The Economics of Managing Patients With Diabetes and Coronary Artery Disease: A Payer Perspective
Diabetes and Coronary Artery Disease Therapy and Outcomes ...
Transcript of Diabetes and Coronary Artery Disease Therapy and Outcomes ...

Diabetes and Coronary Artery Disease -Therapy and Outcomes
John D. Rutherford, MB ChB, FRACP
Internal Medicine Grand Rounds University of Texas Southwestern Medical Center
Dallas, Texas
September 7, 2000
" This is to acknowledge that John D. Rutherford has disclosed no financial interests or other relationships with commercial concerns related directly or indirectly to this program. Dr Rutherford will not be discussing "off-label" uses in his presentation."

Biographical information:
John D. Rutherford, MB ChB, FRACP, FACC Associate Dean, Clinical Affairs, Professor of Internal Medicine, Associate Chief of Cardiology, Gail Griffiths Hill Chair in Cardiology.
Interests:
Acute and Chronic Ischemic Heart Disease Heart Disease in Pregnancy
2

Introduction:
Cardiovascular disease (coronary, cerebral and peripheral vascular disease) is the leading cause of death in people with diabetes and most deaths are due to the complications of coronary artery disease (1). Diabetics have greater morbidity and mortality following acute myocardial infarction and have a higher prevalence of traditional coronary risk factors (hypertension, dyslipidemia and obesity) compared to people without diabetes. However, these risk factors account for less than half of the excess mortality associated with diabetes. The _public health impact of cardiovascular disease in diabetics is enormous and increasing (1 ). Populations that are particularly susceptible to diabetes (African Americans, Hispanics, Native Americans, Pacific Islanders, and Asians) are growing in the United States and Type II diabetes occurs at an earlier age in obese and overweight persons (2). The prevalence of obesity is rising in the United States and is heightened by physical inactivity. Therefore, the relationship between diabetes and coronary artery disease is important and outcomes with medical therapy and following revascularization are issues commonly encountered in clinical practice.
Mortality following acute coronary syndromes:
45
40
35
% 30
25
20
15
10
5
0
Figure 1.
MORTALITY AFTER FIRST Ml 1988-92 Finnish Myocardial Infarction Register
28d Mortality 1 yr Mortality
M jettinen et al, Diabetes Care 1998; 21:69
Compared with non-diabetics when diabetics present with acute coronary syndromes both short and long term mortality are nearly doubled. When diabetics present to an emergency room with a suspected acute myocardial infarction and "rule-out" (3, 4), in the subsequent year their mortality and infarction rate is twice that of non-diabetics (20% versus 10%) (4). In non-insulin requiring diabetics, with unstable angina, one year mortality is 17% compared to 9% in non-diabetic patients (5) and this difference is
3

largely accounted for by excessive early mortality-- the three month mortality was 8.6% and 2.5% respectively. In a Finnish study (1988-1992) examining the impact of diabetes on mortality after a first myocardial infarction (6) diabetic men and women had substantially increased mortality at one month and one year compared with non-diabetics (6, 7), [Figure 1].
When a patient has an acute myocardial infarction the presence of diabetes is one of the major clinical prognostic factors which determines short and long term prognosis. At the time of entry to hospital with acute myocardial infarction the clinical prognostic indicators are: the patients age, a history of prior myocardial infarction, evidence of cardiac dysfunction, and the presence of diabetes. In addition, hospital mortality is determined by the presence of anterior myocardial infarction and hypotension (8-11 ). Other independent prognostic indicators also apply to diabetics. Both proteinuria (12-15) and diabetic retinopathy (16-20) are predictors of future coronary events (13, 18), [Figure 2]. The risk of cardiovascular death is associated
Figure 2.
Proteinuria : Death & Myocardial Infarction during 7 year follow up
35 Proteinuria 30 < 150 mg/L
25 001150-300 mg/L
II> 300 mg/L % 20
15
10
5
0 Non diabetics NIDDM
Meittinen et al, Stroke 1996; 27:2033
with increased urinary albumin and protein excretion rate in non-diabetics and diabetics independent of classic risk factors (18). Population studies have shown that in Type II diabetics as hemoglobin A1c and proteinuria increase the plasma fibrinogen levels increase. The Framingham Study has demonstrated the significant role of fibrinogen as a risk factor for the development of coronary artery disease. Non proliferative diabetic retinopathy may be associated with restricted coronary flow reserve in diabetic patients
4

( 19) and proliferative retinopathy predicts future significant coronary heart disease events (18).
Thrombolytic therapy
In the fibrinolytic therapy trialists (FfT) collaborative overview of mortality and morbidity of acute myocardial infarction (derived from all randomized trials of more than 1,000 patients receiving fibrinolytic therapy) diabetics comprised 10-20% of the population (21). They were older, more likely to have had prior myocardial infarction and were found to have worse left ventricular function, more extensive coronary artery disease and higher morbidity and mortality (21). Importantly, lytic therapy was of greater benefit to diabetic patients [Figure 3].
Figure 3.
AMI : Lytic Therapy in Diabetics
DIABETICS
• 1 0-20o/o of patients
• Older • More prior Ml • Worse LVEF's • More disease • Higher morbidity • Higher mortality
40
35
30
25
20
15
10
5
......------lONon Diabetics
Ill Diabetics
•A ll Patients
0 +-""----Lives sa ved/1 0 00
at 35d
FTT Group Lancet 1994:343:311
At 35 days 37 per 1000 diabetic lives were saved compared with 15 per 1000 nondiabetic lives saved. In a large angiographic trial, of thrombolytic therapy and acute myocardial infarction, diabetes was also found to be an independent determinant of early mortality (22). There was no significant difference in early infarct artery-related patency in response to thrombolytic therapy between diabetics and non-diabetics. However, diabetic patients had significantly narrower "normal" reference coronary artery segments suggesting more extensive, non angiographically identifiable epicardial coronary artery disease. They had a greater frequency of multi-vessel disease, and the non infarct areas of myocardium showed a blunted acute hyperkinetic response in contractility compared to non-diabetics. The 30 day mortality rate was 11.3% in diabetic patients versus 6% in
5

