Dermatology without pics
Transcript of Dermatology without pics

DermatolgyDermatolgy
Dr Alistair BrownDr Alistair Brown

Descriptive terms in dermatologyDescriptive terms in dermatology Common skin conditionsCommon skin conditions Skin cancerSkin cancer Emergency DermatologyEmergency Dermatology InfectionsInfections MCQsMCQs

What are you describing?What are you describing?
PruritusPruritus Lesion – altered area of skinLesion – altered area of skin Rash – eruptionRash – eruption Naevus – localised malformation of Naevus – localised malformation of
tissue structure.tissue structure. Comedone – plug in a sebaceous follicle Comedone – plug in a sebaceous follicle
containing sebum – may be open containing sebum – may be open (blackhead) or closed (whitehead). (blackhead) or closed (whitehead).
““The patient has a rash…”The patient has a rash…”

Where is it?Where is it? Generalised – all over bodyGeneralised – all over body Widespread – extensiveWidespread – extensive Localised – one area of skinLocalised – one area of skin Flexural – body fold eg groin, axillaFlexural – body fold eg groin, axilla Extensor – eg knees, shinsExtensor – eg knees, shins Pressure areas – sacrum, buttocks, ankles, Pressure areas – sacrum, buttocks, ankles,
heels.heels. Dermatome – skin supplied by single nerveDermatome – skin supplied by single nerve Photosensitive areas – sun exposed.Photosensitive areas – sun exposed.““The patient has a widespread rash affecting The patient has a widespread rash affecting
their torso”their torso”

What colour is it?What colour is it? Erythema – redness (due to inflammation Erythema – redness (due to inflammation
and vasodilation) blanches on pressure.and vasodilation) blanches on pressure. Purpura – red or purple colour (due to Purpura – red or purple colour (due to
bleeding into the skin or mucous bleeding into the skin or mucous membranes) does not blanch to pressure. membranes) does not blanch to pressure. Petechiae (small pinpoint macules) and Petechiae (small pinpoint macules) and ecchymoses (larger bruise like patches)ecchymoses (larger bruise like patches)
Hypopigmentation (pityriasis vesicolor)Hypopigmentation (pityriasis vesicolor) De-pigmentation (vitiligo)De-pigmentation (vitiligo) Hyperpigmentation (melasma)Hyperpigmentation (melasma)

ConfigurationConfiguration
Discrete Discrete Confluent – lesions merge togetherConfluent – lesions merge together LinearLinear TargetTarget AnnularAnnular DiscoidDiscoid

What shape is it?What shape is it?
Macule – flat area of altered colourMacule – flat area of altered colour Patch – larger area of altered colourPatch – larger area of altered colour Papule – solid raised lesion <0.5cm in Papule – solid raised lesion <0.5cm in
diameterdiameter Nodule – Solid raised lesion >0.5cm diameterNodule – Solid raised lesion >0.5cm diameter Plaque – palpable raised lesion >0.5cmPlaque – palpable raised lesion >0.5cm Vesicle – raised clear fluid filled lesion Vesicle – raised clear fluid filled lesion
<0.5cm diameter.<0.5cm diameter. Bulla – raised clear fluid filled lesion >0.5cm Bulla – raised clear fluid filled lesion >0.5cm
diameter.diameter.

Test YourselfTest Yourself
Macule Macule Patch Patch Papule Papule Nodule Nodule PlaquePlaque VesicleVesicle BullaBulla

http://www.dermnetnz.org/http://www.dermnetnz.org/dermatitis/atopic.htmldermatitis/atopic.html

Atopic ExcemaAtopic Excema
Itchy papules and vesicles on an Itchy papules and vesicles on an erythematous base.erythematous base.
Affects face and extensor in infants, flexor Affects face and extensor in infants, flexor aspect children and adults.aspect children and adults.
Occurs in early childhood, usually Occurs in early childhood, usually resolves.resolves.
Risk factors: fhx of atopy, assoc asthma, Risk factors: fhx of atopy, assoc asthma, allergic rhinitis etc)allergic rhinitis etc)
Exacerbating factors: infections, allergens Exacerbating factors: infections, allergens (chemical, food, dust, pets), sweating, (chemical, food, dust, pets), sweating, heat, stress.heat, stress.
Complications: secondary bacterial/viral Complications: secondary bacterial/viral infectioninfection

