Differential Diagnosis in Head and Neck Lesions
Transcript of Differential Diagnosis in Head and Neck Lesions

A
Received October 1 5, 1 990; accepted after revision December 1 7, 1990.
1 Both authors: Department of Radiology, University of Utah Medical Center, 50 N. Medical Dr., Salt Lake City, UT 841 32. Address reprint requests to H. A.
Harnsberger.
AJR 157:147-154, July 1991 0361-803x/91/1571-0147 © American Roentgen Ray Society
147
Pictorial Essay
Differential Diagnosis of Head and Neck Lesions Based onTheir Space of Origin. 1. The Suprahyoid Part of the NeckH. Ric Harnsberger1 and Anne G. Osborn
This pictorial essay reviews the spaces of the suprahyoid
portion of the head and neck, focusing on the normal spatialanatomy as defined by the deep cervical fascia, the appearanceof a generic mass in each of the spaces defined, and the uniquedifferential diagnoses involved in each individual space.
The cylindrical soft-tissue core of the extracranial portionof the head and neck, excluding the more anterior parts ofthe orbit, sinonasal region, and oral cavity, can be subdividedat the hyoid bone into two distinct regions: the suprahyoid
and infrahyoid portions. The three layers of deep cervicalfascia that cleave this area of the body into functional spacesconverge on the hyoid bone, dividing the neck into these twoparts (Fig. 1) [i , 2]. The suprahyoid area encompasses thedeep spaces between the skull base and hyoid bone, and theinfrahyoid portion lies inferiorly between the hyoid bone andthe clavicles.
In the suprahyoid area, the three layers of deep cervicalfascia delineate the individual spaces of the deep part of theface (Figs. i -4). As the contents of these spaces are some-
Fig. 1.-A and B, Axial drawing (A)and corresponding MR image (B) ofnormal anatomy of mid nasopharynx.Left side of drawing shows critical nor-mal anatomy of region. Right sideshows three layers of deep cervicalfascia and spaces they define. See keyon page 148. (Reprinted with permis-sion from Harnsberger [2].)
B

Key to Abbreviations and Symbols Used in Figuresi buccinator muscle5 hyoglossus muscle6 intrinsic muscles of tongue7 lateral pterygoid muscle8 masseter muscle9 medial pterygoid muscle
i 0 mylohyoid muscleii palatoglossus muscle (anterior tonsillar pillar)i 2 palatopharyngeus muscle (posterior tonsillar
pillar)paraspinal musclesplatysma muscleprevertebral muscles
soft palateuvulahyoid boneramus of the mandiblemandibular canalstyloid processtemporalis muscle
tensor veli palatini musclelevator veli palatini muscle
spinal accessory nervetorus tubariuslateral pharyngeal recess (fossa of Rosenm#{252}ller)
musclestyloglossus musclesuperior pharyngeal constrictor muscletrapezius muscleinferior alveolar nerve (branch of V3)lingual nerve (branch of V3)facial nerve (VII)
4950Si53
545758
59
60616263a65
CSDSmMS
nPCSPMSPPSPSPVSRPSSLSSMSTS
13
14
15
1617
18
19202122232425263031323334353637
arterybuccal spacecarotid spacedanger spacemusclemasticator spacenode
glossopharyngeal nerve (IX)vagus nerve (X)hypoglossal nerve (XII)sympathetic plexusexternal carotid arteryinternal carotid arteryinternal maxillary arterylingual arteryfacial veinjugular veinpharyngeal venous plexusretromandibular vein
posterior cervical spacepharyngeal mucosal spaceparapharyngeal spaceparotid spaceprevertebral spaceretropharyngeal spacesublingual spacesubmandibular spacetemporal space (suprazygomatic masticator
space)v vein
40 adenoids41 faucial tonsil43 parotid gland45 submandibular gland46 submandibular gland duct48 cartilaginous eustachian tube
heavy black line outlines pharyngobasilar fascia
_____medium black line outlines superficial layer of
deep cervical fasciadotted line outlines middle layer of deep cervical
fascia------ broken line outlines deep layer of deep cervical
fascia
i 48 HARNSBERGER AND OSBORN AJR:157, July 1991
The parapharyngeal space is an area of fatty areolar tissue Anterior to the parapharyngeal space is the masticator
what unique, differential diagnostic possibilities can be sug-gested when a lesion is identified within a given space (Table1). A simple method of assigning a suprahyoid lesion to aspecific space of origin is accomplished by establishing thecenter of the lesion and assessing its displacement of theparapharyngeal space fat (Figs. 5-8) [2, 4]. This method isparticularly effective in lesions involving the four spaces sur-rounding the parapharyngeal space: the pharyngeal mucosal(Fig. 5), masticator (Fig. 6), parotid (Fig. 7), and carotid (Fig.8) spaces.
