Diet, Nutrition and Inflammatory Bowel Disease Jason K. Hou, MD Baylor College of Medicine Houston,...
-
Upload
amy-sewell -
Category
Documents
-
view
225 -
download
0
Transcript of Diet, Nutrition and Inflammatory Bowel Disease Jason K. Hou, MD Baylor College of Medicine Houston,...
Diet, Nutrition Diet, Nutrition and and
Inflammatory Inflammatory Bowel DiseaseBowel Disease
Jason K. Hou, MDJason K. Hou, MD
Baylor College of MedicineBaylor College of Medicine
Houston, TXHouston, TX
ObjectivesObjectives
At the conclusion of the conference, At the conclusion of the conference, participant should be able to:participant should be able to: 1) Describe the possible role of diet in 1) Describe the possible role of diet in
the development of IBDthe development of IBD 2) Identify the importance of nutritional 2) Identify the importance of nutritional
deficiencies in IBDdeficiencies in IBD 3) Describe the potential use of diet as 3) Describe the potential use of diet as
therapy for IBDtherapy for IBD
So doc, what can I eat?So doc, what can I eat?
““Intellectual divide”Intellectual divide” Physicians focus on nutritional Physicians focus on nutritional
deficienciesdeficiencies Patients interested in diet as cause or Patients interested in diet as cause or
cure of symptomscure of symptoms
Malnutrition- then and Malnutrition- then and nownow
20-85% of IBD patients with 20-85% of IBD patients with protein-energy malnutritionprotein-energy malnutrition
Hospital based studies (1970s)Hospital based studies (1970s)
Most prevalent nutritional Most prevalent nutritional abnormality abnormality
= excess body weight (2007)= excess body weight (2007)
Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6
Got milk?Got milk?
Food avoidanceFood avoidance 65% of IBD patients report food 65% of IBD patients report food
avoidanceavoidance 28% of IBD patients on dairy-free diet28% of IBD patients on dairy-free diet
Lactose intolerance no more common or Lactose intolerance no more common or even less common in UC than non-IBD even less common in UC than non-IBD controls. controls.
Gerasimidis et al. Aliment Pharmacol Ther. 2008 Jan 15;27(2):155-65 Bernstein et al. Am J Gastroenterol. 1994 Jun;89(6):872-7
Incidence of IBD is Incidence of IBD is increasingincreasing
Hou et al. Am J Gastroenterol. 2009 Aug;104(8):2100-9
Dietary fatsDietary fats
Omega 3-fatty acids Omega 3-fatty acids Docosahexonenoic acid (DHA)Docosahexonenoic acid (DHA) Eicosapentaenoic acid (EPA)Eicosapentaenoic acid (EPA) Docosepentaenoic acid (DPA)Docosepentaenoic acid (DPA)
Omega 6-fatty acidsOmega 6-fatty acids Linoleic acidLinoleic acid
Dietary fatsDietary fats
Food frequency questionnaire in newly Food frequency questionnaire in newly diagnosed pediatric CD patients (130 diagnosed pediatric CD patients (130 patients)patients)
Dose dependent protective effect of Dose dependent protective effect of omega-3 FA (EPA, DPA, DHA) for CDomega-3 FA (EPA, DPA, DHA) for CD
OR 0.44 (95% CI 0.19-1.00)OR 0.44 (95% CI 0.19-1.00)
Ratio of omega-3 PUFA/ omega-6 PUFARatio of omega-3 PUFA/ omega-6 PUFA OR 0.32 (95% CI 0.14-0.71)OR 0.32 (95% CI 0.14-0.71)
Amre et al. Am J Gastroenterol. 2007 Sep;102(9):2016-25
Dietary fatsDietary fats
Vegetable, fruit, nut, fish, dietary fiber Vegetable, fruit, nut, fish, dietary fiber intake protective in dose dependent intake protective in dose dependent mannermanner
““Western diet” Western diet” meat, fried food, fast food, snacks, dessertmeat, fried food, fast food, snacks, dessert positive associated in development of CD in positive associated in development of CD in
girls [OR 4.7 (95% CI 1.6-14.2)]girls [OR 4.7 (95% CI 1.6-14.2)]
D'Souza et al. Inflamm Bowel Dis. 2008 Mar;14(3):367-73D'Souza et al. Inflamm Bowel Dis. 2008 Mar;14(3):367-73
EPICEPIC
