Delivery of drugs applied topically to the skin
-
Upload
michael-stephen -
Category
Documents
-
view
214 -
download
0
Transcript of Delivery of drugs applied topically to the skin

CME
10.1586/EDM.12.32 383ISSN 1746-9872© 2012 Expert Reviews Ltdwww.expert-reviews.com
Review
Vânia Rodrigues Leite-Silva1,2, Mariana Mandelli de Almeida3,4, Aurélie Fradin5, Jeffrey Ernest Grice2 and Michael Stephen Roberts*2,6
1Universidade Federal de São Paulo, Instituto de Ciências Ambientais Químicas e Farmacêuticas, Diadema SP, Brasil 2The University of Queensland, Therapeutics Research Centre, School of Medicine, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia 3University of São Paulo, Faculty of Pharmaceutical Sciences, Department of Pharmacy, São Paulo, Brazil 4CAPES Foundation, Ministry of Education of Brazil, Brasilia-DF 70040-020, Brazil 5University of Rennes 1, Faculty of Pharmacy, 35043 Rennes Cedex, France 6University of South Australia, School of Pharmacy and Medical Science, City East Campus, Adelaide, South Australia *Author for correspondence: [email protected]
The stratum corneum is a formidable physical, environmental and microbial barrier, protecting mammalian organisms from external insult and maintaining homeostasis. If the skin is to be used as a route of topical drug delivery, the barrier must be overcome, but this can normally only be achieved with small, relatively lipophilic molecules. Strategies to increase the range of substances that are suitable for transdermal delivery and to improve the permeation of particular substances include advanced formulation and the use of chemical and physical enhancement techniques. Nanomaterials are increasingly being exploited as carriers to deliver materials such as drugs, dyes, vaccines or gene fragments to specific cell targets for therapeutic or diagnostic purposes.
Delivery of drugs applied topically to the skinExpert Rev. Dermatol. 7(4), 383–397 (2012)
Keywords: formulation • nanosystems • penetration enhancement • skin barrier • stratum corneum • topical application
Expert Review of Dermatology
2012
7
4
383
397
© 2012 Expert Reviews Ltd
10.1586/EDM.12.32
1746-9872
1746-9880
Delivery of drugs applied topically to the skin
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Expert Rev. Dermatol.
Review
Medscape: Continuing Medical Education Online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the
Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and Expert Reviews Ltd. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To par-ticipate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 70% minimum passing score and complete the evaluation at www.medscape.org/journal/expertderm; (4) view/print certificate.
Release date: 24 September 2012; Expiration date: 24 September 2013
Learning objectives
Upon completion of this activity, participants will be able to:• Assess the protective barrier of the skin
• Analyze the science of transdermal drug therapy
• Distinguish favorable characteristics of mechanisms to help skin penetration by drugs
• Evaluate physical enhancement techniques to improve transdermal drug delivery
For reprint orders, please contact [email protected]
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)384
Review
For thousands of years, medicinal substances have been applied to the skin in the belief that they could treat diseases, and in the past 60 years, there have been considerable advances in the understanding of the mechanisms that govern the absorption of chemicals through the skin [1]. It is known that the skin is a formidable barrier to the passage of substances into and out of the body, but it is also an interactive interface that can be manipu-lated to allow it to become a viable pathway for drug transporta-tion. Consequently, there is increasing commercial and research interest in the transdermal route, which overcomes some of the disadvantages of oral or intravenous administration, such as rapid metabolism, limited bioavailability or poor tolerance [2]. The main advantages of the topical delivery route include the elimination of first-pass metabolism, sustained drug delivery, reduced frequency of administration, reduced side effects and improved patient com-pliance [3]. However, very few drugs are suitable for delivery by the topical route, with passive penetration through skin normally being limited to small molecules (<500 Da), which are neutral and relatively lipophilic [3,4].
To expand the range of commercially available topical prod-ucts, this work has concentrated on four aspects: finding new suitable compounds, enhancing the penetration of drug candi-dates with less than optimal properties, targeting the penetrants
to specific areas within or beyond the skin, and ensuring this is done with a minimum of adverse skin or systemic reactions [2]. However, experimental evaluation of topical drug delivery can be time consuming, expensive, ethically questionable in the case of in vivo experiments, or of limited application, due to the lack of appropriate models. Consequently, there have been many attempts to develop mathematical algorithms to predict skin permeability based on the physicochemical properties of the solute, where experimental data were unavailable, or alter-natively, to eliminate the need for such data [4–9]. Although such techniques have met with limited and varied success, and a globally applicable model of skin penetration has yet to be achieved, the work has nonetheless led to a deeper understand-ing of the mechanisms that control skin absorption. This review will examine the properties of the skin and the vehicle that can influence percutaneous absorption of a particular solute and the use of advanced formulations and other technologies to provide enhanced or targeted drug delivery.
Intrinsic skin properties affecting drug deliveryThe skin barrierThe skin acts as a formidable barrier to the entry of exogenous substances, as well as controlling homeostasis by limiting the loss
Financial & competing interests disclosure
Editor
Elisa Manzotti
Publisher, Future Science Group, London, UK.
Disclosure: Elisa Manzotti has disclosed no relevant financial relationships.
CME Author
Charles P. Vega, MD
Health Sciences Clinical Professor; Residency Director, Department of Family Medicine, University of California, Irvine
Disclosure: Charles P. Vega, MD, has disclosed no relevant financial relationships.
Authors and Credentials
Vânia Rodrigues Leite-Silva, PhD
Universidade Federal de São Paulo, Instituto de Ciências Ambientais Químicas e Farmacêuticas, Diadema SP, Brasil; The University of Queensland,
Therapeutics Research Centre, School of Medicine, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia
Disclosure: Vânia Rodrigues Leite-Silva, PhD, has disclosed the following relevant financial relationships: supported by the Foundation of Research
Support of São Paulo (FAPESP).
Mariana Mandelli de Almeida
University of São Paulo, Faculty of Pharmaceutical Sciences, Department of Pharmacy, São Paulo, Brazil
Disclosure: Mariana Mandelli de Almeida has disclosed the following relevant financial relationships: supported by the CAPES Foundation, Ministry
of Education of Brazil, Brasilia-DF 70040-020, Brazil.
Aurélie Fradin
University of Rennes 1, Faculty of Pharmacy, Rennes Cedex, France
Disclosure: Aurélie Fradin has disclosed no relevant financial relationships.Jeffrey Ernest Grice, PhD
The University of Queensland, Therapeutics Research Centre, School of Medicine, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia
Disclosure: Jeffrey Ernest Grice, PhD, has disclosed no relevant financial relationships.Michael Stephen Roberts, PhD, DSc
The University of Queensland, Therapeutics Research Centre, School of Medicine, Princess Alexandra Hospital, Woolloongabba, Queensland,
Australia; University of South Australia, School of Pharmacy and Medical Science, City East Campus, Adelaide, South Australia, Australia
Disclosure: Michael Stephen Roberts, PhD, DSc, has disclosed no relevant financial relationships.
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
385www.expert-reviews.com
Review
of internal water. This barrier function was first shown to reside in the stratum corneum (SC), or horny layer, in pioneering work by Winsor and Burch in 1944 [10] and in more sophisticated tape-stripping experiments by Blank in 1953 [11]. Transepidermal water loss (TEWL), the rate of water evaporation from the surface of the skin, can be used as a measure of the barrier status [12]. Elevated TEWL is seen in patients with dry skin and atopic dermatitis, who have a perturbed skin barrier [13,14]. In addition, barrier function, assessed by TEWL, was shown to be related to the total lipid content of the SC, particularly sphingo lipids and free sterols, rather than nonpolar species [15]. The lipids, surrounding the proteinaceous corneocytes, are arranged in highly organized lamellar bilayers [16,17], providing essential barrier integrity. As the major route of skin penetration for drugs or other substances is via the intercellular lipids [3], processes that extract lipids or cause disorder in their packing are likely to make the skin more permeable to these materials. This concept forms the basis of many of the penetration enhancement strategies to be discussed in the following sections.
Skin hydrationIn normal skin, where the barrier is intact, increasing the water content of the skin by treatments such as occlusion can lead to enhanced penetration of a substance. This may be due to an altera-tion in the solubility of the permeant in the SC to increase the partitioning from the vehicle into the membrane [18]. Moreover, it could be speculated that increased skin hydration may lead to swelling of the SC structure and a rearrangement of the lipids, resulting in increase in penetration, although there is no experi-mental evidence at this stage. Occlusion is exploited in com-mercially available transdermal patches [19]. An inverse relation-ship between TEWL and SC hydration is well known, and high TEWL values, as a marker of disturbed skin barrier function, are frequently correlated with low hydration of the SC [18]. Some common formulation ingredients such as urea are also effective in increasing skin hydration [20].
Anatomical siteThe permeability of the skin at different body sites has been exten-sively studied over a range of ages, from neonates to adults. Wide differences in permeability have been seen at different anatomical sites, and these may be due to variations in skin properties such as SC thickness (greatest on palmar regions of hands and feet), hair follicle density, skin pH, sebum production and skin hydration [21,22]. Such variations need to be taken into account when prod-ucts are being formulated for specific anatomical applications. The toxicological implications of applying products to areas of high permeability such as the lips or genitals should also be appreciated.
Age, ethnicity & genderChanges in skin structure occur with ageing, with the epidermis becoming thinner and the keratinocytes less adherent to one another. In addition, the dermis becomes atrophic and relatively acellular and avascular, with alterations in collagen, elastin and glycosaminoglycans. On the other hand, barrier function appears
to be unaffected by ageing, at least in adults, with no significant changes in SC thickness [23,24] or protein content [25] and unal-tered permeation of compounds such as estradiol, caffeine, aspi-rin, nicotinates or water [26–28]. However, in children, particularly neonates, skin barrier function may be significantly reduced [29].
The majority of studies have reported no significant differ-ences in skin barrier function across different ethnic groups [30,31]. Indeed, ethnic differences appear to be much less profound than inter-individual differences within a particular ethnic group [32]. However, some differences in skin lipid composition across ethnic groups have been reported, and it is suggested that these may influence the prevalence of skin disease and sensitivity [33].
