Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
-
Upload
ibrahim-rawhi-ayasrah -
Category
Documents
-
view
218 -
download
0
Transcript of Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
1/98
Diabetes Mellitus
Ibrahim R. Ayasreh
RN, MSN
2011
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
2/98
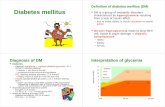
Definition
Diabetes mellitus is a group of metabolic diseases
characterized by elevated levels of glucose in the blood
(hyperglycemia) resulting from defects in insulin secretion,
insulin action, or both.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
3/98
Introduction
Sources of glucose in the blood are : absorption of ingestedfood in the gastrointestinal (GI) tract and formation of glucoseby the liver from food substances
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
4/98
Pancreas
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
5/98
Insulin
Insulin, a hormone produced by the pancreas, controls thelevel of glucose in the blood by regulating the production andstorage of glucose.
In the diabetic state, the cells may stop responding to insulin orthe pancreas may stop producing insulin entirely. This leads tohyperglycemia.
Another pancreatic hormone called glucagon (secreted by thealpha cells of the islets of Langerhans) is released when bloodglucose levels decrease and stimulate the liver to release storedglucose.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
6/98
Functions of insulin
Transports and metabolizes glucose for energy
Stimulates storage of glucose in the liver and muscle (in the form of glycogen).
Signals the liver to stop the release of glucose.
Enhances storage of dietary fat in adipose tissue.
Accelerates transport of amino acids (derived from dietary protein) into cells.
Insulin also inhibits the breakdown of stored glucose, protein, and fat.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
7/98
Regulation of Glucose Level in Blood
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
8/98
Risk factors of DM
Family history of diabetes (ie, parents or siblings withdiabetes).
Obesity ( BMI 27 kg/m2).
Race/ethnicity (eg, African Americans, Hispanic Americans,Native Americans, Asian Americans, Pacific Islanders).
Age 45 years.
Previously identified impaired fasting glucose or impairedglucose Tolerance.
Hypertension (140/90 mm Hg) HDL cholesterol level 35 mg/dL (0.90 mmol/L) and/or
triglyceride level 250 mg/dL (2.8 mmol/L)
History of gestational diabetes or delivery of babies over 9 lbs
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
9/98
Classifications of insulin
Type 1 diabetes (previously referred to as insulin-dependent
diabetes mellitus)
Type 2 diabetes (previously referred to as noninsulin
dependent diabetes mellitus)
Gestational diabetes mellitus.
Diabetes mellitus associated with other conditions or syndrome
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
10/98
Nowadays we dont use terms of dependent
or non-independent insulin DM.
Why
????????????????
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
11/98
Type 1 Diabetes Mellitus
Type 1 diabetes is characterized by destruction of thepancreatic beta cells.
So that no or very little insulin is produced.
Require insulin injections to control their blood glucose levels.
5% to 10% of people with diabetes have type 1 diabetes.
Type 1 diabetes is characterized by an acute onset, usuallybefore age 30
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
12/98
Causes of Type 1 Diabetes Mellitus
Viral Infections.
Genetics predisposition.
Autoimmune response.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
13/98
Pathophysiology of DM type 1
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
14/98
Pathophysiology of DM type 1
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
15/98
Type 2 Diabetes Mellitus
Results from decreased sensitivity to insulin (called insulinresistance) and impaired beta cell functioning resulting indecreased insulin production.
Approximately 90% to 95% of people with diabetes have type2 diabetes.
Type 2 diabetes occurs more among people who are older than
30 years and obese.
Type 2 diabetes is treated with diet and exercise and oralhypoglycemic agents.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
16/98
Insulin Resistance
Normally Insulin resistance
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
17/98
Clinical Manifestations
Polyuria (increased urination).
Polydipsia (increased thirst).
Polyphagia (increased appetite).
fatigue and weakness.
Sudden vision changes.
Tingling or numbness in hands or feet,
Dry skin, skin lesions or wounds that are slow to heal.
Recurrent infections.
