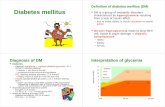
Diabetes mellitus, Classification and Treatment of Diabetes mellitus
Diabetes Mellitus
Transcript of Diabetes Mellitus

Diabetes Mellitus

Pancreas• located in the upper left aspect of the abdominal cavity• mixed gland
1. Acinar Cells (Exocrine Gland)- secretes pancreatic juices which aids in digestion
2. Islets of Langerhans (Endocrine Gland)- produce hormones

Pancreatic IsletsPancreatic Islets

A. alpha cellsglucagons – increases glucose levels (gluconeogenesis)
B. beta cellsinsulin – decreases glucose levels
C. delta cellssomatostatin – inhibits the action of growth
hormone

Diabetes MellitusMetabolic disorder characterized by non-utilization of carbohydrates, protein, and fat metabolism
Characterized by the absence of or a severe decrease in secretion or utilization of insulin

2 Types of Diabetes Mellitus

IDDM – Type 1(Insulin Dependent)
1. Insulin: Absent
2. OnsetChildhoodBefore 18 y/o(10-15 y/o)Juvenile Onset
3. Predisposing FactorsHereditaryViral InfectionsCarbon Tetrachloride TocicityDrugs – Steroids
NIDDM – Type 2(Non Insulin Dependent)
1. Insulin: deficient
2. OnsetAdulthood> 40 yrs oldAdult onset DM
3. Predisposing FactorsObesity

IDDM – Type 1(Insulin Dependent)
NIDDM – Type 2(Non Insulin Dependent)
4. Clinical Manifestations3 P’sWeight LossBed WettingOnset is rapid(days to weeks)Increase frequency of infectionFatigue
4. Clinical Manifestation3 P’sWeight Gain
Onset is slow(over months)Increase frequency of infectionFatigue
5. ComplicationDiabetic Ketoacidosis (DKA)
> ↑ mobilization of fats & CHON> Ketones> Blood Glucose: 300-800mg/dl
5. ComplicationHyperosmolar Non-Ketotic Syndrome
> Extreme hyperglycemia> Blood Glucose: 700-1200mg/dl

↑ CHO uptake of cells↓ insulin requirementsDone 1-2 hr after meals to prevent hypoglycemia
Low calorieHigh fiberComplex carbo
InsulinOHA

IDDM – Type 1(Insulin Dependent)
NIDDM – Type 2(Non Insulin Dependent)
6. ManagementDietExerciseMedication: Insulin
6. ManagementDietExerciseMedication: Oral
Hypoglycemic Agents

Hyperglycemia

Diagnostic Tests1. Glucose Tolerance Test (GTT) – determines the ability to tolerate a standard glucose load without spillage over the urine
•150-300 grams of carbohydrates/p.o.•Series of blood specimen is collected
30 minutes1 hr2 hrs *3, 4, 5 hrs as required
2. Glycated Hemoglobin (Glycohemoglobin, Glycosylated Hemoglobin, HbA)
•Gives average glucose level for prior two to three months•Most accurate
Adult 2.2%-4.0%Adult 2.2%-4.0%Children 1.8%-4.0%Children 1.8%-4.0%

3. Two Hours Postprandial TestInitial blood specimen is withdrawn100 gm of sugar orallythen check after 2 hoursN: <140 mg/dl
Diagnostic Tests
4. Blood glucose monitoring - finger sticks
5. Urine glucose and ketone monitoring

Insulin Therapy Primary function of insulin is to transport glucose into muscle and fat cells.
Sources:1. Animal source – beef and pork; rarely given due
to severe allergic reaction.2. Human – has less antigenecity property
1. Rapid Acting eg. Regular2. Intermediate eg. NPH3. Long Acting eg. Ultra Lente
TypesClear
Cloudy
Cloudy
Color Onset Peak Duration2-4 hrs
8-16 hrs
16-24 hrs

Nursing Considerations1. Administer insulin at room temperature to prevent
lipodystrophy, which is atrophy/ hypertrophy of SQ tissues
2. Insulin is only refrigerated once opened.