No significant differences in SC thickness or protein content [25], or the dynamic friction coefficient of skin [34] were seen between genders, although it was reported that skin barrier func-tion was reduced in the days before the onset of menses [35].
Consequently, little consideration of the effects of age, ethnicity or gender on transdermal delivery has been given, although drug dosage and especially the potential for toxicity in children needs further examination.
Pathological effectsWhile many topical products are intended to be applied to dis-eased skin, most experimental studies on dermal absorption will be performed on healthy skin. This anomaly reinforces the need to obtain data that directly relates to the particular condition that is being treated. A very useful addition to this literature is a recent review by Chiang et al. [36]. This summarizes the available data on percutaneous absorption through skin that is damaged, for example, by tape stripping or abrasion, freezing or heating, delipidization, chemical irritation, UV irradiation, and in clinical diseases, including psoriasis, atopic dermatitis and skin cancers. In the majority of reports, increased flux of particular model penetrants was seen through damaged or diseased skin [36–39]. In addition to increased penetrant flux seen through affected skin in atopic dermatitis, a number of studies show a similar enhancement through uninvolved skin of the same atopic der-matitis patients [40–43]. Interestingly, Moan et al. reported greater permeation of aminolevulinic acid through mouse skin overlying tumors from an implanted human colon adenocarcinoma cell line than through normal uninvolved skin [44]. Unfortunately, there was no histological comparison of the skin from the different sites. However, if validated, this approach could lead to a useful method of tumor detection, particularly as the penetration of aminolevulinic acid or the appearance of its metabolic product, protoporphyrin IX, could be followed noninvasively by modern microscopic imaging techniques [45].
Advanced formulationGreat improvements in transdermal delivery, beyond what might be expected from a consideration of the properties of skin and the active molecule, can be achieved by an appropriate choice of vehicle and the type of formulation [46]. Vehicles can be important, as their effects on the skin can alter the interaction of the penetrant with the skin. For example, the authors have shown
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)386
Review
that a vehicle such as propylene glycol can alter the properties of the SC, so that the solubility of the active drug minoxidil in the membrane is increased [47]. The importance of membrane solubility was seen in other work with phenols, where it was found that their maximum flux through excised human skin was determined by their solubility in the SC, which was in turn influenced by the vehicle [48].
In addition to the components of the vehicle, it is worth remem-bering that often a simple change in properties, such as pH, vis-cosity, the relative amounts of oil, water or surfactant in emul-sions, droplet size, ionic nature or the method of preparation, can influence the process of skin absorption. Some of these properties will be discussed in this article. tablE 1 provides some examples of advanced formulations.
Type of formulationMany pharmaceutical forms are used as vehicles. The various types of formulations, such as emulsions (e.g., oil-in-water, water-in-oil, water-in-oil-in-water or oil-in-water-in-oil) or gels (hydrophilic, lipophilic or alcoholic) are important, among other things, to adapt the hydrophilicity or lipophilicity of the drug with the vehicle. The type of vehicle chosen will be determined by the properties of the penetrant and the intended target area. For example, Kurul and Hekimoglu compared different types of vehicles for their ability to cause skin permeation of the UV filters, the lipophilic oxybenzone (log P 3.8) and the relatively hydrophilic sulisobenzone (log P 0.4) [49]. The order of permea-tion seen with the different vehicles, from highest to lowest, was petrolatum >oil-in-water (o/w) emulsion >hydroxyethylcellulose gel for oxybenzone and the opposite for sulisobenzone (hydroxy-ethylcellulose gel >o/w emulsion >petrolatum). Therefore, to
minimize skin penetration, as required for a sunscreen, different vehicles were required for the different filters.
The proportions in which the same ingredients are mixed can determine the structural forms of the resulting formulation. For example, different proportions of ingredients such as PPG-5-Ceteth-20 (surfactant), dibutyl adipate (oily phase) and water can result in microemulsions, emulsions or liquid–crystal meso-phases. In vivo studies carried out in pigs showed that a hexagonal liquid crystal formulation was most effective in increasing skin permeation of caffeine [50].
Concentration of the components of the formulationThe tactile properties of topical formulations are important in determining product choice by consumers or for the adherence to treatment, with modern oil-in-water emulsions considered more acceptable than ointments. These features can be built in to a formulation without compromising its efficacy. For example, Wirén et al. investigated the effect of changes in vehicle lipid content of o/w emulsions containing two active ingredients: benzyl nicotinate and β-methasone valerate on erythema and blanching of human skin in vivo [51]. Enhanced efficacy of both active ingredients (erythema with benzyl nicotinate and blanching with β-methasone valerate) was seen with the emulsions with the lowest (10%) lipid content, indicating that products can be designed with both efficacy and tactile acceptability in mind.
Skin & formulation pHThe acid mantle of the skin has long been recognized [52]. The skin surface has a pH of approximately 4–6, and there is a gradi-ent towards the neutral pH of the interior extending far into the epidermis [53]. Disturbances in the acid mantle resulting in elevated
Table 1. Nanodelivery systems.
Technique Principle Deliverables Ref.
Nanoemulsion or microemulsion
System of water, oil and an amphiphile, which forms a single optically isotropic liquid solution
Plasmid DNA, ketoprofen, apomorphine, estradiol and lidocaine
[134–138]
Liposomes Vesicles formed by one or multiple lipid bilayers made of mixture of phospholipids
Cosmetics, antibiotics and vaccine adjuvants
[139–141]
Niosomes Mixtures of nonionic surfactants, cholesterol and phospholipids
Tretinoin, peptide drugs and zidovudine [142–144]
Ethosomes Increase skin penetration by increasing the elasticity of the lipidic vesicle; contain up to 20–45% ethanol
5-ALA, salbutamol, finasteride and anti-HIV therapy
[145–148]
Transfersomes Phospholipids with surfactants that act to provide vesicle elasticity and deformability
Vaccines, 5-fluorouracil, IL-2 and IFN-α [149–151]
SECosomes or nanosomes Mixture of surfactant, ethanol and cholesterol siRNA [121]
SLNs Produced with one single solid lipid and surfactants, with perfect crystalline lattice
CoQ-10, glucocorticoids, minoxidil and oxybenzone
[152–155]
NLCs Produced with solid and liquid lipids and surfactants, with distorted crystalline lattice
Targeted tumor delivery, phospholipase A2 inhibitors, benzocaine, lidocaine and psoriasis treatment
[156–159]
Polymeric nanoparticles Consist of micro- and nano-spheres or capsules developed to control the release of the entrapped drug
Chlorhexidine, indomethacin, melatonin and poorly soluble drugs
[160–163]
ALA: Aminolevulinic acid; NLC: Nanostructured lipid carrier; SECosome: Surfactant–ethanol–cholesterol-osome; SLN: Solid lipid nanoparticle.
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
387www.expert-reviews.com
Review
skin surface pH may be contributing factors in the etiology of skin diseases such as contact dermatitis, ichthyosis, psoriasis and atopic dermatitis [18]. The acid mantle confers an antimicrobial function to the skin barrier function, as well as supporting its physical defense [54]. As an example, aggregation of carboxylated polystyrene nanoparticles is promoted by acidic pH due to decreas-ing electrostatic forces, making them less likely to penetrate the skin [55].
The pH in the vehicle and the pH across the skin is important for the diffusion of drugs, because the acid and base properties of the drug influence the solubility and partitioning in the different skin layers and therefore, the penetration of the drug.
ViscosityIt is generally believed that viscous formulations reduce the dif-fusion coefficient of the molecule in the vehicle, thus retarding or eliminating its skin partitioning and absorption [56]. However, this may not always be the case, and careful examination of the experimental conditions is necessary if false interpretations of the data are to be avoided.
Cross et al. from the authors’ laboratory showed that thicker formulations impede the skin penetration of benzophenone-3 under infinite-dose conditions, whereas thin layers of more vis-cous formulations applied under ‘in-use’ conditions enhanced skin penetration [57]. This was believed to be due to the formation of an occlusive layer, which would have the effect of increasing SC hydration, leading to greater diffusivity of the penetrant through the SC. The authors noted that researchers need to be aware of the pitfalls of extrapolating results from infinite-dose experiments to real-life situations.
To understand how the viscosity of a formulation can affect the permeation of active compounds into the skin, Gallagher et al. studied the release of ketoprofen from a series of simple gels of increasing thickener content relative to solvent [58] and its penetration into and through pig skin [59]. While ketoprofen permeation and skin distribution was reduced as the viscosity of the gels increased, as expected, the authors showed that this could be attributed to increasing binding of the drug to the thickener, rather than to changes in viscosity.
ChargeThe final load of the emulsion is generally obtained according to the load of the primary surfactant. The surfactants may be ionic, nonionic or amphoteric. Nonionic surfactants may have better skin tolerance, and only in a very few specific cases, ampho-teric surfactants are used [60]. Cationic surfactants often allow improved skin penetration, as seen in the work of Klang et al. [61], which concerned corneal penetration of indomethacin, and of Kitagawa and Kasamaki [62], which concerned the permea-tion of anionic salicylate through excised guinea pig dorsal skin. On the other hand, cationic and anionic surfactants in various concentrations did not cause any enhancement of finasteride skin absorption in the work of Javadzadeh et al. [63]. Interpretation of these differences is complicated by the use of a range of different cosolvents and cosurfactants in the various formulations.
The importance of emulsion surface charge is seen in work by Klang et al. [61]. Using a nonionic emulsifier and varying the charge with a cationic surfactant and deoxycholic acid (anionic lipid), they prepared positively and negatively charged emulsions. The positively charged emulsion provided significantly higher corneal drug penetration than the negatively charged emulsion, probably by prolonging the residence time of the drop on the epithelial layer of the cornea.
Droplet size: nanoemulsionsThe mixing of oil, water and surfactant allows the formation of structures and variable systems depending on the characteristics and the proportion of components used. Systems microstructured as liquid crystals and microemulsions are used to encapsulate drugs and active ingredients in pharmaceutical and cosmetic products.
