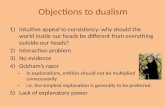
Zimmerman - From Property Dualism to Substance Dualism (Published in PAS)
Diabetes and Cartesian Dualism: what is the evidence … · block or attenuate many neuro-endocrine...
Transcript of Diabetes and Cartesian Dualism: what is the evidence … · block or attenuate many neuro-endocrine...
Ever since Claude Bernard inserted a knitting needleinto the brain of a cat in 1854 there has been aninterest in the part that the brain has to play in
diabetes. The renowned physiologist discovered that bypuncturing the floor of the fourth cerebral ventricle oflaboratory animals they developed diabetes mellitus(‘piqûre diabétique’), thus linking glucose homeostasisand the brain to the pathogenesis of diabetes.1
The discovery of insulin in 1921 rather spoilt this lineof research, and scientists and clinicians subsequentlybecame overly focused on defective insulin secretion and action, meaning that the pancreatic islet cell over-shadowed the brain as the centre of our understandingof diabetes and the target for therapeutic intervention.The problem with this approach is that it serves to control rather than cure the disease.2
Insulin-independent mechanisms account forapproximately 50% of overall glucose disposal, but weknow very little about them. Sometimes described as‘glucose effectiveness’, there is a growing research bodywhich suggests that the brain is in control of dynamicallyregulating the process of glucose control in order toimprove and normalise dysglycaemia. Indeed, defects insuch mechanisms are postulated as contributory causesto the emergence of diabetes, an example of which wasoutlined in a recent leader in this journal ‘Type 3Diabetes’ on the relationship between Alzheimer’s anddiabetes.3 What then is the evidence for a brain-centredgluco-regulatory system (BCGS)?
Thinking about diabetesThere is a growing research literature establishing therole of the brain in glucose homeostasis. This can be asa direct effect of insulin action – injection of insulin intodiscrete hypothalamic areas can lower blood glucose levels and increase liver insulin sensitivity,4 and this hasbeen confirmed by deletion of hypothalamic insulinreceptors causing glucose intolerance and systemicinsulin resistance.5 On the other hand, it has recentlybecome clear that there are insulin-independent mech-anisms through which the brain influences glycaemiccontrol. For example, there have been several animalmodels demonstrating the effects of leptin acting cen-trally to normalise blood glucose even in the context ofsevere insulin deficiency. Leptin action in the brain cancoordinate several complex and connected processesbetween different tissue types to lower blood glucosedespite the absence of insulin signalling.6,7
In clinical practice, physiological leptin infusion canblock or attenuate many neuro-endocrine responsesinduced by insulin deficient diabetes; however, it does notnormalise hyperglycaemia. If exogenous leptin can acti-vate the BCGS why is this the case? The likely answer is thatthere is an extensive overlap between the peripheral and
central gluco-regulatory mechanisms. Insulin deficiencyhas marked effects on adipose tissue and thus its ability tosecrete leptin. It is therefore believed that insulin deficiency leads to leptin deficiency and failure to triggerthe BCGS as neither insulin nor leptin are able to work onthe brain.
Other hormones, such as FGF-19 (fibroblast growthfactor), a gut hormone which is secreted in response to meals, have been shown to act in the brain to pro-mote insulin-independent glucose lowering.8 There are multiple FGF receptor sub-types throughout the cere-bral cortex.9 When administered at pharmacologicaldoses it has strong antidiabetic effects. If given to obeserats via an intra-cerebroventricular route, FGF-19 cansignificantly improve glucose tolerance.
GLP-1 and GIP are both gut hormones as well asneuro-peptides. We know that GLP-1 therapy workspartly by enhancing insulin secretion, but it also works toimprove glucose tolerance through mechanisms ofinsulin-independent action that are incompletely under-stood. Several studies have shown how GLP-1 can havecentral effects other than those relating to blood glu-cose, such as appetite suppression and improvements in mood and quality of life factors.10 GLP-1 action in thehypothalamic accurate nucleus improves glucose toler-ance through centrally-acting mechanisms similar to leptin and FGF-19.