3. Gently roll vial in between palms to redistribute insulin particles. Avoid shaking to prevent formation of bubbles because it makes it difficult to aspirate the exact amount
4. Use gauge 25 – 26 needle
5. Administer insulin at either 45 or 90
6. Rotate injection site to prevent lipodystrophy
7. Most accessible site is the abdomen
8. When mixing 2 types of insulin, aspirate first the clear then the cloudy

Insulin Injection Sites

Complications of Insulin Therapy
1. Local Allergic ReactionsInstruct the client to avoid injecting insulin into affected sites.
2. Insulin Lipodystrophy – development of fatty masses at the injection sites.
Instruct the client about the importance of rotating injection sites
3. Insulin Resistance – the client develops immune antibodies that bind the insulin
Treatment consists of administering purer insulin preparation

4. Dawn Phenomenon – results from reduced tissue sensitivity to insulin that develops between 5 and 8 AM (prebreakfast hyperglycemia occurs) and may be caused by nocturnal release of growth hormone
Treatment includes administering an evening dose of intermediate acting at 10 PM.
5. Somogyi Phenomenon – rebound effect characterized by hypoglycemia and hyperglycemia
Complications of Insulin Therapy

Oral Hypoglycemic AgentsIt stimulates the pancreas to secrete or produce insulin.Indicated only in Type 2 DM
Eg.DiabenaseOrinaseTolinase
Nursing Considerations
1. Administer with food to decrease GIT irritation and prevent hypoglycemia
2. Instruct the client not to take alcoholic beverages because it can lead to severe hypoglycemic reaction.
Micronase GlucotrolDaonilDiamicron

Nursing Processes—Diagnosis of the Patient With Diabetes
• Imbalanced nutrition
• Risk of impaired skin integrity
• Deficient knowledge

Nursing Managementfor Clients with Diabetes Mellitus
1. Monitor sign and symptoms of hypoglycemia or hyperglycemia2. Monitor VS, blood sugar, and I/O3. Exercise after meals to increase glucose utilization4. Monitor for complication
AtherosclerosisMicroangiopathies
Eyes – premature cataract, diabetic retinopathy, or blindnessKidneys – recurrent pyelonephritis and renal failure (nephropathy)
Gangrene FormationShock due to dehydrationPeripheral Neuropathy

5. Diabetic DietCHO – 50%CHON – 30%Fats – 20%
6. Foot care management7. Encourage annual eye and kidney exam8. Monitor for sign of DKA and HONK9. Assist in surgical debridement10. Assist in BKA or AKA
Nursing Managementfor Clients with Diabetes Mellitus

3 Pathies of Diabetes Mellitus
NephropathyNeuropathy
Retinopathy

1. Wash feet daily with mild soap with tepid water. 2. Do not soak feet. 3. Pat dry thoroughly especially in between toes; do not
rub. 4. Observe feet every day, in bright light, for dryness,
redness, swelling, sores. 5. Never cut corns or calluses. 6. Use lotion to prevent dryness but do not use lotion in
between toes. 7. Wear cotton socks and change them several times
each day if feet perspire. 8. Trim toenails only after bathing, when they are soft
and pliable.9. Cut toenails straight across. 10.Never go barefoot.
FOOT CARE

11.Do not wear circular garters or anything that constricts blood flow to feet.
12.Avoid shoes that fit poorly. 13.Treat cuts and scratches right away with antiseptic
and topical antibiotic. 14.Call health care provider for any sign of infection,
blisters, or sores on feet.
FOOT CARE

References: 1. Memory Notebook of Nursing2. Brunner and Suddarth’s Textbook of Medical
Surgical Nursing3. Medical Surgical Nursing by Udan4. Luckmann and Sorensen’s Medical Surgical
Nursing5. NCSBN Learning Extension6. Saunders Comprehensive Review for the NCLEX-
RN Exam7. Illustrated Study Guide for the NCLEX-RN Exam
by Zerwekh8. Fundamentals of Nursing by Kozier