Owing to the ability to deliver the drug through the skin, the microemulsion system should be a promising drug carrier [64], with an expectation of providing a sustained, controlled and pro-longed formulation with higher bioavailability and lower toxic-ity than the conventional methods [65,66], as well as to penetrate membranes [67]. Thus, the bioavailability is expected to be much higher and vary less within and between individuals than the con-ventional formulations [66]. Moreover, these systems have already been shown to be effective in a wide range of formulations for most routes of administration including oral, topical and nasal.
The unique microstructure of these emulsions, containing both hydrophilic and hydrophobic components with nanometer-size, may allow a wide range of different molecules to be solubilized and delivered to the skin. Their transparency makes it possible to check that all components are completely solubilized and their thermodynamic stability allows them to be stored for long periods.
The mechanisms by which such emulsions are able to improve skin penetration have been investigated. Using the spectra from Fourier transform infrared spectrometry and the analysis of skin treated with specific nanoemulsions by differential scanning calorimetry, Shakeel et al. showed that celecoxib permeation occurred following extraction of SC lipids by the nanoemulsion [68]. The significant decrease in activation energy for permeation across rat skin indicates that the SC lipid bilayers were significantly disrupted and photomicrographs showed the disruption and extraction of lipid bilayers as distinct voids. Pharmacokinetic studies revealed significantly greater extent of absorption than the oral capsule formulation. Recent studies with nanoformulation of drugs with chitosan nanoparticles applied to cell monolayers also showed membrane disruption caused by electrostatic interactions with paracellular proteins, resulting in the opening of tight junctions [69]. Different therapeutic drugs with different physicochemical properties could be loaded into nanosystems using a combinatorial approach, suggesting that dextran nanoformulations based on combinatorial principles show promise for the delivery of a wide array of anticancer drugs [70].
Chemical enhancement of skin permeationAs discussed earlier, under normal conditions, the number of com-pounds able to penetrate the skin barrier to a significant degree
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)388
Review
is limited. A commonly used approach to increase the range of available compounds or to enhance the penetration of a particular compound is to apply a chemical penetration enhancer. These are substances that alter the properties of the skin, and the mechanisms by which this can occur include: disruption of the lipid bilayer structure, extraction of the SC lipids, increased partitioning and solubility in the SC, alteration of SC hydration, thereby chang-ing the solubility of the drug, and interaction with corneocyte keratin [19].
An effective skin penetration enhancer should satisfy the fol-lowing requirements: it should be odorless and colorless; it should be specific in its mode of action; it should be pharmacologically inert; it should be compatible with drugs and other excipients; it should be chemically and physically stable; it should be non-allergenic, nonirritant and nontoxic; its effect on the skin barrier should be reversible and it should give a rapid effect for a predict-able duration of time. However, it is unlikely that a particular compound would be able to meet all these criteria.
Penetration enhancers may be natural products, such as terpe-nes or fatty acids, or synthetic materials. Some examples of perme-ation enhancers are alcohols, terpenes, dimethyl isosorbide, urea and derivatives, azone and derivatives, fatty acids, phospholipids, propylene glycol and isopropyl myristate [71,72].
A key issue to consider in the choice of a penetration enhancer is safety, and consequently, there are relatively few in common use with well-understood properties. New, high-throughput screening methods based on electrical conductivity [73] or resistance [74] have been developed to rapidly evaluate panels of chemicals for high enhancement efficiency and a low skin irritation potential.
Synergistic effects, probably resulting from the combined effects of two substances acting by different mechanisms, have been demonstrated for a number of combinations, including azone, terpenes, oleic acid or urea analogues and cosolvents such as pro-pylene glycol, transcutol or alcohols. It is likely that cosolvents such as propylene glycol act to increase the concentration of both the permeant and the enhancer in the SC [19,75].
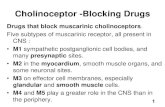
Physical enhancement techniquesVarious physical techniques may be applied before or during topi-cal application to enhance skin penetration. These can be catego-rized according to their effect on the skin (tablE 2). Mechanical methods such as dermal abrasion and tape stripping reduce the SC thickness, while flexing, stretching or massage weaken the bar-rier generally. Direct injection techniques (microneedles and jet propulsion) bypass the SC barrier. Ablative or cavitational tech-niques introduce pores at specific sites by applying energy (thermal, ultrasound, radiofrequency and others) directly to the skin. Finally, techniques such as iontophoresis, magnetophoresis and noncavi-tational ultrasound increase the driving force on the penetrant molecule. As will be seen, each technique has advantages that can make it more suited to specific purposes, as well as disadvantages. Combinations of physical enhancement with optimized formula-tion, including chemical enhancers, are promising strategies that are likely to be increasingly employed.
Direct injection with microneedlesMicroneedles are designed to bypass the skin barrier to deliver pre-cise payload doses to a specific depth and location in the skin. The ability to carry high molecular weight (MW) substances gives them an advantage over conventional delivery methods. Consequently, given the abundant immune cells in the skin [76], most of the suc-cessful applications to date are for vaccine delivery [77–80]. An expo-nential increase in patent applications and peer-reviewed literature in the area of microneedles has occurred since the first patent appli-cation from Alza Corporation (CA, USA) in 1976 [201]. Part of this expansion has been due to advances in fabrication techniques, fuelled by increasing funding. Fabrication of microneedles allows diverse designs to be developed, including dry-coated solid needles [77,81,82], hollow [83,84] or dissolvable polymeric microneedles [85–87]. However, microneedles can also have cost, adherence and safety issues. As with any invasive procedure, there is a potential for local irritation or infection at the application site, or local cell death, as seen with other invasive technologies [88].
Table 2. Physical and electrical enhancement techniques.
Technique Principle Deliverables Ref.
Direct injection with microneedles
Deliver substances with the efficacy of a needle on a transdermal patch
Vaccines for influenza, Chikengunya virus, human papillomavirus, herpes simplex virus and West Nile virus
[77–80,82–88,164]
Cavitation technologies
Electroporation Application of micro- to milli-second electrical pulses to create transient aqueous pores in lipid bilayer
Insulin and vaccines [94,96]
Phonophoresis or sonophoresis
Enhanced delivery by low-frequency ultrasound energy increases lipid fluidity
Insulin, ketoprofen and vaccines [93,95,165]
Increased driving force technologies
Iontophoresis Transdermal delivery by a small direct current Charged molecules, peptides, proteins and indomethacin
[97,98,166]
Dermaportation or magnetophoresis
Delivery using static or variable magnetic fields Benzoic acid, terbutaline sulfate, 5-ALA, Ala–Trp (dipeptide) and naltrexone
[100–104]
ALA: Aminolevulinic acid.
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
389www.expert-reviews.com
Review
Cavitational technologiesThese include thermal ablation (using heating elements, lasers and radiofrequencies), electroporation (high-voltage pulses) and low-frequency ultrasound (also referred to as sonophoresis or phonophoresis). These various energy forms are applied to the skin to eliminate the SC at discrete sites, introducing aqueous cavitational pores or microchannels. This makes such techniques particularly suitable for the transport of relatively hydrophilic macromolecules, including proteins. Examples of enhanced deliv-ery of macromolecules with these technologies include human growth hormone (radiofrequencies) [89]; gene transfer (lasers) [90]; insulin by pulsed laser [91], sonophoresis [92] or electroporation [93]; vaccines by sonophoresis [94] or electroporation [95]. Disadvantages of cavitational techniques include the possibility of infection due to open pores and pain (particularly with electroporation). While attempts have been made to commercialize these technologies, little success has been achieved.
Increased driving force technologiesThese include iontophoresis (electric current) and dermaportation (or magnetophoresis, using static or variable magnetic fields). Iontophoresis uses small electric currents to repel charged mol-ecules. It is particularly effective in driving small water-soluble ionic drugs through the SC, an outcome very difficult to achieve for such compounds under passive conditions. In addition to enhancing the delivery of low MW substances, iontophoresis was seen to be successful with larger peptides and proteins [96,97]. In addition to the direct repulsion mechanism, there are two other mechanisms that contribute to increased skin flux under iontophoresis: electro-osmotic effects on unionized but polar spe-cies and increased permeabilization of the skin as a result of the electric current. Along with sonophoresis, iontophoresis is one of the few transdermal delivery technologies with clearly identifi-able clinical applications, and it is the only one to produce US FDA-approved products [98].
Early work by Murthy and Hiremath reported that static mag-netic fields were able to increase penetration of topically applied benzoic acid and terbutaline sulfate in vitro and in vivo in guinea pigs and humans [99,100]. They suggested that the magnetic fields increased the driving force on the molecules and caused a tem-porary alteration in skin structure. More recently, work from Australia has found an enhanced penetration of 5-aminolevulinic acid [101], a dipeptide, Ala–Trp [102], and naltrexone [103] through excised human epidermis with application of pulsatile magnetic fields. In addition, the magnetic fields caused enhanced penetra-tion of 10-nm gold nanoparticles into the viable epidermis of excised human full-thickness skin [103]. Work from this group is continuing with static magnetic fields generated by thin films that could be easily incorporated into a multifunctional transder-mal patch. These magnetic technologies offer clear commercial advantages as they are small and flexible, easily incorporated into devices and unlikely to contribute to adverse skin effects. Further work is needed to verify these observations for molecules with a wider range of properties and to elucidate the mechanisms that might be responsible for the reported effects. A 2011 report from
the Murthy group suggested that magnetic field-mediated pen-etration enhancement might be occurring though an appendageal pathway [104].