For type 1 patient is usually thin at diagnosis, whereas fortype2 patient is usually obese at diagnosis.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
18/98
Assessment & Diagnostic Findings
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
19/98
Assessment & Diagnostic Findings
Hgb(A1C)
Is a blood test that reflects average blood glucose levels over aperiod of approximately 2 to 3 months.
When blood glucose levels are elevated, glucose moleculesattach to hemoglobin in the red blood cell. The longer theamount of glucose in the blood remains above normal, themore glucose binds to the red blood cell and the higher theglycosylated hemoglobin level.
The normal values differ slightly from test to test and fromlaboratory to laboratory and normally range from 4% to 6%.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
20/98
Other Assessment & Diagnostic Tests
Fasting lipid profile
Test for microalbuminuria Serum creatinine level
Urinalysis
Electrocardiogram
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
21/98
Diabetes Management
The main goal of diabetes
treatment is to normalize
insulin activity and blood
glucose levels to reduce the
development of vascular and
neuropathic complications.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
22/98
Nutritional Management
50% to 60% of calories should be derived from carbohydrates,
20% to 30% from fat, and the remaining 10% to 20% from
protein.
Focus on starchy food rather than sugar (sucrose) foods.
The recommendations regarding fat content of the diabetic dietinclude both reducing the total percentage of calories from fat
sources to less than 30% of the total calories and limiting the
amount of saturated fats to 10% of total calories.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
23/98
Nutritional Management
The meal plan may include the use of some nonanimal sourcesof protein (eg, legumes and whole grains) to help reducesaturated fat and cholesterol intake
Increasing fiber in the diet may also improve blood glucoselevels and decrease the need for exogenous insulin, loweringtotal cholesterol and low-density lipoprotein cholesterol in theblood.
Soluble fiber - in foods such as legumes, oats, and some fruits- plays more of a role in lowering blood glucose and lipidlevels than does insoluble fiber,
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
24/98
Nutritional Management
Soluble fiber is thought to be related to the formation of a gel
in the GI tract. This gel slows stomach emptying and the
movement of food through the upper digestive tract.
Insoluble fiber is found in whole-grain breads and cereals and
in some vegetables. This type of fiber plays more of a role in
increasing stool bulk and preventing constipation.
Both insoluble and soluble fibers increase satiety, which is
helpful for weight loss.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
25/98
Nutritional Management
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
26/98
Exercise
Exercise lowers the blood glucose level by increasing the
uptake of glucose by body muscles and by improving insulin
utilization. It also improves circulation and muscle tone.
Exercise also alters blood lipid levels, increasing levels of
high-density lipoproteins and decreasing total cholesterol and
triglyceride levels. This is especially important to the person
with diabetes because of the increased risk of cardiovascular
disease.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
27/98
Exercise Precautions
Patients who have blood glucose levels exceeding 250 mg/dL(14 mmol/L) and who have ketones in their urine should notbegin exercising until the urine tests negative for ketones andthe blood glucose level is closer to normal.
the patient who requires insulin should be taught to eat a 15-gcarbohydrate snack (a fruit exchange) or a snack of complexcarbohydrate with a protein before engaging in moderateexercise, to prevent unexpected hypoglycemia.
Patients participating in extended periods of exercise shouldtest their blood glucose levels before, during, and after theexercise period, and they should snack on carbohydrates asneeded to maintain blood glucose levels
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
28/98
Exercise Precautions
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
29/98
Exercise Precautions
People with diabetes should exercise at the same time and inthe same amount each day.
Regular daily exercise, rather than sporadic exercise, should beencouraged.
A slow, gradual increase in the exercise period is encouraged.
For many patients, walking is a safe and beneficial form ofexercise.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
30/98
Self-Monitoring of Blood Glucose
(SMBG)
Frequent SMBG enables people with diabetes to :
1) Adjust the treatment regimen to obtain optimal bloodglucose control.
2) Allows for detection and prevention of hypoglycemia and
hyperglycemia
3) Reduce the risk of long-term diabetic complications
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
31/98
Types of SMBG devices
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
32/98
Candidates of SMBG
Diabetes patients who treated with intensive treatment therapy.
