Dietetic Practice in the Management of Adverse Reactions to Foods
-
Upload
amaranta-nova -
Category
Documents
-
view
30 -
download
2
description
Transcript of Dietetic Practice in the Management of Adverse Reactions to Foods

Dietetic Practice in the Management of Adverse
Reactions to Foods
Clinical Practice Workshops
2009-2010

Diagnosis of Adverse Reactions to Foods
Signs, Symptoms, and Differential Diagnosis

3
The Medical Paradigm
• Signs and Symptoms suggest the disease condition
• Tests are used to provide a definitive diagnosis and suggest a probable cause
• Diagnosis determines the treatment
• Treatment typically consists of:– Medications– Surgery– Other appropriate measures

Food Allergy and the Medical Paradigm
• Food does not cause allergy– The immunological or physiological response
to the food is the cause of symptoms
• The same food can trigger entirely different symptoms in different individuals, and sometimes different symptoms in the same individual– “One cause, one disease” does not apply
4

Food Allergy and the Medical Paradigm
• A specific test will not identify the cause– Most people can eat the allergenic food
without symptoms
• Food allergy treatment involves medications to control the symptoms– There is no way to stop the allergic reaction
once it has started
• Prevention involves avoidance of the allergenic food
5

6
Signs and Symptoms of Food Sensitivities
Symptoms vary from individual to individual
Sometimes symptoms vary in presentation and severity in the same individual on different occasions
• Symptoms appear in all organ systems but tend to be most obvious in:– Skin:
• Flushing• Hives• Angioedema (swelling especially of facial areas: lips, throat,
tongue)• Itching• Eczema• Rash

7
Signs and Symptoms of Food Sensitivities
– Digestive tract:• Stomach ache• Abdominal bloating• Diarrhea• Alternating diarrhea and constipation• Nausea• Vomiting• Heart burn and reflux
– Differential diagnosis: Food sensitivity not indicated
• Weight loss• Blood in stool

8
Signs and Symptoms of Food Sensitivities
– Respiratory tract:• Stuffy nose• Runny nose• Itchy, watery eyes• Difficulty breathing, speaking, or swallowing• Throat tightening• Chest tightening

9
Signs and Symptoms of Food Sensitivities
Other organ systems:
– Drop in blood pressure– Rapid heart rate– Anxiety; sense of doom– Faintness– Paleness– Loss of consciousness

10
Signs and Symptoms
• Anaphylaxis– Involves all organ systems– In rare cases can proceed to cardiovascular
collapse– Has the very rare potential to proceed to fatal
anaphylactic shock– Management always involves administration
of injectable adrenalin (epinephrine) and immediate transportation to emergency medical facilities

Epipen and Twinject
• How to use injectable epinephrine (adrenalin)– http://foodallergies.about.com/od/emergencytr
eatment/ht/autoinjector.htm
• Free training kits available:– Epipen 1-877-374-7361– Twinject 1-877-894-6532

12
Signs and Symptoms• In babies and children:
– Digestive tract distress:• Abdominal pain• Spitting up or vomiting• Diarrhea• May be blood in stool
– Irritability– Difficulty sleeping– Failure to thrive– Eczema– Other rashes

13
Diagnosis of Food Hypersensitivity• The symptoms that suggest food
sensitivity may actually be caused by many different medical conditions
• Frequently the idea of food hypersensitivity is suggested when all other causes for the person’s symptoms have been ruled out
• Before food sensitivities are considered, ensure that other causes for the symptoms have been ruled out by appropriate medical investigations

14
Differential Diagnosis
• For example:– Celiac disease: high levels of:
• anti-tissue transglutaminase antibodies (tTGA)• anti-endomysium antibodies (EMA)
– Intestinal infection: stool analysis for:• ova and parasites for parasitic infestations• Clostridium difficile• Other pathogens or potential pathogens
– Inborn errors of metabolism