non-diabetic patients (P < 0.0001) After adjustment for clinical and angiographic variables diabetes remained an independent determinant of mortality.
When the entire GUSTO-I cohort (23) was examined (41,021 patients treated with streptokinase, t-P A and heparin), diabetes in association with its co-morbidities (cardiac failure, cardiogenic shock, atrial tachyarrhythmias and atrioventricular block) accounted for a substantially worse one month (10.5% versus 6.2%) and one year prognosis (14.5% versus 8.9%). Mortality was highest amongst diabetic patients treated with insulin (23). Unfortunately, observational studies in diabetics suggest that thrombolytic therapy is often withheld inappropriately because of concerns about retinal hemorrhage (24). It is important to note that diabetic retinopathy is not a contraindication to thrombolytic therapy. Ocular hemorrhage, and more importantly, intra ocular hemorrhage after thrombolytic therapy is extremely uncommon. The calculated incidence of intra ocular hemorrhage following thrombolytic therapy in patients with diabetes is 0.05% (25).
Insulin and acute myocardial infarction
The DIGAMI (Diabetes Mellitus Insulin-Glucose Infusion in Acute Myocardial Infarction) Study Group randomized patients with acute myocardial infarction (Q and non-Q) and a history of diabetes (on diet, tablets or insulin) or an initial blood glucose greater than 198 mg/dl to conventional therapy or insulin-glucose infusion for at least 24 hours and subsequent subcutaneous insulin administration for at least 3 months. The rationale for this protocol "was based on the assumption that a rapidly achieved and persistent improvement in metabolic control should reduce morbidity and mortality in
%
Figure 4.
DIGAMI: MORTALITY AFTER AMI
45~-----------------------------------------,
40u-------------~
35u--------------4
3ou-------------~
25~------~~--~
2 0 IA-:-:~----i
1 5 J...h~ibl-----1
10
5
0 3 mo 1 year 3 years
Entire Study
3 mo 1 year 3 years
"No Prior Insulin- Low Risk"
diabetic patients with myocardial infarction" (26). Diabetics, particularly those with poor metabolic control, have elevated plasma levels of free fatty acids and increased sensitivity to catecholamine stimulation. There is no
6

anerobic pathway for metabolism of free fatty acids. In addition, free fatty acids and their intermediates may potentiate ischemic injury and there appears to be a direct relationship between high levels of free fatty acids and complications of acute myocardial infarction. In the past insulin-glucose-potassium has been demonstrated to counteract intracellular potassium loss in ischemic myocardium, reduce plasma levels of free fatty acids, improve segmental ejection fraction in the infarcted areas of myocardium and reduce complication rates. Concomitant therapy in DIGAMI patients was lytic therapy in 50%, beta-blockers in 70%, aspirin in 80% and ACE inhibitors in 31%. The patients were stratified into 4 groups before randomization. They were considered high risk with two, or more, of the following: age greater than 70 years, prior myocardial infarction, a history of congestive heart failure, and current treatment with digitalis. They were also stratified according to previous anti-diabetic treatment with insulin. Thus, there were 4 groups: No insulin-low risk, No insulin-high risk, Insulin-low risk, and Insulin-high risk. After 3, 12 and 41 months the patients who had never had insulin prior to hospitalization with acute infarction and were considered "low risk" had a substantial mortality advantage (26-30). In the entire study, insulin therapy reduced mortality significantly at 12 months (26), and 41 months (28) [Figure 4]. The mortality predictors in this population were: Old age, previous myocardial infarction, diabetes mellitus duration, admission blood glucose and admission hemoglobin A1e. Intensive insulin treatment reduced long-term mortality despite high admission blood glucose and hemoglobin A1e (30) and the therapy was cost-effective (31).
Aspirin
The beneficial affect of aspirin is maintained in diabetic patients with acute myocardial infarction (32). In an observational study, performed in a large cohort of diabetic patients with established coronary disease, the 5 year mortality was 18% in aspirin users and 26% in non-aspirin users compared with 9% and 13% in non-diabetics respectively (33). The absolute benefit of aspirin in patients with coronary disease was greater in diabetic patients than in non diabetics.
LDL Lowering:
The importance of LDL lowering in reducing mortality in secondary prevention trials is well established (34-36). Hypertriglyceridemia and low levels of high-density lipoprotein are the most common lipid abnormalities in diabetes mellitus. In Type I diabetes these abnormalities may be reversed with glycemic control however in Type II diabetes, abnormalities commonly persist even after optimal glycemic control has been achieved. Among survivors of myocardial infarction even patients with impaired fasting glucose have a higher risk of recurrent coronary events (coronary heart disease death, non fatal myocardial infarction, coronary artery bypass graft surgery and PTCA) that can be substantially reduced by effective LDL lowering (37).
In the 4S Study of patients with angina or a history of myocardial infarction, over a 5.4 year follow up, LDL lowering produced mean changes in serum lipids in diabetic patients similar to those observed in non-diabetic patients (38). Importantly, the relative risk of
7