Patients with unstable diabetes.
Patients who suffer severe hypoglycemia without warning
signs.
Patients with diabetes type 2 , to examine the effect of diet,
exercise, and oral antidiabetic agents.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
33/98
Frequency of SMBG
For most patients who require insulin, SMBG is recommended
two to four times daily (usually before meals and at bedtime).
For patients not receiving insulin may be instructed to assess
their blood glucose levels at least two or three times per week.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
34/98
Sources of error in SMBG
Improper application of blood (eg, drop too small).
Improper meter cleaning and maintenance (eg,
allowing dust or blood to accumulate on the optic
window).
Damage to the reagent strips by heat or humidity; use
of outdated strips.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
35/98
Urine Testing for Glucose
The advantages of urine glucose testing are that it is less expensive than SMBGand it is not invasive.
Disadvantages of urine testing include the following:
- Results do not accurately reflect the blood glucose level at the time of the test.
- The renal threshold for glucose is 180 to 200 mg/dL (9.9 to 11.1 mmol/L), farabove target blood glucose levels.
- Hypoglycemia cannot be detected because a negative urine glucose result
may occur when the blood glucose level ranges from 0 to 180 mg/dL (9.9
mmol/L) or higher.
- Patients may have a false sense of being in good control when results are
always negative.
-Various medications (eg, aspirin, vitamin C, some antibiotics) may interfere
with test results.
- In elderly patients and patients with kidney disease, the renal threshold (the
level of blood glucose at which glucose starts to appear in the urine) is raised;
thus, false-negative readings may occur at dangerously elevated glucose levels.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
36/98
Pharmacologic Therapy
Insulin therapy.
Oral hypoglycemic drugs.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
37/98
Insulin Therapy
Insulin therapy is necessary for:
- Type 1 diabetes patients.
- Type 2 diabetes patients in which diet and oral agentsfail to control blood glucose.
- Temporarily for type 2 diabetes who is usuallycontrolled by diet alone or by diet and an oral agentmay require insulin during illness, infection,pregnancy, surgery, or some other stressful even
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
38/98
Categories of Insulin
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
39/98
Insulin Species
Animal insulins were obtained from beef
(cow) and pork (pig) pancreases.
Human insulins are now widely available.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
40/98
Insulin Regimens
(Conventional Approach)
One approach is to simplify the insulin regimen as much as
possible, with the aim of avoiding the acute complications ofdiabetes (hypoglycemia and symptomatic hyperglycemia).
With this type of simplified regimen (eg, one or moreinjections of a mixture of short- and intermediate-actinginsulins per day), patients may frequently have blood glucoselevels well above normal.
This approach would be appropriate for the terminally ill, thefrail elderly with limited self-care abilities, or any patient whois completely unwilling or unable to engage in the self-management activities.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
41/98
Insulin Regimens(Intensive Approach)
Intensive treatment (three or four injections of insulin
per day) reduced the risk of complications.
Another reason for using a more complex insulinregimen is to allow patients more flexibility to changetheir insulin doses from day to day in accordance
with changes in their eating and activity patterns, withstress and illness, and as needed for variations in theprevailing glucose level.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
42/98
Complications of insulin therapy
(Local allergic reactions)
A local allergic reaction (redness, swelling, tenderness, and
induration or a 2- to 4-cm wheal) may appear at the injection
site 1 to 2 hours after the insulin administration.
These reactions, which usually occur during the beginning
stages of therapy and disappear with continued use of insulin.
The physician may prescribe an antihistamine to be taken 1
hour before the injection if such a local reaction occurs.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
43/98
Complications of insulin therapy
(Systemic allergic reactions)
An immediate local skin reaction that gradually spreads into
generalized urticaria (hives).
The treatment is desensitization, with small doses of insulin
administered in gradually increasing amounts.
These rare reactions are occasionally associated with
generalized edema or anaphylaxis.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
44/98
Complications of insulin therapy
(Lipodystrophy)
Lipoatrophy is loss of subcutaneous fat and appears as slight
dimpling or more serious pitting of subcutaneous fat.