15
Potential Causes of Adverse Reactions to Foods
• IgE mediated food hypersensitivity – Food allergy and anaphylaxis– Oral allergy syndrome (OAS)– Latex-food syndrome
• Non-IgE mediated food hypersensitivity– Food protein enteropathies– Eosinophilic esophagitis– Eosinophilic gastroenteritis – Eosinophilic proctocolitis– Celiac disease

16
Potential Causes of Adverse Reactions to Foods
• Non-immunologically mediated food sensitivity (food intolerances)– Lactose intolerance– Sucrose intolerance– Fructose intolerance– Histamine intolerance– Sulphite sensitivity– Nickel sensitivity– Sensitivity to food additives:
• Tartrazine and other azo dyes• Benzoates

17
Treatment of Adverse Reactions to Food
• Whatever the physiological basis of the reaction, dietetic management is the same:– Accurate identification of the food
components responsible– Avoidance of the offending food ingredient– Provision of a diet that provides complete
balanced nutrition from alternative sources– Recognition of the development of tolerance

18
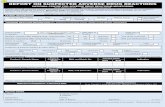
Exercise 1 : Signs and Symptoms Questionnaire

IDENTIFYING THE CULPRITS
Tests

20
Primary RequirementAccurate Identification of the Culprit
Foods
• There is a lack of definitive diagnostic tests for food allergies, food intolerances, and other adverse reactions to foods
• Skin tests and blood tests detect indicators of probable sensitization to an allergen – usually IgE
• They often do not identify the offending food because the mere presence of antibody to the food does not predict the response when the food is consumed

21
TESTS FOR FOOD ALLERGY AND INTOLERANCE
• Skin tests: scratch; prick; intradermal Positive response indicated by wheal and
flare reaction in the skin Size usually measured 0 - 4+ Indicate release of inflammatory
mediators, especially histamine, from skin mast cellsSkin mast cells release inflammatory mediators in response to stimuli different from those that trigger mediator release from mast cells in other body tissues - especially the digestive tract

22
Value of Skin Tests in Practice
• Positive predictive accuracy of skin tests rarely exceeds 50% (estimates 30% - 60%)– Many practitioners rate them lower
• Negative tests for some highly allergenic foods thought to have close to 100% predictive accuracy
• Such foods include: egg milk fish wheat tree nuts peanut

23
Value of Skin Tests in Practice
• Negative skin tests do not rule out the possibility of non-IgE-mediated hypersensitivity reactions
• Do not rule out food intolerances (non-immune-mediated reactions)– “Skin tests for food allergy are especially
unreliable because of the large number of false positive and false negative reactions”
_________David 1993

24
Reasons for False Positive Skin Tests
• Degranulation of skin mast cells by stimuli that do not degranulate mast cells in the digestive tract
• Differences in the form in which the food is applied to the skin compared to that which encounters immune cells in the digestive tract– antigens in fruits and vegetables change when
cooked– allergen may be derived from an unstable food
extract– digestive processes can unmask antigens

25
False Negative Skin Tests
• Children younger than 2-3 years are more likely to have a negative skin test and positive food challenge than adults
• Adverse reaction is not mediated by IgE
• Commercial allergen may contain no material that the immune system can recognize

26
Blood Tests for Food Allergy
– RAST, FAST, ELISA and others Test for the presence of anti-food antibodies Detect anti-food IgE
– The mere presence of the antibody does not indicate clinical significance
– Positive tests often do not correlate well with observed reactions when the food is eaten

27
Value of Allergy Tests in Practice
• A key message is that a positive allergy test result (skin or blood) indicates only the presence of allergen specific IgE (called sensitization)
• It does not necessarily mean clinical allergy (ie, allergic symptoms with exposure).
• It is important for this reason that the allergy evaluation be based on the patient's history and directed by a health care professional with understanding of allergy
____________Cox et al 2008

28
Use of the Information
Use the information obtained from evaluation of the patient to determine:
• which allergy diagnostic tests to order
• how to interpret the allergy diagnostic test results
• how to use the information obtained from the allergy evaluation to develop an appropriate therapeutic treatment plan.