ManagementManagement
Avoid exacerbating agentsAvoid exacerbating agents Frequent emolientsFrequent emolients Topical steroids for flaresTopical steroids for flares Antihistamine for symptomatic reliefAntihistamine for symptomatic relief

http://www.dermnetnz.org/http://www.dermnetnz.org/scaly/psoriasis-general.htmlscaly/psoriasis-general.html

PsoriasisPsoriasis A chronic inflammatory disease hyperproliferation of A chronic inflammatory disease hyperproliferation of
keratinocytes and inflammatory cell infiltration.keratinocytes and inflammatory cell infiltration. Chronic plaque – most common Chronic plaque – most common
(Other types: guttate, seborrhoiec, flexural, pustular, (Other types: guttate, seborrhoiec, flexural, pustular, erythrodermic)erythrodermic)
2% of population2% of population Precipitants: trauma, stress, infection, drugs, alcoholPrecipitants: trauma, stress, infection, drugs, alcohol Signs and symptoms:Signs and symptoms:
Well demarcated lesions with erythematous base, and silver scaly Well demarcated lesions with erythematous base, and silver scaly plaquesplaques
Affecting extensor surfaces and scalpAffecting extensor surfaces and scalp Auspitz sign Auspitz sign 50% nail changes (pitting, onycholysis)50% nail changes (pitting, onycholysis) 5-8% associated arthropathy (symmetric polyarthritis, 5-8% associated arthropathy (symmetric polyarthritis,
asymmetrical oligomonoarthritis, distal interphalangeal disease, asymmetrical oligomonoarthritis, distal interphalangeal disease, spondyloarthropathy, athritis mutilans.)spondyloarthropathy, athritis mutilans.)

ManagementManagement
Avoid precipitants.Avoid precipitants. Topical therapy – vit d analogues, topical Topical therapy – vit d analogues, topical
corticosteroids, coal tar preparations, corticosteroids, coal tar preparations, dithranol, topical retinoids, salicylic acids.dithranol, topical retinoids, salicylic acids.
Phototherapy (extensive disease)Phototherapy (extensive disease) Systemic – methotrexate, oral retinoids, Systemic – methotrexate, oral retinoids,
ciclosporin, mycophenolate mofetil, ciclosporin, mycophenolate mofetil, biologics (adalimumab, etanercept, biologics (adalimumab, etanercept, infliximab and ustekinumab)infliximab and ustekinumab)

http://www.dermnetnz.org/http://www.dermnetnz.org/acne/acne-vulgaris.htmlacne/acne-vulgaris.html

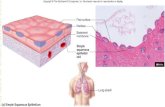
Acne VulgarisAcne Vulgaris Inflammation of pilosebaceous follicle – Inflammation of pilosebaceous follicle –
face, chest, upper back.face, chest, upper back. Hormonal – increased sebum productiomn, Hormonal – increased sebum productiomn,
abnormal follicular keratinisation, p. acnes abnormal follicular keratinisation, p. acnes colonisation and inflammation.colonisation and inflammation.
Non inflammatory lesions - open and Non inflammatory lesions - open and closed comedones, inflammatory lesions – closed comedones, inflammatory lesions – papules, pustules, nodules, cysts.papules, pustules, nodules, cysts.
Complications – post inflammatory Complications – post inflammatory hyperpigmentation, scarring, deformity, hyperpigmentation, scarring, deformity, psychosocial impact.psychosocial impact.