Flexing & massageConditions such as mechanical flexing and massage are encoun-tered in everyday life and their effects on skin penetration have been investigated, particularly for particles. While the focus of this review is drug delivery, topically applied particles are relevant because of their potential as drug carriers, particularly for fol-licular delivery [105]. The first evidence of the effects of flexing came from Tinkle et al. in 2003 [106]. Using confocal microscopy, they showed that 60 min of mechanical flexing of excised human skin caused small numbers of 0.5 and 1 µm, but not 2 or 4 µm, fluorescein isothiocyanate-conjugated dextran beads to penetrate into the epidermis and dermis. They also demonstrated rapid bead accumulation in regions where the SC was discontinuous and significant penetration into the deeper layers when the SC was tape stripped. By contrast, work from this laboratory repli-cating the flexing apparatus and conditions of Tinkle et al., with excised human skin treated with 35-nm zinc oxide nanoparticles, has been unable to demonstrate skin penetration [Sanchez WH, Prow
TW, Sarkar M, Grice JE, Roberts MS, Unpublished Data]. Later, detailed studies by the Monteiro-Riviere group carried out in dermatomed porcine rather than human skin showed that after mechanical flexing, 3.5-nm modified fullerenes were detected in the intercel-lular regions of the epidermis and the dermis [107]. The lack of conclusive evidence available from the contrasting in vitro results increases the need for in vivo studies in humans to shed light on the effect of flexing under normal conditions, for example, with sunscreens containing zinc oxide and titanium dioxide micro- or nano-particles.
The hair follicle is an important drug delivery site as it is easily accessible, supported by a dense blood capillary bed and is closely associated with dendritic and stem cells [108]. It can also be preferentially targeted, as seen in work from this labora-tory, where the authors showed preferential follicular delivery of caffeine in vivo [109] at early times, as well as formulation-dependent minoxidil penetration in vitro [47]. The Lademann group has pioneered much of the work on follicular drug pen-etration using nano- or micro-particles as drug carriers [105], advancing the approach that follicles can be used as reservoirs and targets for drug, immune or gene therapy. They showed that 40-nm nanoparticles were taken up directly by Langerhans cells surrounding the follicles when hair shafts were removed [110]. With massage, they found deep follicular penetration of particles with an optimal size of approximately 300–600 nm, corresponding roughly to the cuticula thickness of vellus and terminal hairs (530 and 320 nm in human and porcine skin, respectively) [111]. They hypothesized that this was due to the cuticulae acting as ‘gears’ to force matching sized particles into the follicles as the hairs move under massage. It is envisaged that a combination of a nano-based delivery system with a sim-ple physical technique such as massage will lead to enhanced therapeutic treatments.
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)390
Review
Tape strippingA simple means of increasing skin penetration of a solute or parti-cle is to gradually reduce or eliminate the SC barrier by the appli-cation and removal of adhesive tape on the skin (tape stripping). The first studies using this technique were done in the early 1970s [112–114]. Flux may be increased as a result of a reduced SC thick-ness, or a penetrant may have direct access to the viable epidermis on complete elimination of the SC. As the SC thickness is reduced, there is increased water loss across the membrane, indicated by increased TEWL [115]. There is also evidence that reducing the SC thickness by tape stripping effectively expands the possible size range of penetrants, as Tsai et al. demonstrated that the MW cutoff for skin penetration of polyethylene glycol oligomers increased in parallel with barrier disruption, shown by increasing TEWL as the skin was tape stripped [116]. While tape stripping is a useful investigatory tool for examining mechanisms of skin penetration and can also be used to sample penetrants retained in the SC in order to obtain depth or kinetic profiles, it has little practical or commercial value as a drug delivery technique.
Nanodelivery systemsIn recent years, the field of nanomaterial-based drug delivery to the skin has progressed to a point where there are well-characterized tools such as solid or flexible lipid nanoparticles and dendrimers that have the capacity for customized or targeted delivery. There are nanoparticles to increase or decrease the flux, customize the drug depot location and size, and even to selectively permeabilize the SC [55]. To further enhance skin permeation of encapsulated molecules, newer particles such as niosomes, ethosomes and trans-fersomes have been developed to improve some of the features of liposomes.
Liposomes are generally made of mixtures of phospholipids, or phospholipids and cholesterol. They are vesicles formed by one or multiple lipid bilayers that enclose an aqueous environ-ment. Liposome deformability depends inversely on the amount of cholesterol in their composition and they can be negatively or positively charged [117]. Niosomes are made of mixtures of nonionic surfactants, cholesterol and, sometimes, small amounts of phospholipids, and were developed to increase the stability of liposomes. These particles are rigid and may be negatively or positively charged [118]. Ethosomes, containing up to 20–45% of ethanol, were designed to increase skin penetration by increasing the elasticity of the lipidic vesicle. Their lipid bilayers are fluid and these particles are generally negatively charged [119]. Transfersomes are made of phospholipids supplemented with surfactants that act as edge activators to provide vesicle elasticity and deformability. They are ultradeformable and generally negatively charged [56,120].
In 2010, Geusens et al. developed nanosomes, called sur-factant–ethanol–cholesterol-osomes (SECosomes), which showed excellent size, surface charge, morphology, deformability, trans-fection efficiency, stability and skin penetration capacity after complexation with siRNA [121]. The increased flexibility in these particles greatly enhances their ability to cross the intact human epidermal membrane and to unload their payload into targeted epidermal cells.
Further advances in fabrication technology and in the under-standing of how nanoparticles interact with the SC barrier, the gross features of the skin such as furrows and its appendages will be essential for the development of viable nano-based drug deliv-ery systems. This information, along with an understanding of the sequestration and elimination kinetics from reservoirs such as furrows and appendages, will allow nanocarriers to be designed with specific properties for accurate delivery of payloads in useful doses to cellular targets. At the same time, it is essential that toxi-cological effects of nano-based delivery systems are understood before regulators can approve their widespread use [55].
Analysis of skin penetrationIn vivo–in vitro correlationAs discussed earlier, it is not often practical, or even possible, to evaluate the skin permeation of new drugs or therapeutics, cos-metics or diagnostic substances in human subjects, even though they are the intended recipients of such treatments. Consequently, other experimental systems must be used, including live ani-mal models, which are becoming increasingly inaccessible, and in vitro human and animal skin and cell preparations. A vital assumption in this approach is that the chosen models are valid and that the in vitro predictions correlate with the expected in vivo findings.
A recent review of the available literature compared in vitro measurements of percutaneous absorption in excised skin with in vivo results [122]. The authors concluded that provided the in vitro studies were tightly controlled so that they adequately duplicated in vivo conditions, there was an excellent correlation between the two sets of results. However, difficulties may arise when interpreting the validity of literature reports of in vitro stud-ies, which may not have been sufficiently well controlled. In par-ticular, they stressed the importance of using skin from identical body sites and vehicles of identical composition and dose.
Skin modelsAs in vitro experiments are less expensive, offering more options to vary application parameters and causing less ethical problems, most skin diffusion experiments have been performed using these methods. Due to the limited availability of excised human skin for regulatory or practical reasons, rat or pig skin is often used, although excised skin from other mammalian species may suffice. Pig skin shows similarity to human skin in terms of morphology and permeability characteristics while rat skin may be used because the majority of regulatory toxicity studies are carried out in this species. However, animal skin shows differences in permeability to human skin and is often more permeable [123,124], which might result in overestimating human percutaneous skin absorption. The successful development of reconstructed human epidermis was intended to be an alternative tool for percutaneous absorp-tion testing. So far, experiments utilizing bioengineered epidermis equivalents resulted in overestimation of skin penetration [125,126]. However, it must always be recognized that the best model for human skin penetration is human skin. If excised human skin is available, experiments may be performed in diffusion cells. The
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
391www.expert-reviews.com
Review
ReferencesPapers of special note have been highlighted as:• of interest
1 Hadgraft J, Lane ME. Transepidermal water loss and skin site: a hypothesis. Int. J. Pharm. 373(1–2), 1–3 (2009).
2 Grice JE, Prow TW, Kendall MA, Roberts MS. Electrical and physical methods of skin penetration enhancement. In: Topical and Transdermal Drug Delivery and Development. Watkinson AC, Benson HA
(Eds). John Wiley & Sons Inc., NJ, USA, 43–65 (2012).
3 Roberts MS, Cross SE, Pellett MA. Skin transport. In: Dermatological and Transdermal Formulations. Walters KA (Ed.). Marcel Dekker Inc., NY, USA, 89–196 (2002).
• Comprehensivereviewcoveringtransportpathwaysthroughthestratumcorneum,withmathematicalmodelingofdiffusionprocesses.
4 Magnusson BM, Anissimov YG, Cross SE, Roberts MS. Molecular size as the main determinant of solute maximum flux across the skin. J. Invest. Dermatol. 122(4), 993–999 (2004).
5 Anissimov YG, Roberts MS. Diffusion modeling of percutaneous absorption kinetics. 1. Effects of flow rate, receptor sampling rate, and viable epidermal resistance for a constant donor concentration. J. Pharm. Sci. 88(11), 1201–1209 (1999).
Key issues
• The stratum corneum forms an effective barrier to the penetration of most exogenous substances, with only a limited number of small (<500 Da), relatively lipophilic molecules able to penetrate skin by passive diffusion, with limited payloads.
• To overcome some of these limitations, a range of chemical and physical enhancement techniques has been used.
• Recently, innovative micro- and nano-based delivery systems have been investigated for targeted cellular delivery, for applications such as gene therapy, vaccination and cancer diagnosis.
• Adverse effects such as chemical toxicity, infection and cellular or DNA damage need to be considered when penetration enhancement techniques are used.
development of noninvasive imaging techniques, exemplified in a recent review from this laboratory [45], improves the ability to study real-life, in-use situations.
In vivoBy 2013, the EU has committed to eliminating animal testing for cosmetics, thereby giving greater prominence to in vivo study in humans, particularly those that can be carried out noninvasively.
For noninvasive human studies, imaging technologies such as confocal laser scanning microscopy and multiphoton tomogra-phy/fluorescence lifetime imaging microscopy are being used to visualize the penetration of fluorescent materials and to image the effect of the physical enhancement technologies on meta-bolic processes occurring in the skin itself. They can provide morphological and biochemical information about the skin by detecting auto fluorescence from endogenous skin fluorophores with little damage to the tissue, particularly with multiphoton tomography [127,128]. Similar imaging studies can also be carried out with freshly excised skin for short periods following exci-sion [129]. Fluorescence lifetime imaging is used in conjunction with multiphoton tomography to provide information about the state or environment of a particular fluorophore, being useful in assessing the effects of physical treatments [130,131]. Time-correlated single photon counting has the potential for enabling studies on exposure and metabolic consequences of nanoparticle-containing topical products in human subjects without the need for painful biopsies or destructive analysis. Lin et al. evaluated time-correlated single photon counting for simultaneous monitoring of zinc oxide nanoparticles and the metabolic state such as NAD(P)H changes in volunteer skin [132].