Lipohypertrophy, the development of fibrofatty masses at theinjection site, is caused by the repeated use of an injection site.
Rotation of injection sites is soimportant
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
45/98
Lipoatrophy
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
46/98
Lipohypertrophy
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
47/98
Rotation is the solution
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
48/98
Complications of insulin therapy
(Insulin Resistance)
Clinical insulin resistance has been defined as a daily insulin
requirement of 200 units or more.
This may occur for various reasons, the most common being
obesity, which can be overcome by weight loss.
It may be related to formation of autoantibodies againstinsulin, but it is rarely occur.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
49/98
Complications of insulin therapy
(Morning Hyperglycemia)
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
50/98
Oral Antidiabetic Agents
Oral antidiabetic agents may be effective for patients who havetype 2 diabetes that cannot be treated by diet and exercisealone.
They cannot be used during pregnancy.
Oral antidiabetic agents include the sulfonylureas, biguanides,
alpha glucosidase inhibitors, thiazolidinediones, andmeglitinides
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
51/98
Sulfonylureas
Directly stimulating the pancreas to secrete insulin. Therefore,a functioning pancreas is necessary for these agents to beeffective.
They cannot be used in patients with type 1 diabetes.
The sulfonylureas can be divided into first- and second-generation categories.
The most common side effects of these medications are GIsymptoms and dermatologic reactions. Hypoglycemia mayoccur when an excessive dose of a sulfonylurea is used orwhen the patient omits or delays meals, reduces food intake, orincreases activity.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
52/98
Biguanides
Metformin (Glucophage) produces its antidiabetic effects byfacilitating insulins action on peripheral receptor sites.
It can be used only in the presence of insulin. Biguanides have
no effect on pancreatic beta cells.
Lactic acidosis is a potential and serious complication ofbiguanide therapy
Metformin is contraindicated in patients with renal impairment(serum creatinine level more than 1.4) or those at risk for renaldysfunction (eg, those with acute myocardial infarction).
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
53/98
Alpha glucosidase inhibitors
Acarbose (Precose) and miglitol (Glyset) are oral alphaglucosidase inhibitors used in type 2 diabetes management.
They work by delaying the absorption of glucose in theintestinal system, resulting in a lower postprandial bloodglucose level. As a consequence of plasma glucose reduction,hemoglobin A1C levels drop.
Their side effects are diarrhea and flatulence. These effectsmay be minimized by starting at a very low dose andincreasing the dose gradually.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
54/98
Thiazolidinediones.
Rosiglitizone (Avandia) and pioglitozone (Actos) are oral
diabetes medications categorized as thiazolidinediones.
Thiazolidinediones enhance insulin action at the receptor site
without increasing insulin secretion from the beta cells of the
pancreas.
These medications may affect liver function; therefore, liver
function studies must be performed at baseline and at frequent
intervals(monthly for the first 12 months of treatment).
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
55/98
Meglitinides
Repaglinide (Prandin), an oral glucose-lowering agent of theclass of oral agents called meglitinides, lowers the bloodglucose level by stimulating insulin release from the pancreaticbeta cells.
Its effectiveness depends on the presence of functioning betacells. Therefore, repaglinide is contraindicated in patients withtype 1 diabetes.
The principal side effect of repaglinide is hypoglycemia;however, this side effect is less severe and frequent than for asulfonylurea because repaglinide has a short half-life(approximately 1 hour).
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
56/98
Self-administration of insulin
Storing Insulin:
- Cloudy insulins should be thoroughly mixed by gently
inverting the vial or rolling it between the hands before
drawing the solution into a syringe.
- Whether insulin is the short- or long-acting preparation, the
vials not in use should be refrigerated and extremes of
temperature should be avoided; insulin should not beallowed to freeze and should not be kept in direct sunlight
or in a hot car.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
57/98
Self-administration of insulin
The insulin vial in use should be kept at room temperature to
reduce local irritation at the injection site, which may occur
when cold insulin is injected.
