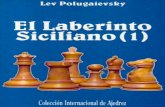
Dermatologic Emergencies - Dr. Siciliano
-
Upload
bcooper876 -
Category
Education
-
view
1.132 -
download
6
description
Transcript of Dermatologic Emergencies - Dr. Siciliano
Don’t be Rash! How to approach the undifferentiated lesion
GENINE SICILIANO, MD
PGY 3, EMERGENCY MEDICINE
SENIOR GRAND ROUNDS
AUGUST 28TH, 2014
Goals
Review EM Dermatology Basics How to describe a rash/talk to our derm consultants
Algorithmic approach to differential diagnosis of the unknown lesion
Quickly recognize toxic from non-toxic rashes
Focus on 3 rare dermatology emergencies you can’t miss
Case 1 35 yo M, h/o psoriasis,
tachycardic, ill appearing
-This covers 90% of his body
http://psoriasisfreetips.com/wp-content/gallery/photos-pustular/pustular-psoriasis-pictures-3-508x338.jpeg
Case 2 Elderly gentleman brought back for fever, tachycardia
Picture: P Mohite, A Bhatnagar. A Case Of Fournier's Gangrene Reconstructed By Pedicle Thigh Flap. The Internet Journal of Plastic Surgery. 2006 Volume 3 Number 1.
Dermatology for the Emergency Physician
Must know:How to describe rashes Basic differentialToxic vs non-toxic rashBasic management/resuscitationWhen/how to talk to your consultant
Why important?5% All ED visits
Step 2: “Get Naked” PolicySkin Exam
MorphologyArrangementDistribution/Pattern ExtentEvolutionary Change
Algorithmic Approach to Differential Diagnosis
Goal: Improve how we think about rashes and categorize them in our minds
Question 1: Rash morphology Question 2: Rash Distribution/Pattern Question 3: Sick or not Sick
Modified Lynch Algorithm
6 categoriesDiffuse erythematousNon-erythematousMaculopapularPetechial/PurpuricVeciulobullosPustular
Picture with permission from Dr. Walt Green
Modified Lynch Algorithm
Possible life- threatening
rash
Solid
Erythematous
Maculopapular Petechial/ Purpuric
Diffuse erythematous
Non-erythematous
Fluid-filled
Clear
Vesiculo-bullous
Pustular
4 yo w/ Fever, 3 days, well appearing
Image obtained from: http://www.sharinginhealth.ca/conditions_and_diseases/kawasaki.html. Author: Dong Soo Kim.
SolidErythematousMaculopapular
Maculopapular
Central
SICK: Viral Exanthem, Kawasaki*,
DRESS
NOT SICK: Drug rxn, pityriasis, tinea, viral
Peripheral
SICK: EM/SJS, Lyme, Meningococcemia*, Syphilis, early TSS,
RMSF
NOT Sick:
Scabies, Atopic
Dermatitis, psoriasis,
tinea
30yo, Fever, nausea, vomiting 2 days. Later developed stiff neck, HA
8yo, abdominal pain, rash.
http://www.vaccineinformation.org/photos/meni_mt002.jpg http://www.pediatricsconsultant360.com/sites/default/files/images/Screen%20Shot%202014-01-28%20at%2010.51.26%20AM.png
Solid ErythematousPetechial/Purpuric
Petechial/Purpuric
PalpableSick:
Meningococcemia*,
disseminated gonococcemi
a, endocarditis, RMSF, HSP
Not Sick: Autoimmune vasculitis,
HSP
Non Palpable
Sick: DIC, TTP
Not Sick: ITP
2 yo male in nursery with fever
25yo Male with HA, fever, tachycardia, nausea after leaving a restaurant
http://www.pediatricsconsultant360.com/sites/default/files/Screen%20Shot%202013-06-03%20at%2011.22.21%20AM.png
https://escholarship.org/uc/item/68h2w3wb/1.jpg
Solid Erythematous Diffuse Erythematous
Diffuse Erythematous
Sick
+ Nikolsky: SSSS/TEN,
DRESS
- Nikolsky: TSS, Kawasaki, Scarlet Fever, Erythroderma, Red man
syndrome , early nec fasc
Not Sick
Anaphylaxis, Scombroid, Alcohol
Flush
Solid Non-erythematous
Secondary SyphilisAnthraxVitiligo
http://manbir-online.com/grafics/Syphilis-hands.jpg
50yo w/ Flank pain 2 days, negative CT renal colic
65 yo with several days of painful, burning rash, now involving oral mucosa
http://www.medicalnewstoday.com/images/articles/154/154912/shingles-on-torso.jpg
http://classconnection.s3.amazonaws.com/445/flashcards/491445/jpg/bullous_pemphigoid_3_0505251328970809379.jpg
Fluid-filled Clear Vesiculo-bullous
Vesiculo-bullous
Diffuse
Sick: Varicella, Smallpox, Dissem
gonococcemia, DIC, TEN, PV
Not sick: PV,
BP
PeripheralSick: Nec Fasc, PV,
Hand-foot-
mouth
Not Sick: Contact dermatitis, Zoster, vesicular eczema,
burns
Fluid-filled Pustular
Bacterial FolliculitisGonorrheaGeneralized pustular
psoriasis
http://www.dermnetnz.org/acne/img/s/folliculitis5-s.jpg
Topical Steroids Potency
Appropriate for rashToo weak= at risk for reboundBased on ability to induce vasoconstriction
Flourination Increases potencyAvoid in pregnancy
http://www.walgreens.com//images/drug/0151672128202.jpg
Topical Steroids- PotencyClass Potency Example
1 Highest Clobetasol (0.05%)
2 High Fluocinonide (0.05%)
3 High-Medium Triamcinolone (0.5%)
4 Medium Mometasone furoate (0.1%)
5 Medium-low Triamcinolone (0.1%)
6 Low Triamcinolone (0.025%)
7 Lowest Hydrocortisone (1%, 2.5%)
Other treatment options
AntihistaminesOther topicals
If it’s dry, keep it wet and if it’s wet, keep it dry
AntimicrobialsScabies, impetigo, candida, dermatophytes, etc.
