Development of a community-based skin integrity service · skin integrity team lead, Norfolk...
Transcript of Development of a community-based skin integrity service · skin integrity team lead, Norfolk...
30 JCN 2019, Vol 33, No 3
SKIN CARE
The authors work as members of a community-based skin integrity team, as dermatology
and tissue viability nurse specialists respectively. The team also consists of one lymphoedema specialist nurse, one support worker, two assistant practitioners (tissue viability), two other dermatology nurses and another tissue viability nurse. The skin integrity team covers a clinical commissioning group (CCG) area including both urban and rural populations totalling around 170,700 people, and has been focusing on the management of patients with lower limb issues in a community setting. Following an audit of the management of patients with oedema of the legs (Sweeney, 2018), this article outlines the development of the team and the benefits that have been seen as a result, including a case study to illustrate collaborative working.
Development of a community-based skin integrity serviceSara Burr, Rachel Sweeney
FORMATION OF THE TEAM
The community nursing services that are provided for the CCG in the area include community and district nurses, assistant practitioners and specialist nurses. Of the specialist nurses, three part-time dermatology, two part-time tissue viability and two lymphoedema nurses all previously worked independently. However, many of the patients they saw would be referred between the three specialities for advice on skin, wound and oedema-related issues. It was recognised that, as the three specialist services overlapped, it would make sense to pool expertise and remodel the way in which they functioned. The creation of a new team was an internal decision to allow clinicians to lead by example by working to respective best practice and sharing practice/knowledge with colleagues, and identify the unique contribution of each specialty for the benefit of individual patients. The team was named the skin integrity team to reflect the fact that maintaining the integrity of the skin is the cornerstone of best practice in all of these specialist areas (Wounds UK, 2018). As a consequence of this collaboration, areas of improvement/change were identified for implementation.
Sara Burr, community dermatology specialist nurse/clinical lead, community skin integrity team, Norfolk Community Health and Care NHS Trust; Rachel Sweeney, tissue viability specialist nurse, skin integrity team lead, Norfolk Community Health and Care NHS Trust
A review of how specialist community nursing services were functioning in a community healthcare trust has led to the development of a skin integrity team. Composed of dermatology, tissue viability and lymphoedema nurses, as well as assistant practitioners and support workers, this team works alongside the community nursing teams. Amalgamating three smaller services has improved patient care and created advantages for staff within the team and their colleagues. This article explores this development and uses a patient case study to illustrate its benefits.
KEYWORDS: Skin integrity Collaboration Oedema Personalised care
AREAS OF CHANGE
Management of patients with leg oedema Lower limb oedema is defined as a persistent, abnormal swelling of the lower limb (Bianchi et al, 2012), which is considered chronic after being present for more than three months (Moffatt et al, 2003). If unrecognised or mismanaged, chronic oedema eventually leads to lymphovenous oedema. However, this disease progression can be prevented if diagnosed and treated early in the disease continuum (Atkin, 2014).
Within local practice, community nurse visits were often being made on a daily basis to see patients with wet, weepy legs, indicating that oedema was not being recognised or treated optimally. Leaking fluid from lower limbs indicates that the lymphatic system can no longer cope with the increased fluid volume, which in turn has a detrimental effect on the skin’s integrity, causing weeping legs, skin breakdown and infection (Mahoney, 2015; Wounds UK, 2018).
Leg ulcers (venous, mixed and unspecified in aetiology) have been estimated to affect 33% of the UK adult population (732,000 patients), contributing to the estimated annual cost of £5.3 billion to the NHS for wound care and associated management of
▼ Practice point
Although change can be daunting, taking steps to review and discuss how things could be improved within your team can lead to many positive practical changes for practitioners and patients.
©Wound
Care
People
2019
medi. I feel better.Discover the medi Wound Care Therapy Chain within the medi World of Compression www.mediuk.co.uk
UCS™ DebridementPre-moistened debridement cloth for all skin and wound treatment.