ManagementManagement
Topical – benzoyl peroxide, topical Topical – benzoyl peroxide, topical antibitics, topical retinoids.antibitics, topical retinoids.
Oral Oral oral antibiotics eg tetracycline’soral antibiotics eg tetracycline’s Females – OCP – dianetteFemales – OCP – dianette Oral retinoids – isotretinoin, severe Oral retinoids – isotretinoin, severe
acneacne

http://www.dermnetnz.org/http://www.dermnetnz.org/lesions/basal-cell-lesions/basal-cell-carcinoma.htmlcarcinoma.html

Basal cell carcinomaBasal cell carcinoma Locally invasive tumour of epidermal Locally invasive tumour of epidermal
keratinocyteskeratinocytes ““pearly papule” with surface telangectasia and pearly papule” with surface telangectasia and
rolled edges, may have ulcerated centre.rolled edges, may have ulcerated centre. Risk factors Risk factors
uv exposureuv exposure Sunburn as a childSunburn as a child Skin type 1 Skin type 1 MaleMale ImmunosuppresionImmunosuppresion Previous hx of skin cancerPrevious hx of skin cancer Genetic predispositionGenetic predisposition
ManagementManagement SurgicalSurgical RadiotherapyRadiotherapy Other: cryotherapy, curretage and cautery, topical Other: cryotherapy, curretage and cautery, topical
photodynamic therapy, imiquimod cream.photodynamic therapy, imiquimod cream.

http://www.dermnetnz.org/http://www.dermnetnz.org/lesions/bowen.htmllesions/bowen.html

Squamous cell carcinomaSquamous cell carcinoma Invasive malignant tumour of epidermal Invasive malignant tumour of epidermal
kertinocytes or appendages with potential to kertinocytes or appendages with potential to metastasise. metastasise.
Risk factors: sun exposure, pre-malignant skin Risk factors: sun exposure, pre-malignant skin condistions eg. Actinic keratoses, chronic condistions eg. Actinic keratoses, chronic inflammation (leg ulcers), immunosuppression, inflammation (leg ulcers), immunosuppression, genetic predisposition, smoking.genetic predisposition, smoking.
Treatment: Treatment: Surgical excision Surgical excision Moh’s micrographic surgeryMoh’s micrographic surgery RadiotherapyRadiotherapy Chemotherapy – metastatic diseaseChemotherapy – metastatic disease

http://http://www.dermnetnz.org/www.dermnetnz.org/
lesions/melanoma.htmllesions/melanoma.html

Malignant melanomaMalignant melanoma Invasive malignant tumour of epidermal melanocytes Invasive malignant tumour of epidermal melanocytes
with metastatic potential.with metastatic potential. ABCDE approach ABCDE approach
AsymettryAsymettry BorderBorder ColourColour DiameterDiameter EvolutionEvolution Symptoms – bleeding, itchSymptoms – bleeding, itch
Risk factors:Risk factors: Atypical molesAtypical moles Large numbers of molesLarge numbers of moles Skin type 1&2Skin type 1&2 Severe sun burn <14Severe sun burn <14 FhxFhx Sun exposureSun exposure Previous melanomaPrevious melanoma immunosuppressionimmunosuppression

ManagementManagement
Surgical excisionSurgical excision Excision biopsyExcision biopsy WLE +/- sentinel node biopsyWLE +/- sentinel node biopsy If node positive – axillary clearanceIf node positive – axillary clearance If further nodes positive – stagingIf further nodes positive – staging
Intensive followupIntensive followup Palliative options – aim to reduce Palliative options – aim to reduce
macroscopic disease burden.macroscopic disease burden.

EmergenciesEmergencies
http://www.dermnetnz.org/http://www.dermnetnz.org/reactions/angioedema.htmlreactions/angioedema.html

Urticaria, Angioedema, Urticaria, Angioedema, AnaphylaxisAnaphylaxis
Causes – food, drugs, insect bites, contact Causes – food, drugs, insect bites, contact eg latex, autoimmune, hereditary eg latex, autoimmune, hereditary (angiodema), etc(angiodema), etc
Urticaria – swelling superficial dermis – Urticaria – swelling superficial dermis – raises epidermis causing itch wheals.raises epidermis causing itch wheals.
Angiodema – deeper swelling involving Angiodema – deeper swelling involving dermis and subcutaneous tissue – tongue dermis and subcutaneous tissue – tongue and lips.and lips.
Anaphylaxis – bronchospasm, facial and Anaphylaxis – bronchospasm, facial and laryngeal oedema, hypotension, can start laryngeal oedema, hypotension, can start with angiodema and urticaria.with angiodema and urticaria.

