Diasease of small intestine
Transcript of Diasease of small intestine
Contents • Anatomy• Physiology• Disorder:
– Crohn’s disease– Intestinal tuberculosis– intestinal ameobiosis– Campylobacter – Salmonellosis– Diverticula– mesenteric ischemia– Intestinal fistula– Celiac disease – Bacterial overgrowth– neoplasm
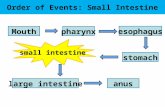
Anatomy
• Small intestines extends from pylorus to ileocaecal junction.
• Practical purposes- starting from duodenojejunal flexure till caecum.
• Small intestine consists of proximal 2/5 jejunum & distal 3/5 ileum.6m in length
• Jejunum reside in the left side of the peritoneal cavity & ileum on the right side.
Anatomy
A. Duodenum: Retro-peritoneal Supplied by the celiac artery & SMA
B. Jejunum: Occupies upper left of the abdomen Thicker wall and wider lumen than the
ileum Mesentery has less fat and forms only 1-2
arcadesC. Ileum:
Occupies the lower right; has more fat and forms more arcades
Contains Payer’s patches Ileum & jejunum is supplied by the SMA
Mesenteric border of the intestine gets more blood supply compared to anti-mesenteric border
• Venous drainage through sup. Mesenteric vein
Lymphatics:• Lymph drainage occur
through lymphatic vessel• Lymhmesenteric
LNcisterna chylithoracic ductLt subclavian vein
Nerve supply:• Parasympathetic- vagus• Sympathetic- splanchnic
Function • Digestion and absorption• Metabolism of plasma lipoproteins• Endocrine function• Immune function
CROHN’S DISEASE• Regional enteristis• Chronic full thickness
inflammatory process• More prevalent in
Ashkenazi Jewish• Female > male, 2x
higher smokers
• Breast feeding is protective
Aetiology • Incompletely understood
but involve interplay of genetic & environmental factor.
• Familial association (30x in siblings / 13 x in 1st degree relatives).( NOD2/CARD15 gene)
• smoking• Higher socioeconomic
status
pathogenesis
CD is associated with a defect in suppressor T cells, which act to prevent escalation of inflammatory process
Pathology• Terminal ileum mc involve.• Macroscopic: fibrotic thickening
of intestinal wall with a narrow lumen & fat wrapping, dilated bowel proximal to stricture & deep mucosal ulceration, cobblestne app., transmural inflammation, skip lesion.
• Microscopic: focal area of chronic inflm. Involving all layers with lymphoid aggregates & non caseating giant cell granuloma.
Clinical features • Intermittent colicky lower abd.
Pain, diarrhea, weight loss.
Extraintestinal manifestation• Related to disease activity:Erythema
nodosum, pyoderma gangrenosum,arthropathy, eye complication, apthous ulceration, amyloidosis.
• Unrelated to disease activity: Gall stone, renal calculi, primary sclerosing cholangitis, chronic active hepatitis, sacroilitis
complication• Colitis, rectal disease, obstruction,
hollow viscus fistulae, nutritional deficiencies.
Investigation:• CBC, endoscopic, imaging.
Treatment: • Steroid, Antibiotic, aminoglycoside,
Immunomodulatory agents, Monoclonal antibody, Nutritional support, surgery.