Another recent imaging technology is confocal Raman spectroscopy, which provides real-time noninvasive in vivo imaging of penetrants and skin components, based on their
specific infrared-Raman signature. It can be used for quantitative estimation of skin penetrants [133].
Expert commentaryTopical application of substances for therapeutic, prophylactic and cosmetic purposes attracts great interest from research and com-mercial points of view and considerable understanding of the key properties of skin, the penetrant and the vehicle has been gained over the past 50 years. The range of compounds that are avail-able for the transdermal route is limited and a good deal of effort has gone into expanding that range, finding ways to enhance the penetration of difficult substances such as hydrophilic compounds or macromolecules, efficient targeting to specific cellular targets and reducing adverse skin reactions. Chemical and physical meth-ods, or combinations of these technologies, have been applied, with varying success, to achieve these goals. Much of the recent research has concentrated on the use of advanced delivery systems based on solid or flexible nanomaterials to deliver payloads that were previously impossible, such as vaccines, gene fragments and therapeutic proteins.
Five-year viewThe key advance in transdermal delivery that will come in the next 5 years is specific cell targeting for therapeutic, prophylactic, diagnostic or cosmetic purposes. In the near future, nano-based drug delivery systems, possibly combined with physical enhance-ment techniques such as iontophoresis, sonophoresis or magneto-phoresis, will allow enhanced delivery of a wide range of poorly penetrating substances to specific targets in the skin, including stem cells found in the hair follicle bulge region, tumor cells and antigen-screening Langerhans cells. These techniques will also allow the accurate delivery of stains for in situ tumor recognition to aid diagnosis and definition of tumor margins.
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)392
Review
6 Higuchi T. Rate of release of medicaments from ointment bases containing drugs in suspension. J. Pharm. Sci. 50, 874–875 (1961).
7 Mitragotri S, Anissimov YG, Bunge AL et al. Mathematical models of skin permeability: an overview. Int. J. Pharm. 418(1), 115–129 (2011).
8 Potts RO, Guy RH. Predicting skin permeability. Pharm. Res. 9(5), 663–669 (1992).
• Themostwidelyacceptedalgorithmforpredictingskindiffusionparameterswasdevelopedinthisstudy.
9 Potts RO, Guy RH. A predictive algorithm for skin permeability: the effects of molecular size and hydrogen bond activity. Pharm. Res. 12(11), 1628–1633 (1995).
10 Winsor T, Burch GE. Differential roles of layers of human epigastric skin on diffusion rate of water. Arch. Intern. Med. (Chic.) 74(6), 428–436 (1944).
11 Blank IH. Further observations on factors which influence the water content of the stratum corneum. J. Invest. Dermatol. 21(4), 259–271 (1953).
12 Fluhr JW, Feingold KR, Elias PM. Transepidermal water loss reflects permeability barrier status: validation in human and rodent in vivo and ex vivo models. Exp. Dermatol. 15(7), 483–492 (2006).
13 Tagami H, Yoshikuni K. Interrelationship between water-barrier and reservoir functions of pathologic stratum corneum. Arch. Dermatol. 121(5), 642–645 (1985).
14 Werner Y, Lindberg M. Transepidermal water loss in dry and clinically normal skin in patients with atopic dermatitis. Acta Derm. Venereol. 65(2), 102–105 (1985).
15 Grubauer G, Feingold KR, Harris RM, Elias PM. Lipid content and lipid type as determinants of the epidermal permeability barrier. J. Lipid Res. 30(1), 89–96 (1989).
16 Elias PM, Friend DS. The permeability barrier in mammalian epidermis. J. Cell Biol. 65(1), 180–191 (1975).
• RepresentativeofthemajorcontributionofEliastothebiologyoftheskinbarrier.
17 Swartzendruber DC, Wertz PW, Kitko DJ, Madison KC, Downing DT. Molecular models of the intercellular lipid lamellae in mammalian stratum corneum. J. Invest. Dermatol. 92(2), 251–257 (1989).
18 Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Exp. Dermatol. 17(12), 1063–1072 (2008).
19 Benson HA. Transdermal drug delivery: penetration enhancement techniques. Curr. Drug Deliv. 2(1), 23–33 (2005).
20 Leite E Silva VR, Schulman MA, Ferelli C et al. Hydrating effects of moisturizer active compounds incorporated into hydrogels: in vivo assessment and comparison between devices. J. Cosm. Dermatol. 8(1), 32–39 (2009).
21 Benson HAE. Skin structure, function, and permeation. In: Topical and Transdermal Drug Delivery and Development. Watkinson AC, Benson HA (Eds). John Wiley & Sons Inc., NJ, USA, 3–22 (2012).
22 Kleesz P, Darlenski R, Fluhr JW. Full-body skin mapping for six biophysical parameters: baseline values at 16 anatomical sites in 125 human subjects. Skin Pharmacol. Physiol. 25(1), 25–33 (2012).
23 Batisse D, Bazin R, Baldeweck T, Querleux B, Lévêque JL. Influence of age on the wrinkling capacities of skin. Skin Res. Technol. 8(3), 148–154 (2002).
24 Lober CW, Fenske NA. Photoaging and the skin: differentiation and clinical response. Geriatrics 45(4), 36–40, 42 (1990).
25 Voegeli R, Rawlings AV, Doppler S, Heiland J, Schreier T. Profiling of serine protease activities in human stratum corneum and detection of a stratum corneum tryptase-like enzyme. Int. J. Cosmet. Sci. 29(3), 191–200 (2007).
26 Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J. Am. Acad. Dermatol. 15(4 Pt 1), 571–585 (1986).
27 Roskos KV, Bircher AJ, Maibach HI, Guy RH. Pharmacodynamic measurements of methyl nicotinate percutaneous absorption: the effect of aging on microcirculation. Br. J. Dermatol. 122(2), 165–171 (1990).
28 Roskos KV, Guy RH. Assessment of skin barrier function using transepidermal water loss: effect of age. Pharm. Res. 6(11), 949–953 (1989).
29 Giusti F, Martella A, Bertoni L, Seidenari S. Skin barrier, hydration, and pH of the skin of infants under 2 years of age. Pediatr. Dermatol. 18(2), 93–96 (2001).
30 Berardesca E, Maibach HI. Racial differences in sodium lauryl sulphate induced cutaneous irritation: black and white. Contact Derm. 18(2), 65–70 (1988).
31 Kompaore F, Marty JP, Dupont C. In vivo evaluation of the stratum corneum barrier function in blacks, Caucasians and Asians with two noninvasive methods. Skin Pharmacol. 6(3), 200–207 (1993).
32 Warrier GA, Kligman AM, Harper RA et al. A comparison of black and white skin using noninvasive methods. J. Soc. Cosmet. Chem. 47, 229–240 (1996).
33 Muizzuddin N, Hellemans L, Van Overloop L, Corstjens H, Declercq L, Maes D. Structural and functional differences in barrier properties of African American, Caucasian and East Asian skin. J. Dermatol. Sci. 59(2), 123–128 (2010).
34 Cua AB, Wilhelm KP, Maibach HI. Frictional properties of human skin: relation to age, sex and anatomical region, stratum corneum hydration and transepidermal water loss. Br. J. Dermatol. 123(4), 473–479 (1990).
35 Muizzuddin N, Marenus KD, Schnittger SF, Sullivan M, Maes DH. Effect of systemic hormonal cyclicity on skin. J. Cosmet. Sci. 56(5), 311–321 (2005).
36 Chiang A, Tudela E, Maibach HI. Percutaneous absorption in diseased skin: an overview. J. Appl. Toxicol. 8, 537–563 (2012).
37 Aalto-Korte K, Turpeinen M. Quantifying systemic absorption of topical hydrocortisone in erythroderma. Br. J. Dermatol. 133(3), 403–408 (1995).
38 Colombo G, Zucchi A, Allegra F, Colombo P, Zani F, Santi P. In vitro and in vivo study of 5-methoxypsoralen skin concentration after topical application. Skin Pharmacol. Appl. Skin Physiol. 16(2), 130–136 (2003).
39 Smits T, Robles CA, van Erp PE, van de Kerkhof PC, Gerritsen MJ. Correlation between macroscopic fluorescence and protoporphyrin IX content in psoriasis and actinic keratosis following application of aminolevulinic acid. J. Invest. Dermatol. 125(4), 833–839 (2005).
40 Hata M, Tokura Y, Takigawa M et al. Assessment of epidermal barrier function by photoacoustic spectrometry in relation to its importance in the pathogenesis of atopic dermatitis. Lab. Invest. 82(11), 1451–1461 (2002).
41 Jakasa I, de Jongh CM, Verberk MM, Bos JD, Kezic S. Percutaneous penetration of sodium lauryl sulphate is increased in uninvolved skin of patients with atopic dermatitis compared with control subjects. Br. J. Dermatol. 155(1), 104–109 (2006).
42 Jakasa I, Verberk MM, Esposito M, Bos JD, Kezic S. Altered penetration of polyethylene glycols into uninvolved skin of atopic dermatitis patients. J. Invest. Dermatol. 127(1), 129–134 (2007).
43 Ortiz PG, Hansen SH, Shah VP, Menné T, Benfeldt E. The effect of irritant dermatitis on cutaneous bioavailability of a
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
393www.expert-reviews.com
Review
metronidazole formulation, investigated by microdialysis and dermatopharmacokinetic method. Contact Derm. 59(1), 23–30 (2008).
44 Moan J, Ma LW, Iani V. On the pharmacokinetics of topically applied 5-aminolevulinic acid and two of its esters. Int. J. Cancer 92(1), 139–143 (2001).
45 Roberts MS, Dancik Y, Prow TW et al. Non-invasive imaging of skin physiology and percutaneous penetration using fluorescence spectral and lifetime imaging with multiphoton and confocal microscopy. Eur. J. Pharm. Biopharm. 77(3), 469–488 (2011).
