laparoscopy can be used for the
diagnosis of GI disease.
This procedure is performed through asmall incision in the abdominal wall.
Go to Video Downloading.
-
8/8/2019 Digestive MUSTAFA Ppt
38/111
-
8/8/2019 Digestive MUSTAFA Ppt
39/111
-
8/8/2019 Digestive MUSTAFA Ppt
40/111
-
8/8/2019 Digestive MUSTAFA Ppt
41/111
Abnormalities of the Lips
Actinic cheilitis
-
8/8/2019 Digestive MUSTAFA Ppt
42/111
)Herpes simplex (coldsore or2
fever blister)
-
8/8/2019 Digestive MUSTAFA Ppt
43/111
-
8/8/2019 Digestive MUSTAFA Ppt
44/111
3- Chancre
-
8/8/2019 Digestive MUSTAFA Ppt
45/111
GASTROESOPHAGEAL REFLUX
DISEASE
Definition: (GERD)
gastroesophageal reflux (backflow of gastric
or duodenal contents into the esophagus).
Excessive reflux may occur because of an
incompetent lower esophageal sphincter,
pyloric stenosis, or a motility disorder.
The incidence of refux seems to increasewith aging.
-
8/8/2019 Digestive MUSTAFA Ppt
46/111
Clinical Manifestations
1- pyrosis (burning sensation in theesophagus).
2- dyspepsia (indigestion).
3- regurgitation.4- dysphagia or odynophagia (difficulty
swallowing, pain on swallowing).
5- hypersalivation.
6- and esophagitis. The symptoms may mimic those of a heart
attack.
-
8/8/2019 Digestive MUSTAFA Ppt
47/111
Assessment and Diagnostic
Findings
Endoscopy
barium swallow
(To evaluate damage to the esophagealmucosa).
-
8/8/2019 Digestive MUSTAFA Ppt
48/111
Management
Management begins with teaching the
patient to avoid .
medications such as antiacids orhistamine receptor blockers.
Proton pump inhibitors (medications
that decrease the release of gastric
acid, such as lansoprazole [Prevacid]
or rabeprazole [Aciphex]) may be used.
-
8/8/2019 Digestive MUSTAFA Ppt
49/111
If medical management is unsuccessful,surgical intervention may be necessary.
Surgical management involves afundoplication
(wrapping of a portion of the gastric fundusaround the sphincter area of the esophagus).
Fundoplication may be performed bylaparoscopy.
In a fundoplication, the gastric fundus (upperpart) of the stomach is wrapped, or plicated,around the lower end of the esophagus andstitched in place, reinforcing the closingfunction of the lower esophageal sphincter:
-
8/8/2019 Digestive MUSTAFA Ppt
50/111
fundoplication
-
8/8/2019 Digestive MUSTAFA Ppt
51/111
Gastritis
(inflammation of the gastric or stomach
mucosa).
Gastritis may be acute, lasting severalhours to a few days, or chronic,
resulting from repeated exposure to
irritating agents or recurring episodes
of acute gastritis.
-
8/8/2019 Digestive MUSTAFA Ppt
52/111
-
8/8/2019 Digestive MUSTAFA Ppt
53/111
6) A more severe form of acute gastritis
is caused by the ingestion of strong
acid or alkali, which may cause themucosa to become gangrenous or to
perforate.
Scarring can occur, resulting in pyloricobstruction.
Gastritis also may be the first sign of
an acute systemic infection.
-
8/8/2019 Digestive MUSTAFA Ppt
54/111
Chronic gastritis
Causes:
1) by either benign or malignant ulcers of thestomach
2) or by the bacteria Helicobacter pylori.
3) associated with autoimmune diseases suchas pernicious anemia.
4) dietary factors such as caffeine; the use
of medications, especially NSAIDs; alcohol;
smoking.5) or reflux of intestinal contents into the
stomach.
-
8/8/2019 Digestive MUSTAFA Ppt
55/111
Pathophysiology
the gastric mucous membrane becomes
edematous and hyperemic (congested with
fluid and blood) and undergoes superficial
erosion (Fig. 37-1). It secretes a scanty amount of gastric juice,
containing very little acid but much mucus.