• Soft loop technology helps to catch wound debris and slough
• Cloth can be used both sides• Sterile and ready to use in boxes of 10
Route to Market Code
NHSSC ELZ746
FP10 PIP 384-4271
Scottish Contract PECOS 217106
Direct from medi UK DT500
T. 01432 373500 | [email protected]
• Sterile and ready to use in boxes of 10
Pre-moistened
Poloxamer 188, cleanse, remove slough, debride most types of necrotic tissue and are known to be effective against biofi lm.Percival SL et al. Surfactants and their role in wound cleansing and biofi lm management. J Wound Care 2017;26(11):680-690.
©Wound
Care
People
2019
SKIN CARE
32 JCN 2019, Vol 33, No 3
comorbidities (Guest et al, 2015). Lymphoedema and chronic oedema have been estimated to affect more than 100,000 people in the UK (Moffatt et al, 2003). A subsequent study of community and inpatients identified 304 patients with chronic oedema, 40% of which also had leg ulceration. The prevalence of chronic oedema was found to increase with age, with the highest proportion being in women aged over 85 (Moffatt and Pinnington, 2012). These statistics support what the authors have identified in the clinical area, which has not, until now, been recognised or actively managed. Work is now being carried out to address these issues in the authors’ locality through training and raising awareness among primary care and community nursing teams.
Development of clinical pathways and formularies Each of the community nursing teams within the authors’ locality has a different clinical lead, with different knowledge and skill sets. This often leads to variations in practice in relation to skin care, wound care, and assessment and management of oedema. The aim of the skin integrity team leads was to standardise practice for skin and wound care and provide training opportunities across the locality using a coordinated approach. Nurses have commented in the past that wound care, although everyone’s job, is no one’s responsibility (Evans, 2017). This could be said for skin care and oedema management as well. The ongoing creation of pathways and/or algorithms aims to streamline the management of clinical needs.
There has been collaborative work with the local commissioning support unit to review the skin formulary. A revision of the
products suggested as first- and second-line therapies for the management of dry skin aims to enable more cost-effective emollient prescribing. These changes could potentially save the community trust £96,000 a year (personal communication with prescribing adviser, who worked out cost-savings if current prescribing trends continued, but with changed products). To support such prescribing modifications, a pictorial algorithm, which outlines
inoculation rate (spreading to other parts of the body from touching between the toes), and prevent secondary bacterial infection (Ilkit and Durdu, 2014).
Review of care plans and templates It became evident that the SystmOne care plans and templates used for patient records needed reviewing to make them fit for purpose, as a result of the different ways of working. Not all of the specialities with the skin integrity team had access to the same templates, and some, none at all. Through collaborative working with the clinicians involved, templates have been amended and made accessible to all to facilitate a consistent approach to documentation and allow easier evaluation of combined care.
Audit and research The skin integrity team has close links with secondary care specialist services in tissue viability and dermatology. Streamlining the services for patients with leg ulcers means that the teams running the clinics are well placed to identify appropriate patients for a national clinical trial of the geko™ device (a medical device powered by OnPulse™ neuromuscular electrostimulation technology, which can be used to increase blood circulation, prevent venous thrombosis, prevent and treat oedema and treat venous insufficiency and ischaemia), which the authors’ team have agreed to do.
Development of a complex case clinic Recognition of the contribution each specialist within the skin integrity team can make to patient care has led to the formation of a monthly specialist clinic, where patients can be seen for all skin,
▼ Practice point
Gaining patient feedback is vital to understanding how to improve services, especially in times of austerity.
▼ Practice point
Continuing to audit and reflect on changes as they are made provides ongoing opportunities for amendments and improvements.
‘Nurses have commented in the past that wound care, although everyone’s job, is no one’s responsibility (Evans, 2017). This could be said for skin care and oedema management as well.’
stages of dry skin severity, has been published alongside the new skin formulary, in the form of an A5 diary insert distributed to all community practitioners for reference. It is hoped that more appropriate skin management decisions can be made as a result, thereby improving patient care as well as reducing costs.