29
Which Tests Should I Order?
• Allergen-specific IgE tests are carried out by a variety of approved methods in Canada
• Provincial medical plans usually pay for 5 tests per person per year
• Order “food mixes” for the initial five tests• If any are positive the lab will test individual
foods within the groups at no additional charge• Do not advise patient to avoid all the foods in the
positive mix without further investigation

30
Examples of Blood Tests for allergen-specific IgE
• Phadia UniCAP System
• This assay system can measure levels of allergen-specific IgE as low as 0.1 kU/L
• The clinical relevance of results in the range of 0.1-0.35 kU/L warrants study.

31
Which Tests Should I Order?
• Examples of food mixes:– Legume mix (peanuts, soy, beans, lentils)– Vegetable mix– Fruits mix– Grains (includes wheat)– Nut and seed mix– Animal origin foods (milk, egg, meats)– Fish mix– Mollusks and shellfish

32
Example: Grains
Code Name Latin name
f6 Barley Hordeum vulgare
f310 Blue vetch Fabaceae (Leguminosae)
f11 Buckwheat Fagopyrum esculentum
f55 Common millet Panicum miliaceum
f56 Foxtail millet Setaria italica
f79 Gluten Common
f57 Japanese millet Echinochloa crus-galli
f8 Maize/Corn Zea mays
f90 Malt Hordeum vulgare
f7 Oat Avena sativa
f9 Rice Oryza sativa
f5 Rye Secale cereale
f124 Spelt wheat Triticum spelta
f4 Wheat Triticum aestivum

33
Legumes
Code Name Latin name
f296 Carob bean gum Ceratonia siliqua
f309 Chick pea Cicer arietinus
f305 Fenugreek Trigonella foenum-graecum
f315 Green bean Phaseolus vulgaris
f246 Guar, Guar gum Cyamopsis tetragonolobus
f297 Gum arabic Acacia spp.
f235 Lentil Lens esculenta
f182 Lima bean Phaseolus lunatus
f12 Pea Pisum sativum
f13 Peanut Arachis hypogaea
f287 Red kidney bean Phaseolus vulgaris
f14 Soybean Glycine max (Soja hispida)
f298 Tragacanth gum Astragalus gummifer
f15 White bean Phaseolus vulgaris

34
Mollusks
Code Name Latin name
f346 Abalone Haliotis spp.
f37 Blue mussel Mytilus edulis
f207 Clam Clam
f59 Octopus Octopus vulgaris
f290 Oyster Ostrea edulis
f58 Pacific Flying Squid Todarodes pacificus
f338 Scallop Pecten spp.
f314 Snail Helix aspersa
f258 Squid Loligo edulis, Loligo vulgaris

35
Milk & constituents
Code Name Latin name
f78 Casein Bos spp.
f81 Cheese, Cheddar type
f82 Cheese, mold type
f2 Cow's milk Bos spp.
f231 Cow's milk, boiled Bos spp.
f236 Cow's whey Bos spp.
f300 Goat's milk
f286 Mare's milk Equus spp.
f325 Sheep's milk Ovis spp.
f326 Sheep's whey Ovis spp.

36
Testing for IgG4 against foods
• Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI Task Force Report.
• Serological tests for immunoglobulin G4 (IgG4) against foods are persistently promoted for the diagnosis of food-induced hypersensitivity
• Many patients believe that their symptoms are related to food ingestion
• Tests for food-specific IgG4 represent a growing market• Testing for blood IgG4 against different foods is
performed with large-scale screening for hundreds of food items by enzyme-linked immunosorbent assay-type and radioallergosorbent-type assays in young children, adolescents and adults.
______________Stapel et al 2008

37
Value of IgG4 Tests in Practice
• Many serum samples show positive IgG4 results without corresponding clinical symptoms.
• IgG4 against foods indicates that the person has been repeatedly exposed to food components, which are recognized as foreign proteins by the immune system
• Its presence should not be considered as a factor which induces hypersensitivity, but rather as an indicator for immunological tolerance, linked to the activity of regulatory T cells.
______________Stapel et al 2008
_______________Tomicic et al 2009