Superficial ulceration may occur and can
lead to hemorrhage. (Look Photo)
-
8/8/2019 Digestive MUSTAFA Ppt
56/111
-
8/8/2019 Digestive MUSTAFA Ppt
57/111
-
8/8/2019 Digestive MUSTAFA Ppt
58/111
-
8/8/2019 Digestive MUSTAFA Ppt
59/111
Clinical Manifestations
The patient with acute gastritis
abdominal discomfort.
headache, lassitude, nausea, anorexia,vomiting, and hiccupping.
Some patients, however, have no
symptoms.
-
8/8/2019 Digestive MUSTAFA Ppt
60/111
The patient with chronic gastritis
Anorexia.
heartburn after eating.
Belching.
a sour taste in the mouth.
or nausea and vomiting.
Patients with chronic gastritis fromvitamin deficiency usually have
evidence of malabsorption of vitaminB12 caused by antibodies againstintrinsic factor.
-
8/8/2019 Digestive MUSTAFA Ppt
61/111
Diagnostic Findings:
Endoscopy.
upper GI radiographic studies.
histologic examination of a tissue
specimen obtained by biopsy.
H. pyloriinclude serologic testing for
antibodies against the H. pyloriantigen.
-
8/8/2019 Digestive MUSTAFA Ppt
62/111
Medical Management
The gastric mucosa is capable of repairing
itself after a bout of gastritis.
(As a rule, the patient recovers in about 1
day, although the appetite may bediminished for an additional 2 or 3 days).
Acute gastritis is also managed by
instructing the patient to refrain from alcohol
and food until symptoms subside.
-
8/8/2019 Digestive MUSTAFA Ppt
63/111
After the patient can take nourishment by
mouth, a nonirritating diet is recommended.
If the symptoms persist,fluids may need tobe administered parenterally.
If bleeding is present, management is similar
to the procedures used for upper GI tract
hemorrhage.
If gastritis is caused by ingestion of strong
acids or alkalis, treatment consists of
diluting and neutralizing the offending agent.
To neutralize acids, common antacids (eg,
aluminum hydroxide) are used.
-
8/8/2019 Digestive MUSTAFA Ppt
64/111
to neutralize an alkali, diluted lemon juice ordiluted vinegar is used.
If corrosion is extensive or severe, emeticsand lavage are avoided because of thedanger of perforation and damage to theesophagus.
Therapy is supportive and may includenasogastric (NG) intubation, analgesicagents and sedatives, antacids, andintravenous (IV) fluids.
Fiberoptic endoscopy may be necessary.
In extreme cases, emergency surgery may berequired to remove gangrenous or perforatedtissue.
-
8/8/2019 Digestive MUSTAFA Ppt
65/111
Gastrojejunostomy or gastric resection may benecessary to treat pyloric obstruction, a
narrowing of the pyloric orifice. Chronic gastritis is managed by modifying
the patients diet, promoting rest, reducingstress, and initiating pharmacotherapy.
H. pylorimay be treated with antibiotics (eg,tetracycline or amoxicillin, combined withclarithromycin) and a proton pump inhibitor(eg, lansoprazole [Prevacid]), and possiblybismuth salts (Pepto-Bismol) (Table 37-1).
Research is being conducted to develop avaccine against H. pylori.
-
8/8/2019 Digestive MUSTAFA Ppt
66/111
antrectomy: removal of the pyloric
(antrum) portion of the stomach with
anastomosis
(surgical connection) to the duodenum
A t t i th ti i l l f
-
8/8/2019 Digestive MUSTAFA Ppt
67/111
An antrectomy is the resection, or surgical removal, of apart of the stomach known as the antrum. The antrum isthe lower third of the stomach that lies between the body
of the stomach and the pyloric canal, which empties intothe first part of the small intestine. It is also known as theantrum pyloricum or the gastric antrum. Because anantrectomy is the removal of a portion of the stomach, itis sometimes called a partial or subtotal gastrectomy.
Purpose An antrectomy may be performed to treat several
different disorders that affect the digestive system:
Peptic ulcer disease (PUD). An antrectomy may be doneto treat complications from ulcers that have not
responded to medical treatment.
-
8/8/2019 Digestive MUSTAFA Ppt
68/111
(gastroduodenostomy or Billroth I)
-
8/8/2019 Digestive MUSTAFA Ppt
69/111
anastomosis to the jejunum
(gastrojejunostomyor Billroth II)
-
8/8/2019 Digestive MUSTAFA Ppt
70/111
-
8/8/2019 Digestive MUSTAFA Ppt
71/111
-
8/8/2019 Digestive MUSTAFA Ppt
72/111
dumping syndrome:
physiologic response to rapid emptying
of gastric contents into the jejunum,
manifested by nausea, weakness,
sweating, palpitations, syncope, and
possibly diarrhea; occurs in patients
who have had partial gastrectomy andgastrojejunostomy.