A further example of how signalling mechanismsbetween the gut and the brain are crucial to our under-standing of diabetes comes from the dramatic improve-ments in glycaemic control which occur following bariatricsurgery even before significant weight loss occurs.
Mechanisms underlying the metabolic benefits ofbariatric surgery are not fully understood but mayinvolve improvements in both the BCGS and islet cellfunction. One previous study of diabetic rats undergoingbariatric surgery (duodenal exclusion) showed insulin-independent activation of a neural circuit that inhibitshepatic glucose production (HGP).11 More recent worksuggests that insulin signalling is required in the ventro-medial hypothalamus for the effect of bariatric surgeryto inhibit HGP in obese rats.12,13 There is increasing evidence to suggest that there are strong links betweenenhanced secretion of FGF-19, the central nervous sys-tem and the gut. The potential is therefore to identifyhow bariatric procedures interfere with the BCGS andperhaps induce diabetes remission through this pathway(without having to resort to surgery).
Fundamental interconnectednessIt is possible that the combined response to risingplasma glucose is a rise in insulin concentration, GLP-1,FGF-19 and leptin which activate the BCGS, whichtogether with the traditional pancreatic islet response,
10 PRACTICAL DIABETES VOL. 31 NO. 1 COPYRIGHT © 2014 JOHN WILEY & SONS
Leader
Diabetes and Cartesian Dualism: what is the evidencefor a brain-centred gluco-regulatory system?Paul Grant, Munachiso Nwokolo
PRACTICAL DIABETES VOL. 31 NO. 1 COPYRIGHT © 2014 JOHN WILEY & SONS 11
Leader
contribute to glucose disposal. However, if this is thecase then why has such a relevant regulatory pathway notbeen detected previously? The theory is that the goldstandard method for assessment of in-vivo glucose con-trol is the euglycaemic-hyperglycaemic clamp, throughwhich insulin sensitivity is assessed as the amount of glucose which needs to be infused to maintain stableplasma concentrations, and this ignores the fact thatsome of the exogenous glucose could have been takenup by insulin-independent mechanisms.
Criticisms of the BCGS hypothesis are that althoughbrain directed interventions can affect glucose homeo -stasis this cannot be taken as direct evidence of the brainhaving a physiological role. It is not clear whether thebrain plays a part on a day-to-day basis.
Schwartz et al., from the US and Germany, have thusproposed that diabetes represents a failure of two systems, both the pancreas and the brain. Studies showthat the BCGS can compensate effectively for severeinsulin deficiency, so the suggestion is that additionalfailure of the BCGS needs to take place in order for diabetes to occur.14
• Proper BCGS function depends on normal islet func-tion, relying on insulin and other insulin-dependenthormones, e.g. leptin, or defective in type 2 diabetes,e.g. GLP-1.• Animal models with selective hypothalamic neuronaldamage show an impaired ability to respond to regulateglucose and weight leading to the metabolic syndrome.15
• Whether some form of hypothalamic injury is occur-ring in humans with diabetes is under investigation butthere are some early data to support this possibility.16
SummaryIt is becoming apparent that glucose homeostasis is notentirely reliant on peripheral mechanisms. Metabolicpathways which are insulin-independent are recognisedto play an important part in glucose effectiveness; however, it is unclear as to the extent that the BCGS regulates this. More research work is required to look atto what degree normal blood glucose control dependson a functioning BCGS. In turn, does the aetiology oftype 2 diabetes relate to BCGS dysfunction and, in con-ditions such as Alzheimer’s disease, is the degree of neuronal damage a glucose mediated effect?
Finally, knowledge that hormones such as GLP-1, GIPand FGF-19 act on the brain to improve glucose toler-ance and insulin sensitivity opens up new therapeuticopportunities for treatment targets. In the complex,developing field of diabetes we are still not sure ofwhether the body rules the mind or whether the mindrules the body.
