DIABETES MELLITUS References: Harrison’s Principles of Internal Medicine 17 th edition .
-
Upload
edward-fitzgerald -
Category
Documents
-
view
224 -
download
1
Transcript of DIABETES MELLITUS References: Harrison’s Principles of Internal Medicine 17 th edition .
DIABETES MELLITUS
References:
Harrison’s Principles of Internal Medicine 17th edition
http://cadre-diabetes.org/r_treatment_guidelines.asp
http://care.diabetesjournals.org/cgi/reprint/31/Supplement_1/S12
http://www.aace.com/meetings/consensus/dcc/pdf/dccwhitepaper.pdf
Undiagnosed diabetes
5.9 million
Prevalence of Glycemic Abnormalities in the United States
Additional 24.6 million
with IGT
Diagnosed type 2 diabetes
10 million
Diagnosed type 1 diabetes
~1.0 million
Centers for Disease Control. Available at: http://www.cdc.gov/diabetes/pubs/estimates.htm; Harris MI. In: National Diabetes Data Group. Diabetes in America. 2nd ed. Bethesda, Md: NIDDK; 1995:15-36; U.S. Census Bureau Statistical Abstract of the U.S.; 2001
US Population: 275 Million in 2000
10
What happens when insulin production and secretion fails?
destruction of Islet beta cells (diabetes type 1)
or loss of response to insulin (diabetes type 2/insulin resistance)
INSULIN ACTION IN MUSCLE AND FAT CELLS
1. Insulin finds and docks onto its receptor.
2. A signal is sent to a pool of glucose transport proteins (Glut 4 Protein) located inside the cell.
3. These Glut 4 proteins move rapidly up to the cell membrane and cause glucose channels to open.
4. Glucose is "escorted " to the interior of the cell where enzymes will begin to break it down to fuel the work of the cell.
Overall Effects of Insulin on Muscle and Fat
MUSCLE blood glucose levels and availability of
energy for muscle contraction Conversion of glucose into glycogen entry of amino acids from the blood breakdown of existing muscle proteins
into glucose
Overall Effects of Insulin on Muscle
What is the effect of diabetes on muscle? lack quick fuel to do their work. Muscle cells then begin to convert glycogen
stores to glucose Muscle cells turn to fat and protein as fuel
sources The result is elevated blood glucose, loss of
muscle mass, weight loss, weakness and fatigue.
Overall Effects of Insulin on FAT
Storage of both excess blood glucose and blood fats inside the fat cell.
provides the body with an energy reserve that can be utilized during prolonged exercise or fasting.
Depositing of blood fats (triglycerides) into fat cells is increased
What is the effect of diabetes on fat? Glucose cannot get in to the fat cell to be
converted to fat. Fat is then broken down for energyproduces ketoacidosis in persons with
Type I diabetes and gestational diabetes
Factors that can contribute
1. Reduced insulin secretion
2. Decreased glucose utilization
3. Increased hepatic glucose production
Figure 338-1
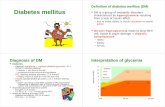
Type NormalPrediabetes DMIFG or IGT + Insulin
Type 1Type 2GDM
FPG<5.6 mmol/L(100 mg/dL)
5.6-6.9 mmol/L(100-125 mg/dL)
>7 mmol/L(126 mg/dL)
2hPG<7.8 (140 mg)
7.8-11.1 (140-199 mg)
>11.1 (200 mg)
Criteria for Diagnosis
1. Symptoms of diabetes (3 P’s, etc) plus RBS >11.1 mmol/L (200 mg/dL) or
2. FBS>7 mmol/L (126 mg/dL) or3. 2 hour PG>11.1 mmol/L (200 mg/dL)
during OGTT (75 gm glucose)
Screening for people >45 yrs. every 3 yrs
• A meal contains 6 to 20 times the glucose content of the blood
• Normally, postprandial hyperglycemia is regulated by• Clearance of ingested glucose by
the liver• Suppression of hepatic glucose
production• Peripheral clearance of glucose
Regulation of Postprandial Glucose
• In impaired glucose tolerance or diabetes, glucose regulation is impaired by • Delayed and reduced insulin secretion• Lack of suppression of glucagon • Hepatic and peripheral insulin
resistance
• Postprandial hyperglycemia results
Impaired Regulation ofPostprandial Glucose
Who Should Be Tested for Diabetes?