Prospective cohort study 203,193 personsProspective cohort study 203,193 persons Case control of 126 incident cases of UCCase control of 126 incident cases of UC
Linoleic acid positively associated with Linoleic acid positively associated with development of UC in a dose dependent manner development of UC in a dose dependent manner
OR 2.49 (95% CI 1.23-5.07 in highest quartile)OR 2.49 (95% CI 1.23-5.07 in highest quartile)
Dose dependent protective effect of DHA for UCDose dependent protective effect of DHA for UC OR 0.23 (95% CI 0.06-0.97)OR 0.23 (95% CI 0.06-0.97)
Hart et al. Gut. 2009 Jul 23
EPIC-UKEPIC-UK
UK subset of EPICUK subset of EPIC 25, 639 persons25, 639 persons Ages 40-74Ages 40-74 22 incident UC (median f/u 3.9 years)22 incident UC (median f/u 3.9 years) The highest tertile of dietary oleic acid The highest tertile of dietary oleic acid
protective for UC (OR 0.11 (95% protective for UC (OR 0.11 (95% CI=0.01-0.87)CI=0.01-0.87)
De Silva et al. Abstract DDW 2010
CarbohydratesCarbohydrates
FODMAPsFODMAPs FFermentable ermentable OOligo-ligo- DDi-i- MMono-saccharides ono-saccharides AAndnd PPolyolsolyols
FODMAPsFODMAPs
May increase bacterial overgrowth May increase bacterial overgrowth in distal small bowelin distal small bowel
Increase intestinal permeabilityIncrease intestinal permeability Trigger CD in susceptible hostTrigger CD in susceptible host
No dataNo data
Gibson et al. Aliment Pharmacol Ther. 2005 Jun 15;21(12):1399-409
Nutritional deficienciesNutritional deficiencies
CDCD 32% overweight32% overweight 8% obese8% obese 2.6% underweight2.6% underweight
5.3 % considered malnourished 5.3 % considered malnourished by SGAby SGA
Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6
Nutritional deficienciesNutritional deficiencies
Food avoidance 29% excluded grains 28% excluded milk 18% excluded vegetables 11% excluded fruits
Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6
Nutritional deficienciesNutritional deficiencies
Percentage of patients who Percentage of patients who reached daily recommended intakereached daily recommended intake
CD patients Controls
Fiber 15 38Calcium 25 61Selenium 6 80Vitamin A 21 40Vitamin C 47 73Vitamin D 10 26Vitamin E 5 24Vitamin K 0 0
Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6Sousa Guerreiro et al. Am J Gastroenterol. 2007 Nov;102(11):2551-6
Calcium and Vitamin DCalcium and Vitamin D
21-40% increased risk of fractures21-40% increased risk of fractures Increased risk even after adjusting for Increased risk even after adjusting for
steroid usesteroid use
ManagementManagement BisphosphonateBisphosphonate
Bernstein et al. Gastroenterology. 2003 Mar;124(3):795-841 Siffledeen et al. Clin Gastroenterol Hepatol. 2005 Feb;3(2):122-32 von Tirpitz et al. Eur J Gastroenterol Hepatol. 2000 Jan;12(1):19-24
AGA guidelines (2003)AGA guidelines (2003)
Who to ScreenWho to Screen > 3 months > 3 months
steroidssteroids Low trauma Low trauma
fracturefracture Postmenopausal Postmenopausal
femalefemale Male > 50 Male > 50 HypogonadismHypogonadism
ManagementManagement DEXADEXA T score < -2.5 OR T score < -2.5 OR
history of history of compression fracturecompression fracture
BisphosphonateBisphosphonate -2.5 <T score < -1-2.5 <T score < -1
Bisphosphonate if Bisphosphonate if need to continue need to continue steroidssteroids
Bernstein et al. Gastroenterology. 2003 Mar;124(3):795-841
Folate/B12Folate/B12
Decreased intestinal transport- Decreased intestinal transport- sulfasalazinesulfasalazine
Deficiency may result in Deficiency may result in hyperhomocystinemiahyperhomocystinemia
Hypercoagulable stateHypercoagulable state
Folate supplementation- possible Folate supplementation- possible protective against colorectal protective against colorectal cancer/dysplasiacancer/dysplasia
Lashner et al. Gastroenterology. 1989 Aug;97(2):255-9
Lashner et al. Gastroenterology. 1997 Jan;112(1):29-32
MicronutrientsMicronutrients