• Acomprehensivereviewoftheuseofnoninvasivemicroscopicimagingtechniques,particularlytheuseoffluorescencelifetimeimagingindescribinginteractionsbetweenfluorescentmoleculesandtheirenvironment,suchastheskin.
46 Otto A, du Plessis J, Wiechers JW. Formulation effects of topical emulsions on transdermal and dermal delivery. Int. J. Cosmet. Sci. 31(1), 1–19 (2009).
47 Grice JE, Ciotti S, Weiner N, Lockwood P, Cross SE, Roberts MS. Relative uptake of minoxidil into appendages and stratum corneum and permeation through human skin in vitro. J. Pharm. Sci. 99(2), 712–718 (2010).
48 Zhang Q, Li P, Roberts MS. Maximum transepidermal flux for similar size phenolic compounds is enhanced by solvent uptake into the skin. J. Control. Release 154(1), 50–57 (2011).
49 Kurul E, Hekimoglu S. Skin permeation of two different benzophenone derivatives from various vehicles. Int. J. Cosmet. Sci. 23(4), 211–218 (2001).
50 Longo DP. [Collection, characterization and release studies; in vitro and in vivo permeation of microstructured systems containing caffeine]. PhD thesis, São Paulo State University ‘Julio de Mesquite Filho’, São Paulo, Brazil (2006).
51 Wirén K, Frithiof H, Sjöqvist C, Lodén M. Enhancement of bioavailability by lowering of fat content in topical formulations. Br. J. Dermatol. 160(3), 552–556 (2009).
52 Goodman H. The acid mantle of the skin surface. Ind. Med. Surg. 27(2), 105–108 (1958).
53 Dikstein S, Zlotogorski A. Measurement of skin pH. Acta Derm. Venereol. Suppl. (Stockh.) 185, 18–20 (1994).
54 Schmid-Wendtner MH, Korting HC. The pH of the skin surface and its impact on the
barrier function. Skin Pharmacol. Physiol. 19(6), 296–302 (2006).
55 Prow TW, Grice JE, Lin LL et al. Nanoparticles and microparticles for skin drug delivery. Adv. Drug Deliv. Rev. 63(6), 470–491 (2011).
56 Baroli B. Penetration of nanoparticles and nanomaterials in the skin: fiction or reality? J. Pharm. Sci. 99(1), 21–50 (2010).
57 Cross SE, Pugh WJ, Hadgraft J, Roberts MS. Probing the effect of vehicles on topical delivery: understanding the basic relationship between solvent and solute penetration using silicone membranes. Pharm. Res. 18(7), 999–1005 (2001).
58 Gallagher SJ, Trottet L, Carter TP, Heard CM. Effects of membrane type and liquid/liquid phase boundary on in vitro release of ketoprofen from gel formulations. J. Drug Target. 11(6), 373–379 (2003).
59 Gallagher SJ, Heard CM. Solvent content and macroviscosity effects on the in vitro transcutaneous delivery and skin distribution of ketoprofen from simple gel formulations. Skin Pharmacol. Physiol. 18(4), 186–194 (2005).
60 Kumar KS, Kumar PM, Kumar KA et al. A new three-component reaction: green synthesis of novel isoindolo[2,1-a]quinazoline derivatives as potent inhibitors of TNF-α. Chem. Commun. (Camb.) 47(17), 5010–5012 (2011).
61 Klang S, Abdulrazik M, Benita S. Influence of emulsion droplet surface charge on indomethacin ocular tissue distribution. Pharm. Dev. Technol. 5(4), 521–532 (2000).
62 Kitagawa S, Kasamaki M. Enhancement effects of double-chained cationic surfactants of n-dimethyldialkylammoniums on permeability of salicylate through guinea pig dorsal skin. Chem. Pharm. Bull. 50(10), 1370–1372 (2002).
63 Javadzadeh Y, Shokri J, Hallaj-Nezhadi S, Hamishehkar H, Nokhodchi A. Enhancement of percutaneous absorption of finasteride by cosolvents, cosurfactant and surfactants. Pharm. Dev. Technol. 15(6), 619–625 (2010).
64 Kreilgaard M. Influence of microemulsions on cutaneous drug delivery. Adv. Drug Deliv. Rev. 54(Suppl. 1), S77–S98 (2002).
65 Chen H, Chang X, Weng T et al. A study of microemulsion systems for transdermal delivery of triptolide. J. Control. Release 98(3), 427–436 (2004).
66 Garti N, Anserin A. Microemulsions for solubilization and delivery of nutraceuticals and drugs. In: Microencapsulation: Methods and Industrial Applications. Benita S (Ed.).
Taylor & Francis Group, NY, USA, 345–428 (2006).
67 Kogan A, Garti N. Microemulsions as transdermal drug delivery vehicles. Adv. Colloid Interface Sci. 123–126, 369–385 (2006).
68 Shakeel F, Baboota S, Ahuja A, Ali J, Shafiq S. Skin permeation mechanism and bioavailability enhancement of celecoxib from transdermally applied nanoemulsion. J. Nanobiotechnology 6, 8 (2008).
69 Sadighi A, Ostad SN, Rezayat SM, Foroutan M, Faramarzi MA, Dorkoosh FA. Mathematical modelling of the transport of hydroxypropyl-β-cyclodextrin inclusion complexes of ranitidine hydrochloride and furosemide loaded chitosan nanoparticles across a Caco-2 cell monolayer. Int. J. Pharm. 422(1–2), 479–488 (2012).
70 Abeylath SC, Amiji MM. ‘Click’ synthesis of dextran macrostructures for combinatorial-designed self-assembled nanoparticles encapsulating diverse anticancer therapeutics. Bioorg. Med. Chem. 19(21), 6167–6173 (2011).
71 Trommer H, Neubert RH. Overcoming the stratum corneum: the modulation of skin penetration. A review. Skin Pharmacol. Physiol. 19(2), 106–121 (2006).
72 Williams AC, Barry BW. Penetration enhancers. Adv. Drug Deliv. Rev. 56(5), 603–618 (2004).
73 Karande P, Jain A, Mitragotri S. Relationships between skin’s electrical impedance and permeability in the presence of chemical enhancers. J. Control. Release 110(2), 307–313 (2006).
74 Rachakonda VK, Yerramsetty KM, Madihally SV, Robinson RL Jr, Gasem KA. Screening of chemical penetration enhancers for transdermal drug delivery using electrical resistance of skin. Pharm. Res. 25(11), 2697–2704 (2008).
75 Gu S, Gao J, Hou X et al. Effects of penetration enhancers on Shuangwu traumatic formula: in vitro percutaneous absorption and in vivo pharmacodynamic evaluation of an herb medicine. Eur. J. Pharm. Biopharm. 73(3), 385–390 (2009).
76 Fernando GJ, Chen X, Prow TW et al. Potent immunity to low doses of influenza vaccine by probabilistic guided micro-targeted skin delivery in a mouse model. PLoS ONE 5(4), e10266 (2010).
77 Chen X, Prow TW, Crichton ML et al. Dry-coated microprojection array patches for targeted delivery of immunotherapeutics to the skin. J. Control. Release 139(3), 212–220 (2009).
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)394
Review
78 Corbett HJ, Fernando GJ, Chen X, Frazer IH, Kendall MA. Skin vaccination against cervical cancer associated human papillomavirus with a novel micro-projection array in a mouse model. PLoS ONE 5(10), e13460 (2010).
79 Prow TW, Chen X, Prow NA et al. Nanopatch-targeted skin vaccination against West Nile virus and Chikungunya virus in mice. Small 6(16), 1776–1784 (2010).
80 Quan FS, Kim YC, Yoo DG, Compans RW, Prausnitz MR, Kang SM. Stabilization of influenza vaccine enhances protection by microneedle delivery in the mouse skin. PLoS ONE 4(9), e7152 (2009).
81 Gill HS, Söderholm J, Prausnitz MR, Sällberg M. Cutaneous vaccination using microneedles coated with hepatitis C DNA vaccine. Gene Ther. 17(6), 811–814 (2010).
82 Koutsonanos DG, del Pilar Martin M, Zarnitsyn VG et al. Transdermal influenza immunization with vaccine-coated microneedle arrays. PLoS ONE 4(3), e4773 (2009).
83 Morefield GL, Tammariello RF, Purcell BK et al. An alternative approach to combination vaccines: intradermal administration of isolated components for control of anthrax, botulism, plague and staphylococcal toxic shock. J. Immune Based Ther. Vaccines 6, 5 (2008).
84 Van Damme P, Oosterhuis-Kafeja F, Van der Wielen M, Almagor Y, Sharon O, Levin Y. Safety and efficacy of a novel microneedle device for dose sparing intradermal influenza vaccination in healthy adults. Vaccine 27(3), 454–459 (2009).
85 Garland MJ, Caffarel-Salvador E, Migalska K, Woolfson AD, Donnelly RF. Dissolving polymeric microneedle arrays for electrically assisted transdermal drug delivery. J. Control. Release 159(1), 52–59 (2012).
86 Lee JW, Park JH, Prausnitz MR. Dissolving microneedles for transdermal drug delivery. Biomaterials 29(13), 2113–2124 (2008).
87 Sullivan SP, Koutsonanos DG, Del Pilar Martin M et al. Dissolving polymer microneedle patches for influenza vaccination. Nat. Med. 16(8), 915–920 (2010).
88 Raju PA, McSloy N, Truong NK, Kendall MA. Assessment of epidermal cell viability by near infrared multi-photon microscopy following ballistic delivery of gold micro-particles. Vaccine 24(21), 4644–4647 (2006).
89 Levin G, Gershonowitz A, Sacks H et al. Transdermal delivery of human growth
hormone through RF-microchannels. Pharm. Res. 22(4), 550–555 (2005).
90 Ogura M, Sato S, Nakanishi K et al. In vivo targeted gene transfer in skin by the use of laser-induced stress waves. Lasers Surg. Med. 34(3), 242–248 (2004).
91 Lee S, McAuliffe DJ, Mulholland SE, Doukas AG. Photomechanical transdermal delivery of insulin in vivo. Lasers Surg. Med. 28(3), 282–285 (2001).