dying was reduced more in diabetics (0.57 for diabetics versus 0.71 for others). [Figure 5]. These results strongly suggest that the absolute clinical benefit achieved by cholesterol lowering may be greater in diabetic patients with coronary heart disease since they have a higher absolute risk of recurrent coronary events (38).
Figure 5.
0.8
0.7
0.6
0.5
RR 0.4
0.3
0.2
4S - INFLUENCE OF LDL LOWERING ON EVENTS OVER 5.4 YEARS
0.1 04,242 Treated Non Diabetics
0 ~.---~~~2~0~2~T~r~e~a~t~e~d~D~ia~b~e~t~ic~s~-----Mortality Major CH D Events
Pyorala et al : Diabetes Care 1997: 20:614
In the CARE study of myocardial infarction survivors (a secondary prevention LDL lowering study of patients with baseline LDL cholesterol 136 mg/dl, HDL cholesterol 38 mg/dl, and triglycerides 164 mg/dl) both the diabetic patients and the patients with impaired fasting glucose (110-125 mg/dl) had a higher rate of recurrent coronary events during 5-year follow up (35). In the placebo group, the diabetic patients suffered more recurrent coronary events than did the non-diabetic patients (37% versus 25%) and LDL lowering reduced the absolute risk of coronary events for diabetic and non-diabetic patients by 8.1% and 5.2% respectively. In those patients with impaired fasting blood glucose in CARE recurrent coronary event rates tended to be lower in the patients randomized to LDL lowering with Pravastatin (37).
Last, in a prospective, examination of the cost-effectiveness of lipid-lowering in patients with diabetes effective LDL lowering reduced hospitalizations for cardiovascular problems (39). The resulting substantial hospital cost savings offset the drug cost and showed a favorable cost-effectiveness ratio.
8

ACE Inhibitors
In a retrospective analysis of the GISSI-III (18,895 patients with suspected acute myocardial infarction who were randomized to treatment with Lisinopril (2.5-10 mg a day), with, or without nitroglycerin, within the frrst 24 hours of infarction and continued for 6 weeks) 15% of the patients had a history of diabetes (40).
Figure 6.
GISSI- 3: INFLUENCE OF LISINOPRIL, INITIATED IN 1st 24 HOURS OF ACUTE Ml, ON MORTALITY
1 8 DNonDiabetic
1 6
1 4
1 2
1 0 %
8
6
4
2
0 Control Lisinopril Control Lisinopril
Zuanetti et al. Circulation 1997:96: 4239
Treatment with Lisinopril was associated with a reduced 6-week mortality in diabetic patients (8.7% versus 12.4%, OR = 0.68) an effect that was significantly greater (P < 0.025) than observed in non-diabetic patients. The survival benefit in diabetics was maintained at 6 months even though treatment was withdrawn at 6 weeks (40). [Figure 6]. In a retrospective analysis of the TRACE Study (41), (a randomized, double-blind, placebo-control trial of Trandolapril, 1-4 mg a day, in 1,749 patients with acute myocardial infarction and ejection fractions less than 36%) in the diabetics the ACE inhibitor resulted in a reduced relative risk of death from any cause of 0.64 compared with 0.82 for non-diabetics. In addition, in diabetics the ACE inhibitor markedly reduced progression to severe heart failure (relative risk 0.38) when no significant reduction of this end point was found in non-diabetics.
Recently, the beneficial effects of an ACE inhibitor (Ramipril, 10 mg once per day) in patients who had evidence of vascular disease or diabetes (plus one other cardiovascular risk factor in the absence of a low ejection fraction or heart failure) were demonstrated over a follow up period of 5 years (42). A total of 9,297 high-risk patients (55 years or
9

older) were randomized to placebo or Ramipril. The primary outcome was a composite of myocardial infarction, stroke, or death from cardiovascular causes. Treatment with Ramipril reduced the rates of death from cardiovascular causes (6.1% versus 8.1%), myocardial infarction (9.9% versus 12.3% ), stroke (3.4% versus 4.9% ), and death from any cause (10.4% versus 12.2% ). Complications related to diabetes were also reduced (6.4% versus 7.6%, RR, 0.84, P = 0.03) and diabetic nephropathy (defmed as urinary albumin excretion of at least 300 mg per day or urinary protein excretion of 500 mg per day), the need for renal dialysis, and the need for laser therapy for diabetic retinopathy were all reduced. In addition, a new diagnosis of diabetes was seen in fewer patients taking Ramipril (3.6% versus 5.4%, P =less than 0.001) (42). The beneficial effect of ACE inhibition was seen regardless of the presence or absence of cardiovascular disease, diabetes, age, gender, presence of hypertension, history of coronary artery disease, history of cerebrovascular disease, peripheral vascular disease and microalbuminuria. It was estimated that treating 1000 patients with Ramipril for 4 years prevented about 150 events in approximately 70 patients. There are a number of potential mechanisms by which ACE inhibitors might benefit diabetics including improved insulin sensitivity and a decrease in hepatic clearance of insulin. These results are consistent with the results of the Captopril Prevention Project ( hypertensive patients randomly assigned to Captopril or conventional treatment of thiazides and beta-blockers and followed for 6.1 years) which also found a reduced incidence of newly diagnosed diabetes in patients who were randomly assigned to receive Captopril ( 43). While ACE inhibitors are known to preserve renal function and reduce albuminuria in diabetics and non-diabetics they have also recently been shown to improve NO-dependent endothelial function in the forearm of Type II diabetic subjects without evidence of vascular disease ( 44 ).
Beta-Blockers
Mortality Reductions (compared with placebo) with Post- Ml Beta- Blockers
50
45
40
35
30
% 25 Nondiabetic
llllil Diabetic 20
15
1 0
5
0-""""'---Early Therapy Long Term
Kendall et al. Ann Intern Med 1995:123 :358
10