Lesions involving the two midline spaces, the retropharyn-geal and prevertebral spaces, are best evaluated by notingthe relationship of the lesion to the prevertebral muscles. Aretropharyngeal space lesion displaces the prevertebral mus-des posteriorly (Fig. 9), whereas a prevertebral space lesiondisplaces the muscles anteriorly (Fig. i 0) [4].
with complex fascial margins that lies in a central location inthe deep face (Figs. 1-3). It extends from the skull base tothe hyoid bone, containing only fat, branches of the trigemmnalnerve, and the pterygoid venous plexus. In order to definitelyascribe a lesion as primary to the parapharyngeal space, fatmust be identified surrounding the whole circumference ofthe lesion [5].
The pharyngeal mucosal space is medial to the parapha-ryngeal space. It is delimited by the middle layer of deepcervical fascia (Fig. 5). Its major contents include the mucosa,lymphoid tissues of Waldeyer ring, minor salivary glands,cartilaginous eustachian tube, superior and middle constrictormuscles, pharyngobasilar fascia, and levator palatini muscles.A mass in the pharyngeal mucosal space is centered medialto the parapharyngeal space, displacing it laterally (Fig. 5A)[2,4].

.. 0
/
Fig. 3.-A and B, Coronal drawing (A) with corresponding MR image (B) of normal anatomy of spacesof suprahyoid part of neck. Note craniocaudal extent of these spaces, especially parapharyngeal andmasticator spaces. Critical contents of spaces on left three layers of deep cervical fascia on right. Seekey on page 148. (Reprinted with permission from Harnsberger [2].)
Fig. 4.-Axialdrawing of skull base showsrelationship of spaces of suprahyoid part ofneck to skull base apertures. Foramen ovale(FO), through which passes mandibular divi-sion of trigeminal nerve, empties into masti-cator space, whereas stylomastold foremen(SF) transmits facial nerve directly into pa-rotid space. Carotid space receives cranialnerves lX-Xl from jugular foramen (J) andcranial nerve XII from hypoglossal canal(HC). FL = foramen lacerum, FS = foramenspinosum, C = carotid canal. See key onpage 148. (Reprinted with permission fromOsborn et al [3].)
AJR:157, July 1991 SITES OF SUPRAHYOID LESIONS 149
Fig. 2.-A and B, Axial drawing (A)and corresponding MR image (B) ofnormal anatomy of mid oropharynx.Critical contents of spaces are on leftthree layers of deep cervical fascia areon right. See key on page 148. (Re-printed with permission from Hamsber-ger [2].)
A B
B
space. The superficial layer of deep cervical fascia splits toenvelop this space. It has a suprazygomatic component (Fig.3A) and extends mnferiorly to the inferior margin of the man-dible. Principal components include the muscles of mastica-tion, ramus and posterior body of the mandible, masticatorand inferior alveolar nerves, and inferior alveolar vein andartery. A mass is said to originate from the masticator spacewhen its center is anterior to the parapharyngeal space,displacing the fat from anterior to posterior (Fig. 6A). Masti-cator space malignancy may spread permneurally along themandibular division of the trigeminal nerve into the middlecranial fossa (Fig. 6C).