92 Boucaud A, Garrigue MA, Machet L, Vaillant L, Patat F. Effect of sonication parameters on transdermal delivery of insulin to hairless rats. J. Control. Release 81(1–2), 113–119 (2002).
93 Tokumoto S, Higo N, Sugibayashi K. Effect of electroporation and pH on the iontophoretic transdermal delivery of human insulin. Int. J. Pharm. 326(1–2), 13–19 (2006).
94 Tezel A, Paliwal S, Shen Z, Mitragotri S. Low-frequency ultrasound as a transcutaneous immunization adjuvant. Vaccine 23(29), 3800–3807 (2005).
95 Zhao YL, Murthy SN, Manjili MH, Guan LJ, Sen A, Hui SW. Induction of cytotoxic T-lymphocytes by electroporation-enhanced needle-free skin immunization. Vaccine 24(9), 1282–1290 (2006).
96 Kalia YN, Naik A, Garrison J, Guy RH. Iontophoretic drug delivery. Adv. Drug Deliv. Rev. 56(5), 619–658 (2004).
97 Cázares-Delgadillo J, Naik A, Ganem-Rondero A, Quintanar-Guerrero D, Kalia YN. Transdermal delivery of cytochrome C – a 12.4 kDa protein – across intact skin by constant-current iontophoresis. Pharm. Res. 24(7), 1360–1368 (2007).
98 Kalaria DR, Dubey S, Kalia YN. Clinical applications of transdermal iontophoresis. In: Topical and Transdermal Drug Delivery and Development. Watkinson AC, Benson HA (Eds). John Wiley & Sons Inc., NJ, USA, 67–83 (2012).
99 Murthy SN. Magnetophoresis: an approach to enhance transdermal drug diffusion. Pharmazie 54(5), 377–379 (1999).
100 Murthy SN, Hiremath SR. Physical and chemical permeation enhancers in transdermal delivery of terbutaline sulphate. AAPS PharmSciTech 2(1), E–TN1 (2001).
101 Namjoshi S, Caccetta R, Edwards J, Benson HA. Liquid chromatography assay for 5-aminolevulinic acid: application to in vitro assessment of skin penetration via dermaportation. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 852(1–2), 49–55 (2007).
102 Namjoshi S, Chen Y, Edwards J, Benson HA. Enhanced transdermal delivery of a
dipeptide by dermaportation. Biopolymers 90(5), 655–662 (2008).
103 Krishnan G, Roberts MS, Grice J, Anissimov YG, Benson HA. Enhanced transdermal delivery of 5-aminolevulinic acid and a dipeptide by iontophoresis. Biopolymers 96(2), 166–171 (2011).
104 Sammeta SM, Repka MA, Narasimha Murthy S. Magnetophoresis in combination with chemical enhancers for transdermal drug delivery. Drug Dev. Ind. Pharm. 37(9), 1076–1082 (2011).
105 Lademann J, Richter H, Teichmann A et al. Nanoparticles – an efficient carrier for drug delivery into the hair follicles. Eur. J. Pharm. Biopharm. 66(2), 159–164 (2007).
• Summarizesanimportantdrug-deliveryroutethatcouldbeexploitedfordrug,immuneandgenetherapy.
106 Tinkle SS, Antonini JM, Rich BA et al. Skin as a route of exposure and sensitization in chronic beryllium disease. Environ. Health Perspect. 111(9), 1202–1208 (2003).
• Oneoftheearliestpapershighlightingthepotentialhazardsassociatedwithabsorptionofparticlesintotheskin.
107 Rouse JG, Yang J, Ryman-Rasmussen JP, Barron AR, Monteiro-Riviere NA. Effects of mechanical flexion on the penetration of fullerene amino acid-derivatized peptide nanoparticles through skin. Nano Lett. 7(1), 155–160 (2007).
108 Moresi JM, Horn TD. Distribution of Langerhans cells in human hair follicle. J. Cutan. Pathol. 24(10), 636–640 (1997).
109 Liu X, Grice JE, Lademann J et al. Hair follicles contribute significantly to penetration through human skin only at times soon after application as a solvent deposited solid in man. Br. J. Clin. Pharmacol. 72(5), 768–774 (2011).
110 Toll R, Jacobi U, Richter H, Lademann J, Schaefer H, Blume-Peytavi U. Penetration profile of microspheres in follicular targeting of terminal hair follicles. J. Invest. Dermatol. 123(1), 168–176 (2004).
111 Lademann J, Patzelt A, Richter H, Antoniou C, Sterry W, Knorr F. Determination of the cuticula thickness of human and porcine hairs and their potential influence on the penetration of nanoparticles into the hair follicles. J. Biomed. Opt. 14(2), 021014 (2009).
112 Hojyo-Tomoka MT, Kligman AM. Does cellophane tape stripping remove the horny layer? Arch. Dermatol. 106(5), 767–768 (1972).
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
395www.expert-reviews.com
Review
113 Kammerau B, Zesch A, Schaefer H. Absolute concentrations of dithranol and triacetyl-dithranol in the skin layers after local treatment: in vivo investigations with four different types of pharmaceutical vehicles. J. Invest. Dermatol. 64(3), 145–149 (1975).
114 Weigand DA, Gaylor JR. Removal of stratum corneum in vivo: an improvement on the cellophane tape stripping technique. J. Invest. Dermatol. 60(2), 84–87 (1973).
115 Kalia YN, Pirot F, Guy RH. Homogeneous transport in a heterogeneous membrane: water diffusion across human stratum corneum in vivo. Biophys. J. 71(5), 2692–2700 (1996).
116 Tsai JC, Shen LC, Sheu HM, Lu CC. Tape stripping and sodium dodecyl sulfate treatment increase the molecular weight cutoff of polyethylene glycol penetration across murine skin. Arch. Dermatol. Res. 295(4), 169–174 (2003).
117 El Maghraby GM, Williams AC, Barry BW. Can drug-bearing liposomes penetrate intact skin? J. Pharm. Pharmacol. 58(4), 415–429 (2006).
118 Choi MJ, Maibach HI. Liposomes and niosomes as topical drug delivery systems. Skin Pharmacol. Physiol. 18(5), 209–219 (2005).
119 Godin B, Touitou E. Ethosomes: new prospects in transdermal delivery. Crit. Rev. Ther. Drug Carrier Syst. 20(1), 63–102 (2003).
120 Benson HA. Transfersomes for transdermal drug delivery. Expert Opin. Drug Deliv. 3(6), 727–737 (2006).
121 Geusens B, Van Gele M, Braat S et al. Flexible nanosomes (SECosomes) enable efficient siRNA delivery in cultured primary skin cells and in the viable epidermis of ex vivo human skin. Adv. Funct. Mater. 20(23), 4077–4090 (2010).
122 Lehmann PA, Raney SG, Franz TJ. Skin permeation assessment in man: in vitro–in vivo correlation. In: Topical and Transdermal Drug Delivery and Development. Watkinson AC, Benson HA (Eds). John Wiley & Sons Inc., NJ, USA, 167–182 (2012).
123 Bronaugh RL, Stewart RF. Methods for in vitro percutaneous absorption studies IV: the flow-through diffusion cell. J. Pharm. Sci. 74(1), 64–67 (1985).
124 Feldmann RJ, Maibach HI. Absorption of some organic compounds through the skin in man. J. Invest. Dermatol. 54(5), 399–404 (1970).
125 Schäfer-Korting M, Bock U, Gamer A et al. Reconstructed human epidermis for skin absorption testing: results of the German
prevalidation study. Altern. Lab. Anim. 34(3), 283–294 (2006).
126 Henning A, Neumann D, Kostka KH, Lehr CM, Schaefer UF. Influence of human skin specimens consisting of different skin layers on the result of in vitro permeation experiments. Skin Pharmacol. Physiol. 21(2), 81–88 (2008).
127 Alvarez-Román R, Naik A, Kalia YN, Fessi H, Guy RH. Visualization of skin penetration using confocal laser scanning microscopy. Eur. J. Pharm. Biopharm. 58(2), 301–316 (2004).
128 Tsai TH, Jee SH, Dong CY, Lin SJ. Multiphoton microscopy in dermatological imaging. J. Dermatol. Sci. 56(1), 1–8 (2009).
129 Sanchez WY, Prow TW, Sanchez WH, Grice JE, Roberts MS. Analysis of the metabolic deterioration of ex vivo skin from ischemic necrosis through the imaging of intracellular NAD(P)H by multiphoton tomography and fluorescence lifetime imaging microscopy. J. Biomed. Opt. 15(4), 046008 (2010).
130 Galletly NP, McGinty J, Dunsby C et al. Fluorescence lifetime imaging distinguishes basal cell carcinoma from surrounding uninvolved skin. Br. J. Dermatol. 159(1), 152–161 (2008).
131 König K, Uchugonova A, Gorjup E. Multiphoton fluorescence lifetime imaging of 3D-stem cell spheroids during differentiation. Microsc. Res. Tech. 74(1), 9–17 (2011).
132 Lin LL, Grice JE, Butler MK et al. Time-correlated single photon counting for simultaneous monitoring of zinc oxide nanoparticles and NAD(P)H in intact and barrier-disrupted volunteer skin. Pharm. Res. 28(11), 2920–2930 (2011).
133 Mélot M, Pudney PD, Williamson AM, Caspers PJ, Van Der Pol A, Puppels GJ. Studying the effectiveness of penetration enhancers to deliver retinol through the stratum corneum by in vivo confocal Raman spectroscopy. J. Control. Release 138(1), 32–39 (2009).
134 Peira E, Scolari P, Gasco MR. Transdermal permeation of apomorphine through hairless mouse skin from microemulsions. Int. J. Pharm. 226(1–2), 47–51 (2001).
135 Peltola S, Saarinen-Savolainen P, Kiesvaara J, Suhonen TM, Urtti A. Microemulsions for topical delivery of estradiol. Int. J. Pharm. 254(2), 99–107 (2003).