ManagementManagement
ABC approach – call for help if ABC approach – call for help if concerned.concerned.
Urticaria only – antihistaminesUrticaria only – antihistamines Angioedema and severe urticaria – Angioedema and severe urticaria –
corticosteroids and antihistamines.corticosteroids and antihistamines. Anaphylaxis – get help!Anaphylaxis – get help!
Adrenaline 0.5 mg IM = 0.5 mL of 1:1000Adrenaline 0.5 mg IM = 0.5 mL of 1:1000 Antihistamine – chlorphenamineAntihistamine – chlorphenamine CorticosteroidsCorticosteroids

https://www.google.co.uk/https://www.google.co.uk/search?search?
q=stevens+johnson+syndroq=stevens+johnson+syndrome+derm+nz&oq=steven&ame+derm+nz&oq=steven&aqs=chrome.1.69i57j69i59l2jqs=chrome.1.69i57j69i59l2j0l3.3052j0j4&sourceid=chr0l3.3052j0j4&sourceid=chrome&espv=210&es_sm=122ome&espv=210&es_sm=122
&ie=UTF-8&ie=UTF-8

Stevens-johnson Stevens-johnson syndrome and Toxic syndrome and Toxic epidermal necrolysisepidermal necrolysis
•Primarily a drug reaction: sulfonamides (eg cotrimoxazole), NSAIDs, Carbamazepine, Phenytoin, Phenobarbital, Valproic acid, Lamotrigine.•Can also be caused by infections: HSV, mycoplasma.•Prodromal illness – fever, cough, sore throat, general malaise followed by abrupt onset macular or purpuric blistering rash.•Prominent mucosal involvement, at least 2 of:
•Eyes (conjunctivitis) – red, sore, sticky •Lips/mouth (cheilitis, stomatitis) – red crusted lips, mouth ulcers •Oesophagus – causing difficulty eating •Upper respiratory tract (trachea and bronchi) – causing cough and respiratory distress •Genital area and urinary tract – ulcers •Gastrointestinal tract – causing diarrhoea.
•SJS <10%BSA TEN>30% BSA•Mortality 5-12% SJS, >30%TEN•Management – stop drug cause, supportive – preferably burns unit

http://www.dermnetnz.org/reactions/
erythroderma.html

ErythrodermaErythroderma Exfoliative dermatitis involving >90% of Exfoliative dermatitis involving >90% of
skin surface. 20-40% mortality.skin surface. 20-40% mortality. Treat cause – eg. atopic dermatitis, Treat cause – eg. atopic dermatitis,
psoriasis, blistering diseases (pemphigus psoriasis, blistering diseases (pemphigus and bullous pemphigoid), cutaneous T-cell and bullous pemphigoid), cutaneous T-cell lymphomalymphoma
Supportive management – fluid loss, Supportive management – fluid loss, elctrolyte imbalance, hypothermia, high elctrolyte imbalance, hypothermia, high output cardiac failure, capillary leak, output cardiac failure, capillary leak, prevention of secondary infection.prevention of secondary infection.
Prognosis depends on cause, mortality 20-Prognosis depends on cause, mortality 20-40%40%

http://www.dermnetnz.org/bacterial/necrotising-
fasciitis.html

Necrotising fasiitisNecrotising fasiitis
• Rapidly spreading infection of the deep fascia with secondary tissue necrosis
• Group A haemolytic strep or mixed anaerobic and aerobic bacteria.
• Risk factors – abdominal surgery, diabetes, immunosuppression, age, malignancy
• BUT 50% occur in previously healthy individuals
• Pain disproportionate to signs, erythematous blistering necrotic skin, systemically unwell with fever and tachycardia, subcutanceos emphysema (crepitus).
• Urgent surgical debridement and antibiotics

http://www.dermnetnz.org/
viral/eczema-herpeticum.html

Excema HerpeticumExcema Herpeticum
• Caused by HSV infection superimposed on a skin condition most commonly atopic eczema.
• Extensive papules and erosions with systemic fever and malaise
• Management – antivirals (aciclovir) +/- abx for secondary bacterial infection
• Complications – Encephalitis, DIC, opthalmic involvement, rarely death

http://http://www.dermnetnz.org/www.dermnetnz.org/
bacterial/impetigo.htmlbacterial/impetigo.html