Lateral to the parapharyngeal space is the parotid space.It too is circumscribed by the superficial layer of deep cervicalfascia (Fig. 7A). The superior margin of the parotid spaceabuts the external auditory canal, whereas the parotid tailoften extends mnferiorly below the inferior mandibular margin.Important contents include the parotid gland, intraparotidfacial nerve, retromandibular vein, external carotid artery, andlymph nodes. A mass is described as originating in the parotidspace when it is centered within the parotid gland lateral tothe parapharyngeal space and displaces the parapharyngealfat from lateral to medial. Associated widening of the stylo-mandibular notch (Fig. 7A) is usually seen. Parotid space

150 HARNSBERGER AND OSBORN AJA:157, July 1991
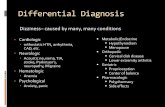
TABLE 1: Differential Diagnosis of Deep Facial Lesions Based on Their Space of Origin
Space/Type of P ssible D
Abnormality 0 agnosis
ParapharyngealPseudomass Asymmetric pterygoid venous plexusCongenital Second branchial cleft cyst, atypicalinflammatory Infection spreading from adjacent spaces
Benign tumor Pleomorphic adenoma of salivary gland rest; lipoma;nerve sheath tumors
Malignancy Malignant tumor of salivary gland rest; direct spread oftumor from adjacent spaces
Pharyngeal mucosalPseudomass Asymmetric fossa of RosenmUller; mucosal inflammation
(pharyngitis or radiation)Inflammatory Tonsil hypertrophy, tonsillitis, abscess; postinflammatory
calcification or retention cystBenign tumor Benign mixed tumor of minor salivary gland originMalignancy Squamous cell carcinoma; non-Hodgkin lymphoma; mi-
nor salivary gland malignancy; metastasesMiscellaneous Thornwaldt cyst
MasticatorPseudomass Benign masseteric hypertrophy; accessory parotid gland;
denervation atrophy (mandibular division V)Congenital Hemangioma/lymphangiomaInflammatory Odontogenic abscess, mandibular osteomyelitisBenign tumor Leiomyoma; nerve sheath tumorMalignancy Sarcoma (soft tissue, chondrosarcoma, osteosarcoma);
malignant schwannoma; non-Hodgkin lymphoma; man-dibular metastases; squamous cell carcinoma from or-opharynx
ParotidCongenital First branchial cleft cyst; hemangioma/lymphangiomaInflammatory Abscess/cellulitis/reactive adenopathy; benign lymphoep-
ithelial cysts (AIDS); autoimmune/SjOgren syndrome
Benign tumor Benign mixed tumor (pleomorphic adenoma); Warthin tu-mor; lipoma
Malignancy Mucoepidermoid carcinoma; adenoid cystic carcinoma;
non-Hodgkin lymphoma; malignant mixed tumor;other: acinar cell carcinoma, adenocarcinoma, squa-mous cell carcinoma
Metastases Skin squamous cell carcinoma or melanoma; breast orlung carcinoma; nodal non-Hodgkin lymphoma
CarotidPseudomass Ectatic common or internal carotid artery; asymmetric
internal jugular vein
Inflammatory Carotid space cellulitis or abscessVascular Jugular vein thrombosis or thrombophlebitis; internal ca-
rotid artery mural thrombus, aneurysm; internal carotidartery dissection
Benign tumor Paraganglioma; nerve sheath tumor (schwannoma, neu-rofibroma)
Malignancy Squamous cell carcinoma nodal metastasis; direct inva-sion by primary squamous cell carcinoma; non-Hodg-kin lymphoma; metastases
RetropharyngealPseudomass Tortuous carotid artery; edema secondary to deep ye-
nous obstructionCongenital Hemangiomainflammatory Reactive adenopathy/cellulitis/abscessBenign tumor LipomaMalignancy Nodal metastases from squamous cell carcinoma, mela-
noma, thyroid carcinoma, non-Hodgkin lymphoma; di-rect invasion from primary squamous cell carcinoma
PrevertebralPseudomass Vertebral body osteophyte/anterior disk herniation
Vascular Vertebral artery aneurysm, pseudoaneurysm, ectasiaInflammatory Vertebral body osteomyelitis
Benign tumor Chordoma; schwannoma, neurofibroma (brachial plexus);vertebral body benign bony tumors
Malignancy Vertebral body/epidural metastasis; non-Hodgkin lym-phoma; vertebral body primary malignant tumor

A
A
AJR:157, July 1991 SITES OF SUPRAHYOID LESIONS 1S1
Fig. 5.-A, Axial drawing throughlow nasopharynx shows contents andfascial boundaries of pharyngeal mu-cosal space (PMS) on left and pharyn-geal mucosal space mass on right. Mid-dlelayer of deep cervicalfascia (dottedline) encompasses posterolateral mar-gin of superior constrictor muscle, do-fining pharyngeal mucosal space. Cen-ter of pharyngeal mucosal space mass(black dot) is medial to laterally dis-placed parapharyngeal space (blackarea), invading parapharyngeal spacefrom medial to lateral. m = muscle.(Reprinted with permission from Harns-berger [4].)