Symptoms suggesting diabetes: weight loss, hunger, urinary frequency, blurred vision
Age >45 (>30 if patient has other risk factors) Prior IGT or IFG or family history of diabetes Prior gestational diabetes or baby weighing >9 lb Women with polycystic ovarian syndrome (PCOS) Obesity (BMI 25 kg/m2), especially adolescents African, Latino, Asian, or Native American ancestry History of vascular disease or hypertension
American Diabetes Association. Diabetes Care. 2004;27(suppl 1):S11-S14;AACE/ACE medical guidelines. Endocr Pract. 2002;8(suppl 1):40-82 19
Classification of Diabetes Mellitusby Etiology
Type 1 -cell destruction—complete lack of insulin
Type 2 -cell dysfunction and insulin resistance
Gestational -cell dysfunction and insulin resistance during pregnancy
Other specific types • Genetic defects of -cell function• Exocrine pancreatic diseases• Endocrinopathies• Drug- or chemical-induced• Other rare forms
11
Type 1
injury to β-cells of the pancreas, leading to complete β-cell destruction and total insulin deficiency
5% to 10% of all cases of diabetes and is most frequently diagnosed in children and adolescents
Islet destruction mediated by T lymphocytes Genetic susceptibility (islet cell autoantibodies-
GAD 65)
Type 1
unrestrained glucose production by the liver and impaired uptake of glucose by peripheral target tissue
Environmental factorsViruses (coxsackie, rubella)Bovine milk proteinsNitrosourea compounds (cured meat, cheese)
Putativetrigger
Circulating autoantibodies (ICA, GAD65)
Cellular autoimmunityCellular autoimmunity
Loss of first-phase insulin response (IVGTT)
Glucose intolerance (OGTT)
Clinicalonset—
only 10% of-cells remain
Time
-Cell mass 100%
“Pre”-diabetes
Geneticpredisposition
Insulitis-Cell injury
Eisenbarth GS. N Engl J Med. 1986;314:1360-1368
Diabetes
Natural History Of “Pre”–Type 1 Diabetes
14
Type 2 Pathophysiology
Impaired insulin secretion Insulin resistance Excessive hepatic glucose production Abnormal fat metabolism
Pathogenesis of Type 2 DiabetesTwo Defects
Excessiveglucose production
Impaired glucoseclearance
Hepaticinsulin
resistance
Muscle/fatinsulin
resistance
Impairedinsulin
secretion
Hyperglycemia
16
More glucose entersthe blood stream
Less glucose entersperipheral tissues
Glycosuria
Etiology of Type 2 Diabetes Impaired Insulin Secretion and Insulin Resistance
Genes and environment
Type 2 diabetes
Impaired glucose tolerance
Impaired insulin secretion
Insulin resistance+
Adapted from Ramlo-Halsted BA, Edelman SV. Prim Care. 1999;26:771-789
Natural History of Type 2 Diabetes
Macrovascular complicationsMicrovascular complications
Insulin resistanceInsulin resistance
ImpairedImpairedglucose toleranceglucose tolerance
UndiagnosedUndiagnoseddiabetesdiabetes Known diabetesKnown diabetes
Insulin secretionInsulin secretion Postprandial glucose
Fasting glucoseFasting glucose
17
Acute Complications
Absolute/relative insulin deficiency
Volume depletion Acid-base
abnormalities Hyperglycemia +
Ketosis
Hyperglycemic Hyperosmolar State Type 2
DKA
Signs and symptoms of dehydrationNausea, vomiting, abdominal pain, thirst,
polyuriaTrigger: infection, inadequate insulin,
cocaine, pregnancy
DKA
Hyperglycemia Ketosis Increased anion gap
metabolic acidosis Bicarbonate <10
mmol/L Arterial pH 6.8-7.3
Low sodium Leukocytosis Serum ketones > 1:8
β-hydroxybutyrate
Kidney function tests Fluid deficit 3-5 liters
Goals of Treatment
Hydration: 2-3 L 0.9 saline over the first 3 hours 0.45 saline at 150-300 ml/hr
Short acting Insulin (IV 0.1 units/kg) then 0.1 units/kg/hr by continuous IV infusion
K supplement Monitor anion gap, serum electrolytes, VS, I & O Glucose level: 150-250 mg
Hyperosmolar Hyperglycemic State Elderly type 2 diabetic Trigger: other illness, sepsis, pneumonia,
stroke, AMI Causes: inadequate fluid intake, relative
insulin deficiency Absence of nausea, vomiting, abdominal
pain, Kussmaul breathing
Microvascular Complications of Diabetes
Retinopathy (proliferative and non-proliferative)Leading cause of blindness for ages 20-74
in the USANeovascularization (hallmark -
proliferative)
Nephropathy
-Annual urinary microalbumin screen (normal <30 mg/g creatinine)
-leading cause of ESRD (USA)
-Microalbuminuria 30-300 µg/mg (spot collection)
Neuropathy
-Annual foot exam with 10-g monofilament test
- 50% of patients
- poly, mono, autonomic
- Distal symmetric neuropathy (most common)