Current work is now underway to improve assessment and management of patients with tinea pedis (Athlete’s foot fungal infection). There is a well-recognised correlation between dermatomycosis (fungal infection) of the foot and acute bacterial cellulitis of the leg (Roujeau et al, 2004). The risk of tinea infections developing in between toes is increased for those with lymphoedema, obesity, diabetes and any trauma/lacerations (Al-Niaimi and Cox, 2009). The use of a pathway with clinical images and treatment algorithms aims to raise staff awareness of the condition. A proactive approach to identifying fungal infections of the feet can minimise cellulitis, reduce the self-
©Wound
Care
People
2019
JCN 2019, Vol 33, No 3 33
shopping, pain and psychosocial elements. Her initial score was 26/30, which went down to 2/30 after the intensive treatment plan.
There were four areas of ulceration on the front and lateral aspect of the leg. These were up to 2cm deep and the wound beds were obscured by the presence of thick devitalised tissue. The plan was to clean the leg and wounds with warm tap water (Fernandez and Griffiths, 2012) in a lined bucket, using a simple cream emollient as a soap substitute (Lymphoedema Framework, 2006). Once dried, a monofilament debridement lolly was used to aid debridement of
wound and oedema issues at one appointment. Interim visits between these clinics can also be done jointly by practitioners if necessary, as in the case study outlined below.
CASE STUDY: COLLABORATIVE WORKING
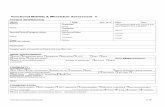
A woman aged 21 was referred to the lymphoedema service for assessment of her leg oedema following an acute admission (for 27 days) to a secondary setting out of county, for unilateral lower limb cellulitis. On initial assessment, her medical history indicated a two-year history of bilateral lipolymphoedema to both legs, associated with a body mass index (BMI) of 80, and a weight of 34 stone. The patient lives with her parents and works within the family business; she does not drive and sleeps in a bariatric chair. She has had several episodes of cellulitis in the past, mainly affecting her left leg.
On presentation she had a positive Stemmer’s sign. In a healthy person, a fold of skin can be pinched and lifted up at the base of the second toe, indicating that the Stemmer’s sign is negative. If you cannot raise the skin fold, the sign is positive, indicating lymphoedema (Lymphoedema Framework, 2006). There were four wounds, of which one was significant: a deep wound on the front of her left leg with yellow/green slough and significant malodour. The surrounding skin was eczematous in places and macerated in some of the skin folds (Figure 1).
At follow-up, the lymphoedema nurses recognised that the patient would benefit from a collaborative approach to her skin and wound management. Assessment from the tissue viability and dermatology nurse specialists allowed a new care plan to be implemented, addressing skin integrity and wound presentation. Part of the assessment included a life quality index questionnaire (Finlay and Khan, 1994), which assessed the impact of her condition on various lifestyle factors, such as work, sport,
SKIN CARE
Figure 1.Initial presentation of leg.
Figure 5.Eczema settling.
Figure 2.Removal of slough.
Figure 3.Bone nearly visible in wound.
Figure 4.Exudative eczema.
©Wound
Care
People
2019
34 JCN 2019, Vol 33, No 3
SKIN CARE
the slough from the wound beds. An antimicrobial alginate gel was applied to the wound to encourage further autolytic debridement (Figures 2 and 3). The wounds were then covered with a superabsorbent wound pad.