NURSING PROCESS
-
8/8/2019 Digestive MUSTAFA Ppt
73/111
NURSING PROCESS:
THE PATIENT WITH GASTRITIS Anxiety related to treatment.
Imbalanced nutrition, less than bodyrequirements, related to inadequate intake ofnutrients
Risk for imbalanced fluid volume related toinsufficient fluid intake and excessive fluidloss subsequent to vomiting.
Deficient knowledge about dietary
management and disease process. Acute pain related to irritated stomach
mucosa
-
8/8/2019 Digestive MUSTAFA Ppt
74/111
Gastric and Duodenal Ulcers
A peptic ulcer:
is an excavation (hollowed-outarea) that forms in the mucosal wall of the
stomach. in the pylorus (opening between stomach
and duodenum).
in the duodenum (first part of small
intestine),or in the esophagus. A peptic ulcer is frequently referred to as a
gastric, duodenal, or esophageal ulcer.
-
8/8/2019 Digestive MUSTAFA Ppt
75/111
Peptic ulcers are more likely to be in
the duodenum than in the stomach (As
a rule they occur alone, but they mayoccur in multiples).
Table 37-2 compares the features of
gastric and duodenal ulcers. Peptic ulcer disease occurs with the
greatest frequency in people between
the ages of 40 and 60 years.
-
8/8/2019 Digestive MUSTAFA Ppt
76/111
-
8/8/2019 Digestive MUSTAFA Ppt
77/111
The ingestion of milk and caffeinated
beverages, smoking, and alcohol also may
increase HCl secretion. Familial tendency may be a significant
predisposing factor.
A further genetic link is noted in the finding
that people with blood type O are more
susceptible to peptic ulcers than are those
with blood type A, B, or AB.
There also is an association betweenduodenal ulcers and chronic pulmonary
disease or chronic renal disease.
Oth di i f t i t d
-
8/8/2019 Digestive MUSTAFA Ppt
78/111
Other predisposing factors associatedwith peptic ulcer include chronic use of
NSAIDs, alcohol ingestion, andexcessive smoking.
Rarely, ulcers are caused by excessiveamounts of the hormone gastrin,
produced by tumors. This Zollinger-Ellison syndrome (ZES)
consists of severe peptic ulcers,extreme gastric hyperacidity, andgastrin secreting benign or malignanttumors of the pancreas.
St l hi h li i ll
-
8/8/2019 Digestive MUSTAFA Ppt
79/111
Stress ulcers, which are clinicallydifferent from peptic ulcers, are
ulcerations in the mucosa that canoccur in the gastroduodenal area.
Stress ulcers may occur in patientswho are exposed to stressful
conditions. Esophageal ulcers
occur as a result of the backward flow
ofHCl from the stomach into theesophagus (gastroesophageal re.uxdisease [GERD]).
-
8/8/2019 Digestive MUSTAFA Ppt
80/111
Table 37-2 Comparing Duodenal and
Gastric Ulcers
Pathophysiology
-
8/8/2019 Digestive MUSTAFA Ppt
81/111
Pathophysiology
Peptic ulcers occur mainly in thegastroduodenal mucosa because this tissuecannot withstand the digestive action ofgastric acid (HCl) and pepsin.
The erosion is caused by the increasedconcentration or activity of acid-pepsin, orby decreased resistance of the mucosa.
A damaged mucosa cannot secrete enoughmucus to act as a barrier against HCl.
The use of NSAIDs inhibits the secretion ofmucus that protects the mucosa.
-
8/8/2019 Digestive MUSTAFA Ppt
82/111
Patients with duodenal ulcer diseasesecrete more acid than normal,
whereas patients with gastric ulcertend to secrete normal or decreasedlevels of acid.
ZES is suspected when a patient hasseveral peptic ulcers or an ulcer that isresistant to standard medical therapy.
It is identified by the following findings:
hypersecretion of gastric juice,duodenal ulcers, and gastrinomas (isletcell tumors) in the pancreas.