Beta blockers may theoretically inhibit catecholamine-induced glycogenolysis and glucose mobilization and prolong an episode of hypoglycemia in patients with diabetes. They may also mask tachycardia that is characteristic of the hypoglycemic state. These effects have been seen with agents such as Propranolol but are less likely to occur with cardio selective agents. After acute myocardial infarction the pooled results of the effect of beta-blocker therapy on mortality and reinfarction in patients with, and without, diabetes (compared with placebo) indicate that diabetic patients, compared with nondiabetic patients, have increased benefits of therapy ( 45), [Figure 7].
In a retrospective, cohort study data abstracted from the medical records of Medicare beneficiaries admitted to hospital with acute myocardial infarction ( 1994-1995) out of 45,308 patients without contraindications to beta-blocker therapy, 7.4% were insulin treated diabetics and 18.5% were non-insulin treated diabetics (46). Beta-blockers were prescribed at discharge for 45% of insulin-treated diabetics, 48% of non-insulin treated diabetics and 51% of non-diabetics. After adjusting for confounding factors beta blockers were associated with lower one year mortality for insulin treated diabetics (hazard ratio = 0.87), non-insulin-treated diabetics (hazard ratio 0.77) and non diabetics (hazard ratio= 0.87). Beta-blockers were not shown to increase diabetic complications in this cohort (46). In a data base study of 14,417 patients with chronic coronary artery disease 19% had non insulin-dependent diabetes. Over a three year period 2/3 of the patients received beta blockers. Mortality was 7.8% in those taking beta blockers compared with 14% in those who were not. Multivariate analysis identified beta-blocker therapy as a significant, independent contributor to improved survival (relative risk = 0.58). The main benefit appeared to be in older patients particularly those with a history of prior myocardial infarction (47).
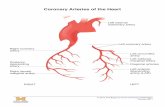
Coronary angiography
In diabetic patients with "normal" coronary arteries the arteries and their branches, as assessed by coronary angiography, appear to have a smaller diameter than "normal" nondiabetic coronary arteries (48). In addition, in a large cohort of patients undergoing angiography after lytic therapy, diabetics had a significantly narrower "normal" reference segment of the coronary arteries than non-diabetic patients, suggesting more extensive, non angiographically identifiable epicardial coronary artery disease (22). In general, diabetic patients presenting with acute coronary syndromes are older, have more prior myocardial infarction, and therefore worse left ventricular function (21). However, even in patient groups matched by age, sex, weight and classic risk factors, ( 49) or, in large populations of patients of similar age and gender, (50) diabetic patients are more likely to have multivessel coronary artery disease.
Percutaneous transluminal coronary angioplasty, CPTCA)
In the mid 1990s attention was drawn to the results of coronary angioplasty in diabetic patients. In an NHLBI Registry Study (1985-1986) of 281 diabetic and 1833 non-
11

diabetic patients undergoing PTCA there was a similar, high probability of initial angiographic success, but 9 year event-free survival was reduced in diabetic patients (51), [Figure 8] . Similarly, in an Emory University study, 1,133 diabetic and 9,300 non diabetic patients undergoing elective PTCA ( 1980-1990) were analyzed. In diabetics the 5 year survival was lower (89% versus 93%), freedom from myocardial infarction was lower (81% versus 89% ), and subsequent revascularization was required more often (52). Diabetics appear to have a higher rate of infarction and a greater need for additional revascularization after PTCA presumably because of increased early restenosis and accelerated progression of coronary disease.
%
Figure 8.
45
40
35
30
25
20
NHLBI PTCA Registry 1985-1986 9 Year Follow up
DNonDiabetlc
M ortallty NonFata l Ml CABG PTCA
Kip et al, Circulation 1996: 94 :1818
In a relatively small study of 376 consecutive patients presenting with non-Q-wave myocardial infarction (53) and treated with PTCA during hospitalization (80% non diabetics and 20% diabetics) success rates for diabetics and non diabetics were similar (96 versus 97% ), in hospital complications were the same and one year survival was similar (92% versus 94% ). However, survival free of events (PTCA, CABO, MI and death) was worse in diabetics (55% versus 67% ).
PTCA carries an increased risk of platelet aggregation and thrombotic complications which should be prevented by blocking the platelet glycoprotein lib/lila receptor and thus reducing adhesion and aggregation of platelets. In 1997 the CAPTURE Study (54) examined the influence of a lib/lila inhibitor (Abciximab) before, and during, coronary intervention in patients with refractory unstable angina. The rate of myocardial infarction was reduced by the lib/lila inhibitor before, during, and for a few days after PTCA. Major bleeding was infrequent but occurred more often with the treatment than with placebo (3.8% versus 1.9%). To determine whether treatment with lib/lila glycoprotein receptor blockers was also effective in reducing complications after PTCA in diabetics the outcome in 638 diabetic patients, of a total of 2792 patients enrolled in the EPILOG Study, was examined (55). Abciximab treatment reduced death, or myocardial infarction, among diabetic and non diabetic patients at 30 days (respective hazard ratios 0.28 and
12