38
Use of IgG4 Test Results
• Food-specific IgG4 does not indicate food allergy or intolerance, but rather a physiological response of the immune system after exposure to food components.
• Testing of IgG4 to foods is considered as irrelevant for the laboratory work-up of food allergy or intolerance and should not be performed in case of food-related complaints.
______________Stapel et al 2008

39
Unorthodox Tests
• Many people turn to unorthodox tests when avoidance of foods positive by conventional test methods have been unsuccessful in managing their symptoms
• Tests include:– Vega test (electro-acupuncture)– Biokinesiology (muscle strength)– Analysis of hair, urine, saliva– Radionics– ALCAT (lymphocyte cytotoxicity)

40
Disadvantages of Unreliable Tests
• Diagnostic inaccuracy
• Therapeutic failure
• False diagnosis of allergy
• Creation of fictitious disease entities
• Failure to recognize and treat genuine disease
• Inappropriate diets
• Malnutrition

41
Consequences of Mismanagement of Adverse Reactions to Foods
• Malnutrition; weight loss, due to extensive elimination diets
• Food phobia due to fear that “the wrong food” will cause permanent damage, and in extreme cases, death
• Frustration and anger with the “medical system” that is perceived as failing them
• Disruption of lifestyle, social and family relationships

42
The Bottom Line
• Elimination and Challenge is the only accurate method of identifying the specific foods responsible for a person’s adverse reactions
• Suspect foods are eliminated from the diet for a specific period of time
• Challenge is conducted by reintroducing each eliminated food individually and monitoring the person’s response

Identifying the Culprits
Elimination and Challenge

44
Elimination and Challenge
• Removal of the suspect foods from the diet, followed by reintroduction is the only way to:– identify the culprit food components– confirm the accuracy of any allergy tests
• Long-term adherence to a restricted diet should not be advocated without clear identification of the culprit food components

45
Elimination and Challenge
Stage 1: Exposure Diary– Record each day, for a minimum of 5-7
days:
all foods, beverages, medications, and supplements ingested
composition of compound dishes and drinks, including additives in manufactured foods
approximate quantities of each the time of consumption

46
Exposure Diary(continued)
– all symptoms experienced graded on severity:
1 (mild); 2 (mild-moderate) 3 (moderate) 4 (severe)
– time of onset
– how long they last
• Record status on waking in the morning.• Was sleep disturbed during the night, and if
so, was it due to specific symptoms?

47
Exercise 2: Food RecordSymptoms Record

48
Food Intolerance: Clinical Diagnosis
Symptoms Disappear
Elimination Diet: Avoid Suspect Food
Symptoms Persist
Increase Restrictions
Reintroduce Foods Sequentially or Double-blind
Symptoms Provoked No Symptoms
Diagnosis Confirmed Diagnosis Not Confirmed

49
Elimination DietBased on:
– detailed medical history– analysis of Exposure Diary– any previous allergy tests– foods suspected by the patient
• Formulate diet to exclude all suspect allergens and intolerance triggers
• Provide excluded nutrients from alternative sources
• Duration: Usually four weeks

50
Therapeutic Diets
• Certain conditions tend to be associated with specific food components
• Suspect food components are those that are probable triggers or mediators of symptoms
• Examples:– Eczema: highly allergenic foods– Migraine: biogenic amines– Urticaria/angioedema: histamine– Chronic diarrhea: disaccharides– Asthma: cyclo-oxygenase inhibitors; sulphites

51
Conditions that suggest Specific Food Involvement: Infant eczema
– Egg– Milk proteins– Peanut– Soy– Shellfish– Less frequently:
• Tomato• Green pea

52
Conditions that suggest Specific Food Involvement: Adult eczema
• May start as contact allergy (atopic dermatitis)– Could be indicator of latex allergy
• May be symptom of IgE-mediated allergy to any food: – Most common foods as in infant eczema– Less common: tomato; onion
• May be exacerbated by foods high in histamine– Include histamine-restricted diet during elimination
phase*
______________
*Worm et al 2009