-
8/8/2019 Digestive MUSTAFA Ppt
83/111
Stress ulcer
is the term given to the
acute mucosal ulceration of the
duodenal or gastric area that occurs
after physiologically stressful events,
such as burns, shock, severe sepsis,and multiple organ traumas.
Usually, it is preceded by shock; this
leads to decreased gastric mucosalblood flow and to reflux of duodenal
contents into the stomach.
-
8/8/2019 Digestive MUSTAFA Ppt
84/111
In addition, large quantities of pepsin
are released.
The combination of ischemia, acid, and
pepsin creates an ideal climate for
ulceration.
Stress ulcers should be distinguishedfrom Cushings ulcers
-
8/8/2019 Digestive MUSTAFA Ppt
85/111
Clinical Manifestations
1)pain or a burning sensation in the
midepigastrium or in the back.
2) pyrosis (heartburn)
3)vomiting.
4) constipation or diarrhea.
5) bleeding.
Assessment and Diagnostic
-
8/8/2019 Digestive MUSTAFA Ppt
86/111
Assessment and Diagnostic
Findings A physical examination may reveal pain, epigastric
tenderness, or abdominal distention.
A barium study of the upper GI tract may show anulcer.
Endoscopy is the preferred diagnostic procedurebecause it allows direct visualization of inflammatorychanges, ulcers, and lesions.
Through endoscopy, a biopsy of the gastric mucosaand of any suspicious lesions can be obtained.
Endoscopy may reveal lesions that are not evident
on x-ray because of their size or location. Stools may be tested periodically until they are
negative for occult blood.
-
8/8/2019 Digestive MUSTAFA Ppt
87/111
Gastric secretory studies are of value
in diagnosing achlorhydria and ZES.
H. pyloriinfection may be determined
by biopsy and histology with culture.
There is also a breath test that detects
H. pylori, as well as a serologic test forantibodies to the H. pyloriantigen.
Pain that is relieved by ingesting food
or antacids and absence of pain onarising are also highly suggestive of an
ulcer
-
8/8/2019 Digestive MUSTAFA Ppt
88/111
Medical Management
Once the diagnosis is established, thepatient is informed that the problem can becontrolled.
Recurrence may develop.
peptic ulcers treated with antibiotics toeradicate H. pylorihave a lower recurrencerate than those not treated with antibiotics.
The goals are to eradicate H. pyloriand to
manage gastric acidity. Methods used include medications,
lifestyle changes, and surgical intervention.
-
8/8/2019 Digestive MUSTAFA Ppt
89/111
B) STRESS REDUCTION AND REST
-
8/8/2019 Digestive MUSTAFA Ppt
90/111
B) STRESSREDUCTION AND REST
C) SMOKING CESSATION
D) DIETARYMODIFICATION
E) SURGICAL MANAGEMENT
surgery is usually recommended
for patients with intractable ulcers (those that fail toheal after 12 to 16 weeks of medical treatment).
life-threatening hemorrhage,perforation, orobstruction, and for those with ZES not respondingto medications
(Surgical procedures include vagotomy, with orwithout pyloroplasty, and the Billroth I and Billroth II
procedures (Table 37-3; see also the section ongastric surgery later in this chapter).
-
8/8/2019 Digestive MUSTAFA Ppt
91/111
Patients who need ulcer surgery may
have had a long illness. They may be
discouraged and have had
interruptions in their work role and
pressures in their family life.
THE PATIENT WITH ULCER
-
8/8/2019 Digestive MUSTAFA Ppt
92/111
THE PATIENT WITH ULCER
DISEASE
NURSING DIAGNOSES Acute pain related to the effect of gastric acid
secretion on damaged tissue
Anxiety related to coping with an acutedisease
Imbalanced nutrition related to changes in
diet
Deficient knowledge about prevention of
symptoms and management of the condition
Abnormalities of Fecal
-
8/8/2019 Digestive MUSTAFA Ppt
93/111
Abnormalities of Fecal
Elimination Changes in patterns of fecal elimination are
symptoms of functional disorders or disease of theGI tract.
The most common changes seen are constipation,
diarrhea, and fecal incontinence. The nurse should be aware of the possible causes
and therapeutic management of these problems andof nursing management techniques.
Education is important for patients with these
abnormalities.