B, Axial density-weighted MR imagein patient with early nasopharyngealcarcinoma (N) in lateral pharyngeal re-cess of nasopharyngeal mucosalspace. p = parapharyngeal space.
Fig. 6.-A, Axial drawing through low nasopharynx shows contentsand fascial boundaries of masticator space on left and appearanceof masticator space mass (MS) on right. Superficial layer of deepcervical fascia surrounds muscles of mastication and mandible, de-fining masticator space. Center of masticator space mass (black dot)is anterior to posteriorly displaced parapharyngeal space (blackarea), invading parapharyngeal space from anterior to posterior. Seekey on page 148. (Reprinted with permission from Harnsberger [4].)
B, Axial Ti-weighted unenhanced MR image of masticator spacechondrosarcoma (C). Tumor involves muscles of mastication andmandible.
C, Coronal MR image of masticator space malignant schwannoma(5) with perineural tumor spread along mandibular division of trigem-mel nerve (arrows) to skull base and through foramen ovale. p =
parapharyngeal space.
B
C
B
malignancy may follow the facial nerve into the temporal bone sheath that circumscribes this space (Fig. 8A). This space(Fig. 7C). extends from the skull base to the aortic arch. Its suprahyoid
Posterior to the parapharyngeal space is the carotid space. contents include the internal carotid artery, jugular vein, cra-All three layers of deep cervical fascia contribute to the carotid nial nerves IX-Xll, and deep cervical lymph node chain. A

A
A B
152 HARNSBERGER AND OSBORN AJR:157, July 1991
B
Fig. 7.-A, Axial drawing through low nasopharynx shows contents andfascial boundaries of parotid space on left and appearance of a parotidspace mass (PS) on right. Superficial layer of deep cervical fascia sur-rounds parotid gland and its contents, defining parotid space. Center ofmass (black dot) is lateral to medially displaced parapharyngeal space(black area), invading parapharyngeal space from lateral to medial. Seekey on page 148. (Reprinted with permission from Harnsberger [4].)
B, Ti-weighted axial MR image in a patient with a large benign mixedtumor (BMT) of parotid space that widens stylomandibular notch (dottedllne) and impinges on fatty parapharyngeal space from lateral to medial(open arrow). Note lack of identifiable fat plane between remaining normalparotid gland and mass (solid arrows).
C, Mucoepidermoid carcinoma of parotid space with penneural tumorfollowing mastoid segment of facial nerve. Coronal Ti-weighted MR imageshows an intraparotid tumor (T) with a long “tail” extending to posteriorgenu of facial nerve canal within adjacent temporal bone along mastoidsegment of facial nerve (arrows).
C
Fig. 8.-A, Axial drawing throughlow nasopharynx shows contents andfascial boundaries of carotid space onleft and appearance of a carotid spacemass (CS) on right. All three layers ofdeep cervical fascia contribute to ca-rotid sheath, which circumscribes ca-rotid artery, jugular vein, and associ-ated cranial nerve and lymph nodes,defining carotid space. Center of mass(blackdot) is posteriorto anteriorly dis-placed parapharyngeal space (blackarea), invading it from posterior to an-terior. a = artery, v = vein. (Reprintedwith permission from Harnsberger [4].)
B, Glomus vagale paraganglioma ofnasopharyngeal carotid space. AxialTI-weighted MR image of a right ca-
rotid space paraganglioma (PG) showsanterior displacement of parapharyn-goal space fat (P). Plethora of serpigi-nous vascular flow voids within tumorsignals its vascular nature and proba-
ble histology. Right internal carotid ar-tory is thrombosed. j = internal jugularvein.

A B
DC
A B
AJR:i57,July 1991 SITES OF SUPRAHYOID LESIONS 153
Fig. 9.-A, Axial drawing of extra-nodal mass lesion of retropharyngealspace (RPS) at level of oropharynxcausing posterior displacement of pre-vertebral muscles (arrows) within pre-vertebral space proper (PVS) and an-terior displacement of pharyngeal mu-cosal space (PMS). Note somewhat“bow tie” shape of retropharyngealspace mass. See key on page 148.(Reprinted with permission from Harns-berger [4].)