Prognosis:• No cure for the disease• 10-20% come with relapses & recurrent• But repeated treatment & surgical
procedures give good prognosis
Non-operative management of Crohn’s Disease:Endoscopic treatment balloon dilatation of fibrostenotic disease symptomatic improvement
Indication for surgery• Recurrent intestinal obstruction• Bleeding• Perforation• Failure of medical therapy• Intestinal fistula• Fulminant colitis• Malignant changes• Perianal disease
Great range of operation is performed depending on disease pattern• Ileocaecal resection• Segmental resection• Colectomy& ileorectal anastomosis• Subtotal colectomy & ileostomy• Temporary loop ileostomy• Proctocolectomy• strictureplasty
Intestinal Tuberculosis• It is secondary to pulmonary
tuberculosis.• Commonly involve in ileoceacal
region
• Types: – Ulcerative – Hyperplastic
• Clinical features:– Abdominal pain– Diarrhea– Abdominal distension– Nonspecific symptoms
• Signs– Malnourished & pale– Visible peristalsis– Distended bowel loop– Rolled up omentum– Mass in RIF/ lumbar region
• Management – No int. obstruction ATT– Obstruction:
• Solitary stricturoplasty• Multiple at long interval
stricturoplasty• Multiple at short segmentresection
– Surgical treatment of hyperplastic TB• Limited resection• ATT• Nutritional supplementation• Blood transfusion
Comparison of two form of intestinal tuberculosis
ulcerative hyperplastic
Aetiology
SiteVirulence of organismResistance of bodyPathology
Clinical features
Complications
Investigation Barium studies
CXR & sputum AFB
Scndry to pulm. TB
Terminal ileumMore virulentVery poorMultiple ulcerations in the terminal ileum with/ wo LN involvement. Ulcers are transverse. Serosa reddened & edematousSymps. Of TB, diarrhea, blood & mucus in stool
Acute: ulcer perforationChronic: healing ulcer result in stricture of terminal ileum SAIO
Demonstrate strictures
Positive
It may be primary intestinal TB, due to M. Bovis.Ileocaecal regionLess virulentGoodLow grade, chronic continuous inflammation involving IC region.
Abd. Pain & diarrhea (initially)Fever, weight loss & SAIO (later)
Nodular, mobile, firm mass in RIF which later produces SAIO
Demonstrate: contracted caecum, pulled up caecum, luminal obs., obtuse IC anglenegative
Intestinal ameobiasis• An infection with Entamoeba
histolytica.• Transmitted through
contaminated drinking water• Can cause colonic ulcer described
as ‘bottlenecked’• Ulcer have yellow necrotic floor,
from which blood & pus exude.• Can mimic UC • Pericolitis is common & may
result adhesion int. obst.• Ameobiasis may cause liver
absceses & amoeboma
• Clinical features:– Bloody diarrhea– Severe hemorrhage– Stricture– Perforation
• Inv: endoscopic biopsies or fresh hot stool
• Treatment: metronidazole 400-600mg TID x 10days
• Diloxanide furoate 500mg TID for 10days
• Surgery is frought with danger as the bowel is to friable.
campylobacter
• Infection with Campylobacter jejuni
• Mc form gastroenteritis in UK
CF– Dairrhea– Abd. Pain– Mimic acute abdomen
• May also resemble UC• INV: stool culture• Treatment: supportive,
usually resolve w/o antiboitic
Yersinia
• Yersinia enterocolitica• Infect terminal ileum, appendix,
a.colon, mesenteric LN• Can cause a granulomatous
inflammatory process (mimic CD)• CF:
– Fever– Gastroenteritis– Persistterminal ileitisperforate
• INV: stool culture, serological• Treatment: normally self limiting,
respond to cotrimoxazole/ chloramphenical
Salmonellosis, typhoidsalmonellosis• Salmonella are family of gram –ve rods• Salmonella GE typically caused by s.
enteritidis from poultry (self limiting)headache, fever & watery diarrhea.
• When severehospitalization+antibiotic+iv fluid
• Diagnosis: stool culturetyphoid• Typhoid feverS.typhi• CF:
– Fever– Abd.pain after IP(10-20 days)– Distension, diarrhea,
splenomegaly, ‘rose spots’ on abdomen.
• Complication– Paralytic ileus– Intestinal haemorrhage– Perforation– Cholecystitis
• Invasion of systemic circulationsevere gram-ve sepsis & septic shock
• Metastatic sepsis– Septic arthritis– Osteomyleitis– Encephalitis– DIC– pancreatitis
• Perforation of typhoid ulcer (3rd week)• Diagnosis: culture of blood or stool• Treatment: antibiotic-chloramphenicol• Perforation-surgery to wash out & closed
perforated ulcer
Diverticula • Hollow out-pouchings• Common structural
abnormality occur from esophagus-rectosigmoidal junction.
• classified:– Congenital-all 3 coats of
bowel are present in the wall (Meckel’s Diverticulum)
– Acquired-no muscularis layer present ( sigmoid diverticula)
Jejunal diverticula• Arises from the mesenteric side of
the bowel • Can vary in size & multiple• Clinical features:
– asymptomatic– Malabsorption – Acute abdominal emergency (perforate)
• Investigation: – Radiological imaging
• Treat: – elective resection of affected small
bowel– If perforate resection & anastomosis
& stoma formation.