53
Conditions that suggest Specific Food Involvement:
Oral Allergy Syndrome (OAS):Foods with allergens similar to birch pollen
Fruit
Apple
Apricot
Cherry
Kiwi fruit
Melon
Nectarine
Orange
Peach
Watermelon
Vegetables
Carrot
Celery
Fennel
Potato
Tomato
Legumes and Grains
Peanuts
Nuts and Seeds
Hazelnuts
“Tree nuts” (species unspecified)
Others
Spices (unspecified)

54
Latex-Food Syndrome:Foods with allergenic structures similar to latex
Fruit and VegetablesAvocado
Banana
Celery
Citrus fruits
Eggplant
Fig
Grapes
Kiwi fruit
Mango
Melon
Papaya
Passion fruit
Peach
Potato
Pineapple
Tomato
Legumes and Grains
Peanut
Soy
Wheat
Nuts and Seeds
Chestnut
Pistachio
Walnut

Category Food
Type IIIClinical findingsIdentification of cross-reactive allergens
Avocado ChestnutBanana PistachioBell pepper WalnutCassavaCeleryCherimoyaChestnutCustard appleKiwi fruitMangoPapayaPassion fruitPotatoTomato
Type IIClinical findings Characterization of cross-reactive components by extract inhibition assays
Fig TurnipMelon Zucchini PeachPineapple
Type IClinical findings only
AppleApricotAubergine (eggplant)CarrotCherryCoconutLoquatSpinachStrawberryWatermelon
Foods with Allergens Similar to Latex: PEN Pathway

56
Conditions that suggest Specific Food Involvement:Irritable Bowel Syndrome (IBS):Foods most frequently associated with symptoms
• Food allergens (individual reactivity)• Intolerance triggers
– Disaccharides (e.g. lactose; sucrose)– Monosaccharides (fructose)
• Free starches:– White flour; white rice– Root vegetables (potato; carrot)– Starchy fruits (banana)
• Raw fruits and vegetables• Processed (fermented) meats and sausages• High level of insoluble fibre (dried peas, beans; bran
from grains; whole nuts and seeds)• “Irritant” spices

57
Conditions that suggest Specific Food Involvement:Eosinophilic gastroenteritis:Abnormal number of eosinophils in the stomach and small intestine
Foods most frequently implicated
• Egg• Cow’s milk• Soy• Wheat
• Peanuts• Tree nuts• Shellfish• Fish

Conditions that suggest Specific Food Involvement:Eosinophilic esophagitis:Abnormal number of eosinophils in the esophagus
Foods most frequently implicated
• Egg • Cow’s milk• Soy• Wheat• Corn• Peanuts
• Tree nuts• Shellfish• Fish• Beef• Rye

Conditions that suggest Specific Food Involvement:Eosinophilic proctocolitis:Abnormal number of Eosinophils confined to the colon
Foods most frequently implicated
• Cow’s milk
• Soy proteins
Most frequently develops within the first 60 days of life
Is a non-IgE-mediated condition

60
Conditions that suggest Specific Food Involvement:Celiac disease (gluten-sensitive enteropathy)Offending Foods and their derivatives
• Wheat
• Rye
• Barley
• And in some cases Oats

61
Conditions that suggest Specific Food Involvement:Histamine intolerance:Histamine-containing and Histamine-releasing foodsAnimal
Proteins
Eggs
Shellfish
Fish (unless freshly caught)
Processed and fermented meats and sausages
Left-over meats
Milk Products
Fermented milk products:
Cheese of all types
Yogurt
Buttermilk
Kefir
Fruit
Citrus fruits
Berries
Raisins
Cherries
Apricots
Pineapple
Prunes
Dates
Currants
Grapes
Vegetable
Tomato
Spinach
Eggplant
Pumpkin
Soy
Red beans
Olives
Avocado
Additives
Tartrazine
Benzoates
Sulphites
Other
Cinnamon
Cloves
Anise
Nutmeg
Vinegar
Tea
Chocolate
Colas
Alcoholic and dealcoholise
beverages