ZincZinc wound healingwound healing
SeleniumSelenium possible anti-inflammatory and anti-possible anti-inflammatory and anti-
neoplastic propertiesneoplastic properties
Antioxident vitaminsAntioxident vitamins
Possible pathwaysPossible pathways
Remove toxin/antigenic stimulus Remove toxin/antigenic stimulus (elemental diet)(elemental diet)
Alter bacteria flora (prebiotic)Alter bacteria flora (prebiotic)
Alter intestinal fluid transport/gas Alter intestinal fluid transport/gas productionproduction
Enteral therapyEnteral therapy
Elemental and non-elemental dietElemental and non-elemental diet No differences in efficacyNo differences in efficacy
LimitationsLimitations PalatabilityPalatability
May require nasogastric feedingMay require nasogastric feeding
Enteral Therapy- Cochrane Enteral Therapy- Cochrane review (2007)review (2007)
Induction of remission: 20-84%Induction of remission: 20-84% Beneficial but inferior to Beneficial but inferior to
corticosteroidscorticosteroids Open label RCTOpen label RCT
37 pediatric new diagnosed CD37 pediatric new diagnosed CD Remission (10 wk)Remission (10 wk)
ET: 79%; 95% confidence interval (CI), 56%-92%ET: 79%; 95% confidence interval (CI), 56%-92% Steroid 67%; 95% CI, 44%-84% P = .4Steroid 67%; 95% CI, 44%-84% P = .4
Endoscopic healing seen only in ET groupEndoscopic healing seen only in ET group
Zachos et al. Cochrane Database Syst Rev. 2007 Jan 24;(1):CD000542Borrelli et al. Clin Gastroenterol Hepatol. 2006 Jun;4(6):744-53
Nutritional supplementsNutritional supplements
Omega-3- PUFA (Fish oil) and CDOmega-3- PUFA (Fish oil) and CD EPIC-1 (quiescent disease)EPIC-1 (quiescent disease) EPIC-2 (flare, remission induction by EPIC-2 (flare, remission induction by
steroids)steroids) 4 grams daily4 grams daily Control- MCTControl- MCT
Feagan et al. JAMA. 2008 Apr 9;299(14):1690-7
Nutritional supplementsNutritional supplements
Omega-3- PUFA Omega-3- PUFA EPIC-1 EPIC-1
At 1 year 31.6 % vs. 35.7% relapseAt 1 year 31.6 % vs. 35.7% relapse HR 0.82, 95% CI 0.57- 1.19HR 0.82, 95% CI 0.57- 1.19
EPIC-2EPIC-2 At 1 year 47.8% vs. 48.8% relapseAt 1 year 47.8% vs. 48.8% relapse HR 0.90, 95% CI 0.67- 1.21HR 0.90, 95% CI 0.67- 1.21
Feagan et al. JAMA. 2008 Apr 9;299(14):1690-7
Nutritional supplementsNutritional supplements
Omega-3- PUFAOmega-3- PUFA Cochrane review (2009)Cochrane review (2009)
Small pooled benefitSmall pooled benefit RR 0.77, 95% CI 0.61-0.98RR 0.77, 95% CI 0.61-0.98
Authors conclude likely no benefit based on Authors conclude likely no benefit based on EPICEPIC
Turner et al. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD006320
Nutritional supplementsNutritional supplements
Fiber and UCFiber and UC Converted to short chain fatty acids Converted to short chain fatty acids
(SCFA)(SCFA) Energy source for colonocytesEnergy source for colonocytes Modulate local immune responseModulate local immune response
(attenuate IL-6, IL-8, TNF-(attenuate IL-6, IL-8, TNF-αα, , leukocyte adhesionleukocyte adhesion)) Modify microbiota (prebiotic)Modify microbiota (prebiotic)
Menzel et al. Inflamm Bowel Dis. 2004 Mar;10(2):122-8Galvez et al. Mol Nutr Food Res. 2005 Jun;49(6):601-8
Nutritional supplementsNutritional supplements
Butyrate (SCFA)Butyrate (SCFA) Increase in dietary fiber can increase Increase in dietary fiber can increase
fecal butyratefecal butyrate Germinated barley foodstuff (GBF)Germinated barley foodstuff (GBF)
Alter colonic bacterial concentrationsAlter colonic bacterial concentrations Increase in Increase in BifidobacteriumBifidobacterium sp. and sp. and
Eubacterium limosumEubacterium limosum
Hallert et al. Inflamm Bowel Dis. 2003 Mar;9(2):116-21Kanauchi et al. J Gastroenterol. 2002 Nov;37 Suppl 14:67-72
Nutritional supplementsNutritional supplements Butyrate (SCFA)Butyrate (SCFA)