0.47) and at six months. Target vessel revascularization during follow up was reduced among non diabetic patients but not among diabetic patients. Thus, lib/lila receptor blocker treatment in diabetics reduced morbid and fatal events at least as much as in nondiabetics but the need for target vessel revascularization was not reduced in diabetics but was reduced in non-diabetics.
Van Belle et al ( 1997) analyzed the effect of diabetes on coronary artery restenosis in 600 patients who were enrolled in a six month angiographic follow up study (56).
USE OF PTCA +/- STENTS 6 months Angiographic follow up
80
70
60
50 IA--- - ----1
PTCA PTCA · Diabetes s tent Stent·D labetes
VanBelle et al. Circulation 1997: 96:1454
Figure 9.
Patients were treated with either PTCA alone, or PTCA and coronary stenting. In the PTCA group (control group) the restenosis rate was almost doubled in diabetic patients (63% versus 36%) because of greater late diameter loss and a higher rate of late vessel occlusion (14% versus 3%). In the group treated with PTCA and stents the restenosis rates were similar in diabetics and non-diabetics (25% versus 27%) and the late diameter loss and rate of late vessel occlusion did not differ significantly. ( Figure 9). Therefore, while the use of PTCA and stents in diabetic patients (compared to PTCA alone) reduced restenosis during six month follow up the late diameter loss of the coronary vessels was seen in approximately 80% of all patients who had stents implanted. A subsequent study by the EPISTENT Investigators (57) showed that the combination of stenting and lib/lila receptor blockade (Abciximab) among diabetics resulted in a significant reduction in 6 month events (death, myocardial infarction, and target-vessel revascularization) compared with patients treated with stent alone or patients treated with balloon angioplasty and Ilb/llla blockade (without stents).
13

Importantly, diabetics appear to have more events than non diabetics after coronary artery stenting (58). In a consecutive series of patients treated with PTCA and stent placement (2,839 non-diabetics and 715 diabetics) the diabetics suffered more events during one year of follow up (death, myocardial infarction and target lesion revascularization), they were more likely to have myocardial infarction, coronary artery restenosis (37.5% versus 28.3%) and stent vessel occlusion (5.3% versus 3.4%), [Figure 10].
40
35
% 30
25
20
15
10
5
0
Figure 10.
EVENTS AFTER CORONARY ARTERY STENTING
Events= Death, Ml, Revascularization
Events 1yr Mlln 1yr Restenosis Occlusion
Elezi et al. JACC 1998: 32:1866
In a multivariate analysis diabetes was identified as an independent risk factor for adverse clinical events and restenosis after PTCA and stent implantation (58).
Coronary artery bypass graft surgery (CABG)
Coronary artery surgery is performed commonly in diabetics and particularly in patients with multivessel coronary artery disease may be the preferred revascularization technique. In a major, prospective, randomized comparison of revascularization by PTCA or CABG in patients with multivessel coronary artery disease, ( BARI =Bypass Angioplasty Revascularization Investigation ), an initial strategy of PTCA did not increase 5-year all-cause mortality, although subsequent revascularization was required more often after PTCA (59), [Figure 11]. It was noted, in patients with diabetes mellitus (353 of 1,829 patients, 19%) being treated with oral hypoglycemic agents or insulin (a subgroup not specified by the protocol), the 5 year survival was 80.6% with CABG and 65.5% with PTCA (P= 0.003) (59-62). Diabetics had less favorable baseline characteristics than other patients but the process of randomization distributed the patients evenly to the CABG and PTCA treatments. Better survival after CABG was due to reduced cardiac mortality (5.8% versus 20.6%, P = 0.0003) which was confined to those patients receiving at least one internal mammary artery graft (61). Subsequent analyses showed there were no significant differences in cardiac mortality rates, or myocardial infarction risks, in non diabetic patients with multivessel coronary artery
14

disease in BARI treated by either PTCA or CABG (63) . However, diabetic patients with multivessel disease had increased cardiac mortality rates after an initial treatment strategy of PTCA compared with CABG. The difference was manifest in diabetic patients on drug therapy. In a further registry study (patients who were eligible for the BARI trial but were not randomized and therefore underwent CABG or PTCA by choice
%
90
80
70
60
50
40
30
20
10
BARI : Bypass Angioplasty Revascularization Investigation
OPTCA (N=915) ~CABG (N=914)
o ~----
* p < 0.01
Figure 11.
Survival Repeat Revasc Diabetes Survival
N Engl J Med 1996 :335:217
of the physician rather than random assignment) the results were consistent with the findings in the randomized trial (60). In the randomized trial diabetics taking insulin, rather than oral hypoglycemic agents, appeared to have a greater cumulative survival advantage with revascularization by CABG (60). This suggests a dose-response treatment difference between CABG and PTCA that increases with the severity of diabetes. In another study (64) looking at long-term survival in diabetic patients following first-time revascularization by CABG or PTCA the overa1110 year survival for diabetics was better after CABG (60%) than PTCA (46%), (P < 0.0001) . In this study, the risk adjusted survival advantage conferred by CABG was strongest for patients receiving oral agents (75% versus 62%), and less for diet (84% versus 81 %), and insulintreated diabetics (63% versus 64% ). Incomplete revascularization and sulfonylurea therapy worsened outcome after PTCA and the use of left internal mammary artery grafts improved outcome after bypass surgery (64).
In further BARI Study analyses among patients with diabetes, revascularization by CABG as compared with PTCA had a highly favorable influence on prognosis after
15