B, Squamous cell carcinoma of pos-tenor wall of oropharynx invading ad-jacent retropharyngeal space. En-hanced axial CT scan shows tumor (T)within oropharyngeal retropharyngealspace. Pharyngeal mucosal space(broken line) is displaced anteriorly,whereas prevertebral muscles (p) areflattened along their anterior surface.
C, Axial drawing through low naso-pharynx shows appearance of nodalmass lesion of retropharyngeal space(RPS), which has its center (black dot)posteromedial to parapharyngealspace (black area) and displaces it an-terolaterally (compare with Fig. 8A).Carotid space masses can be confusedwith lateral retropharyngeal space le-sions unless there is awareness of theirunique characteristics. Key differentialfeature is direction of displacement ofcarotid space contents, especially ca-rotid artery. In lateral retropharyngealspace masses, internal carotid arteryis displaced laterally. (Reprinted withpermission from Harnsberger [4].)
D, Malignant squamous cell carci-noma node within lateral nodal chainof retropharyngeal space. Density-weighted MR image through low naso-pharynx reveals a lateral retropharyn-goal space malignant node (N) thatdisplaces internal carotid artery (c)posterolaterally, parapharyngeal spacefat (black p) anterolaterally, and pro-vertebral muscle (white p) posteriorly.
Fig. 10.-A, Axial drawing at level oflow oropharynx shows a mass lesionoriginating within prevertebral space(PVS) proper with anterior displace-ment of prevertebral muscles (arrows),retropharyngeal space (RPS), and pha-ryngeal mucosal space (PMS). As iscommonly the case in infection and ma-lignancy of the prevertebral space, ver-tebral body is partially destroyed bylesion. See key on page 148. (Re-printed with permission from Harnsber-ger [4].
B, Colonic metastasis to lower clivuswith extension into adjacent preverte-bral space. Axial Ti-weighted MR im-age shows clival colonic metastaticdeposit (CM) extending into adjacentprevertebral space (asterisks). Pre-vertebral muscles (m) are displacedanteriorly.

154 HARNSBERGER AND OSBORN AJR:i57, July 1991
mass lesion is primary to the carotid space when it is centeredposterior to the parapharyngeal space and displaces it ante-riorly (Fig. 8B).
The retropharyngeal space is a posterior midline space thathas the middle layer of deep cervical fascia as its anteriormargin and the deep layer of deep cervical fascia as itsposterior and lateral margins (Fig. 9A). It extends from theskull base to the level of the T3 vertebral body. The supra-
hyoid retropharyngeal space contains only lymph nodes andfat. When disease affects the retropharyngeal space diffusely,the prevertebral muscles are seen to be displaced posteriorly(Fig. 9B). When the mass occurs in the laterally placed nodes,
it will impinge on the parapharyngeal space posteromedially
(Figs. 9C and 9D).The prevertebral space proper is defined by the deep layer
of deep cervical fascia as it passes superficial to the prever-tebral muscles to attach to the cervical transverse processes
(Fig. 1 OA). This space contains the prevertebral muscles; thevertebral body, artery, and vein; and the spinal cord. A lesionoriginates from the prevertebral space proper when it dis-places the prevertebral muscles anteriorly (Fig. 1 OB).
REFERENCES
1 . Grodlinsky M, Holyoke E. The fascia and fascial spaces of the head andneck and adjacent regions. Am J Anat 1938;63:367-407
2. Hamsberger HR. CT and MRI of masses of the deep face. Curr ProblDiagn Radiol i987;i6:147-173
3. Osborn AG, Harnsberger HA, Smoker WAK. Base of skull imaging. Semin
Ultrasound CTMR i986;7:91-1064. Harnsberger HR. Handbooks in radiology. Head and neck radiology vol-
ume. St. Louis: Mosby-Year Book Medical, 19905. Som PM, Sacher M, Stollman AL, Biller HF, Lawson W. Common tumors
of the parapharyngeal space: refined imaging diagnosis. Radiology1988:169:81-85