‘And what more am I? I look for aid to the imagination. [Buthow mistakenly!] I am not that assemblage of limbs we call thehuman body; I am not a subtle penetrating air distributedthroughout all these members; I am not a wind, a fire, a vapor,a breath or anything at all that I can image. I am supposing allthese things to be nothing. Yet I find, while so doing, that I amstill assured that I am a something.’
– René Descartes. ‘Meditations on First Philosophy: Inwhich the existence of God and the distinction of thesoul from the body are demonstrated.’
Dr Paul Grant, MRCP, Consultant Diabetologist,Diabetes & Endocrine Day Centre, St Thomas’Hospital, London, UKDr Munachiso Nwokolo, MRCP, Clinical ResearchFellow, Department of Diabetes, King’s CollegeHospital, London, UK
Declaration of interestsThere are no conflicts of interest declared.
References1. Han KW. The formation and background of Claude Bernard’s general physiology.
Uisahak 2010;19(2):507–52.2. Wu YL, et al. Risk factors and primary prevention trials for type 1 diabetes. Int J Biol
Sci 2013;9(7):666–79.3. Shaw K. ‘Type 3 diabetes’: linking a brain insulin-resistant state with dementia and
Alzheimer’s disease. Pract Diabetes 2013;30(3):102–3.4. Khan AM, et al. Neural input is critical for arcuate hypothalamic neurons to mount
intracellular signaling responses to systemic insulin and deoxyglucose challengesin male rats: implications for communication within feeding and metabolic controlnetworks. Endocrinology 2013 Nov 21. [Epub ahead of print.]
5. Jackson HM, et al. Clustering of transcriptional profiles identifies changes to insulinsignaling as an early event in a mouse model of Alzheimer’s disease. BMCGenomics 2013;14(1):831.
6. Kalra SP. Should leptin replace insulin as a lifetime monotherapy for diabetes type1 and 2? Indian J Endocrinol Metab 2013;17(Suppl 1):S23–4.
7. Moullé VS, et al. Lipid sensing in the brain and regulation of energy balance.Diabetes Metab 2013 Nov 6. [Epub ahead of print.]
8. Morton GJ, et al. FGF19 action in the brain induces insulin-independent glucoselowering. J Clin Invest 2013 Oct 1. [Epub ahead of print.]
9. Angelin B, et al. Circulating fibroblast growth factors as metabolic regulators – acritical appraisal. Cell Metab 2012;16(6):693–705.
10. Grant P, et al. Psychological and quality of life changes in patients using GLP-1analogues. J Diabetes Complications 2011;25(4):244–6.
11. Muñoz R, et al. Isolated duodenal exclusion increases energy expenditure andimproves glucose homeostasis in diet-induced obese rats. Am J Physiol RegulIntegr Comp Physiol 2012;303(10):R985–93.
12. Jiao J, et al. Restoration of euglycemia after duodenal bypass surgery is reliant oncentral and peripheral inputs in Zucker fa/fa rats. Diabetes 2013;62(4):1074–83.
13. Cazzo E, et al. Impact of Roux-en-Y Gastric Bypass on Metabolic Syndrome andInsulin Resistance Parameters. Diabetes Technol Ther 2013 Dec 3. [Epub ahead of print.]
14. Schwartz MW, et al. Cooperation between brain and islet in glucose homeostasisand diabetes. Nature 2013;503:59–66.
15. Thaler JP, et al. Obesity is associated with hypothalamic injury in rodents andhumans. J Clin Invest 2012;122:153–62.
16. Cai D. One step from prediabetes to diabetes: hypothalamic inflammation?Endocrinology 2012;153:1010–3.
Visit our websiteThe Practical Diabetes website carries a wide range of additional informationin support of the journal. You can access the current issue online, searchthrough back issues in our archive or download our growing collection ofABCD position statements.Find out more at www.practicaldiabetes.com