Patients should be instructed to always have a spare vial of the
type or types of insulin they use.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
58/98
Self-administration of insulin
Selecting Syringes:
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
59/98
Self-administration of insulin
Mixing Insulins:
When rapid- or short-acting insulins are to be given simultaneously
with longer-acting insulins, they are usually mixed together in thesame syringe.
the longer-acting insulins must be mixed thoroughly before useWhile there are varying opinions regarding which type of insulin(short- or longer-acting) should be drawn up into the syringe first
when they are going to be mixed, the ADA recommends that theregular insulin be drawn up first.
The most important issue isthat patients not inject one type ofinsulin into the bottle containing a different type of insulin.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
60/98
Self-administration of insulin
The ratio of 70/30 (70% NPH and 30% regular insulin in one
bottle) is the most common.
Most (if not all) of the printed materials available on insulin
dose preparation instruct patients to inject air into the bottle of
insulin equivalent to the number of units of insulin to be
withdrawn.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
61/98
Self-administration of insulin
Selecting and rotating injection site:
- The four main areas for injection are the abdomen, arms (posterior surface),thighs (anterior surface), and hips.
- The speed of absorption is greatest in the abdomen and decreasesprogressively in the arm, thigh, and hip.
- Systematic rotation of injection sites within an anatomic area isrecommended to prevent localized changes in fatty tissue (lipodystrophy).
- Patients should try not to use the same site more than once in 2 to 3 weeks. I
- if the patient is planning to exercise, insulin should not be injected into thelimb that will be exercised
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
62/98
Sites of insulin injections
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
63/98
Self-administration of insulin
Preparing the skin:
- Use of alcohol to cleanse the skin is not recommended, butpatients who have learned this technique often continue to use
it.
- If alcohol is used to cleanse the injection area, patients should
be cautioned to allow the skin to dry after cleansing with
alcohol. If the skin is not allowed to dry before the injection.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
64/98
Pinching is preferable
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
65/98
Acute complications of DM
Hypoglycemia.
Diabetic Ketoacidosis (DKA).
Hyperglycemic Hyperosmolar Nonketotic Syndrome
(HHNS).
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
66/98
Hypoglycemia
Hypoglycemia (abnormally low blood glucose level) occurs
when the blood glucose falls to less than 50 to 60 mg/dL (2.7
to 3.3 mmol/L).
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
67/98
Causes of hypoglycemia
Too much insulin.
Too much oral hypoglycemic agents.
Too little food.
Excessive physical activity
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
68/98
Clinical manifestations of hypoglycemia
They can be categorized into:
- Adrenergic symptoms.
- Central nervous system (CNS) symptoms.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
69/98
Mild hypoglycemia
In mild hypoglycemia, as the blood glucose level falls, the
sympathetic nervous system is stimulated, resulting in anincrease of epinephrine and norepinephrine.
Sweating.
Tremor.
Tachycardia.
Palpitation. Nervousness.
hunger
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
70/98
Moderate hypoglycemia
In moderate hypoglycemia, the fall in blood glucose leveldeprives the brain cells of needed fuel for functioning. Signs ofimpaired function of the CNS may include:
- inability to concentrate. - headache.
- lightheadedness. - confusion.
- memory lapses. - numbness of the lips and tongue.
- slurred speech. - impaired coordination,- emotional changes. - irrational or combative behavior.
- double vision.
- drowsiness.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
71/98
Severe hypoglycemia
In severe hypoglycemia, CNS function is so impaired that thepatient needs the assistance of another person for treatment of
hypoglycemia.
Symptoms may include:
- Disoriented behavior.
- Seizures.- Difficulty arousing from sleep.
- Loss of consciousness
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
72/98
Management of hypoglycemia
For patients who are unconscious and cannot swallow, an
injection of glucagon 1 mg can be administered either
subcutaneously or intramuscularly.
A concentrated source of carbohydrate followed by a snack
should be given to the patient on awakening to prevent
recurrence of hypoglycemia.