62
Basic Hypoallergenic Elimination Diet
• Only listed foods are allowed• No vitamin supplements or non-essential medications
• GRAINS: Rice
Tapioca
• FRUITS: Pears; pear juice
Cranberries; cranberry juice
• VEGETABLES: Squash (all varieties)
Carrots
Parsnips
Lettuce
• MEAT: Lamb
Wild game
Turkey

63
Basic Hypoallergenic Elimination Diet
• MEAT Lentils
SUBSTITUTES: Split pea
Garbanzo beans
(chick peas)
• FLAVOURINGS: Sea salt• BEVERAGES: Distilled water in glass containers• OILS Canola oil
Olive oil
Safflower oil• OTHER Agar-agar
(Make jelly dessert s)

64
Exercise 3: Determining the Appropriate Elimination Diet

65
Duration of the Elimination Diet
• The “Basic Hypoallergenic (few foods) Diet” is nutritionally inadequate and should not be followed for longer than 10 to 14 days
• A selective elimination diet with nutritionally equivalent substitutes is followed for four weeks– Four weeks seems to be optimum for remission of
symptoms and for elicitation of symptoms on challenge

66
Expected Results of Elimination Diet
• Symptoms often worsen on days 2-4 of elimination
• By day 5-7 symptomatic improvement is experienced
• Symptoms disappear after 10-14 days of exclusion

67
Challenge• Use incremental dose challenge (SIDC) to each
eliminated food in its purest form to determine:– immediate reaction– delayed reaction– degree of tolerance (dosage)
• Do not test any food suspected to have caused a severe or an anaphylactic reaction except under medical supervision in a facility equipped for resuscitation

68
Food Challenge Record: Seattle Lab MetabisulfiteTable 1 Schedule
Dose Number
Amount (mg)
Dose Number
Amount (mg)
1 0.1 8 Placebo
2 0.5 9 50
3 1.0 10 75
4 5.0 11 100
5 10.0 12 150
6 15.0 13 200
7 25

69
Spirometric measurements for pulmonary function performed during and after all challenges were normal: No breathing impairmentConclusions: Reaction to bisulfite is ruled out
Table 2 ResultsChallenge dose in gelatin capsule administered every 10 minutes
Time Blood Pressure Dose (mg) Effects Reported
9.00 100/58 0.1 Patient feels good
9.10 110/73 0.5 No reaction
9.25 112/71 1.0 No reaction
9.35 118/81 5.0 Itching eyesPlugged ears
9.45 103/81 10 Plugged ears
9.55 118/83 15 No reaction
10.05 103/69 25 Chest tightness
10.20 108/76 Placebo Tingling around mouth
10.30 110/80 50 Patient feels goodNo reactions
10.45 107/72 75 Patient feels goodNo reactions
10.55 107/72 100 No reactions
11.10 114/75 150 Numbness of upper lip and tongue
11.25 114/75 200 Patient feels goodNo significant numbness of upper lip

70
Challenge
• The basic elimination diet, or therapeutic diet, continues during this phase
• For adults: – Do not add any test foods to the diet until all eliminated
foods have been tested separately, even if they produce no reaction during the challenge
• Children: – Add foods causing no adverse reaction when all tests
in a single food category have been tested (e.g. add milk when all tests in the “milk category” have been completed)

71
Incremental Dose Challenge
Day 1:• Morning: Eat a small quantity of the test food
Wait four hours, monitoring for adverse reaction; if no symptoms:
• Afternoon: Eat double the quantity of test food eaten in the morning.
• Wait four hours, monitoring for any adverse reactions; if no symptoms:
• Evening: Eat double the quantity of test food eaten in the afternoon

72
Incremental Dose Challenge Day 2:• Do not eat any of the test food
– Continue to eat elimination diet
• Monitor for any adverse reactions during the night and day. This may be due to a delayed reaction to the test food
• If an adverse reaction to the test food occurs at any time during the test: STOP. – Do not continue to eat the test food
• Wait 48 hours after all symptoms have subsided before testing another food