The skin integrity on the left leg was compromised by circumferential eczematous areas due to the adverse response to copious lymphorrhoea. The skin was red, sore and macerated in places, with tenderness and pain to touch. The patient also had secondary eczematous areas on the outer aspects of her arms, which
› Patient’s story
It all started on 28 May 2018, when I went on holiday with my best friend and god daughter to a local holiday park. Shortly after arriving, I started feeling a tingling sensation in my left leg. It was bright red and very hot. I put a cold compress onto it, hoping it would settle down; little did I know I would be so wrong. Due to the agonising pain I was in, I had to cut my holiday short and arranged a doctor’s appointment for the next day. I was prescribed oral antibiotics and told I had cellulitis. After four days of taking oral antibiotics, my parents took me to the local A&E department, as my leg had swollen to three times the size and was very painful and leaking a lot of fluid. On admission, a doctor told me I had a severe case of cellulitis and I would be put on intravenous (IV) antibiotics for the infection. A tissue viability nurse came and saw me and also diagnosed me with lymphoedema. I spent a further 26 days in hospital, spending my 21st birthday there. I can remember how happy I felt when they told me I was coming home — I burst into tears, as it had been such a stressful and worrying time.
I was seen by the community nurses a few times to redress my leg after coming home from hospital. However, as I was not classed as housebound, I was asked to see the general practice nurse for my dressings. The first appointment did not go very well, as she was a new nurse and appeared very stressed. Unfortunately, I think she took it out on me and told her manager that she was unable to deal with my leg, as it was too difficult. I ended up having my parents redressing my leg as the GP surgery staff were still struggling to know how best to manage it.
I finally received my first appointment for the community lymphoedema service. When that day arrived, I remember feeling so nervous and scared, but once my appointment was over I remember feeling very happy and positive, as I had been put at ease and told everything would be ok.
Since mid-October, my leg has gone from strength to strength and, having my legs bandaged, I have lost a lot of inches off my legs. To help with my healing progress, I decided to join a local slimming club. I have lost five and a half stone so far. My leg will never be the same, but at least I am alive and I am a lot happier!
were possibly due to increased sweating. The skin was protected using an emollient spray where it was not eczematous and a potent topical antibacterial steroid cream to the exuding eczema, using fingertip units (Wounds UK, 2018; Figures 4 and 5).
The patient was reviewed three times a week by the lymphoedema team and also intermittently (when needed) by the tissue viability and dermatology nurses. The use of compression bandaging was initiated on both legs, when they could be tolerated by the patient, as pain levels reduced (Figures 6 and 7).
Ongoing use of compression bandaging, wound management strategies and skin care led to complete healing of the wounds after 16 weeks. Ongoing
management included compression wraps and skin hygiene (using emollients as soap substitutes to wash the skin, as well as a layer of emollient left on the skin to soak into dry areas. The patient was to be monitored every three to four weeks to check progress and offer emotional support.
This has been quite an ordeal for the patient and her family. The authors believe that continuing her consultations for a further short period will help to build her self-esteem and confidence, and encourage her (with her parents) to maintain a self-care regimen with compression wraps and skin care.
CONCLUSION
This article has described the steps taken to identify and respond to
▼ Remember...
It is important to reflect continually on the service that we offer, and the outcomes we achieve.
Figure 6.Wound healing.
Figure 7.Skin and wound healing.
©Wound
Care
People
2019
JCN 2019, Vol 33, No 3 35
SKIN CARE
patient needs more effectively in relation to skin, wound and oedema associated with lower limb conditions. It was recognised that staff skills could be optimised through amalgamating smaller services into one team. The formation of the skin integrity team within a local community NHS trust has reduced several areas of concern. Clinical pathways for lower limb oedema, leg ulceration, tinea pedis and hyperkeratosis have been developed and implemented for use in primary and community care. Wound and skin care formularies have been reviewed, with supporting material produced for dressing choice guidance and an emollient pathway to support appropriate product usage. A training programme for registered and unregistered staff involved in the care and management of patients with lower limb issues has been embedded within the trust, supported by the skin integrity team.
One patient’s story illustrates the benefit of collaborative working within a community setting.
Future areas for improvement have been highlighted in relation to documentation, and the interlinking of care plans to reflect joint working changes has already been made in terms of SystmOne templates. These will be monitored and evaluated by the skin integrity team and further amendments applied as identified.