GastointestinalGastroparesis (most prominent)
GUTErectile dysfunction
Lower Extremity ComplicationsDM – leading cause of nontraumatic
lower extremity amputation
Identifying Cardiovascular Complications of DiabetesAssess CV risk factors annually and screen for coronary artery disease
Perform stress ECG testing if Cardiac symptoms or abnormal ECG Peripheral or carotid vascular disease Multiple risk factors Plans to begin vigorous exercise program
Refer to cardiologist if Positive exercise ECG test Unable to perform exercise test
300
200
100
0
Plasma glucose (mg/dL)
Postprandialhyperglycemia
Normal
Fasting hyperglycemia
Riddle MC. Diabetes Care. 1990;13:676-686
Time of day
0600 1200 1800 2400 0600
A1C Reflects Both Fasting and Postprandial Hyperglycemia
6
Glycated hemoglobin
hemoglobin A1C, HbA1c, or A1C
reflects the glycemic exposure of a patient’s red blood cells over a 60- to 90-day period and has become the standard indicator of glycemic control in diabetes
The CADRE Recommended A1C
Normal A1C (nondiabetes): 4.0% - 6.0% Target A1C in diabetes: Lowest A1C
possible without unacceptable hypoglycemia* Action recommended: A1C >7.0%
ADA Treatment Goals Table 338-8
A1c <7% Premeal 90-130 mg/dL Peak postmeal <180 mg/dL
BP < 130/80 Lipids
LDL <100 mg/dL HDL >40 mg/dL TG <150 mg/dL
Nutrition Table 338-9
Fat 20-35% Saturated<7% <200 mg/day of dietary
cholesterol 2 or more servings of
fish/week
Carbohydrate 45-65%
Protein 10-35%
45
Antihyperglycemic AgentsMajor Sites of Action
Carbohydrate absorption
Glucose production
Insulin secretion
Secretagogues
Glucose uptake
Injected insulin
Glitazones-Glucosidase inhibitors
–
+
+
+
Pancreas
Metformin
Muscle/Fat
–
–
–
+
GI tract
Liver
Plasma glucose
46
Oral Antihyperglycemic Agentsfor Type 2 Diabetes
Class Agents
Secretagogue SulfonylureasRepaglinide, nateglinide
Biguanide Metformin
α-Glucosidase inhibitor Acarbose, miglitol
Glitazone (TZD) Pioglitazone, rosiglitazone
47
Insulin Secretagogues Sulfonylureas, Repaglinide, and Nateglinide
Mechanism of action Increase basal and/or postprandialinsulin secretion
Efficacy depends upon Functioning -cells
Power Sulfonylureas, repaglinide: decrease A1C 1%–2%
Nateglinide: decreases A1C 0.5%–1%
Dosing Sulfonylureas: 1 or 2 times daily Repaglinide, nateglinide:
3 or 4 times daily with meals
Side effects Weight gain, allergy (rare)
Main risk Hypoglycemia
48
BiguanidesMetformin
Primary mechanism Decreases hepatic glucose of action production
Efficacy depends upon Presence of insulin
Power Decreases A1C 1%–2%Dosing 2 or 3 times daily
(metformin)1 or 2 times daily (metformin
XR)
Side effects Diarrhea, nausea
Main risk Lactic acidosis
49
α-Glucosidase InhibitorsAcarbose and Miglitol
Mechanism of action Delay carbohydrate
absorption
Efficacy depends upon Postprandial hyperglycemia
Power Decrease A1C 0.5%–1%
Dosing 3 times daily
Side effects Flatulence
Main risk Liver enzyme elevation
(rare)Riddle MC. Am Fam Physician. 1999;60:2613-2620; Lebovitz HE. Endocrinol Metab Clin North Am. 1997;26:539-551
50
Glitazones (TZDs)Pioglitazone and Rosiglitazone
Mechanism of action Enhance tissue response to insulinEfficacy depends upon Presence of insulin and resistance
to its action
Power Decrease A1C 0.9%–1.6%
Dosing Once daily
Side effects Edema, weight gain, anemia
Main risk Congestive heart failure
51
Treatment of Postprandial GlycemiaConclusions From Studies
• Most oral agents control mainly fasting (basal)
hyperglycemia
• Acarbose, miglitol, and nateglinide have the greatest
effect on postprandial increments and the least ability
to reduce A1C
52
Efficacy of Oral AntihyperglycemicsDeclines With Time
• A1C rises at ~0.2% to 0.3% yearly on stable therapy
• This rate is the same as for diet alone, sulfonylureas, and metformin
-Cell function declines at the same rate with all these treatments
• Combination treatments are routinely needed
53
Summary of Oral Antihyperglycemic Agents• Four major classes of oral agents acting at different sites
are available• Fasting and preprandial glucose are reduced by
sulfonylureas, repaglinide, metformin, and glitazones (TZDs), with lesser effects on postprandial increments
• Postprandial glucose increments are reduced best by -glucosidase inhibitors and nateglinide
• A1C reductions are similar using sulfonylureas, metformin, and glitazones
• Secondary failure to monotherapy routinely occurs