73
Incremental Dose Challenge
Day 3:• If no adverse reactions have been experienced
proceed to a new food• If the results of Day 1 and/or Day 2 are
unclear :– Repeat Day 1, using the same food, the same
test protocol, but larger doses of the test food
• Day 4:– Monitor for delayed reactions as on Day 2

74
Challenge Test
• Continue testing in the same manner until all excluded foods, beverages, and additives have been tested
• The first day is the test day and the second is a monitoring day for delayed reactions

Maintenance Diets
The Essentials in Providing Complete Balanced Nutrition

DIET FOR OPTIMUM NUTRITION Provide a nutritionally balanced diet that
supplies all essential macronutrients (protein, fat, carbohydrate) and micronutrients (vitamins and minerals) every day
Diets restricted because of food sensitivities:• Each meal and snack should contain three components:
1. Protein (PRO) 2. Grain (GR) or Starch (ST) 3. Fruit and/or Vegetable (FR/VEG)
76

Examples of Foods in Each Major Food Category:
Protein• Meat of all types• Poultry• Fish• Shellfish• Eggs• Nuts• Seeds• Tofu• Milk
– Milk products such as:– Cheese of all types– Yogurt– Buttermilk
77

Examples of Foods in Each Major Food Category:
Grains• Wheat • Rye• Oats• Barley• Rice• Corn• Amaranth• Quinoa• Buckwheat• Millet• Varieties and derivatives of wheat, such as:
– Spelt– Kamut– Bulgur– Triticale – Semolina
78

Examples of Foods in Each Major Food Category:
Starches• Flours and starches derived from “Grains”• Starchy vegetables and fruits, such as:• Potato• Sweet potato• Yam• High-starch root vegetables• Lentils• Dried beans• Dried peas• Garbanzo bean (chick pea)• Lima beans• Broad beans (fava)• Cassava• Plantain• Banana 79

Examples of Foods in Each Major Food Category:
FruitBerries:
Strawberry
Raspberry
Blueberry
Cranberry
Blackberry
Others
Stone fruits:PeachesApricotNectarinesCherriesPlumsOthers
Melons:CantaloupeHoneydewWatermelonOthers
Apple
Pear
Rhubarb
Grape
Citrus Fruits:Orange
Grapefruit
Lemon
Lime
Tropical fruits:Pineapple
Mango
Papaya
Passion fruit
Lychee
Longon
Star fruit
Dragon fruit80

Examples of Foods in Each Major Food Category:
VegetablesGreen leafy vegetables, e.g.:
Lettuce
Chard
Spinach
Broccoli
Beans:Green
String
French
Runner
Yellow wax
PeasGreen peas
Sugar peas
Green, red, yellow peppers
Squashes of all types
Onions
Garlic
Tomatoes
Carrots
Beets
Radishes
Cauliflower
Asparagus
Eggplant81

MILK
EGG
PEANUT
SOY
FISH
WHEAT
RICE
CORN
A + + +
Biotin + + +
Folacin (Folate; Folic acid) + + + +
B1 (Thiamin) + + + +
B2 (Riboflavin) + + + + + +
B3 (Niacin) + + + + +
B5 (Pantothenic acid) + + +
B6 (Pyridoxine) + + + +
B12 (Cobalamine) + + +
C
D + + +
E (alpha-tocopherol) + + + +
K + + +
IMPORTANT NUTRIENTS IN COMMON ALLERGENS
Vitamins
82

MILK
EGG
PEANUT
SOY
FISH
WHEAT
RICE
CORN
Calcium + + +
Phosphorus + + + + +
Iron + + + + + +
Zinc + + +
Magnesium + + +
Selenium + + +
Potassium + + +
Molybdenum +
Chromium + + +
Copper +
Manganese +
IMPORTANT NUTRIENTS IN COMMON ALLERGENSMinerals
83

84
Invitation to Further Information
www.allergynutrition.com
Joneja, J.M.Vickerstaff
Dealing with Food Allergies
Bull Publishing Company, Boulder, Colorado. 2004