Meckel’s diverticulum
• A persistent remnant of vitellointestinal duct
• Present in about 2% of population• Found on antimesenteric side of
ileum at 2feet from IC valve and 2inches long
• 20% cases heterotrophic epithelium
• It contains all 3 coats & have its own blood supply.
• Vulnerable to obstruction & inflammation.
• If MD in an inguinal / femoral hernia Littre’s hernia
• Can present clinically:– Hemorrhage– Diverticulitis– Intussusception– Chronic ulceration– Intestinal obstruction– Perforation
• Treat: Meckel’s diverticulectomy Should not amputated its base &
invaginate Should excise by resecting & suturing
at the base or liner stapler cutter If base is indurated limited small
bowel resection + anastomosis
Mesenteric ischemia• Mesenteric vascular disease classified
as acute intestinal ischemia:– With/w/o occlusion, – venous, chronic arterial, – central / peripheral
• Superior mesenteric vessel most likely to be affected by embolization/thrombosis.
• Occlusion of SMA thrombosis• Middle colic artery emboli lodge• Inferior mesenteric involvement
clinically silent• Sources of embolization of SMA:
– LA ass. With fibrillation, mural MI, artheromatous plaque from aortic aneurysm, mitral valve vegetation ass. With endocarditis
• Primary thrombosis: artherosclerosis, thromboangitis obliternas
• Primary thrombosis of SMV occur in association: factor v leiden, Portal HTN, portal pyaemia, sickle cell disease, women take OCP
• Occlusion hemorrhagic infarctionintestine & its mesentery become swollen & edematous blood stained fluid exudes peritoneal cavity & bowel lumen
• Main trunk SMA infarction covers area from duodonejejunal flexure to splenic flexure
• CF: sudden onset of acute abdominal pain ( atrial fibrillation/atherosclerosis), persistent vomiting & defecation (early), then passaged of altered blood hypovolemic shock
• O/E: mild abdominal tenderness , rigidity (late)
• Pain central & out of propotion of physical findings
• Inv: CBC- profound neutrophil leukocytosis
• Abdominal radiograph- absence of gas in the thickened small intestine, presence of gas bubble in mesenteric vein
• Treatment: early cases: resuscitate, embolectomy via the ileocolic artery/ revascularization of SMA
• Late cases: resected affected bowel, anticoagulation should be give early in post-op period
• Iv alimentation required extensive enterctomy
• Selected cases small bowel transplantation
Intestinal fistula
• Abnormal communication between 2 portion of intestine, between intestine & other hollow vicus/ skin of abd. Wall
• Involve skin & intestines enterocutaneous fistula
• Classification– Anatomical
• Internal: colovesical fistula• External: duodenal, jejunal
fistula• Mixed: crohn’s disease
– Depending on contents• Low output: <200ml• Moderate output 200-500ml• High output: >500ml
• Etiology:– Iatrogenic– Stump blow out– Inadequate resection of
diseased segment– Instrumentation– spontaneous
• Management:– Recognition and etiology– Phase of stabilisation– Nutrition– Investigative phase– Phase of definitive
management:• Surgery• Skin care • Abdominal wall defect
Celiac disease• Most common cause of
malabsorption in UK• Characterised by hypertrophic
small bowel mucosa + atrophic villi & deep cypts
• Caused by gluten • Genetic association with HLA
B8• Children: steartorrhea &
growth retardation• Adults: diarrhea, loss of
weight, anaemia
Diagnose: – endoscopy duodenal biopsy– Antiendomysial antibody tests
• Increased risk of SB lymphoma & adenocarcinima
• Extraintestinal mnfstn: dermatitis herpetiformis, neurological problem
Treatment: withdrawn gluten from diet• Surgery malignancy
Tumors
• Small bowel tumors are rare
• Benign – Peutz-jeghers
syndrome• Malignant
– Adenocarcinoma– Carcinoid tumor– Lymphoma– GIST
Benign • Majority of small bowel neoplasm are
benign• Adenomas, lipomas, hemangiomas,
neurogenic tumors • Frequently asymtomatic & identified
incidentally• Can present with intersusception,
small bowel obstruction, bleeding, anaemia
• Inv: capsule endoscopy & small bowel endoscopy
• Symptomatic lesion can be treated by small bowel resection & anastomosis.