Butyrate enemasButyrate enemas Benefit in UC (pilot study)Benefit in UC (pilot study) Did not reach statistical significance in RCTDid not reach statistical significance in RCT
Plantago ovata seedsPlantago ovata seeds Open label randomized trial (105 pts)Open label randomized trial (105 pts)
Mesalamine 500 TID vs. fiber 10 gm BIDMesalamine 500 TID vs. fiber 10 gm BID Increased fecal butyrate in fiber groupIncreased fecal butyrate in fiber group No difference @ 1 yearNo difference @ 1 year
Relapse 40% in fiberRelapse 40% in fiber Relapse 35% in mesalamineRelapse 35% in mesalamine
Scheppach et al. Gastroenterology. 1992 Jul;103(1):51-6Fernández-Bañares et al. Fernández-Bañares et al. Am J Gastroenterol. 1999 Feb;94(2):427-33Am J Gastroenterol. 1999 Feb;94(2):427-33
Nutritional supplementsNutritional supplements
Defined diets- No dataDefined diets- No data
Specific Carbohydrate DietSpecific Carbohydrate Diet ““Breaking the Viscious Cycle”Breaking the Viscious Cycle”
Maker’s dietMaker’s diet
““juicing” dietsjuicing” diets
Nutritional supplements- Nutritional supplements- CAMCAM
Common name Clinical trials
Crohn's disease
Artemisia absinthium Wormwood RCT Boswellia Serrata Frankincense RCT
Tripterygium wilfordii Lei gong teng open, prospective Pistacia lentiscus Chios mastic open, prospective
Curcuma longa Linn Curcumin open, prospective
Ulcerative ColitisCurcuma longa Linn Curcumin RCT
Aloe barbadensis Miller Aloe vera RCTTriticum aestivum Wheat grass RCT
Oenothera biennis Evening primrose RCT Boswellia Serrata Frankincense open prospective
Hou et al. Therapy, Mar 2010, 7(2), 179-189
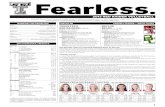
BCM Food aversion studyBCM Food aversion study
Hypothesis: Hypothesis: Food aversion in IBD is common.Food aversion in IBD is common. Food aversion in IBD may be related to Food aversion in IBD may be related to
several factorsseveral factors PhysicianPhysician Patient directed educationPatient directed education Patient symptom correlationPatient symptom correlation
BCM Food aversion studyBCM Food aversion study
Primary aim: To define the Primary aim: To define the frequency and character of dietary frequency and character of dietary alterations that occur in patients alterations that occur in patients with IBD with IBD
Secondary aims:Secondary aims: Identify the reason IBD patients initiate Identify the reason IBD patients initiate
dietary modificationsdietary modifications Identify if IBD patients feel dietary Identify if IBD patients feel dietary
modifications are effectivemodifications are effective
MethodsMethods Prospective, controlled data Prospective, controlled data
acquisition acquisition 100 IBD patients100 IBD patients
50 CD50 CD 50 UC50 UC
100 healthy controls100 healthy controls Non-IBSNon-IBS Matched for age, sexMatched for age, sex
BCM Food aversion studyBCM Food aversion study
GoalsGoals Establish food aversion patterns in IBDEstablish food aversion patterns in IBD Identify etiology of food aversion Identify etiology of food aversion
patterns in IBDpatterns in IBD Create pilot data for further studies Create pilot data for further studies
regarding dietary habits and IBDregarding dietary habits and IBD Establish if unnecessary food aversion Establish if unnecessary food aversion
result in nutritional deficiencyresult in nutritional deficiency Apply educational tools to correct Apply educational tools to correct
nutritional deficienciesnutritional deficiencies
ConclusionsConclusions
Diet as Etiology Diet as Etiology Fatty acids composition may play a role Fatty acids composition may play a role
in pathogenesisin pathogenesis Nutritional deficienciesNutritional deficiencies
Protein-calorie malnutrition becoming Protein-calorie malnutrition becoming less common, but Micronutrient less common, but Micronutrient deficiencies commondeficiencies common
Diet as TherapyDiet as Therapy Fiber, enteral therapy, CAMFiber, enteral therapy, CAM