ImpetigoImpetigo Streptococcus pyogenes and/or Streptococcus pyogenes and/or
Staphylococcus aureus Staphylococcus aureus Enlarging pustules and round, oozing Enlarging pustules and round, oozing
patches +/- golden yellow crusts. patches +/- golden yellow crusts. Exposed areas such as the hands and face, or Exposed areas such as the hands and face, or
in skin folds particularly the armpits.in skin folds particularly the armpits. Management:
Antiseptic or antibiotic ointment eg. Fusidic acid
Oral antibiotics Avoid spread
Avoid close contact with others. Affected children must stay away from school until
crusts have dried out. Use separate towels and flannels. Change and launder clothes and linen daily.

http://http://www.dermnetnz.org/www.dermnetnz.org/
arthropods/scabies.htmlarthropods/scabies.html

ScabiesScabies
Itchy rash on trunk and limbs, finger Itchy rash on trunk and limbs, finger webspaces, wrist, spares the scalpwebspaces, wrist, spares the scalp
Burrow tracts can be seenBurrow tracts can be seen Diagnosis on microscopic examination of Diagnosis on microscopic examination of
tracts.tracts. Treatment (all contacts simultaneously!)Treatment (all contacts simultaneously!)
25% Benzyl benzoate lotion, applied daily for 3 days
5% Permethrin cream, left on for 8-10 hours 0.5% Aqueous malathion lotion, left on for 24 hours

MCQsMCQs
Atopic Eczema True or FalseA. a family history of atopyB. If occurs early and defined has bad prognosisC. In children it is common on cheeksD. In adults more common on flexor areaE. Pruritis is absent

MCQ 2MCQ 2
What skin condition What skin condition is this likely to be?is this likely to be?- Atopic dermatitisAtopic dermatitis- Tinea corporis Tinea corporis - PsoriasisPsoriasis- Vitiligo Vitiligo - ScabiesScabies
What else should What else should you examine?you examine?

MCQ 3MCQ 3
True or False which of the following True or False which of the following are known risk factors for are known risk factors for melanoma?melanoma?
Sun bed useSun bed use Xeroderma pigmentosumXeroderma pigmentosum SmokingSmoking CiclosporinCiclosporin Living in the South WestLiving in the South West ObesityObesity

MCQ4MCQ4 How would you manage How would you manage
this patient?this patient? Imiquimod creamImiquimod cream Watch and waitWatch and wait Punch biopsy of the lesion Punch biopsy of the lesion
for histologyfor histology Take a picture and review in Take a picture and review in
3months to see if it has 3months to see if it has growngrown
Surgically remove with a Surgically remove with a 2mm margin for histology2mm margin for histology
WLE with a 2-3cm marginWLE with a 2-3cm margin

MCQ 5MCQ 5 A 60 year old woman presents with raised,
erythematous lesions on the limbs and blistering in the mouth and eyes. She had been taking a number of drugs prescribed by her GP. Which may be responsible for her presentation?
nifedipine paracetamol paroxetine prednisolone Sulphasalazine
What is the most important first management?

MCQ 6MCQ 6 A 22 year old male presents with
generalised pruritus of six weeks duration. Examination reveals little except for erythematous papules between the fingers. Which of the following therapies would be most appropriate for this patient?
astemizole calamine lotion chlorpromazine ciprofloxacin permethrin cream

MCQ 7MCQ 7
Which of the following is a recognised feature of psoriasis?
angular stomatitis iridocyclitis Koebner Phenomenon loss of hair response to chloroquine