Dermatologic Emergencies
Definition:
Acute skin loss leading to loss of thermoregulatory, metabolic, infection control sepsis
Dermatologic Emergencies you CAN’T afford to miss…
Fixed Drug Eruption Disseminated viral infections: VZV, HSV
EM/SJS/TEN – Note: not necessarily same spectrum
Anaphylaxis/angioedema BP/PV RMSF TTP, DIC
Meningiococcemia, Disseminated Gonoccoccal infection
Toxin mediated: SSSS, TSS Exfoliative Erythroderma: eczema, psoriasis
DRESS Syndrome Necrotizing Soft tissue infections
DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms syndrome)
Definition: Severe adverse drug reaction with fever, rash, and internal organ involvement (liver= #1)
Causes:Mostly antiepileptics/mood stabilizers
Phenobarabital, carbamazepine, phenytoin, lamictal, sulfa, dapsone, modafanil, ? HHV6
DRESS Syndrome Pathophysiology: T cell mediated reaction (suspected), potential genetic predisposition
10% Mortality
Diagnostic Criteria:
RegiSCAR and Japanese consensus group
Management: Supportive, admission, support associated organ dysfunction
Case 1 - Generalized Pustular Psoriasis
Rare form of psoriasis in which most or all of the skin surface is involved with a scaly erythematous dermatitis (subset of erythroderma), puss filled blisters and plaques. Immune-mediated.
Diagnosis Febrile, systemically ill-appearing, leukocytosis. Triggering factors: drugs, infection, stress, steroids
Why important to ED Doc?Mortality – 8-20% worse with delayed diagnosis
Generalized Pustular Psoriasis
Complications: Metabolic (low albumin, Ca), amyloidosis, inflammatory polyarthritis, cholestatic jaundice, DVT, secondary staff infection.
Management: Withdraw provocative factors, admit, bed rest, fluid/electrolyte repletion, analgesia, antihistamines. Often need ICU.
Wound care: Bland emollients, wet dressings, mild-moderate topical steroids, systemic steroids in severe cases
Case 2: Necrotizing Soft Tissue InfectionsClassification: by microbial cause
Type I: Polymicrobial (aerobe and anaerobes) - 55-75%Common with DM, PVDClostridium less common in recent years
Type II: Group A Strep, StaphHealthy person with recent trauma, operation
?Type III: Vibrio Vulnificus
Necrotizing Soft Tissue Infections Risk Factors
Age, DM, alcoholism, PVD, CAD, RF, HIV/CA/immunocompromised, NSAIDs, IVDA, chronic ulcers/skin infections
Why Important?25-30% Mortality
Bacteremia = strong predictor of mortality
Exponentially worse with delayed diagnosis
Pathophysiology
Direct inoculation/invasion from injury site vs spontaneous
Bacteria proliferate invade subcutaneous & deep fascia release exotoxins tissue ischemia, necrosis, systemic toxicity
Spreads as fast as 1 inch/ hour Note: Early involvement causes little skin change
Signs/Symptoms & Diagnosis
PAIN out of proportion Fever, tachycardia Recent trauma/break in skin Cellulitic findings, edema Crepitus (only present 13-30% of time) Late findings: bronze/brownish discoloration, malodorous discharge, bullae
Labs: CBC, CMP, coags, cultures, blood gas Imaging: XR/CT
Picture from Dr. Walt Green
ED management EARLY DIAGNOSIS!!! Subtle findings in unclear cases Early Broad spectrum antibiotics
Rarely effective alone Fluids, transfusion as indicated Careful with pressors Early Surgical Intervention!!! Hyperbaric oxygen
Picture from Dr. Walt Green
Conclusions Have a systematic, simple approach to the unknown rash
Start with “Sick” vs “Not Sick”
EM physician MUST be the expert in recognition of the TOXIC RASH
Get your consultants involved EARLY
GET NAKED!!!
References
Craig K, Meadows S. What is best duration of steroid therapy for contact dermatitis. Journal of Family Medicine. 2006
Life in the Fast lane
Nguyen T., Freedman J. Emergency Medicine Practice Bulletin. Dermatologic Emergencies: Diagnosing and Managing Life-Threatening Rashes. September 2002.
Tintinalli’s Emergency Medicine. 7th Edition.
Thank you to Helen Mayo, Drs Dustin William, Walter Green