-
8/8/2019 Digestive MUSTAFA Ppt
94/111
CONSTIPATION
Constipation is a term used to describe
an abnormal infrequency or irregularity
of defecation, abnormal hardening of
stools that makes their passagedifficult and sometimes painful, a
decrease in stool volume, or retention
of stool in the rectum for a prolongedperiod.
Constipation can be caused by :
-
8/8/2019 Digestive MUSTAFA Ppt
95/111
Constipation can be caused by :
1- certain medications (ie,tranquilizers,anticholinergics,
antidepressants, antihypertensives, opioids,antacids with aluminum, and iron).
2- rectal or anal disorders (eg, hemorrhoids,fissures).
3- obstruction (eg, cancer of the bowel).4- metabolic, neurologic, and neuromuscularconditions (eg, diabetes mellitus,Hirschsprungs disease, Parkinsonsdisease, multiple sclerosis).
5- endocrine disorders (eg, hypothyroidism,pheochromocytoma).
-
8/8/2019 Digestive MUSTAFA Ppt
96/111
M l d l i i
-
8/8/2019 Digestive MUSTAFA Ppt
97/111
Many people develop constipation
because they do not take the time to
defecate or they ignore the urge todefecate.
In the United States, constipation is
also a result of dietary habits (ie, lowconsumption of fiber and inadequate
fluid intake), lack of regular exercise,
and a stress-filled life.
-
8/8/2019 Digestive MUSTAFA Ppt
98/111
Any of the causative factors previously
-
8/8/2019 Digestive MUSTAFA Ppt
99/111
Any of the causative factors previously
identified can interfere with any of
these three processes.Go to page 201
-
8/8/2019 Digestive MUSTAFA Ppt
100/111
Assessment and Diagnostic
-
8/8/2019 Digestive MUSTAFA Ppt
101/111
Assessment and Diagnostic
Findings
patients history.
physical examination.
barium enema or sigmoidoscopy.
stool testing for occult blood. Anorectal manometry (ie, pressure studies)
may be performed to determine malfunctionof the muscle and sphincter.
Defecography and bowel transit studies canalso
assist in the diagnosis.
-
8/8/2019 Digestive MUSTAFA Ppt
102/111
M di l M t
-
8/8/2019 Digestive MUSTAFA Ppt
103/111
Medical Management
Treatment is aimed at the underlyingcause of constipation and includeseducation, bowel habit training,
increased fiber and fluid intake, andjudicious use of laxatives.
Management may also includediscontinuing laxative abuse.
Routine exercise to strengthenabdominal muscles is encouraged.
-
8/8/2019 Digestive MUSTAFA Ppt
104/111
-
8/8/2019 Digestive MUSTAFA Ppt
105/111
-
8/8/2019 Digestive MUSTAFA Ppt
106/111
DIARRHEA
-
8/8/2019 Digestive MUSTAFA Ppt
107/111
DIARRHEA
Diarrhea is increased frequency of
bowel movements (more than three per
day), increased amount of stool (more
than 200 g per day), and alteredconsistency (ie, looseness) of stool.
It is usually associated with urgency,
perianal discomfort, incontinence, or acombination of these factors.
P th h i l
-
8/8/2019 Digestive MUSTAFA Ppt
108/111
Pathophysiology
Types of diarrhea include secretory,
osmotic, and mixed diarrhea.
Secretory diarrhea is usually high-
volume diarrhea and is caused by
increased production and secretion of
water and electrolytes by the intestinal
mucosa into the intestinal lumen.
-
8/8/2019 Digestive MUSTAFA Ppt
109/111
Osmotic diarrhea occurs when water is
pulled into the intestines by theosmotic pressure of unabsorbed
particles, slowing the reabsorption of
water.
Mixed diarrhea is caused by increased
peristalsis (usually from IBD) and a
combination of increased secretion and
decreased absorption in the bowel.
-
8/8/2019 Digestive MUSTAFA Ppt
110/111
-
8/8/2019 Digestive MUSTAFA Ppt
111/111













![[PPT]Digestive System Infections - The University of …ocean.otr.usm.edu/~w536943/Courses/BSC381/Chapter 23a.ppt · Web viewArial Default Design Digestive System Infections Slide](https://static.fdocuments.us/doc/165x107/5afd280c7f8b9a944d8d115f/pptdigestive-system-infections-the-university-of-oceanotrusmeduw536943coursesbsc381chapter.jpg)