REFERENCES
Al-Niaimi F, Cox N (2009) Cellulitis and lymphoedema, a vicious cycle. J Lymphoedema 4(2): 38–42
Atkin L (2014) Lower-limb oedema — assessment, treatment and challenges. Br Community Nurs 19(Sup10): S22–S28
Bianchi J, Vowden K, Whitaker J (2012) Chronic oedema made easy. Wounds UK 8(2): 1–4
Evans K (2017) Improving wound care through reducing variation in practice. J Community Nursing 31(2): 20–1
Fernandez R, Griffiths R (2012) Water for wound cleansing. Cochrane Database of Systematic Reviews (2): 1–30
Finlay AY, Khan GK (1994) Dermatology Life Quality Index (DLQI) — a simple practical measure for routine clinical use. Clin Exp Dermatol 19(3): 210–16
Guest J, Ayoub N, Mcllwraith T, Uchegbu I, Gerrish A, Weidlich D, Vowden V, Vowden P (2015) Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 5: e009283
Ilkit M, Durdu M (2014) Tinea pedis: the aetiology and global epidemiology of a common fungal infection. Clin Rev Microbiol 41(3): 374–88
Lymphoedema Framework (2006) Best Practice for the management of Lymphoedema. International consensus. London: MEP Ltd
Mahoney K (2015) Identifying and managing ‘wet’ or ‘leaky’ legs. Skin Care Today 1(1): 34–43
Moffatt C, Franks F, Doherty D, Williams A, Badger C, Jeffs E, Bosanquet N, Mortimer P (2003) Lymphoedema: an underestimated health problem. QJM 96(10): 731–8
Moffatt C, Pinnington L (2012) Project
KEY POINTS The team was named the skin
integrity team to reflect the fact that maintaining the integrity of the skin is the cornerstone of best practice in all of these specialist areas.
The aim of the skin integrity team leads was to standardise practice for skin and wound care and provide training opportunities across the locality using a coordinated approach.
A proactive approach to identifying fungal infections of the feet can minimise cellulitis, reduce the self-inoculation rate, and prevent secondary bacterial infection.
If unrecognised or mismanaged, chronic oedema eventually leads to lymphovenous oedema. However, this disease progression can be prevented if diagnosed and treated early in the disease continuum.
Leaking fluid from lower limbs indicates that the lymphatic system can no longer cope with the increased fluid volume, which in turn has a detrimental effect on the skin’s integrity, causing weeping legs, skin breakdown and infection.
Having read this article, reflect on:
How you could improve collaborative working at your trust
The importance of maintaining skin integrity
Your knowledge of chronic oedema and disease progression
How clinical pathways can improve patient outcomes.
Then, upload the article to the free JCN revalidation e-portfolio as evidence of your continued learning: www.jcn.co.uk/revalidation
RevalidationAlert
Evaluation Report. Facilitating Development of Community Based Lymphoedema Services through Clinical Education: A report prepared for the East Midlands Health, Innovation and Education Cluster. University of Nottingham and Derby Hospitals NHS Foundation Trust
Roujeau JC, Sigurgeirsson B, Korting HC, Kerl H, Paul C (2004) Chronic dermatomycoses of the foot as risk factors for acute bacterial cellulitis of the leg: a case-control study. Dermatology 209: 301–7
Sweeney R (2018) Chronic oedema; identifying areas for service improvement. J Community Nurs 31(6): 21–6
Wounds UK (2018) Best Practice Statement. Maintaining Skin Integrity. Wounds UK, London
JCN
©Wound
Care
People
2019











![Skin integrity and wound care [autosaved] (2)](https://static.fdocuments.us/doc/165x107/554b4695b4c905ff268b5052/skin-integrity-and-wound-care-autosaved-2.jpg)


![Skin integrity and wound care [autosaved]](https://static.fdocuments.us/doc/165x107/554b5a28b4c9051b458b4cd6/skin-integrity-and-wound-care-autosaved.jpg)