ADA Consensus Conlerence Suggestions lor Cardiac Stress Testing
! ' ~· i ! '/ 11p1VIIIUIIV 1.1
! I
I I I
ECG shows Ml or isc hemia Vascular disease or One or !ewer risk !actors and norm al ECG starting exercise program or
2 or more risk !actors or Minor ECG changes
I I I 1 C:tro•· ~ o rJusion imaging or echo 1 l~ular exercise stress test I
,.,.,........_,.~H>'>--'~...,.><W-I<V-'»-~ L_~.,-~~utine lollow up I
subsequent acute myocardial infarction (65). Last, in the BARI Study, at 7 years there was a statistically significant survival advantage for patients randomized to CABG (84.4%) compared with PTCA (80.9%, p = 0.043). This difference could be explained by the 353 patients with treated diabetes mellitus for whom estimates of 7 year survival with CABG were 76.4% and with PTCA 55.7% (p = 0.0011). Among non-diabetic patients, there was essentially no difference in survival (66).
Diagnosis of coronary artery disease
In diabetics coronary artery disease occurs prematurely, is often more extensive at the time of diagnosis, and is associated with a higher morbidity and mortality after myocardial infarction. In my opinion, because of the adverse prognostic implications of diabetes with respect to coronary artery disease in particular, and vascular disease in general, and the demonstrable benefits of medical and revascularization therapy, the diagnosis of diabetes even in the absence of known coronary artery disease, should trigger initiation of a vigorous "secondary prevention program" with goals similar to patients who have known coronary artery disease. This includes the prophylactic use of aspirin, aggressive lipidlowering strategies aiming to achieve LDL lowering below 100 mg/dl, the appropriate use of beta-blockers, the aggressive control of hypertension, and the use of ACE
16

inhibitors as a first line treatment of hypertension and proteinuria. It is also important to identify diabetic patients in whom coronary artery revascularization is appropriate.
Stress testing to identify coronary artery disease is warranted in diabetic patients with the following "risk factors":
1. Typical or atypical cardiac symptoms 2. A resting electrocardiogram suggestive of ischemia or infarction. 3. Peripheral or carotid occlusive arterial disease. 4. Sedentary lifestyle, age 35 years, and plans to begin exercise program. 5. No symptoms but two or more of the following five risk factors:
a. Total cholesterol 240 mg/dl, LDL cholesterol 160 mg/dl or HDL cholesterol less than 35 mg/ dl.
b. Blood pressure greater than 140/90. c. Smoker. d. Family history of premature coronary artery disease. e. Positive micro-macro albuminuria test.
Asymptomatic patients with diabetes and one, or fewer, risk factor( s) and a normal electrocardiogram do not require cardiac testing
When initial stress testing is performed in an asymptomatic diabetic patient the type of follow up depends on the pre-test risk and the degree of stress test abnormality.
Pre-Test Risk
High 4-5 "Risk
Moderate 2-3 "Risk
Low 0-1 "Risk Factor"
Screening Stress Testing Results
Normal
17

A suggested routine follow up would include annual re-evaluation of symptoms and signs of coronary artery disease and an electrocardiogram. A repeat stress test could be considered in 3 to 5 years if the clinical status is unchanged. Closer follow up would imply shorter intervals between evaluation and a follow up exercise test every 1 or 2 years (1).
References
1. Consensus development conference on the diagnosis of coronary heart disease in people with diabetes: 10-11 February 1998, Miami, Florida. American Diabetes Association. Diabetes Care 1998;21(9): 1551-9.
2. A Joint Editorial Statement by the American Diabetes Association; the National Heart L, and Blood Institute; the Juvenile Diabetes Foundation International; the National Institute of Diabetes and Digestive and Kidney Diseases; and the American Heart Association,. Diabetes Mellitus: A Major Risk Factor for Cardiovascular Disease. Circulation 1999;100: 1132-1133.
3. Herlitz J, Karlson BW, Edvardsson N, Emanuelsson H, Hjalmarson A. Prognosis in diabetics with chest pain or other symptoms suggestive of acute myocardial infarction. Cardiology 1992;80(3-4):237-45.
4. Karlson BW, Strombom U, Ekvall HE, Herlitz J. Prognosis in diabetics in whom the initial suspicion of acute myocardial infarction was not confrrmed. Clin Cardiol 1993; 16(7):559-64.
5. Fava S, Azzopardi J, Agius-Muscat H. Outcome of unstable angina in patients with diabetes mellitus. Diabet Med 1997;14(3):209-13.
6. Miettinen H, Lehto S, Salomaa V, et al. Impact of diabetes on mortality after the first myocardial infarction. The FINMONICA Myocardial Infarction Register Study Group, Diabetes Care 1998;21(1):69-75.
7. Zuanetti G, Latini R, Maggioni AP, Santoro L, Franzosi MG. Influence of diabetes on mortality in acute myocardial infarction: data from the GISSI-2 study. JAm Coli Cardiol 1993 ;22(7): 1788-94.
8. Merrilees MA, Scott PJ, Norris RM. Prognosis after myocardial infarction: results of 15 year follow up. BMJ 1984;288:356-359.
9. Lee KL, WoodliefLH, TopolEJ, et al. Predictors of30-day mortality in the era of reperfusion for acute myocardial infarction. Circulation 1995;91:1659-1668.
18