136 Rhee YS, Choi JG, Park ES, Chi SC. Transdermal delivery of ketoprofen using microemulsions. Int. J. Pharm. 228(1–2), 161–170 (2001).
137 Sintov AC, Shapiro L. New microemulsion vehicle facilitates percutaneous penetration in vitro and cutaneous drug bioavailability in vivo. J. Control. Release 95(2), 173–183 (2004).
138 Wu H, Ramachandran C, Bielinska AU et al. Topical transfection using plasmid DNA in a water-in-oil nanoemulsion. Int. J. Pharm. 221(1–2), 23–34 (2001).
139 Betz G, Aeppli A, Menshutina N, Leuenberger H. In vivo comparison of various liposome formulations for cosmetic application. Int. J. Pharm. 296(1–2), 44–54 (2005).
140 Christensen D, Korsholm KS, Rosenkrands I, Lindenstrøm T, Andersen P, Agger EM. Cationic liposomes as vaccine adjuvants. Expert Rev. Vaccines 6(5), 785–796 (2007).
141 Drulis-Kawa Z, Dorotkiewicz-Jach A. Liposomes as delivery systems for antibiotics. Int. J. Pharm. 387(1–2), 187–198 (2010).
142 Manconi M, Valenti D, Sinico C, Lai F, Loy G, Fadda AM. Niosomes as carriers for tretinoin. II. Influence of vesicular incorporation on tretinoin photostability. Int. J. Pharm. 260(2), 261–272 (2003).
143 Manosroi A, Khanrin P, Werner RG, Götz F, Manosroi W, Manosroi J. Entrapment enhancement of peptide drugs in niosomes. J. Microencapsul. 27(3), 272–280 (2010).
144 Ruckmani K, Sankar V. Formulation and optimization of zidovudine niosomes. AAPS PharmSciTech 11(3), 1119–1127 (2010).
145 Dubey V, Mishra D, Nahar M, Jain V, Jain NK. Enhanced transdermal delivery of an anti-HIV agent via ethanolic liposomes. Nanomedicine 6(4), 590–596 (2010).
146 Fang YP, Huang YB, Wu PC, Tsai YH. Topical delivery of 5-aminolevulinic acid-encapsulated ethosomes in a hyperproliferative skin animal model using the CLSM technique to evaluate the penetration behavior. Eur. J. Pharm. Biopharm. 73(3), 391–398 (2009).
147 Rao Y, Zheng F, Zhang X, Gao J, Liang W. In vitro percutaneous permeation and skin accumulation of finasteride using vesicular ethosomal carriers. AAPS PharmSciTech 9(3), 860–865 (2008).
148 Bendas ER, Tadros MI. Enhanced transdermal delivery of salbutamol sulfate via ethosomes. AAPS PharmSciTech 8(4), E107 (2007).
149 Alvi IA, Madan J, Kaushik D, Sardana S, Pandey RS, Ali A. Comparative study of transfersomes, liposomes, and niosomes for topical delivery of 5-fluorouracil to skin cancer cells: preparation, characterization,
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
Expert Rev. Dermatol. 7(4), (2012)396
Review
in-vitro release, and cytotoxicity analysis. Anticancer. Drugs 22(8), 774–782 (2011).
150 Hofer C, Hartung R, Göbel R, Deering P, Lehmer A, Breul J. New ultradeformable drug carriers for potential transdermal application of interleukin-2 and interferon-α: theoretic and practical aspects. World J. Surg. 24(10), 1187–1189 (2000).
151 Mahor S, Rawat A, Dubey PK et al. Cationic transfersomes based topical genetic vaccine against hepatitis B. Int. J. Pharm. 340(1–2), 13–19 (2007).
152 Farboud ES, Nasrollahi SA, Tabbakhi Z. Novel formulation and evaluation of a Q10-loaded solid lipid nanoparticle cream: in vitro and in vivo studies. Int. J. Nanomedicine 6, 611–617 (2011).
153 Gulbake A, Jain A, Khare P, Jain SK. Solid lipid nanoparticles bearing oxybenzone: in-vitro and in-vivo evaluation. J. Microencapsul. 27(3), 226–233 (2010).
154 Padois K, Cantiéni C, Bertholle V, Bardel C, Pirot F, Falson F. Solid lipid nanoparticles suspension versus commercial solutions for dermal delivery of minoxidil. Int. J. Pharm. 416(1), 300–304 (2011).
155 Schlupp P, Blaschke T, Kramer KD, Höltje HD, Mehnert W, Schäfer-Korting M. Drug release and skin penetration from solid lipid nanoparticles and a base cream: a systematic
approach from a comparison of three glucocorticoids. Skin Pharmacol. Physiol. 24(4), 199–209 (2011).
156 Agrawal Y, Petkar KC, Sawant KK. Development, evaluation and clinical studies of Acitretin loaded nanostructured lipid carriers for topical treatment of psoriasis. Int. J. Pharm. 401(1–2), 93–102 (2010).
157 Chen J, Chen HY, Cui SS et al. Glucosamine derivative modified nanostructured lipid carriers for targeted tumor delivery. J. Mater. Chem. 22(12), 5770–5783 (2012).
158 Pardeike J, Schmidt C, Volz I, Müller RH. Nanostructured lipid carriers as delivery system for the phopholipase A2 inhibitors PX-18 and PX-13 for dermal application. Pharmazie 66(5), 357–361 (2011).
159 Puglia C, Sarpietro MG, Bonina F, Castelli F, Zammataro M, Chiechio S. Development, characterization, and in vitro and in vivo evaluation of benzocaine- and lidocaine-loaded nanostructrured lipid carriers. J. Pharm. Sci. 100(5), 1892–1899 (2011).
160 Hafner A, Lovric J, Pepic I, Filipovic-Grcic J. Lecithin/chitosan nanoparticles for transdermal delivery of melatonin. J. Microencapsul. 28(8), 807–815 (2011).
161 Lboutounne H, Chaulet JF, Ploton C, Falson F, Pirot F. Sustained ex vivo skin
antiseptic activity of chlorhexidine in poly(epsilon-caprolactone) nanocapsule encapsulated form and as a digluconate. J. Control. Release 82(2–3), 319–334 (2002).
162 Morgen M, Lu GW, Du D et al. Targeted delivery of a poorly water-soluble compound to hair follicles using polymeric nanoparticle suspensions. Int. J. Pharm. 416(1), 314–322 (2011).
163 Tomoda K, Terashima H, Suzuki K, Inagi T, Terada H, Makino K. Enhanced transdermal delivery of indomethacin using combination of PLGA nanoparticles and iontophoresis in vivo. Colloids Surf. B. Biointerfaces 92, 50–54 (2012).
164 Prausnitz MR. Microneedles for transdermal drug delivery. Adv. Drug Deliv. Rev. 56(5), 581–587 (2004).
165 Herwadkar A, Sachdeva V, Taylor LF, Silver H, Banga AK. Low-frequency sonophoresis mediated transdermal and intradermal delivery of ketoprofen. Int. J. Pharm. 423(2), 289–296 (2012).
166 Kanebako M, Inagi T, Takayama K. Transdermal delivery of indomethacin by iontophoresis. Biol. Pharm. Bull. 25(6), 779–782 (2002).
Patent
201 Gerstel MS, Place VA: US3964482 (1976).
Leite-Silva, de Almeida, Fradin, Grice & Roberts
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

CME
397www.expert-reviews.com
Review
Delivery of drugs applied topically to the skin
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions (with a minimum 70% passing score) and earn continuing medi-cal education (CME) credit, please go to www.medscape.org/journal/expertderm. Credit cannot be obtained for tests com-pleted on paper, although you may use the worksheet below to keep a record of your answers. You must be a registered user on Medscape.org. If you are not registered on Medscape.org, please click on the New Users: Free Registration link on the left hand side of the website to register. Only one answer is correct for each question. Once you successfully answer all post-test questions you will be able to view and/or print your certificate. For ques-tions regarding the content of this activity, contact the accredited provider, [email protected]. For technical assistance, contact [email protected]. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please refer to http://www.ama-assn.org/ama/pub/category/2922.html. The AMA has determined
that physicians not licensed in the US who participate in this CME activity are eligible for AMAPRACategory1Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit may be acceptable as evidence of participation in CME activities. If you are not licensed in the US, please complete the questions online, print the AMA PRA CME credit certificate and present it to your national medical association for review.
Activity Evaluation Where 1 is strongly disagree and 5 is strongly agree
1 2 3 4 5
1. The activity supported the learning objectives.
2. The material was organized clearly for learning to occur.
3. The content learned from this activity will impact my practice.
4. The activity was presented objectively and free of commercial bias.
1. Which of the following statements regarding the skin and its permeability to drugs is most accurate?
£ A Atopic dermatitis is associated with elevated transepidermal water loss (TEWL)
£ B Stratum corneum (SC) thickness is greatest in the axillae and inner thighs
£ C The skin barrier is strongest among African Americans
£ D The skin barrier is stronger among men vs women
2. Which of the following choices is an important consideration in the development of transdermal drug systems?
£ A Different vehicles will be more or less effective based on the properties of the drug
£ B Ointments are preferred to oil-in-water emulsions by patients
£ C Ionic surfactants have the best skin tolerance
£ D Cationic surfactants are associated with reduced skin penetration
3. Which of the following is a desired quality of a skin penetration enhancer?
£ A It should have a color to help identify that it is working
£ B It should use multiple modes of action to maximize skin penetration
£ C It should have a mechanism of action which mimics that of the active drug
£ D Its effect on the skin barrier should be reversible
4. What else should be considered regarding physical enhancement techniques to improve transdermal drug delivery?
£ A The most successful application of microneedles has been with vaccines
£ B Cavitational technologies are particularly effective for hydrophobic macromolecules
£ C Iontophoresis does not improve delivery of larger molecules
£ D The hair follicle should be avoided as a drug delivery site
Delivery of drugs applied topically to the skin
Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.

Exp
ert R
evie
w o
f D
erm
atol
ogy
Dow
nloa
ded
from
info
rmah
ealth
care
.com
by
McM
aste
r U
nive
rsity
on
10/1
6/14
For
pers
onal
use
onl
y.