In the hospital or emergency department, patients who are
unconscious or cannot swallow may be treated with 25 to 50
mL 50% dextrose in water (D50W) administered
intravenously. The effect is usually seen within minutes.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
73/98
Glucagon injection
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
74/98
Prevention of hypoglycemia
DM patients must carry some form of simple sugar
with them at all times.
Patients are advised to refrain from eating high-calorie, high fat dessert foods (eg, cookies, cakes,
doughnuts, ice cream) to treat hypoglycemia. The
high fat content of these foods may slow the
absorption of the glucose.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
75/98
Diabetic Ketoacidosis
DKA is caused by an absence or markedly inadequate amountof insulin. This deficit in available insulin results in disorders
in the metabolism of carbohydrate, protein, and fat.
The three main clinical features of DKA are:
- Hyperglycemia
- Dehydration and electrolyte loss
- Acidosis.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
76/98
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
77/98
Clinical manifestations
Polyuria and polydipsia.
Blurred vision,
Weakness, and headache.
Orthostatic hypotension.
GI symptoms such as anorexia, nausea, vomiting, and
abdominal pain.
Patients may have acetone breath (a fruity odor), which occurs
with elevated ketone levels.
Hyperventilation.
Patients may be alert, lethargic, or comatose.
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
78/98
Kussmaul respirations
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
79/98
Assessment and Diagnostic Findings
Blood glucose levels may vary from 300 to 800 mg/dL (16.6to 44.4 mmol/L).
low serum bicarbonate (0 to 15 mEq/L) and low pH (6.8 to
7.3).
low PCO2 level (10 to 30 mm Hg).
Elevated levels of creatinine, blood urea nitrogen (BUN),hemoglobin, and hematocrit may also be seen withdehydration.
Medical management
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
80/98
Medical management
(Rehydration)
Patients may need up to 6 to 10 liters of IV fluid to replace
fluid losses caused by polyuria, hyperventilation, diarrhea, andvomiting.
Initially, 0.9% sodium chloride (normal saline) solution isadministered at a rapid rate, followed by 0.45% sodiumchlorise solution.
When the blood glucose level reaches 300 mg/dL (16.6mmol/L) or less, the IV fluid may be changed to dextrose 5%in water (D5W) to prevent a precipitous decline in the bloodglucose level.
Medical management
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
81/98
Medical management
(Restoring electrolytes)
The major electrolyte of concern during treatment of DKA is
Potassium. Why ???????????
Cautious but timely potassium replacement is vital to avoid
dysrhythmias that may occur with hypokalemia. Up to 40 mEqper hour may be needed for several hours.
Frequent (every 2 to 4 hours initially) electrocardiograms and
laboratory measurements of potassium are necessary duringthe first 8 hours of treatment.
Potassium replacement is withheld only if hyperkalemia ispresent or if the patient is not urinating
Medical management
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
82/98
Medical management
(Reversing acidosis)
The acidosis that occurs in DKA is reversed with insulin,
which inhibits fat breakdown, thereby stopping acid buildup.
Insulin is usually infused intravenously at a slow, continuousrate.
Dextrose water such as (D5NS or D50.45NS), are
administered when blood glucose levels reach 250 to 300mg/dL (13.8 to 16.6 mmol/L) to avoid too rapid a drop in theblood glucose level
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
83/98
Hyperglycemic Nonketotic Syndrome
(HHNS)
Hyperosmolar
L li i f DM
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
84/98
Long-term complications of DM
Macrovascular complications.
Microvascular complications.
M l li i
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
85/98
Macrovascualr complications
Coronary artery disease, cerebrovascular disease, and peripheral
vascular disease are the three main types of macrovascularcomplications.
Myocardial infarction is twice as common in diabetic men and threetimes as common in diabetic women,
cerebrovascular disease includes transient ischemic attacks andstrokes.
Signs and symptoms of peripheral vascular disease includediminished peripheral pulses and intermittent claudication (pain inthe buttock, thigh, or calf during walking). The severe form ofarterial occlusive disease in the lower extremities is largelyresponsible for the increased incidence of gangrene leading to
diabetic foot.
Mi l li i
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
86/98
Microvascualr complications
Diabetic microvascular disease (or microangiopathy) is
characterized by capillary basement membrane thickening.