10. Hillis L, Forman S, Braunwald E, and the Thrombolysis in Myocardial Infarction (TIMI) Phase II Co-Investigators. Risk Stratification Before Thrombolytic Therapy in Patients with Acute MI. Journal of the American College of Cardiology 1990;16:313-315.
11. Behar S, Boyko V, Reicher-Reiss H, Goldbourt U. Ten-year survival after acute myocardial infarction: comparison of patients with and without diabetes. SPRINT Study Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. Am Heart J 1997; 133(3):290-6.
12. Walters DP, Gatling W, Houston AC, Mullee MA, Julious SA, Hill RD. Mortality in diabetic subjects: an eleven-year follow-up of a community-based population. Diabet Med 1994;11(10):968-73.
13. Miettinen H, Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Proteinuria predicts stroke and other atherosclerotic vascular disease events in nondiabetic and non-insulin-dependent diabetic subjects. Stroke 1996;27:2033-2039.
14. Delcourt C, Vauzelle-Kervroedan F, Cathelineau G, Papoz L. Low prevalence of long-term complications in non-insulin-dependent diabetes mellitus in France: a multicenter study. J Diabetes Complications 1998;12(2):88-95.
15. Marso SP, Ellis SG, Tuzcu M, et al. The importance of proteinuria as a determinant of mortality following percutaneous coronary revascularization in diabetics. Journal of the American College of Cardiology 1999;33(5):1269-77.
16. Fava S, Azzopardi J, Muscat HA, Fenech FF. Factors that influence outcome in diabetic subjects with myocardial infarction. Diabetes Care 1993;16(12):1615-8.
17. Lloyd CE, Becker D, Ellis D, Orchard TJ. Incidence of complications in insulin-dependent diabetes mellitus: a survival analysis. Am J Epidemiol1996;143(5):431-41.
18. Miettinen H, Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Retinopathy predicts coronary heart disease events in NIDDM patients. Diabetes Care 1996;19(12): 1445-8.
19. Akasaka T, Yoshida K, Hozumi T, et al. Retinopathy identifies marked restriction of coronary flow reserve in patients with diabetes mellitus. J Am Coll Cardiol 1997;30(4):935-41.
20. Lunetta M, Infantone L, Calogero AE, lnfantone E. Increased urinary albumin excretion is a marker of risk for retinopathy and coronary heart disease in patients with type 2 diabetes mellitus. Diabetes Research & Clinical Practice 1998;40(1):45-51.
19

21. Fibrinolytic Therapy Trialists'(FTT) Collaborative Group. Indications for Fibrinolytic Therapy in Suspected Acute Myocardial Infarction: Collaborative Overview of Mortality and Major Morbidity Results From All Randomised Trials of More Than 1000 Patients. Lancet 1994;343:311-322.
22. Woodfield SL, Lundergan CF, Reiner JS, et al. Angiographic findings and outcome in diabetic patients treated with thrombolytic therapy for acute myocardial infarction: the GUSTO-I experience. J Am Coli Cardiol 1996;28(7): 1661-9.
23. Mak KH, Moliterno DJ, Granger CB, et al. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction. GUSTO-I Investigators. Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries. JAm Coli Cardiol1997;30(1):171-9.
24. Shotliff K, Kaushal R, Dove D, Nussey SS. Withholding thrombolysis in patients with diabetes mellitus and acute myocardial infarction. Diabet Med 1998;15(12):1028-30.
25. Mahaffey KW, Granger CB, Toth CA, et al. Diabetic retinopathy should not be a contraindication to thrombolytic therapy for acute myocardial infarction: review of ocular hemorrhage incidence and location in the GUSTO-I trial. Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries. J Am Coli Cardiol 1997 ;30(7): 1606-10.
26. Malmberg K, Ryden L, Efendic S, et al. Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year. JACC 1995;26(1):57-65.
27. Malmberg K, Ryden L, Hamsten A, Herlitz J, Waldenstrom A, Wedel H. Effects of insulin treatment on cause-specific one-year mortality and morbidity in diabetic patients with acute myocardial infarction. DIGAMI Study Group. Diabetes InsulinGlucose in Acute Myocardial Infarction. European Heart Journal1996;17(9):1337-44.
28. Malmberg K, Ryden L, Hamsten A, Herlitz J, Waldenstrom A, Wedel H. Mortality prediction in diabetic patients with myocardial infarction: experiences from the DIGAMI study. Cardiovasc Res 1997;34(1):248-53.
29. Malmberg K. Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. DIGAMI (Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction) Study Group. Bmj 1997;314(7093):1512-5.
30. Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes
20

and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation 1999;99(20):2626-32.
31. Almbrand B, Johannessen M, Sjostrand B, Malmberg K, Ryden L. Costeffectiveness of intense insulin treatment after acute myocardial infarction in patients with diabetes mellitus; results from the DIGAMI study. European Heart Journal 2000;21(9):733-9.
32. Zuanetti G, Latini R. Impact of pharmacological treatment on mortality after myocardial infarction in diabetic patients. J Diabetes Complications 1997; 11 (2): 131-6.
33. Harpaz D, Gottlieb S, Graff E, Boyko V, Kishon Y, Behar S. Effects of aspirin treatment on survival in non-insulin-dependent diabetic patients with coronary artery disease. Israeli Bezafibrate Infarction Prevention Study Group. Am J Med 1998;105(6):494-9.
34. Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study ( 4S). Lancet 1994;344: 1383-89.
35. Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Theroux P, Warnica JW, Arnold MO, Nash DT, Wun C-C, Davis BR, Hawkins CM, Braunwald E, for the Cholesterol and Recurrent Events (CARE) Trial Investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med 1996;335(14):1001-1009.
36. LIPID Study Group, Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 1998;339(19):1349-1357.
37. Goldberg RB, Mellies MJ, Sacks FM, et al. Cardiovascular events and their reduction with pravastatin in diabetic and glucose-intolerant myocardial infarction survivors with average cholesterol levels: subgroup analyses in the cholesterol and recurrent events (CARE) trial. The Care Investigators. Circulation 1998;98(23):2513-9.
38. Pyorala K, Pedersen TR, Kjekshus J, Faergeman 0, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997;20(4):614-20.
39. Jonsson B, Cook JR, Pedersen TR. The cost-effectiveness of lipid lowering in patients with diabetes: results from the 4S trial. Diabetologia 1999;42(11): 1293-301.
40. Zuanetti G, Latini R, Maggioni AP, Franzosi M, Santoro L, Tognoni G. Effect of the ACE inhibitor lisinopril on mortality in diabetic patients with acute myocardial infarction: data from the GISSI-3 study. Circulation 1997;96(12):4239-45.
21