Peutz-jeghers syndrome
• Autosomal dominant disease• Melanosis of the mouth & lips
& multiple hamartomatous tumour like malformation.
• Melanin spot also can occur on digits & perianal skin.
• Gene STK11 on chromosome 19
• Consequence of complication of bowel obstruction & development of wide range of cancers
• Malignant changes rarely occur
• Resection may be indicated:– Heavy & persistent
bleeding– Intususception– Heavy involve segments of
small intestine• May be remove by enterotomy
/ laparotomy snared via a colonoscope
Malignant
• Rare & classically present late
• Often diagnose after surgery for small bowel obstruction
• 4 types that account over 99% of small bowel malignancies.
Adenocarcinoma• More often found in jejunum than
ileum• Etiology unknown but mc in pt : CD,
coeliac disease, FAP & Peutz Jeghers syndrome
• CF: anaemia, overt GI bleeding, intususception, obstruction
• Prognosis: poor espcially pt with CD• Treatment: resection of 5cm of non
involved bowel either side of lesion & the affected mesentery
• Right hemicolectomy if tumors at distal ileum.
Carcinoid tumor
• Neuroendocrine tumor occur throughout GIT• Mc appendix, ileum, rectum• Arise from Kulchitsky cells at the base of intestinal
crypts• Primary: usually small, significant LN metastases
• May produce dense fibrosis in surrounding tissues distortion & scarring of bowel
• Can produce vasoactive peptides: serotonin, histamine, prostaglandin, kallikrein,
• Liver mets carcinoid syndrome become evidentCF:• reddish-blue cyanosis, flushing attacks, diarrhea,
borborygmi, asthmatic attack, pulmonary & tricuspid stenosis
Inv: • octreotide scanning extent of disease• Plasma markers tumor bulk (chromogranin A
concentration) disease recurrenceTreatment: primary surgical resection• Mets hepatic resection • Octreotide can be give to prevent carcinoid crisis• Tumors not sensitive to chemo /radiotherapy
Lymphoma
• Small bowel lymphoma may be primary, mc secondary to systemic lymphoma.
• Mc in pt CD & immunodeficiency syndromes
• Hodgkin’s lymphoma rare to affect small bowel
• Most western type of lymphoma non-hodgkin’s type B lymphoma
• CF: anemia, bleeding, perforation, anorexia, weight loss
• T-cell lymphoma pt with coeliac disease• CF: worsening diarrhea, PUO, local
obstructive symptoms• Mediterranean lymphoma north Africa,
middle east• Burkitt’s lymphoma aggressively affect
IC region ( children)• Treatment: chemotherapy• Surgery : obstruction, perforation ,
bleeding
GIST• Mesenchymal tumors• Distinction between benign &
malignant is difficult• Increase in size & high level of
c-kit (CD117) staining ass. With malignant potential
• Mc found in stomach, can also found in other parts of gut
• Mc 50-70 years• Unknown cause but pt with
neurofibromatosis may have risk to develop
• CF: asymptomtic, lethargy, pain, nausea, haematemesis, melaena
Treatment:• surgery removing GIST
(radioresistant)
• Glivec (imatinib) tyrosine kinase inhibitor, effective in advanced cases
Short bowel obstructuion
aetiologies• Intarluminal:foreign
bodies, gallstones, meconium
• Intramural: tumor, CD• Extrinsic: adhesion,
carcinomatosis, hernias
Clinical features• Colicky abd. Pain• Nausea• vomiting (proximal)• Obstipation• Continous passage of
flatus /stool beyond 6-12 hrs (partial)
• Abd distaention ( distal ileum)
• Bowel sound-hyperactive(initial)decrease
• Lab: mild leukocytosis• Hemoconcentration• Electrolytes abnornal• Strangulated:
– Abd pain disproportionate to degree of abd. Finding
– Tachycardia– Localised abd.tenderness– Fever– Leukocytosis– acidosis