The basement membrane surrounds the endothelial cells of the
capillary.
Two areas affected by these changes are the retina and the
kidneys.
N l R ti
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
87/98
Normal Retina
Background Retinopathy
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
88/98
Background Retinopathy
Early stage, asymptomatic retinopathy. Blood vessels within the retinadevelop microaneurysms that leak fluid, causing swelling and formingdeposits (exudates).
P lif ti R ti th
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
89/98
Preproliferative Retinopathy
Represents increased destruction of retinal blood vessels
P lif ti R ti th
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
90/98
Proliferative Retinopathy
Abnormal growth of new blood vessels on the retina. New vessels rupture,bleeding into the vitreous and blocking light. Ruptured blood vessels in thevitreous form scar tissue, which can pull on and detach the retina.
N h th
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
91/98
Nephropathy
The earliest detectable change in the course of
diabetic nephropathy is a thickening in the
glomerulus. At this stage, the kidney may startallowing moreserum albumin ( plasma protein) than
normal in theurine ( albuminuria ), and this can be
detected by sensitivemedical testsfor albumin. This
stage is called " microalbuminuria "
Di b ti N th
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
92/98
Diabetic Neuropathy
Refers to a group of diseases that affect all types of nerves,
including peripheral (sensorimotor), autonomic, and spinal
nerves.
P i h l N th
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
93/98
Peripheral Neuropathy
Initial symptoms include paresthesias and burning sensations(especially at night).
As the neuropathy progresses, the feet become numb.
In addition, a decrease in proprioception (awareness of postureand movement of the body and of position and weight ofobjects in relation to the body).
Decreased sensation of light touch may lead to an unsteadygait.
Decreased sensations of pain and temperature place patientswith neuropathy at increased risk for injury and undetected foot
infections.
A t i N thi
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
94/98
Autonomic Neuropathies
Neuropathy of the autonomic nervous system results in a broadrange of dysfunctions affecting almost every organ system of the
body.
Three manifestations of autonomic neuropathy are related to the
cardiac, GI, and renal systems.
Cardiovascular symptoms range from fixed, slightly tachycardic
heart rate; orthostatic hypotension; and silent, or painless,
myocardial ischemia and infarction.
GI symptoms include: Delayed gastric emptying may occur with the
typical symptoms of early satiety, bloating, nausea.
Urinary retention, a decreased sensation of bladder fullness, and
other urinary symptoms of neurogenic bladder result from
autonomic neuropathy.
Sudomotor Neuropathy
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
95/98
Sudomotor Neuropathy
This neuropathic condition refers to a decrease or absence of
sweating (anhidrosis) of the extremities.
Foot and Leg ulcers
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
96/98
Foot and Leg ulcers
From 50% to 75% of lower extremity amputations are performed on people withdiabetes.
Complications of diabetes that contribute to the increased risk of foot infectionsinclude:
- Neuropathy: Sensory neuropathy leads to loss of pain and pressure sensation, and
autonomic neuropathy leads to increased dryness and fissuring of the
skin (secondary to decreased sweating). Motor neuropathy results in
muscular atrophy, which may lead to changes in the shape of the
foot.
- Peripheral vascular disease: Poor circulation of the lower extremities contributes
to poor wound healing and the development
of gangrene.- Immunocompromise: Hyperglycemia impairs the ability of specialized leukocytes
to destroy bacteria. Thus, in poorly controlled diabetes,
there is a lowered resistance to certain infections.
Foot and Leg ulcers
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
97/98
Foot and Leg ulcers
Foot and Leg ulcers
-
7/30/2019 Diabetes Mellitus - by Ibrahim Rawhi Ayasreh
98/98
Foot and Leg ulcers
High-risk characteristics include:
- Duration of diabetes more than 10 years
- Age older than 40 years
- History of smoking
- Decreased peripheral pulses
- Decreased sensation
- Anatomic deformities or pressure areas (eg, bunions,calluses, hammer toes)
- History of previous foot ulcers or amputation