41. Gustafsson I, Torp-Pedersen C, Kober L, Gustafsson F, Hildebrandt P. Effect of the angiotensin-converting enzyme inhibitor trandolapril on mortality and morbidity in diabetic patients with left ventricular dysfunction after acute myocardial infarction. JACC 1999;34(1):83-89.
42. The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an Angiotensin-Converting-Enzyme Inhibitor, Ramipril, on Cardiovascular Events in HighRisk Patients. N Engl J Med 2000;342: 145-53.
43. Hansson L, Lindholm LH, Niskanen L, et al. Effect of angiotensin-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet 1999;353:611-16.
44. O'Driscoll GO, Green D, Maiorana A, Stanton K, Colreavy F, Taylor R. Improvement in endothelial function by angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus. JACC 1999;33(6): 1506-1511.
45. Kendall MJ, Lynch KP, Hjalmarson A, Kjekshus J. B-blockers and Sudden Cardiac Death. Ann Intern Med 1995;123:358-367.
46. Chen J, Marciniak TA, Radford MJ, Wang Y, Krumholz HM. Beta-blocker therapy for secondary prevention of myocardial infarction in elderly diabetic patients. Results from the national cooperative cardiovascular project. JACC 1999;34(5): 1388-1394.
47. Jonas M, Reicher-Reiss H, Boyko V, et al. Usefulness of beta-blocker therapy in patients with non-insulin-dependent diabetes mellitus and coronary artery disease. Bezafibrate Infarction Prevention (BIP) Study Group. Am J Cardiol 1996;77 (15): 1273-7.
48. Mosseri M, Nahir M, Rozenman Y, et al. Diffuse narrowing of coronary arteries in diabetic patients: the earliest phase of coronary artery disease. Cardiology 1998;89(2): 103-10.
49. Melidonis A, Dimopoulos V, Lempidakis E, et al. Angiographic study of coronary artery disease in diabetic patients in comparison with nondiabetic patients. Angiology 1999;50(12):997-1006.
50. Lindvall B, Brorsson B, Herlitz J, Albertsson P, Werko L. Comparison of diabetic and non-diabetic patients referred for coronary angiography. International Journal of Cardiology 1999;70(1):33-42.
51. Kip KE, Faxon DP, Detre KM, Yeh W, Kelsey SF, Currier JW. Coronary angioplasty in diabetic patients. The National Heart, Lung, and Blood Institute
22

Percutaneous Transluminal Coronary Angioplasty Registry. Circulation 1996;94(8): 1818-25.
52. Stein B, Weintraub WS, Gebhart SP, et al. Influence of diabetes mellitus on early and late outcome after percutaneous transluminal coronary angioplasty. Circulation 1995;91( 4):979-89.
53. Gowda MS, Vacek JL, Hallas D. One-year outcomes of diabetic versus nondiabetic patients with non-Q-wave acute myocardial infarction treated with percutaneous transluminal coronary angioplasty. Am J Cardiol1998;81(9):1067-71.
54. Randomised placebo-controlled trial of abciximab before and during coronary intervention in refractory unstable angina: the CAPTURE Study. Lancet 1997;349(9063): 1429-35.
55. Kleiman NS, Lincoff AM, Kereiakes DJ, et al. Diabetes mellitus, glycoprotein lib/lila blockade, and heparin: evidence for a complex interaction in a multicenter trial. EPILOG Investigators. Circulation 1998;97(19): 1912-20.
56. Van Belle E, Bauters C, Hubert E, et al. Restenosis rates in diabetic patients: a comparison of coronary stenting and balloon angioplasty in native coronary vessels [see comments]. Circulation 1997 ;96( 5): 1454-60.
57. Marso SP, Lincoff AM, Ellis SG, et al. Optimizing the percutaneous interventional outcomes for patients with diabetes mellitus: results of the EPISTENT (Evaluation of platelet lib/lila inhibitor for stenting trial) diabetic substudy. Circulation 1999;100(25):2477-84.
58. Elezi S, Kastrati A, Pache J, et al. Diabetes mellitus and the clinical and angiographic outcome after coronary stent placement. J Am Coli Cardiol 1998;32(7): 1866-73.
59. The bypass angioplasy revascularization investigation (BARI) investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med 1996;335:217-25.
60. Detre KM, Gui P, Holubkov R, et al. Coronary revascularization in diabetic patients. A comparison of the randomized and observational components of the bypass angioplasty revascularization investigation (BARI). Circulation 1999;99(5):633-640.
61. The BARI Investigators. Influence of Diabetes on 5-year Mortality and Morbidity in a Randomized Trial Comparing CABG and PTCA in Patients with Multivessel Disease. Circulation 1997;96:1761-1769.
23

62. Barsness GW, Peterson ED, Ohman EM, et al. Relationship between diabetes mellitus and long-term survival after coronary bypass and angioplasty. Circulation 1997 ;96(8) :2551-6.
63. Chaitman BR, Rosen AD, Williams DO, et al. Myocardial Infarction and Cardiac Mortality in the Bypass Angioplasty Revascularization Investigation (BARI) Randomized Trial. Circulation 1997;96:2162-2170.
64. O'Keefe JH, Blackstone EH, Sergeant P, McCallister BD. The optimal mode of coronary revascularization for diabetics. A risk-adjusted long-term study comparing coronary angioplasty and coronary bypass surgery. European Heart Journal 1998;19(11): 1696-703.
65. Detre KM, Lombardero MS, Brooks MM, et al. The effect of previous coronaryartery bypass surgery on the prognosis of patients with diabetes who have acute myocardial infarction. Bypass Angioplasty Revascularization Investigation Investigators . N Engl J Med 2000;342(14):989-97.
66. Seven-year outcome in the Bypass Angioplasty Revascularization Investigation (BARI) by treatment and diabetic status, JACC 2000;35(5):1122-9.
24